Depression and Anxiety Changes Associated with Matched Increases in Physical Activity in Education-, Self-Regulation-, and Self-Regulation Plus Relaxation-Based Obesity Treatments in Women: A Pilot Study Investigating Implications for Controlling Emotional Eating
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Data Analyses
3. Results
3.1. Score Changes, Across Treatment Types
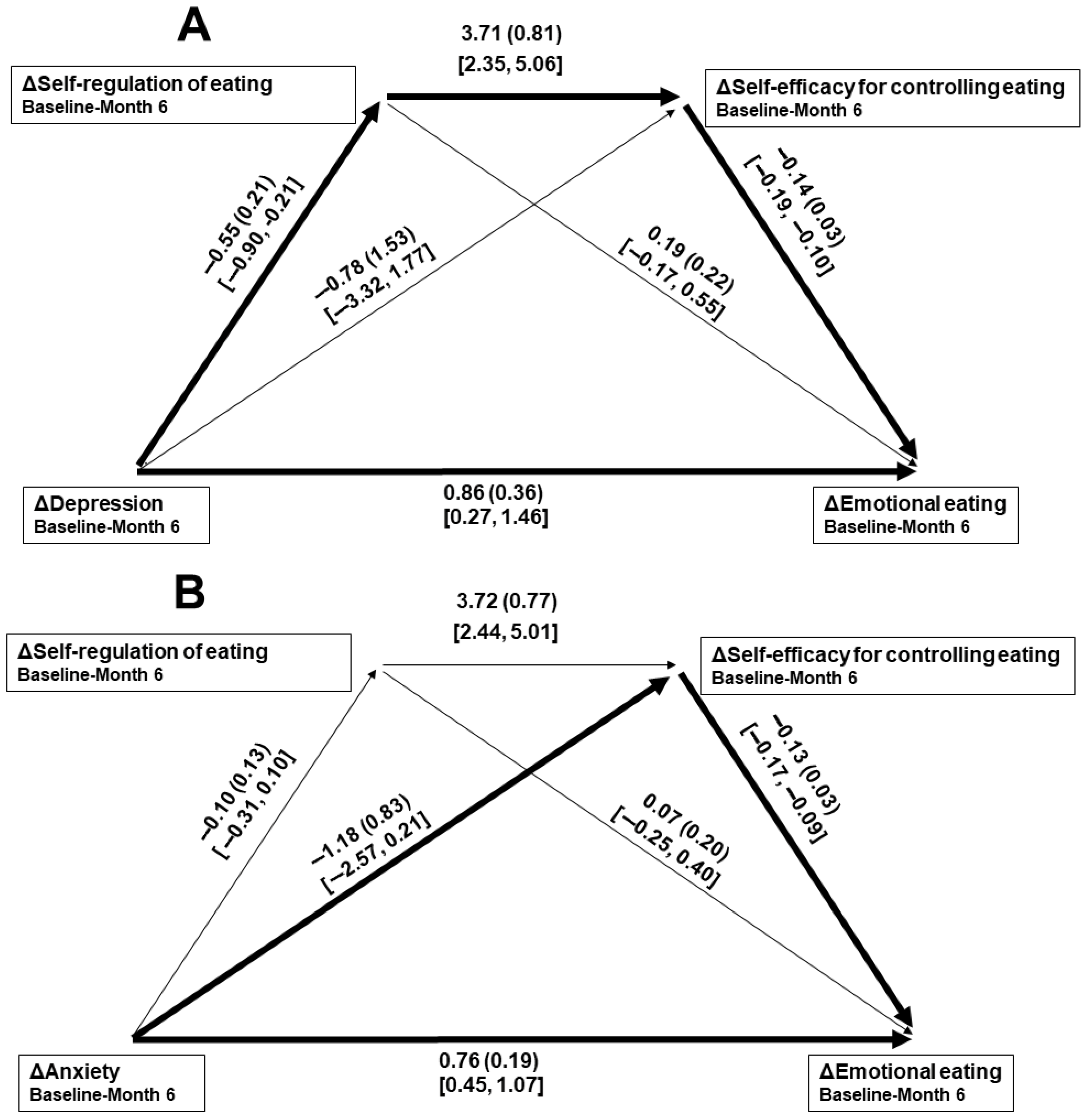
3.2. Regression Analyses Predicting Emotional Eating Changes
3.3. Weight Changes, by Treatment Types
3.4. Post Hoc Analyses of Psychosocial Predictors of Weight Changes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2021 US Obesity Forecasting Collaborators. National-level and state-level prevalence of overweight and obesity among children, adolescents, and adults in the USA, 1990–2021, and forecasts up to 2050. Lancet 2024, 404, 2278–2298. [Google Scholar] [CrossRef] [PubMed]
- Koenders, P.G.; van Strien, T. Emotional eating, rather than lifestyle behavior, drives weight gain in a prospective study in 1562 employees. J. Occup. Environ. Med. 2011, 53, 1287–1293. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.M.; Serier, K.N.; Belon, K.E.; Sebastian, R.M.; Smith, J.E. Evaluation of the relationships between dietary restraint, emotional eating, and intuitive eating moderated by sex. Appetite 2020, 155, 104817. [Google Scholar] [CrossRef] [PubMed]
- Dakanalis, A.; Mentzelou, M.; Papadopoulou, S.K.; Papandreou, D.; Spanoudaki, M.; Vasios, G.K.; Pavlidou, E.; Mantzorou, M.; Giaginis, C. The association of emotional eating with overweight/obesity, depression, anxiety/stress, and dietary patterns: A review of the current clinical evidence. Nutrients 2023, 15, 1173. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Lau, S.T.; Lau, Y. Weight-loss interventions for improving emotional eating among adults with high body mass index: A systematic review with meta-analysis and meta-regression. Eur. Eat. Disord. Rev. 2022, 30, 304–327. [Google Scholar] [CrossRef]
- Frayn, M.; Knäuper, B. Emotional eating and weight in adults: A review. Curr. Psychol. 2018, 37, 924–933. [Google Scholar] [CrossRef]
- Smith, J.; Ang, X.Q.; Giles, E.L.; Traviss-Turner, G. Emotional eating interventions for adults living with overweight or obesity: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2023, 20, 2722. [Google Scholar] [CrossRef]
- Knoedler, S.; Matar, D.Y.; Friedrich, S.; Knoedler, L.; Haug, V.; Hundeshagen, G.; Kauke-Navarro, M.; Kneser, U.; Pomahac, B.; Orgill, D.P.; et al. The surgical patient of yesterday, today, and tomorrow—A time-trend analysis based on a cohort of 8.7 million surgical patients. Int. J. Surg. 2023, 109, 2631–2640. [Google Scholar] [CrossRef]
- Kosmalski, M.; Deska, K.; Bąk, B.; Różycka-Kosmalska, M.; Pietras, T. Pharmacological support for the treatment of obesity-present and future. Healthcare 2023, 11, 433. [Google Scholar] [CrossRef]
- Salas, X.R. The ineffectiveness and unintended consequences of the public health war on obesity. Can. J. Public Health 2015, 106, e79–e81. [Google Scholar] [CrossRef]
- Arent, S.M.; Walker, A.J.; Arent, M.A. The effects of exercise on anxiety and depression. In Handbook of Sport Psychology, 4th ed.; Tennenbaum, G., Eklund, R.C., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2020; pp. 872–890. [Google Scholar]
- Annesi, J.J.; Eberly, A.A. Early effects of improved mood on propensity for emotional eating during the physical activity-only phase of a community-based behavioral treatment for obesity in women with high mood disturbance. Health Behav. Res. 2022, 5, 4. [Google Scholar] [CrossRef]
- Annesi, J.J. Contrast of biochemical and psychosocial explanations of the relationship of exercise and improved mood. Percept. Mot. Skil. 2012, 114, 693–697. [Google Scholar] [CrossRef] [PubMed]
- Wipfli, B.M.; Rethorst, C.D.; Landers, D.M. The anxiolytic effects of exercise: A meta-analysis of randomized trials and dose-response analysis. J. Sport Exerc. Psychol. 2008, 30, 392–410. [Google Scholar] [CrossRef]
- Collado-Mateo, D.; Lavín-Pérez, A.M.; Peñacoba, C.; Del Coso, J.; Leyton-Román, M.; Luque-Casado, A.; Gasque, P.; Fernández-Del-Olmo, M.Á.; Amado-Alonso, D. Key factors associated with adherence to physical exercise in patients with chronic diseases and older adults: An umbrella review. Int. J. Environ. Res. Public Health 2021, 18, 2023. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.G.; Owen, N.; Bauman, A.E.; Sallis, J.F.; Brown, W. Correlates of adults’ participation in physical activity: Review and update. Med. Sci. Sports Exerc. 2002, 34, 1996–2001. [Google Scholar] [CrossRef] [PubMed]
- Annesi, J.J. Behavioral weight loss and maintenance: A 25-year research program informing innovative programming. Perm. J. 2002, 26, 98–117. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Macht, M. How emotions affect eating: A five-way model. Appetite 2008, 50, 1–11. [Google Scholar] [CrossRef]
- White, R.L.; Vella, S.; Biddle, S.; Sutcliffe, J.; Guagliano, J.M.; Uddin, R.; Burgin, A.; Apostolopoulos, M.; Nguyen, T.; Young, C.; et al. Physical activity and mental health: A systematic review and best-evidence synthesis of mediation and moderation studies. Int. J. Behav. Nutr. Phys. Act. 2024, 21, 134. [Google Scholar] [CrossRef]
- Di Corrado, D. Biological underpinnings of mood and the role of physical exercise. Sport Sci. Health 2017, 13, 461–468. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Bandura, A. The primacy of self-regulation in health promotion. Appl. Psychol.-Int. Rev. 2005, 54, 245–254. [Google Scholar] [CrossRef]
- Baumeister, R.F.; Tice, D.M.; Vohs, K.D. The strength model of self-regulation: Conclusions from the second decade of willpower research. Perspect. Psychol. Sci. 2018, 13, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman: New York, NY, USA, 1997. [Google Scholar]
- Khir, S.M.; Wan Mohd Yunus, W.M.A.; Mahmud, N.; Wang, R.; Panatik, S.A.; Mohd Sukor, M.S.; Nordin, N.A. Efficacy of progressive muscle relaxation in adults for stress, anxiety, and depression: A systematic review. Psychol. Res. Behav. Manag. 2024, 2024, 345–365. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.S.; Winett, R.A.; Wojcik, J.R. Self-regulation, self-efficacy, outcome expectations, and social support: Social cognitive theory and nutrition behavior. Ann. Behav. Med. 2007, 34, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Konttinen, H.; Silventoinen, K.; Sarlio-Lähteenkorva, S.; Männistö, S.; Haukkala, A. Emotional eating and physical activity self-efficacy as pathways in the association between depressive symptoms and adiposity indicators. Am. J. Clin. Nutr. 2010, 92, 1031–1039. [Google Scholar] [CrossRef]
- Ling, J.; Zahry, N.R. Relationships among perceived stress, emotional eating, and dietary intake in college students: Eating self-regulation as a mediator. Appetite 2021, 163, 105215. [Google Scholar] [CrossRef]
- White, K.; Kendrick, T.; Yardley, L. Change in self-esteem, self-efficacy and the mood dimensions of depression as potential mediators of the physical activity and depression relationship: Exploring the temporal relation of change. Ment. Health Phys. Act. 2009, 2, 44–52. [Google Scholar] [CrossRef]
- Galesic, M.; Bosnjak, M. Effects of questionnaire length on participation and indicators of response quality in a web survey. Pub. Opin. Q. 2009, 73, 349–360. [Google Scholar] [CrossRef]
- Godin, G. The Godin-Shephard Leisure-Time Physical Activity Questionnaire. Health Fit. J. Can. 2011, 4, 18–22. [Google Scholar] [CrossRef]
- Amireault, S.; Godin, G. The Godin-Shephard Leisure Time Physical Activity Questionnaire: Validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Percept. Mot. Skil. 2015, 120, 604–622. [Google Scholar] [CrossRef]
- Amireault, S.; Godin, G.; Lacombe, J.; Sabiston, C.M. Validation of the Godin-Shephard Leisure-Time Physical Activity Questionnaire classification coding system using accelerometer assessment among breast cancer survivors. J. Cancer Surviv. 2015, 9, 532–540. [Google Scholar] [CrossRef]
- Jacobs, D.R.; Ainsworth, B.E.; Hartman, T.J.; Leon, A.S. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med. Sci. Sports Exerc. 1993, 25, 81–91. [Google Scholar] [CrossRef]
- Miller, D.J.; Freedson, P.S.; Kline, G.M. Comparison of activity levels using Caltrac accelerometer and five questionnaires. Med. Sci. Sports Exerc. 1994, 26, 376–382. [Google Scholar] [CrossRef]
- Pereira, M.A.; FitzGerald, S.J.; Gregg, E.W.; Joswiak, M.L.; Ryan, W.J.; Suminski, R.R.; Utter, A.C.; Zmuda, J.M. A collection of physical activity questionnaires for health-related research. Med. Sci. Sports Exerc. 1997, 29 (Suppl. S6), S1–S205. [Google Scholar]
- McNair, D.M.; Heuchert, J.W.P. Profile of Mood States Technical Update; Multi-Health Systems: North Tonawanda, NY, USA, 2009. [Google Scholar]
- Arnow, B.; Kenardy, J.; Agras, W.S. The Emotional Eating Scale: The development of a measure to assess coping with negative affect by eating. Int. J. Eat. Disord. 1995, 18, 79–90. [Google Scholar] [CrossRef]
- Annesi, J.J.; Marti, C.N. Path analysis of exercise treatment-induced changes in psychological factors leading to weight loss. Psychol. Health 2011, 26, 1081–1098. [Google Scholar] [CrossRef]
- Clark, M.M.; Abrams, D.B.; Niaura, R.S.; Eaton, C.A.; Rossi, J.S. Self-efficacy in weight management. J. Consult. Clin. Psychol. 1991, 59, 739–744. [Google Scholar] [CrossRef]
- National Institutes of Health/National Cancer Institute. Evidence-Based Cancer Control Program: Obesity. Available online: https://ebccp.cancercontrol.cancer.gov/topicPrograms.do?topicId=1592287&choice=default (accessed on 1 July 2025).
- Champion, V.L.; Skinner, C.S. The health belief model. In Health Behavior: Theory, Research, and Practice, 5th ed.; Glanz, K., Rimer, B.K., Viswanath, K.V., Eds.; Jossey-Bass/Wiley: Hoboken, NJ, USA, 2015; pp. 45–65. [Google Scholar]
- Brownell, K.D. The LEARN Program for Weight Management, 10th ed.; American Health Publishing: Dallas, TX, USA, 2004. [Google Scholar]
- Aljadani, H.M.; Patterson, A.; Sibbritt, D.; Hutchesson, M.J.; Jensen, M.E.; Collins, C.E. Diet quality, measured by fruit and vegetable intake, predicts weight change in young women. J. Obes. 2013, 2013, 525161. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Darmon, N.; Briend, A. Replacing fats and sweets with vegetables and fruits–a question of cost. Am. J. Public Health 2004, 94, 1555–1559. [Google Scholar] [CrossRef] [PubMed]
- Te Morenga, L.; Mallard, S.; Mann, J. Dietary sugars and body weight: Systematic review and meta-analysis of randomized controlled trials and cohort studies. BMJ 2012, 346, e7492. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, D.A.; Carlson, C.R.; Schmidt, J.E. Progressive Relaxation: Abbreviated Methods. In Principles and Practice of Stress Management, 3rd ed.; Lehrer, P.M., Woolfolk, R.L., Sime, W.E., Eds.; Guilford: New York, NY, USA, 2017; pp. 88–122. [Google Scholar]
- Michie, S.; Ashford, S.; Sniehotta, F.F.; Dombrowski, S.U.; Bishop, A.; French, D.P. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy. Psychol. Health 2011, 26, 1479–1498. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services/Office of Disease Prevention and Health Promotion. Physical Activity Guidelines for Americans. Available online: https://odphp.health.gov/our-work/nutrition-physical-activity/physical-activity-guidelines (accessed on 1 July 2025).
- Rosenthal, R. Interpersonal Expectations: Effects of the Experimenter’s Hypothesis. In Artifacts in Behavioral Research; Rosenthal, R., Rosnow, R.L., Eds.; Oxford University Press: Cary, NC, USA, 2009; pp. 138–210. [Google Scholar]
- White, I.R.; Horton, N.J.; Carpenter, J.; Pocock, S.J. Strategy for intention to treat data in randomized trials with missing outcome data. BMJ 2011, 342, d40. [Google Scholar] [CrossRef] [PubMed]
- Little, R.J.; Rubin, D.B. Statistical Analysis with Missing Data, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2014. [Google Scholar]
- McLachlan, G.J.; Krishnan, T. The EM Algorithm and Extensions; John Wiley & Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
- Cohen, J.; Cohen, P.; West, S.G.; Aiken, L.S. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences, 3rd ed.; Lawrence Erlbaum Publishers: Mahwah, NJ, USA, 2003. [Google Scholar]
- Teixeira, P.J.; Carraça, E.V.; Marques, M.M.; Rutter, H.; Oppert, J.M.; De Bourdeaudhuij, I.; Lakerveld, J.; Brug, J. Successful behavior change in obesity interventions in adults: A systematic review of self-regulation mediators. BMC Med. 2015, 13, 84. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; Guilford: New York, NY, USA, 2022. [Google Scholar]
- Sharafi, S.E.; Garmaroudi, G.; Ghafouri, M.; Bafghi, S.A.; Tabesh, M.R.; Alizadeh, Z. Prevalence of anxiety and depression in patients with overweight and obesity. Obes. Med. 2020, 17, 100169. [Google Scholar] [CrossRef]
- Baranowski, T.; Anderson, C.; Carmack, C. Mediating variable framework in physical activity interventions: How are we doing? How might we do better? Am. J. Prevent. Med. 1998, 15, 266–297. [Google Scholar] [CrossRef]
- Cerin, E.; Mackinnon, D.P. A commentary on current practice in mediating variable analyses in behavioural nutrition and physical activity. Public Health Nutr. 2009, 12, 1182–1188. [Google Scholar] [CrossRef]
- Dent, R.; McPherson, R.; Harper, M.E. Factors affecting weight loss variability in obesity. Metab. Clin. Exp. 2020, 113, 154388. [Google Scholar] [CrossRef]

| Demographic Characteristic | Educational Methods (n = 28) | Self-Regulation Methods (n = 24) | Self-Regulation + Relaxation (n = 24) | F/χ2 | p |
|---|---|---|---|---|---|
| Age, M (SD), years | 46.36 (6.25) | 44.71 (11.05) | 46.63 (10.14) | 0.38 a | 0.736 |
| Body mass index (BMI), M (SD), kg/m2 | 35.58 (2.89) | 35.15 (3.22) | 35.26 (3.08) | 0.14 a | 0.868 |
| Racial/ethnic group, n (%) | 6.01 b | 0.198 | |||
| White | 27 (96.4%) | 18 (75.0%) | 18 (75.0%) | ||
| Black | 1 (3.6%) | 3 (12.5%) | 3 (12.5%) | ||
| Hispanic | 0 (0.0%) | 3 (12.5%) | 3 (12.5%) | ||
| Yearly family income, n (%) | 3.27 b | 0.774 | |||
| <US $25,000 | 4 (14.3%) | 1 (4.2%) | 2 (8.3%) | ||
| US $25,000–US $49,999 | 12 (42.9%) | 9 (37.5%) | 9 (37.5%) | ||
| US $50,000–US $99,999 | 11 (39.2%) | 12 (50.0%) | 10 (41.7%) | ||
| ≥US $100,000 | 1 (3.6%) | 2 (8.3%) | 3 (12.5%) | ||
| Educational level, n (%) | 1.13 b | 0.981 | |||
| High school/GED | 6 (21.4%) | 4 (16.7%) | 4 (16.7%) | ||
| Some college | 6 (21.4%) | 5 (20.8%) | 5 (20.8%) | ||
| Bachelor’s degree | 9 (32.2%) | 6 (25.0%) | 7 (29.2%) | ||
| More than bachelor’s degree | 7 (25.0%) | 9 (37.5%) | 8 (33.3%) |
| Measure | Baseline | Month 3 | Month 6 | ΔBaseline–Month 3 | ΔBaseline–Month 6 | Overall Change | Change × Treatment Type | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment Type | M | SD | M | SD | M | SD | M | SD | M | SD | F(1, 73) | p | η2partial | F(1, 73) | p | η2partial |
| Physical activity | ||||||||||||||||
| Educational methods | 8.43 | 8.31 | 23.32 | 10.68 | 25.14 | 13.87 | 14.89 | 5.01 | 16.71 | 8.44 | ||||||
| Self-regulation methods | 8.85 | 7.43 | 26.31 | 8.07 | 30.38 | 13.46 | 17.46 | 4.77 | 21.52 | 9.88 | ||||||
| Self-regulation + relaxation | 8.48 | 7.65 | 25.63 | 8.44 | 29.69 | 12.77 | 17.15 | 4.79 | 21.21 | 8.98 | ||||||
| Aggregated data | 8.58 | 7.73 | 24.99 | 9.20 | 28.23 | 13.44 | 16.41 | 4.94 | 19.65 | 9.24 | 359.84 | <0.001 | 0.83 | 2.33 | 0.105 | 0.06 |
| Depression | ||||||||||||||||
| Educational methods | 3.14 | 2.53 | 1.64 | 1.39 | 2.57 | 1.89 | −1.50 | 2.20 | −0.57 | 1.83 | ||||||
| Self-regulation methods | 4.00 | 3.28 | 2.04 | 2.74 | 1.54 | 2.02 | −1.96 | 2.73 | −2.46 | 2.19 | ||||||
| Self-regulation + relaxation | 4.17 | 3.47 | 2.13 | 2.88 | 1.53 | 2.03 | −2.04 | 2.73 | −2.63 | 2.30 | ||||||
| Aggregated data | 3.74 | 3.09 | 1.92 | 2.37 | 1.92 | 2.01 | −1.82 | 2.52 | −1.82 | 2.28 | 60.81 | <0.001 | 0.45 | 7.81 | <0.001 | 0.18 |
| Anxiety | ||||||||||||||||
| Educational methods | 3.96 | 2.10 | 3.54 | 2.33 | 3.50 | 3.12 | −0.43 | 2.39 | −0.46 | 2.73 | ||||||
| Self-regulation methods | 4.71 | 5.00 | 2.25 | 2.56 | 1.88 | 2.03 | −2.46 | 4.59 | −2.83 | 4.77 | ||||||
| Self-regulation + relaxation | 4.63 | 4.85 | 2.17 | 2.33 | 1.71 | 1.63 | −2.46 | 4.58 | −2.92 | 4.74 | ||||||
| Aggregated data | 4.41 | 4.07 | 2.70 | 2.46 | 2.42 | 2.50 | −1.71 | 3.99 | −1.99 | 4.23 | 19.10 | <0.001 | 0.21 | 3.03 | 0.055 | 0.08 |
| Emotional eating | ||||||||||||||||
| Educational methods | 27.96 | 12.46 | 32.93 | 9.36 | 24.46 | 10.92 | 4.96 | 6.70 | −3.50 | 6.39 | ||||||
| Self-regulation methods | 27.58 | 8.93 | 28.25 | 12.04 | 18.58 | 8.93 | 0.67 | 10.03 | −9.67 | 10.03 | ||||||
| Self-regulation + relaxation | 27.54 | 12.28 | 27.42 | 9.69 | 18.42 | 9.69 | −0.13 | 9.10 | −9.13 | 9.10 | ||||||
| Aggregated data | 27.92 | 12.11 | 29.50 | 9.58 | 20.70 | 10.23 | 1.58 | 8.90 | −7.22 | 8.90 | 57.27 | <0.001 | 0.44 | 4.24 | 0.018 | 0.10 |
| Self-regulation of eating | ||||||||||||||||
| Educational methods | 17.71 | 4.56 | 21.54 | 4.94 | 20.09 | 4.51 | 3.83 | 3.87 | 2.37 | 3.98 | ||||||
| Self-regulation methods | 17.87 | 4.04 | 24.07 | 3.32 | 25.03 | 3.03 | 6.20 | 4.65 | 7.17 | 3.87 | ||||||
| Self-regulation + relaxation | 18.50 | 4.48 | 24.48 | 3.45 | 25.53 | 3.28 | 5.98 | 4.72 | 7.03 | 4.25 | ||||||
| Aggregated data | 18.01 | 4.33 | 23.27 | 4.19 | 23.37 | 4.45 | 5.26 | 4.48 | 5.36 | 4.60 | 141.62 | <0.001 | 0.66 | 12.14 | <0.001 | 0.25 |
| Self-efficacy for controlling eating | ||||||||||||||||
| Educational methods | 89.96 | 32.39 | 98.18 | 23.87 | 96.93 | 24.35 | 8.21 | 29.79 | 6.96 | 30.86 | ||||||
| Self-regulation methods | 86.50 | 30.88 | 115.54 | 22.91 | 120.71 | 22.59 | 29.04 | 34.92 | 34.21 | 34.90 | ||||||
| Self-regulation + relaxation | 89.46 | 31.14 | 116.08 | 24.94 | 124.10 | 24.66 | 26.63 | 33.56 | 34.65 | 33.59 | ||||||
| Aggregated data | 88.71 | 31.14 | 109.32 | 25.11 | 113.02 | 26.67 | 20.61 | 33.62 | 24.31 | 35.22 | 44.24 | <0.001 | 0.38 | 6.11 | 0.004 | 0.14 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. ΔDepression B–3 | --- | |||||||||
| 2. ΔDepression B–6 | 0.67 ** | --- | ||||||||
| 3. ΔAnxiety B–3 | 0.42 ** | 0.21 | --- | |||||||
| 4. ΔAnxiety B–6 | 0.23 * | 0.27 * | 0.89 ** | --- | ||||||
| 5. ΔEmotional eating B–3 | 0.34 ** | 0.29 * | 0.45 ** | 0.46 ** | --- | |||||
| 6. ΔEmotional eating B–6 | 0.36 ** | 0.32 * | 0.46 ** | 0.46 ** | 0.98 ** | --- | ||||
| 7. ΔSelf-regulation of eating B–3 | −0.08 | 0.00 | −0.01 | 0.18 | −0.31 * | −0.29 * | --- | |||
| 8. ΔSelf-regulation of eating B–6 | −0.14 | −0.29 * | −0.17 | −0.10 | −0.27 * | −0.25 * | 0.68 ** | --- | ||
| 9. ΔSelf-efficacy for controlled eating B–3 | −0.24 * | −0.02 | −0.26 * | −0.14 | −0.49 ** | −0.44 ** | 0.60 ** | 0.37 ** | --- | |
| 10. ΔSelf-efficacy for controlled eating B–6 | −0.23 * | −0.20 * | −0.20 * | −0.19 | −0.61 ** | −0.56 ** | 0.45 ** | 0.50 ** | 0.79 ** | --- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Annesi, J.J.; Machek, S.B. Depression and Anxiety Changes Associated with Matched Increases in Physical Activity in Education-, Self-Regulation-, and Self-Regulation Plus Relaxation-Based Obesity Treatments in Women: A Pilot Study Investigating Implications for Controlling Emotional Eating. Nutrients 2025, 17, 2475. https://doi.org/10.3390/nu17152475
Annesi JJ, Machek SB. Depression and Anxiety Changes Associated with Matched Increases in Physical Activity in Education-, Self-Regulation-, and Self-Regulation Plus Relaxation-Based Obesity Treatments in Women: A Pilot Study Investigating Implications for Controlling Emotional Eating. Nutrients. 2025; 17(15):2475. https://doi.org/10.3390/nu17152475
Chicago/Turabian StyleAnnesi, James J., and Steven B. Machek. 2025. "Depression and Anxiety Changes Associated with Matched Increases in Physical Activity in Education-, Self-Regulation-, and Self-Regulation Plus Relaxation-Based Obesity Treatments in Women: A Pilot Study Investigating Implications for Controlling Emotional Eating" Nutrients 17, no. 15: 2475. https://doi.org/10.3390/nu17152475
APA StyleAnnesi, J. J., & Machek, S. B. (2025). Depression and Anxiety Changes Associated with Matched Increases in Physical Activity in Education-, Self-Regulation-, and Self-Regulation Plus Relaxation-Based Obesity Treatments in Women: A Pilot Study Investigating Implications for Controlling Emotional Eating. Nutrients, 17(15), 2475. https://doi.org/10.3390/nu17152475







