The WHO BMI System Misclassifies Weight Status in Adults from the General Population in North Italy: A DXA-Based Assessment Study (18–98 Years)
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Design of the Study
2.2. Body Weight and Height
2.3. Body Composition
- For males:
- 18–39 years BF% < 8% (underweight); ≥8% (normal weight); ≥21% (overweight; ≥26% (obesity);
- 40–59 years BF% < 11% (underweight); ≥11% (normal weight); ≥23% (overweight; ≥29% (obesity);
- 60–98 years BF% < 13% (underweight); ≥13% (normal weight); ≥25% (overweight; ≥31% (obesity).
- For females:
- 18–39 years BF% < 21% (underweight); ≥21% (normal weight); ≥33% (overweight; ≥39% (obesity);
- 40–59 years BF% < 23% (underweight); ≥23% (normal weight); ≥35% (overweight; ≥41% (obesity);
- 60–98 years BF% < 26% (underweight); ≥26% (normal weight); ≥36% (overweight; ≥41% (obesity).
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Findings and Concordance with Previous Studies
4.2. Strengths and Limitations
4.3. Clinical Implications and New Directions for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nuttall, F. Body Mass Index. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef]
- Stenholm, S.; Head, J.; Aalto, V.; Kivimäki, M.; Kawachi, I.; Zins, M.; Goldberg, M.; Platts, L.G.; Zaninotto, P.; Magnusson Hanson, L.L.; et al. Body mass index as a predictor of healthy and disease-free life expectancy between ages 50 and 75: A multicohort study. Int. J. Obes. 2017, 41, 769–775. [Google Scholar] [CrossRef]
- Pett, K.D.; Willett, W.C.; Vartiainen, E.; Katz, D. The Seven Countries Study. Eur. Heart J. 2017, 38, 3119–3121. [Google Scholar] [CrossRef]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut Off Points. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Adult BMI Categories. Available online: https://www.cdc.gov/bmi/adult-calculator/bmi-categories.html (accessed on 20 May 2025).
- Overweight and Obesity Management. Available online: https://www.nice.org.uk/guidance/ng246 (accessed on 20 May 2025).
- Nevill, A.M.; Holder, R. Body mass index: A measure of fatness or leanness? Br. J. Nutr. 1995, 73, 507–516. [Google Scholar] [CrossRef]
- Orsi, E.; Solini, A.; Penno, G.; Bonora, E.; Fondelli, C.; Trevisan, R.; Vedovato, M.; Cavalot, F.; Lamacchia, O.; Haxhi, J.; et al. Body mass index versus surrogate measures of central adiposity as independent predictors of mortality in type 2 diabetes. Cardiovasc. Diabetol. 2022, 21, 266. [Google Scholar] [CrossRef]
- Kennedy, A.P.; Shea, J.L.; Sun, G. Comparison of the classification of obesity by BMI vs. dual-energy X-ray absorptiometry in the Newfoundland population. Obesity 2009, 17, 2094–2099. [Google Scholar] [CrossRef]
- Huang, C.; Lopes, A.; Britton, A. Which adiposity index is best? Comparison of five indicators and their ability to identify type 2 diabetes risk in a population study. Diabetes Res. Clin. Pract. 2025, 225, 112268. [Google Scholar] [CrossRef]
- Shanks, C.B.; Bruening, M.; Yaroch, A. BMI or not to BMI? debating the value of body mass index as a measure of health in adults. Int. J. Behav. Nutr. Phys. Act. 2025, 22, 23. [Google Scholar] [CrossRef]
- Wu, Y.; Li, D.; Vermund, S. Advantages and Limitations of the Body Mass Index (BMI) to Assess Adult Obesity. Int. J. Environ. Res. Public Health 2024, 21, 757. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Itani, L.; El Ghoch, M.; Gualtieri, P.; Frank, G.; Raffaelli, G.; Pellegrini, M.; Di Renzo, L. Difference in Body Composition Patterns between Age Groups in Italian Individuals with Overweight and Obesity: When BMI Becomes a Misleading Tool in Nutritional Settings. Nutrients 2024, 16, 2415. [Google Scholar] [CrossRef]
- Kyle, U.G.; Genton, L.; Hans, D.; Karsegard, L.; Slosman, D.O.; Pichard, C. Age-related differences in fat-free mass, skeletal muscle, body cell mass and fat mass between 18 and 94 years. Eur. J. Clin. Nutr. 2001, 55, 663–672. [Google Scholar] [CrossRef]
- Marra, M.; Sammarco, R.; De Lorenzo, A.; Iellamo, F.; Siervo, M.A.; Pietrobelli, A.; Donini, L.M.; Santarpia, L.; Cataldi, M.; Pasanisi, F.; et al. Assessment of Body Composition in Health and Disease Using Bioelectrical Impedance Analysis (BIA) and Dual Energy X-Ray Absorptiometry (DXA): A Critical Overview. Contrast Media Mol. Imaging 2019, 2019, 3548284. [Google Scholar] [CrossRef]
- Bodell, L.P.; Mayer, L. Percent Body Fat is a Risk Factor for Relapse in Anorexia Nervosa: A Replication Study. Int. J. Eat. Disord. 2011, 44, 118–123. [Google Scholar] [CrossRef]
- Lin, T.Y.; Lim, P.S.; Hung, S. Impact of Misclassification of Obesity by Body Mass Index on Mortality in Patients with CKD. Kidney Int. Rep. 2017, 3, 447–455. [Google Scholar] [CrossRef]
- Golubnitschaja, D.; Liskova, A.; Koklesova, L.; Samec, M.; Biringer, K.; Büsselberg, D.; Podbielska, H.; Kunin, A.A.; Evsevyeva, M.E.; Shapira, N.; et al. Caution, “normal” BMI: Health risks associated with potentially masked individual underweight-EPMA Position Paper 2021. EPMA J. 2021, 12, 243–264. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Del Gobbo, V.; Premrov, M.G.; Bigioni, M.; Galvano, F.; Di Renzo, L. Normal-weight obese syndrome: Early inflammation? Am. J. Clin. Nutr. 2007, 85, 40–45. [Google Scholar] [CrossRef]
- Potter, A.W.; Chin, G.C.; Looney, D.P.; Friedl, K. Defining Overweight and Obesity by Percent Body Fat Instead of Body Mass Index. JCEM 2025, 100, e1103–e1107. [Google Scholar] [CrossRef]
- How Does BMI Affect the Cost of Life Insurance? Available online: https://extendfinance.co.uk/how-does-bmi-affect-the-cost-of-life-insurance/ (accessed on 23 June 2025).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef]
- Düppe, H.; Gärdsell, P.; Hanson, B.S.; Johnell, O.; Nilsson, B.E. Importance of participation rate in sampling of data in population based studies, with special reference to bone mass in Sweden. J. Epidemiol. Community Health 1996, 50, 170–173. [Google Scholar] [CrossRef]
- International Society for Advancement of Kinanthropometry. International Standards for Anthropometric Assessment; International Society for Advancement of Kinanthropometry: Potchefstroom, South Africa, 2001. [Google Scholar]
- Cavedon, V.; Milanese, C.; Zancanaro, C. Are body circumferences able to predict strength, muscle mass and bone characteristics in obesity? A preliminary study in women. Int. J. Med. Sci. 2020, 17, 881–891. [Google Scholar] [CrossRef]
- Cavedon, V.; Zancanaro, C.; Milanese, C. Anthropometric prediction of DXA-measured body composition in female team handball players. PeerJ 2018, 6, e5913. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, D.; Heymsfield, S.B.; Heo, M.; Jebb, S.A.; Murgatroyd, P.R.; Sakamoto, Y. Healthy percentage body fat ranges: An approach for developing guidelines based on body mass index. Am. J. Clin. Nutr. 2000, 72, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.; Wright, C. The kappa statistic in reliability studies: Use, interpretation, and sample size requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Weighted kappa: Nominal scale agreement provision for scaled disagreement or partial credit. Psychol. Bull. 1968, 70, 213–220. [Google Scholar] [CrossRef]
- McHugh, M. Interrater reliability: The kappa statistic. Biochem. Medica 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Bogduk, N. On understanding reliability for diagnostic tests. Interv. Pain Med. 2022, 1, 100124. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows; Version 27.0; IBM Corp.: Armonk, NY, USA, 2020. [Google Scholar]
- NCSS 2023 Statistical Software; NCSS, LLC.: Kaysville, UT, USA, 2023; Available online: https://www.ncss.com/software/ncss/ (accessed on 10 May 2025).
- Jahanlou, A.S.; Kouzekanani, K. The Accuracy of Body Mass Index and Gallagher’s Classification in Detecting Obesity among Iranians. Iran. J. Med. Sci. 2016, 41, 288–295. [Google Scholar]
- Itani, L.; Kreidieh, D.; El Masri, D.; Tannir, H.; Chehade, L.; El Ghoch, M. Revising BMI Cut-Off Points for Obesity in a Weight Management Setting in Lebanon. Int. J. Environ. Res. Public Health 2020, 17, 3832. [Google Scholar] [CrossRef]
- Di Renzo, L.; Itani, L.; Gualtieri, P.; Pellegrini, M.; El Ghoch, M.; De Lorenzo, A. New BMI Cut-Off Points for Obesity in Middle-Aged and Older Adults in Clinical Nutrition Settings in Italy: A Cross-Sectional Study. Nutrients 2022, 14, 4848. [Google Scholar] [CrossRef]
- Wan Nudri, W.D.; Wan Abdul Manan, W.M.; Rusli, A. Body Mass Index and Body Fat Status of Men Involved in Sports, Exercise, and Sedentary Activites. Malays. J. Med. Sci. 2009, 16, 21–26. [Google Scholar]
- Grier, T.; Canham-Chervak, M.; Sharp, M.; Jones, B. Does body mass index misclassify physically active young men. Prev. Med. Rep. 2015, 2, 483–487. [Google Scholar] [CrossRef]
- Lahav, Y.; Kfir, A.; Gepner, Y. The paradox of obesity with normal weight; a cross-sectional study. Front. Nutr. 2023, 10, 1173488. [Google Scholar] [CrossRef]
- Kaluski, D.N.; Keinan-Boker, L.; Stern, F.; Green, M.S.; Leventhal, A.; Goldsmith, R.; Chinich, A.; Berry, E. BMI may overestimate the prevalence of obesity among women of lower socioeconomic status. Obesity 2007, 15, 1808–1815. [Google Scholar] [CrossRef]
- Charbonneau-Roberts, G.; Saudny-Unterberger, H.; Kuhnlein, H.V.; Egeland, G. Body mass index may overestimate the prevalence of overweight and obesity among the Inuit. Int. J. Circumpolar Health 2005, 64, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Bagust, A.; Walley, T. An alternative to body mass index for standardizing body weight for stature. QJM 2000, 93, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Bredella, M.A.; Ghomi, R.H.; Thomas, B.J.; Torriani, M.; Brick, D.J.; Gerweck, A.V.; Misra, M.; Klibanski, A.; Miller, K. Comparison of DXA and CT in the Assessment of Body Composition in Premenopausal Women with Obesity and Anorexia Nervosa. Obesity 2010, 18, 2227–2233. [Google Scholar] [CrossRef]
- LaForgia, J.; Dollman, J.; Dale, M.J.; Withers, R.T.; Hill, A. Validation of DXA body composition estimates in obese men and women. Obesity 2009, 17, 821–826. [Google Scholar] [CrossRef] [PubMed]
- Murad, M.H.; Katabi, A.; Benkhadra, R.; Montori, V. External validity, generalisability, applicability and directness: A brief primer. BMJ Evid. Based Med. 2018, 23, 17–19. [Google Scholar] [CrossRef]
- Hackshaw, A. Small studies: Strengths and limitations. Eur. Respir. J. 2008, 32, 1141–1143. [Google Scholar] [CrossRef]
- Delgado, R.; Tibau, X.A. Why Cohen’s Kappa should be avoided as performance measure in classification. PLoS ONE 2019, 14, e0222916. [Google Scholar] [CrossRef]
- Bradbury, K.E.; Guo, W.; Cairns, B.J.; Armstrong, M.E.G.; Key, T.J. Association between physical activity and body fat percentage, with adjustment for BMI: A large cross-sectional analysis of UK Biobank. BMJ Open 2017, 7, e011843. [Google Scholar] [CrossRef] [PubMed]
- Goss, A.M.; Goree, L.L.; Ellis, A.C.; Chandler-Laney, P.C.; Casazza, K.; Lockhart, M.E.; Gower, B.A. Effects of diet macronutrient composition on body composition and fat distribution during weight maintenance and weight loss. Obesity 2013, 21, 1139–1142. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Park, S.J.; Choi, S.; Han, M.; Cho, Y.; Oh, Y.H.; Park, S.M. Effect of changes in sleeping behavior on skeletal muscle and fat mass: A retrospective cohort study. BMC Public Health 2023, 23, 1879. [Google Scholar] [CrossRef] [PubMed]
- Audrain-McGovern, J.; Benowitz, N.L. Cigarette Smoking, Nicotine, and Body Weight. Clin. Pharmacol. Ther. 2011, 90, 164–168. [Google Scholar] [CrossRef]
- Solem, R. Limitation of a cross-sectional study. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 205. [Google Scholar] [CrossRef]
- Itani, L.; El Ghoch, M. Waist-to-Height Ratio Cut-Off Points for Central Obesity in Individuals with Overweight Across Different Ethnic Groups in NHANES 2011–2018. Nutrients 2024, 16, 3838. [Google Scholar] [CrossRef]
- Tinsley, G.M.; Rodriguez, C.; Florez, C.M.; Siedler, M.R.; Tinoco, E.; McCarthy, C.; Heymsfield, S.B. Smartphone three-dimensional imaging for body composition assessment using non-rigid avatar reconstruction. Front. Med. 2024, 11, 1485450. [Google Scholar] [CrossRef]

| Total (n = 1351) | Males (n = 541) | Females (n = 810) | Significance | |
|---|---|---|---|---|
| Age (year) | 45.5 (21.4) | 49.7 (21.7) | 42.7 (20.7) | p < 0.001 γ |
| Weight (kg) | 69.6 (13.8) | 77.7 (11.8) | 64.3 (12.3) | p < 0.001 ¥ |
| Height (cm) | 166.9 (8.7) | 173.6 (6.2) | 162.4 (7.2) | p < 0.001 γ |
| BMI (kg/m2) | 25.0 (4.6) | 25.8 (3.9) | 24.5 (5.0) | p < 0.001 γ |
| ALM (kg) | 20.5 (4.9) | 25.1 (3.5) | 17.4 (2.9) | p < 0.001 γ |
| Body fat (kg) | 19.4 (8.4) | 17.8 (7.4) | 20.5 (8.8) | p < 0.001 γ |
| Body fat (%) | 27.7 (8.7) | 22.5 (6.7) | 31.2 (8.1) | p < 0.001 γ |
| BMI Classification ¥ | Body Fat (%) Classification £ | |
|---|---|---|
| Underweight | 19 (1.4) | 84 (6.2) |
| Normal weight | 787 (58.3) | 773 (57.2) |
| Overweight | 354 (26.2) | 316 (23.4) |
| Obesity | 191 (14.1) | 178 (13.2) |
| BMI Classification | |||||||
|---|---|---|---|---|---|---|---|
| BF% Classification | Underweight | Normal Weight | Overweight | Obesity | Total | Chi-Squared | Weighted Kappa |
| Under fat | 6 (31.6%) | 76 (9.7%) | 2 (0.6%) | 0 (0.0%) | 84 (6.2%) | X2 = 884.17; p < 0.001 | 0.126, p < 0.0001 |
| Normal fat | 13 (68.4%) | 615 (78.1%) | 141 (39.8%) | 4 (2.1%) | 773 (57.2%) | ||
| Over fat | 0 (0.0%) | 90 (11.4%) | 165 (46.6%) | 61 (31.9%) | 316 (23.4%) | ||
| Excess fat | 0 (0.0%) | 6 (0.8%) | 46 (13.0%) | 126 (66.0%) | 178 (13.2%) | ||
| Males (n = 541) | Females (n = 810) | Total (n = 1351) | ||||
|---|---|---|---|---|---|---|
| Age Group | Correctly Classified | Misclassified | Correctly Classified | Misclassified | Correctly Classified | Misclassified |
| Overall sample | ||||||
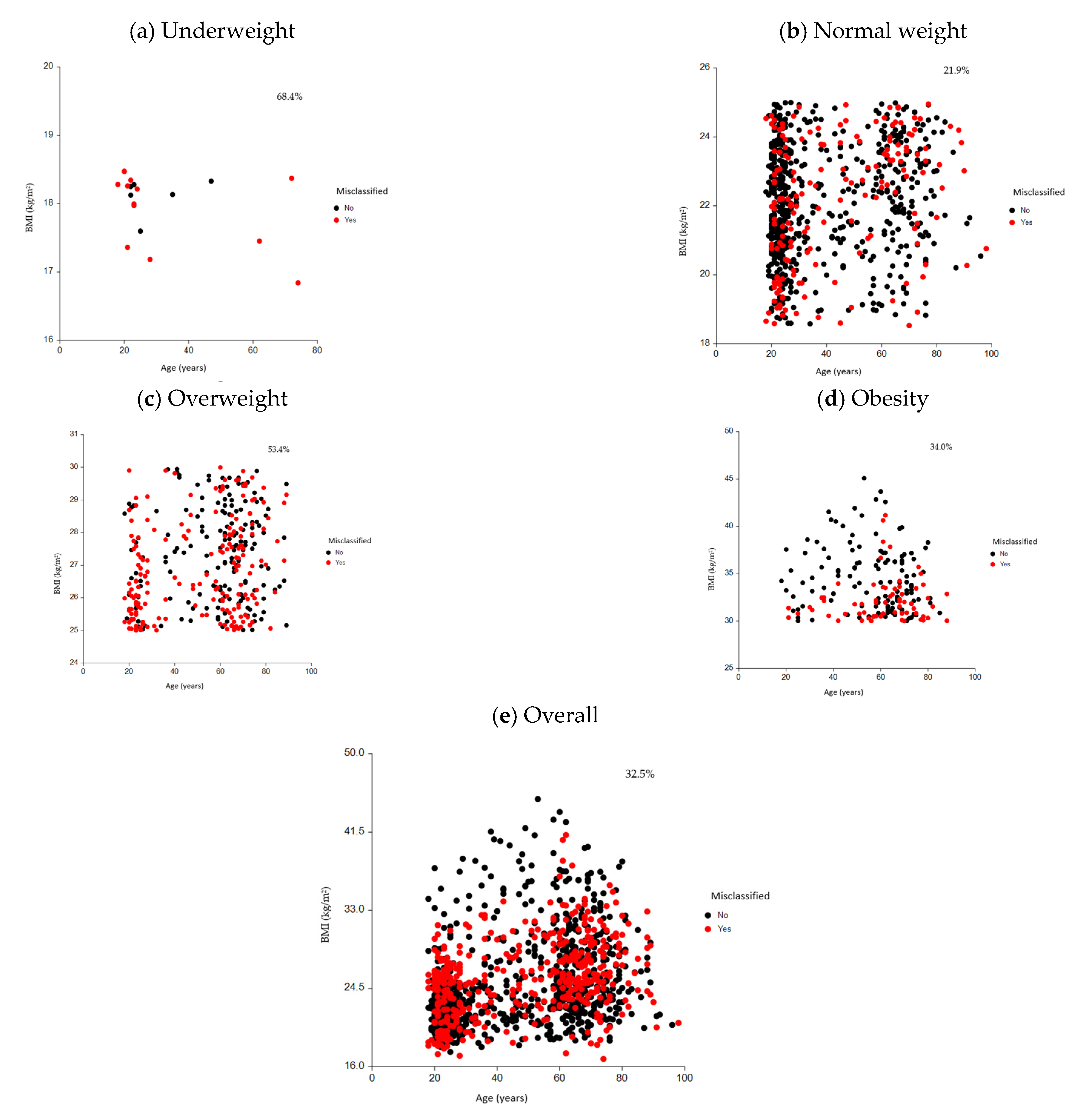
| Total | 364 (67.3%) | 177 (32.7%) | 548 (67.7%) | 262 (32.3%) | 912 (67.5%) | 439 (32.5%) |
| 18–39 | 157 (43.1%) | 59 (33.3%) | 301 (54.9%) | 126 (48.1%) | 458 (50.2%) | 185 (42.1%) |
| 40–59 | 34 (9.3%) | 20 (11.3%) | 107 (19.5%) | 41 (15.6%) | 141 (15.5%) | 61 (13.9%) |
| 60–79 | 161 (44.2%) | 92 (52.0%) | 129 (23.5%) | 79 (30.2%) | 290 (31.8%) | 171 (39.0%) |
| 80+ | 12 (3.3%) | 6 (3.4%) | 11 (2.0%) | 16 (6.1%) | 23 (2.5%) | 22 (5.0%) |
| BMI < 18.5 kg/m2 | ||||||
| Total | 0(0.0) | 4 (100) | 6 (40.0) | 9 (60.0) | 6 (31.6) | 13 (68.4) |
| 18–39 | 0(0.0) | 1(100) | 5 (35.7) | 9 (64.3) | 5 (33.3) | 10 (66.7) |
| 40–59 | 0(0.0) | 0(0.0) | 1 (100.0) | 0(0.0) | 1(100) | 0(0.0) |
| 60–79 | 0(0.0) | 3(100) | 0(0.0) | 0(0.0) | 0(0.0) | 3(100) |
| 80+ | 0(0.0) | 0(0.0) | 0(0.0) | 0(0.0) | 0(0.0) | 0(0.0) |
| 18.5 ≤ BMI < 25 kg/m2 | ||||||
| Total | 219 (83.3) | 44 (16.7) | 396 (75.6) | 128 (24.4) | 615 (78.1) | 172 (21.9) |
| 18–39 | 136 (90.1) | 15 (9.9) | 262 (76.6) | 80 (23.4) | 398 (80.7) | 95 (19.3) |
| 40–59 | 17 (89.5) | 2 (10.5) | 53 (71.6) | 21 (28.4) | 70 (75.3) | 23 (24.7) |
| 60–79 | 64 (72.7) | 24 (27.3) | 73 (77.7) | 21 (22.3) | 137 (75.3) | 45 (24.7) |
| 80+ | 2 (40.0) | 3 (60.0) | 8 (57.1) | 6 (42.9) | 10 (52.6) | 9 (47.4) |
| 25 ≤ BMI < 30 kg/m2 | ||||||
| Total | 94 (47.7) | 103 (52.3) | 71 (45.2) | 86 (54.8) | 165 (46.6) | 189 (53.4) |
| 18–39 | 15 (28.3) | 38 (71.7) | 16 (32.7) | 33 (67.3) | 31 (30.4) | 71 (69.6) |
| 40–59 | 8 (38.1) | 13 (61.9) | 25 (71.4) | 10 (28.6) | 33 (58.9) | 23 (41.1) |
| 60–79 | 64 (56.6) | 49 (43.4) | 28 (42.4) | 38 (57.6) | 92 (51.4) | 87 (48.6) |
| 80+ | 7 (70.0) | 3 (30.0) | 2 (28.6) | 5 (71.4) | 9 (52.9) | 8 (47.1) |
| BMI ≥ 30 kg/m2 | ||||||
| Total | 51 (66.2) | 26 (33.8) | 75 (65.8) | 39 (34.2) | 126 (66.0) | 65 (34.0) |
| 18–39 | 6 (54.5) | 5 (45.5) | 18 (81.8) | 4 (18.2) | 24 (72.7) | 9 (27.3) |
| 40–59 | 9 (64.3) | 5 (35.7) | 28 (73.7) | 10 (26.3) | 37 (71.2) | 15 (28.8) |
| 60–79 | 33 (67.3) | 16 (32.7) | 28 (58.3) | 20 (41.7) | 61 (62.9) | 36 (37.1) |
| 80+ | 3 (100.0) | 0 (0.0) | 1 (16.7) | 5 (83.3) | 4 (44.4) | 5 (55.6) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Milanese, C.; Itani, L.; Cavedon, V.; El Ghoch, M. The WHO BMI System Misclassifies Weight Status in Adults from the General Population in North Italy: A DXA-Based Assessment Study (18–98 Years). Nutrients 2025, 17, 2162. https://doi.org/10.3390/nu17132162
Milanese C, Itani L, Cavedon V, El Ghoch M. The WHO BMI System Misclassifies Weight Status in Adults from the General Population in North Italy: A DXA-Based Assessment Study (18–98 Years). Nutrients. 2025; 17(13):2162. https://doi.org/10.3390/nu17132162
Chicago/Turabian StyleMilanese, Chiara, Leila Itani, Valentina Cavedon, and Marwan El Ghoch. 2025. "The WHO BMI System Misclassifies Weight Status in Adults from the General Population in North Italy: A DXA-Based Assessment Study (18–98 Years)" Nutrients 17, no. 13: 2162. https://doi.org/10.3390/nu17132162
APA StyleMilanese, C., Itani, L., Cavedon, V., & El Ghoch, M. (2025). The WHO BMI System Misclassifies Weight Status in Adults from the General Population in North Italy: A DXA-Based Assessment Study (18–98 Years). Nutrients, 17(13), 2162. https://doi.org/10.3390/nu17132162







