Nutritional Risk Factors Model of Community-Dwelling Older People in Poland–Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Questionnaire
2.3. Statistical Analysis
3. Results
3.1. Characteristics of Study Sample
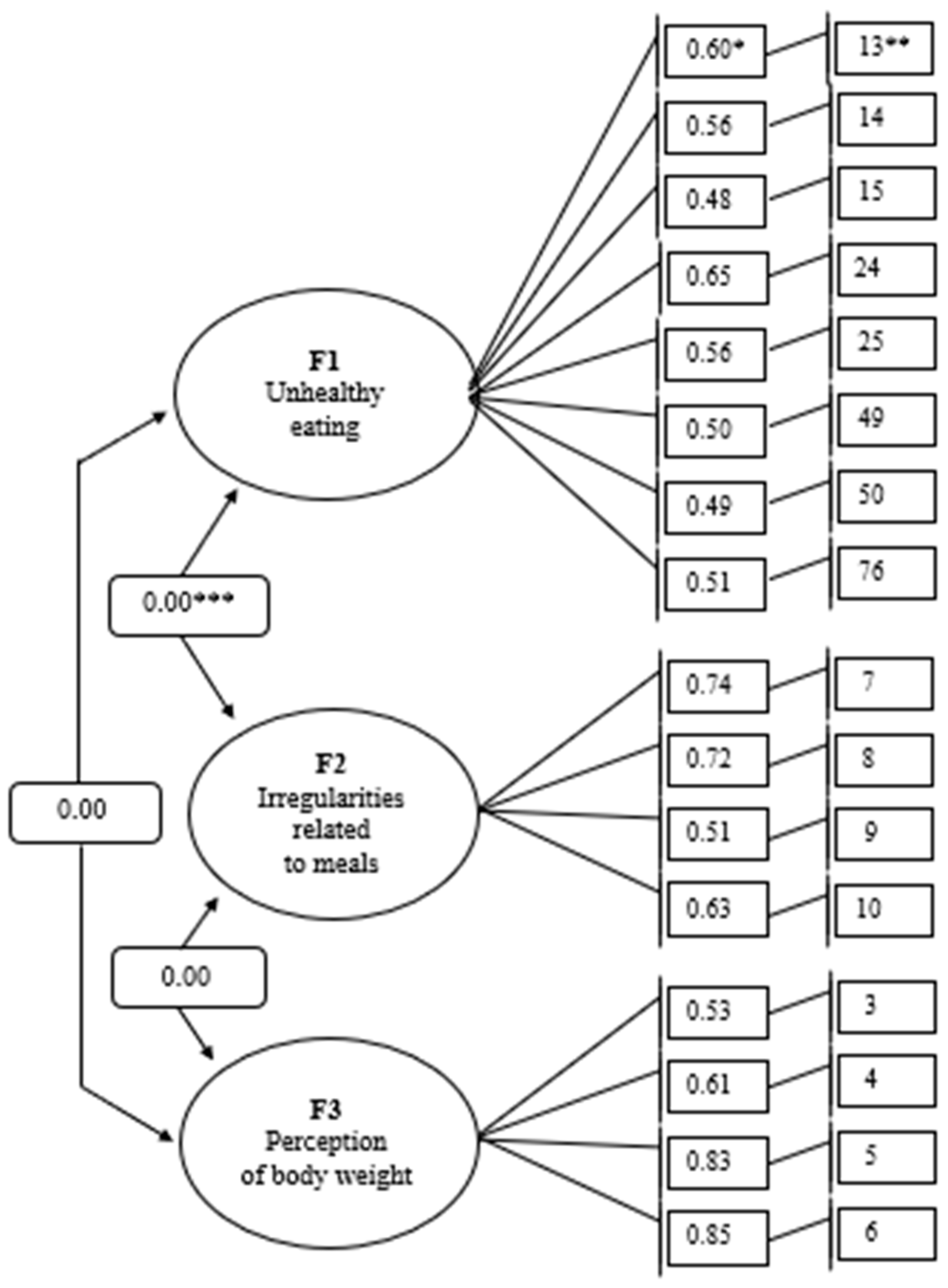
3.2. Structure of the Factorial Model
3.3. Characteristics of Factorial Model
3.4. Sociodemographic and Economic Determinants of the Nutritional Risk Factors
4. Discussion
4.1. Limitations of the Study
4.2. Practical Application of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Test Item Number | Description of the Situation |
|---|---|
| 1 | My body weight has increased in the last 6 months. |
| 2 | My body weight has decreased in the last 6 months. |
| 3 | I would like to increase my body weight. |
| 4 | I would like to decrease my body weight. |
| 5 | I think my body weight is too high. |
| 6 | I think my body weight is too low. |
| 7 | I usually eat three or fewer meals a day. |
| 8 | I usually eat six or more meals a day. |
| 9 | Breaks between my meals are less than two hours. |
| 10 | Breaks between my meals are longer than four hour. |
| 11 | I eat irregularly, that is, at different times of the day. |
| 12 | I happen not to eat main meals such as breakfast or dinner. |
| 13 | I usually limit or omit healthy foods from my meals. |
| 14 | Usually, my meals have little variety (I usually eat the same thing every day). |
| 15 | Usually, my meals are not healthy (e.g., I eat fast food). |
| 16 | Usually, the portions of my meals are too small. |
| 17 | Usually, the portions of my meals are too large. |
| 18 | I usually eat even if I’m not hungry. |
| 19 | I often feel hungry. |
| 20 | I rarely feel hungry. |
| 21 | I often have an appetite (desire to eat). |
| 22 | I rarely have an appetite (reluctance to eat). |
| 23 | I usually overeat unhealthy food between meals, such as candy, salty snacks, fast food, etc. |
| 24 | I eat fresh (raw) vegetables or fruits less than twice a day. |
| 25 | Any vegetables and fruits I eat less than twice a day (e.g., raw, cooked, pickled). |
| 26 | I usually eat vegetables and fruits between meals instead of during meals. |
| 27 | I eat potatoes or potato dishes (e.g., boiled potatoes, baked potatoes, potato noodles, potato pancakes, etc.) more than once a day. |
| 28 | I eat potatoes or potato dishes (e.g., boiled potatoes, baked potatoes, potato noodles, potato pancakes, etc.) rarely or not at all. |
| 29 | Grain products (e.g., bread, groats, rice, pasta, etc.) I usually eat more than four times a day. |
| 30 | Grain products (e.g., bread, groats, rice, pasta, etc.) I usually eat less than twice a day. |
| 31 | I eat whole grain cereal products (e.g., wholemeal or graham bread, dark pasta, coarse groats, brown rice, etc.) once a week or less frequently. |
| 32 | I eat processed grain products (e.g., light bread, white rice, fine groats, light pasta, sweet rolls, croissants, etc.) at least once a day. |
| 33 | My daily meals include fried foods such as meat or flour dishes. |
| 34 | I usually use butter for food preparation or to spread on bread. |
| 35 | I usually use margarine or a mix of butter and margarine to prepare meals or spread on bread. |
| 36 | I usually use lard or other animal fat (other than butter) to prepare meals or to spread on bread. |
| 37 | I usually use oil or olive oil to prepare meals. |
| 38 | I eat red meat, fatty cold cuts, offal meats, and processed meat products such as canned goods more than once daily. |
| 39 | I eat fish less than twice a week. |
| 40 | I eat two eggs less than once a week. |
| 41 | I eat two eggs more than once a week. |
| 42 | I eat legumes (e.g., peas, broad beans, soybeans, lentils, chickpeas, etc.) less than once a week. |
| 43 | I drink two glasses of milk or dairy drinks less than once a day. |
| 44 | I usually drink sweetened dairy drinks (e.g., flavoured milk, cocoa, coffee with milk and sugar or honey). |
| 45 | I drink natural fermented dairy beverages (e.g., natural yogurt, kefir, buttermilk, etc.) less than once a day. |
| 46 | I usually drink sweetened fermented milk drinks (e.g., flavoured yogurt, kefir, buttermilk, etc.). |
| 47 | I eat yellow cheeses, including processed and blue cheese, more than once daily. |
| 48 | I eat cottage cheese, including homogenised and granular cheese, less than once a day. |
| 49 | Prepared store-bought foods (refrigerated or frozen, e.g., soups, dumplings, croquettes, potato noodles, dumplings, etc., which can be quickly cooked or reheated in the microwave) I eat every day. |
| 50 | I eat powdered soups or canned or jarred foods, etc., every day. |
| 51 | When preparing dishes or eating them at the table, I usually add salt to them. |
| 52 | I usually use sugar for cooking and sweetening drinks. |
| 53 | I usually drink less than six glasses/cups of water per day, such as filtered tap, spring or mineral water (do not include flavoured waters). |
| 54 | I usually drink sweetened hot beverages (e.g., tea, herbal infusions, coffee, etc.) |
| 55 | I usually drink more than two cups or two mugs of coffee in a day. |
| 56 | I drink sweetened carbonated or non-carbonated drinks every day or almost every day. |
| 57 | I drink one glass or one cup of freshly squeezed juice less than once a day. |
| 58 | I drink one glass or one cup of sweetened juice “from the carton” or from a bottle more than once a day. |
| 59 | I drink energy drinks (such as 2KC, Black Horse, Red Bull, Burn, Shot, and others) more than once a week. |
| 60 | I drink strong alcoholic beverages (e.g., pure spirits, whiskey, brandy, etc.) more than once a week. |
| 61 | I eat nuts, almonds, and seeds less than once a week. |
| 62 | I take vitamin D in tablets or another form, such as liquid, less than once a day. |
| 63 | I take various dietary supplements (e.g., vitamins, minerals, omega-3 fatty acids, etc.) without consulting a doctor or nutritionist or reading the leaflet. |
| 64 | Instead of a meal, I consume dietary supplements (such as tablets, powder, or liquid). |
| 65 | Instead of a meal, I consume special products for nutrition (e.g., shakes, nutri-drinks, bars, etc.). |
| 66 | I usually have trouble biting or chewing when consuming a meal or drink. |
| 67 | I usually get choked up when consuming a meal or drink. |
| 68 | Usually, the consumption of a meal or drink triggers a coughing fit. |
| 69 | I usually experience gastrointestinal discomfort while eating a meal. |
| 70 | I usually get heartburn during or after a meal. |
| 71 | I usually get severe bloating or gas during or after a meal. |
| 72 | I usually experience constipation during the day. |
| 73 | I usually have diarrhoea after a meal. |
| 74 | I usually experience painful bowel movements during the day. |
| 75 | I have problems buying food. |
| 76 | I have trouble choosing healthy foods when shopping. |
| 77 | I have a problem accessing the foods I like. |
| 78 | I have difficulty accessing any food. |
| 79 | I’m having trouble getting help with food purchases. |
| 80 | I have a problem preparing meals at home. |
| 81 | I’m having trouble getting help preparing meals at home. |
| 82 | I have trouble eating at the table on my own. |
| 83 | I eat too little because I don’t like to eat alone. |
| 84 | I eat too much because I eat alone. |
| 85 | I eat too little because I have health problems that make it difficult for me to leave the house or get to the store for groceries. |
| 86 | I eat too little because I have health problems that make it difficult for me to prepare meals. |
| 87 | I eat too little because people close to me restrict my access to food. |
| 88 | I eat too much because people close to me force me to eat. |
| 89 | I eat too little because people close to me do not want to prepare meals for me, even though I have trouble preparing them. |
| 90 | I eat too little because I don’t know how to prepare meals. |
| 91 | I eat too little because I don’t like to prepare meals. |
| 92 | I eat too little because I have trouble eating on my own and in this situation I do not receive help from loved ones. |
| 93 | I eat too little because I have trouble eating on my own, and in this situation I do not receive help from the State (e.g., welfare centres). |
| 94 | I eat too much because I like to prepare meals. |
| 95 | Consumption of drugs reduces my appetite. |
| 96 | Consumption of drugs increases my appetite. |
| 97 | Consumption of drugs discourages me from eating. |
References
- Eurostat. Ageing Europe—Statistics on Population Development. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Ageing_Europe_-_statistics_on_population_developments (accessed on 21 June 2025).
- United Nations. World Population Ageing 2020: Highlights; United Nations, Department of Economic and Social Afiairs, Population Division: New York, NY, USA, 2020; ISBN 978-92-1-148347-5. [Google Scholar]
- Informacja o Sytuacji Osób Starszych w Polsce za 2023 Rok. Available online: https://www.google.com/search?q=populacja+os%C3%B3b+starszych+w+polsce+w+2023 (accessed on 12 August 2024).
- Afshar, S.; Roderick, P.J.; Kowal, P.; Dimitrov, B.D.; Hill, A.G. Multimorbidity and the inequalities of global ageing: A crosssectional study of 28 countries using the World Health Surveys. BMC Public Health 2015, 15, 776. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.J.; Wu, F.; Guo, Y.; Gutierrez Robledo, L.M.; O’Donnell, M.; Sullivan, R.; Yusuf, S. The burden of disease in older people and implications for health policy and practice. Lancet 2015, 385, 549–562. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Statistics 2021: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-002705-3.
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Chen, A.; Jacobsen, K.H.; Deshmukh, A.A.; Cantor, S.B. The evolution of the disability-adjusted life year (DALY). Soc.-Econ. Plan. Sci. 2015, 49, 10–15. [Google Scholar] [CrossRef]
- Vesnaver, E.; Keller, H.H.; Sutherland, O.; Maitland, S.B.; Locher, J.L. Food behawior change in late-life windowhood: A two-stange proces. Appetite 2015, 95, 399–407. [Google Scholar] [CrossRef]
- Alvarenga, M.; Figueiredo, M.; Timerman, F.; Antonaccio, C. Nutrição Comportamental, 2nd ed.; Manole: São Paulo, Brazil, 2019. [Google Scholar]
- González-Monroy, C.; Gómez-Gómez, I.; Olarte-Sánchez, C.M.; Motrico, E. Eating behaviour changes during the COVID-19 pandemic: A systematics review of longitudinal studies. Int. J. Environ. Res. Public Health 2021, 18, 11130. [Google Scholar] [CrossRef] [PubMed]
- Frates, B.; Smith, A. Nutrition and behawior change: A review of recent literaturę. Curr. Opin. Clin. Nutr. Metab. Care 2022, 22, 407–414. [Google Scholar] [CrossRef]
- Govindaraju, T.; Owen, A.J.; McCaffrey, T.A. Past, present and future influences of diet among older adults—A scoping review. Aging Res. Rev. 2022, 77, 101600. [Google Scholar] [CrossRef]
- White, J.V.; Ham, R.J.; Lipschitz, D.A.; Dwyer, J.T.; Wellman, N.S. Consensus of the Nutrition Screening Initiative: Risk factors and indicators of poor nutritional status in older Americans. J. Am. Diet. Assoc. 1991, 91, 783–787. [Google Scholar] [CrossRef]
- Council on Practice Quality Management Committee. Identifying patients at risk: ADA’s definitions for nutrition screening and nutrition assessment. J. Am. Diet. Assoc. 1994, 94, 838–839. [Google Scholar] [CrossRef]
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.L.; Aravkin, A.Y.; Zheng, P.; Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Czenczek-Lewandowska, E.; Wyszyńska, J.; Leszczak, J.; Baran, J.; Weres, A.; Mazur, A.; Lewandowski, B. Health behaviours of young adults during the outbreak of the COVID-19 pandemic—A longitudinal study. BMC Public Health 2021, 21, 1038. [Google Scholar] [CrossRef] [PubMed]
- Deschasaux-Tanguy, M.; Druesne-Pecollo, N.; Esseddik, Y.; De Edelenyi, F.S.; Allès, B.; Andreeva, V.A.; Baudry, J.; Charreire, H.; Deschamps, V.; Egnell, M.; et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March–May 2020): Results from the French NutriNet-Santé cohort study. Am. J. Clin. Nutr. 2021, 113, 924–938. [Google Scholar] [CrossRef] [PubMed]
- Herle, M.; Smith, A.D.; Bu, F.; Steptoe, A.; Fancourt, D. Trajectories of eating behavior during COVID-19 lockdown: Longitudinal analyses of 22,374 adults. Clin. Nutr. ESPEN 2021, 42, 158–165. [Google Scholar] [CrossRef]
- Maffoni, S.; Brazzo, S.; De Giuseppe, R.; Biino, G.; Vietti, I.; Pallavicini, C.; Cena, H. Lifestyle changes and body mass index during COVID-19 pandemic lockdown: An Italian online-survey. Nutrients 2021, 13, 1117. [Google Scholar] [CrossRef]
- Szostak-Węgierek, D. (Ed.) Żywienie Osób Starszych; PZWL: Warszawa, Poland, 2020; pp. 1–5. [Google Scholar]
- Błędowski, P. Sytuacja materialna. In Badanie Poszczególnych Obszarów Zdrowia Osób Starszych, w Tym Jakości Życia Związanej ze Zdrowiem; Błędowski, P., Grodzicki, T., Mossakowska, M., Zdrojewski, T., Eds.; Gdański Uniwersytet Medyczny: Gdańsk, Poland, 2021; pp. 851–855. [Google Scholar]
- Older Adult Nutrition Screening. Available online: https://olderadultnutritionscreening.com (accessed on 12 July 2022).
- Krzymińska-Siemieszko, R.; Lewandowicz, M.; Wieczorowska-Tobis, K. Niedożywienie jako wielki problem geriatryczny. Geriatria 2016, 10, 179–183. [Google Scholar]
- Borkent, J.W.; Naumann, E.; Vasse, E.; van der Heijden, E.; de van der Schueren, M.A.E. Prevelence and determinants of undernutrition in a sample of dutch community-dwelling older adults: Results from two online screening tools. Int. J. Environ. Res. Public Health 2019, 16, 1562. [Google Scholar] [CrossRef]
- Gajewska, D.; Gosa, P. Dietary intervention effectiveness clinical outcomes and nutrient and salicylate intakes in older adults living in long-term care homes: The results from the senior’s plate project. Nutrients 2022, 14, 871. [Google Scholar] [CrossRef]
- Wądołowska, L. Żywieniowe Podłoże Zagrożeń Zdrowia w Polsce; Uniwersytetu Warmińsko-Mazurskiego w Olsztynie: Olsztyn, Poland, 2010; pp. 84–94. [Google Scholar]
- Barkoukis, H. Nutrition recomendations in elderly and aging. Med. Clin. 2016, 100, 1237–1250. [Google Scholar] [CrossRef]
- Narodowe Centrum Edukacji Żywieniowej. Dział. Żywienie Osób w Starszym Wieku. Available online: https://ncez.pzh.gov.pl/seniorzy/zasady-zywienia-seniorow/ (accessed on 1 September 2022).
- Jayawardena, R.; Wickramawardhane, P.; Dalpatadu, C.; Hills, A.; Ranasinghe, P. Impact of an oral nutritional suplement on the boody composition of older adults with or at risk of malnutrition in an institutionalised setting: A randomised controlled trial. J. Hum. Nutr. Diet. 2024, 37, 1296–1307. [Google Scholar] [CrossRef]
- Okawa, Y. The impact of nutritional therapy on gastrointestional motility in older adults. Healthcare 2023, 11, 2829. [Google Scholar] [CrossRef]
- Choi, Y.J.; Ailshire, J.A.; Crimmins, E.M. Living alone, social networks in neighbourhoods, and daily fruit and vegetable consumption among middle-aged and older adults in the USA. Public Health Nutr. 2020, 23, 3315–3323. [Google Scholar] [CrossRef]
- Sakr-Ashour, F.A.; Wambogo, E.; Sahyoun, N.R. Social relationship, food insecurity, protei intake and hospitalization in homebound older adults: A PATH analysis. J. Nutr. Gerontol. Geriatr. 2022, 41, 201–216. [Google Scholar] [CrossRef]
- Govindaraju, T.; Sahle, B.W.; McCaffrey, T.A.; McNeil, J.J.; Owen, A.J. Dietary patterns and quality of life in older adults: A systematic review. Nutrients 2018, 10, 971. [Google Scholar] [CrossRef]
- Mohammadifard, N.; Talaei, M.; Sadeghi, M.; Oveisegharan, S.; Golshahi, J.; Esmaillzadeh, A. Dietary patterns and mortality from cardiovascular disease: Isfahan cohort study. Eur. J. Clin. Nutr. 2017, 71, 252–258. [Google Scholar] [CrossRef]
- Yu, D.; Zheng, W.; Cai, H.; Xiang, Y.B.; Li, H.; Gao, Y.T.; Shu, X.O. Long-term diet quality and risk of type 2 diabetes among urban Chinese adults. Diabetes Care 2018, 41, 723–730. [Google Scholar] [CrossRef]
- Rashidi Pour Fard, N.; Amirabdollahian, F.; Haghighatdoost, F. Dietary patterns and frailty: A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 498–513. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Xiao, Y.W.; Lai, X.X. The influence of lifestyle on the elderly with mild cognitive impairment in China. World Survey Res. 2020, 317, 50–57. [Google Scholar] [CrossRef]
- Hu, E.A.; Coresh, J.; Anderson, C.A.M.; Appel, L.J.; Grams, M.E.; Crews, D.C.; Mills, K.T.; He, J.; Scialla, J.; Rahman, M.; et al. Adherence to healthy dietary patterns and risk of CKD progression and all-cause mortality: Findings from the CRIC (chronic renal insufficiency cohort) study. Am. J. Kidney Dis. 2021, 77, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Knight, E.; Geetha, T.; Burnett, D.; Babu, J.R. The role of diet and dietary patterns in Parkinson’s disease. Nutrients 2022, 14, 4472. [Google Scholar] [CrossRef]
- Tang, L.; Yu, X.; Qiu, C.; Liu, F.; Zhu, X. Adherence to the planetary health diet is associated with slower cognitive decline: A prospective cohort analysis of Chinese older adults. Int. J. Behav. Nutr. Phys. Act. 2025, 21, 56. [Google Scholar] [CrossRef] [PubMed]
- Seifu, C.N.; Fahey, P.P.; Hailemariam, T.G.; Frost, S.A.; Atlantis, E. Dietary patterns associated with obesity outcomes in adults: An umbrella review of systematic reviews. Public Health Nutr. 2021, 24, 6390–6414. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, Y.; Zhang, Z. Trends in Population Dynamics: A Statistical Analysis. J. Popul. Res. 2021, 45, 123–187. [Google Scholar]
- Wang, Y.-L.; Wang, Y.-H.; Leung, D.K.Y.; Wong, G.H.Y.; Lum, T.Y.S. The effect of diet quality and body mass index on depression in older adults: A growth curve analysis. BMC Geriatr. 2024, 24, 834. [Google Scholar] [CrossRef]
- Coşkun, H.; Yildiz, I.; Alkan, Ö. Prevalence and predictors of psychological assistance services for older individuals in Turkish society. Front. Public Health 2023, 10, 1060845. [Google Scholar] [CrossRef]
- Güney, E.; Aydemir, A.F.; Iyit, N.; Alkan, Ö. Gender differences in psychological help-seeking attitudes: A case in Türkiye. Front. Psychol. 2024, 15, 1289435. [Google Scholar] [CrossRef]
- Mao, D.; Li, G.; Liang, M.; Wang, S.; Ren, X. Dietary patterns and multiple chronic deiseases in older adults. Nutr. Metab. 2024, 21, 36. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Bido, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines of definition and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Ahmed, T.; Haboubi, N. Assessment and management of nutrition in older people and its importance to health. Clin. Inter. Aging. 2010, 5, 207–216. [Google Scholar] [CrossRef]
- Bernstein, M.; Munoz, N. Position of the academy of nutrition and dietetics: Food and nutrition for older adults: Promoting health and wellness. J. Acad. Nutr. Diet. 2012, 112, 8. [Google Scholar] [CrossRef] [PubMed]
- Teodoro, M.A.; Silva, W.R.D.; Spexoto, M.C.B.; Silva Júnior, S.I.D. Factors of food choice and nutritional intake of Brazilian older adults according sociodemographic and health characteristics. Appetite 2024, 199, 107379. [Google Scholar] [CrossRef] [PubMed]
- Borkent, J.W.; Keller, H.; Wham, C.; Wijers, F.; de van der Schueren, M.A.E. Cross-country differences and similarities in undernutrition prevalence and risk as measured by SCREEN II in community-dwelling older adults. Healthcare 2020, 8, 151. [Google Scholar] [CrossRef] [PubMed]
- Eckert, C.; Gell, N.M.; Wingood, M.; Schollmeyer, J.; Tarleton, E.K. Malnutrition risk, rurality, and falls among community dwelling older adults. J. Nutr. Health Aging 2021, 25, 624–627. [Google Scholar] [CrossRef]
- Gajda, R.; Raczkowska, E.; Mazurkiewicz, D.; Suliga, E. Differentiation of nutritional risk among Polish seniors based on delected lifestyle characteristics. Nutrients 2022, 14, 607. [Google Scholar] [CrossRef]
- Gajda, R.; Raczkowska, E.; Wyka, J.; Suliga, E.; Sobaś, K. Differentiation of the nutritional risk of Polish elderly people according to selected demographic characteristics and declared socioeconomic status. Nutrients 2022, 14, 1582. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Choi, Y.J.; Crimmins, E.M.; Ailshire, J.A. Food insecurity, food envirinments, and disoarities in diet quality and obesity in nationally representative sample of community-dwelling older Americans. Prev. Med. Rep. 2022, 29, 101912. [Google Scholar] [CrossRef]
- KomPan®. Kwestionariusz do Badania Poglądów i Zwyczajów Żywieniowych Oraz Procedura Opracowania Danych, 2nd ed.; Komitet Nauki o Żywieniu Człowieka Polskiej Akademii Nauk: Warszawa, Poland, 2014; Available online: http://www.medprew.cm-uj.krakow.pl/doku/kwestionariusz_kompan2016.pdf (accessed on 7 September 2022).
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Kline, R. Principles and Practices of Structural Equation Modeling, 4th ed.; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Seigel, D.G.; Podgo, M.J.; Remaley, N.A. Acceptable Values of Kappa for Comparison of Two Groups. Am. J. Epidemiol. 1992, 135, 571–578. [Google Scholar] [CrossRef]
- Masson, L.F.; McNeill, G.; Tomany, J.O.; Simpson, J.A.; Peace, H.S.; Wei, L.; Grubb, D.A.; Bolton-Smith, C. Statistical approaches for assessing the relative validity of a food-18 frequency questionnaire: Use of correlation coefficients and the kappa statistic. Public Health Nutr. 2002, 6, 313–321. [Google Scholar] [CrossRef]
- Zieliński, A. Błąd klasyfikacji w badaniach epidemiologicznych. Przegl. Epidemiol. 2008, 62, 461–470. [Google Scholar]
- Rosseel, Y. Lavaan: An R package for structural equation modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Tarka, P. An overview of structural equation modeling: Its beginnings, historical development, usefulness and controversies in the social sciences. Qual. Quant. 2017, 52, 313–354. [Google Scholar] [CrossRef]
- Stanisz, A. Przystępny Kurs Statystyki, Tom. 3, Analizy Wielowymiarowe; StatSoft: Kraków, Poland, 2007; pp. 218, 449. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Fit Indices in Covariance Structure Modeling: Sensitivity to Underparameterized Model Misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Schumacker, R.E.; Lomax, R.G. A Beginner’s Guide to Structural Equation Modeling; Lawrence Erlbaum Associates Publishers: London, UK, 2004. [Google Scholar]
- Schreiber, J.B.; Stage, F.K.; King, J.; Nora, A.; Barlow, E.A. Reporting Structural Equation Modeling and Confirmatory Factor Analysis Results: A Review. J. Educ. Res. 2010, 99, 323–338. [Google Scholar] [CrossRef]
- Loehlin, J.C.; Beaujean, A.A. Latent Variable Models. An Introduction to Factors, Path, and Structural Equation Analysis, 5th ed.; Routledge: New York, NY, USA, 2017. [Google Scholar]
- Campbell, D.T.; Fiske, T.W. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol. Bull. 1959, 56, 81–105. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariances structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Marsh, H.W.; Hocevar, D. Application Of confirmatory factor analysis to the study of self-concept: First- and higher-order factor models and their invariance across groups. Psychol. Bull. 1985, 97, 562–582. [Google Scholar] [CrossRef]
- Holmes-Smith, P.; Coote, L.; Cunningham, E. Structural Equation Modeling: From the Fundamental to Advanced Topics; School Research, Evaluation and Measurement Services: Melbourne, Australia, 2006. [Google Scholar]
- Sabri, A.; Zulkurnain, N.N.A.; Khairushalimi, F.I. Assessing the Validity and Reliability of a Measurement Model in Structural Equation Modeling (SEM). J. Adv. Math. Comput. Sci. 2016, 15, 1–8. [Google Scholar] [CrossRef]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Mc Callum, R.C.; Roznowski, M.; Necowitz, L.B. Model modification in covariance structure analysis: The problem of capitalization on chance. Psychol. Bull. 1992, 111, 490–504. [Google Scholar] [CrossRef]
- Nazri, N.; Vanoh, D.; Leng, S. Malnutrition, low diet quality and its risk factors among older adults with low socio-economic status: A scoping review. Nutr. Res. Rev. 2021, 34, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Parker, E.A.; Perez, W.J.; Phipps, B.; Ryan, A.S.; Prior, S.J.; Katzel, L.; Serra, M.C.; Addison, O. Dietary Quality and Perceived Barriers to Weight Loss among Older Overweight Veterans with Dysmobility. Int. J. Environ. Res. Public Health 2022, 19, 9153. [Google Scholar] [CrossRef]
- Niedźwiedzka, E.; Wądołowska, L. Analiza urozmaicenia spożycia żywności w kontekście statusu socjo-ekonomicznego osób starszych. Probl. Hig. Epidemiol. 2010, 94, 576–584. [Google Scholar]
- Jaroch, A.; Górczewska-Siedlecka, E.; Jaroch, K.; Podhorecka, M. Usual food intake described by Food Intake Variety Questionnaire (FIVeQ) of elderly patients with frailty syndrome—Preliminary results. Gerontol. Pol. 2017, 25, 163–167. [Google Scholar]
- Allès, B.; Samieri, C.; Lorrain, S.; Jutand, M.-A.; Carmichael, P.-H.; Shatenstein, B.; Gaudreau, P.; Payette, H.; Laurin, D.; Barberger-Gateau, P. Nutrient patterns and their food sources in older persons from France and quebec: Dietary and lifestyle characteristics. Nutrients 2016, 8, 225. [Google Scholar] [CrossRef]
- Bamia, C.; Orfanos, P.; Ferrari, P.; Overvad, K.; Hundborg, H.H.; Tjønneland, A.; Olsen, A.; Kesse, E.; Boutron-Ruault, M.-C.; Clavel-Chapelon, F.; et al. Dietary patterns among older Europeans: The EPIC-Elderly study. Br. J. Nutr. 2005, 94, 100–113. [Google Scholar] [CrossRef]
- Morris, M.C.; Evans, D.A.; Tangney, C.C.; Bienias, J.L.; Wilson, R.S. Associations of vegetable and fruit consumption with age-related cognitive change. Neurology 2006, 67, 1370–1376. [Google Scholar] [CrossRef] [PubMed]
- Andreeva, V.A.; Allès, B.; Feron, G.; Gonzalez, R.; Sulmont-Rossé, C.; Galan, P.; Hercberg, S.; Méjean, C. Sex-specific sociodemographic correlates of dietary patterns in a large sample of French elderly individuals. Nutrients 2016, 8, 484. [Google Scholar] [CrossRef]
- Jang, K.; Baek, Y.M. How to effectively design public health interventions: Implications from the interaction effects between socioeconomic status and health locus of control beliefs on healthy dietary behaviours among US adults. Health Soc. Care Commun. 2018, 26, 664–674. [Google Scholar] [CrossRef]
- Bishop, N.J.; Zuniga, K.E.; Ramirez, C.M. Latent profile analysis of dietary intake in a community-dwelling sample of older Americans. Public Health Nutr. 2020, 23, 243–253. [Google Scholar] [CrossRef] [PubMed]
- Mumme, K.; Conlon, C.; von Hurst, P.; Jones, B.; Stonehouse, W.; Heath, A.-L.M.; Coad, J.; Haskell-Ramsay, C.; de Seymour, J.; Beck, K. Dietary patterns, their nutrients, and associations with socio-demographic and lifestyle factors in older New Zealand adults. Nutrients 2020, 12, 3425. [Google Scholar] [CrossRef] [PubMed]
- Conklin, A.I.; Forouhi, N.G.; Surtees, P.; Khaw, K.-T.; Wareham, N.J.; Monsivais, P. Social relationships and healthful dietary behaviour: Evidence from over-50s in the EPIC cohort, UK. Soc. Sci. Med. 2014, 100, 167–175. [Google Scholar] [CrossRef]
- Bloom, I.; Edwards, M.; Jameson, K.A.; Syddall, H.E.; Dennison, E.; Gale, C.R.; Baird, J.; Cooper, C.; Aihie Sayer, A.; Robinson, S. Influences on diet quality in older age: The importance of social factors. Age Ageing 2017, 46, 277–283. [Google Scholar] [CrossRef]
- Bloom, I.; Lawrence, W.; Barker, M.; Baird, J.; Dennison, E.; Sayer, A.A.; Cooper, C.; Robinson, S. What influences diet quality in older people? A qualitative study among community-dwelling older adults from the Hertfordshire Cohort Study, UK. Public Health Nutr. 2017, 20, 2685–2693. [Google Scholar] [CrossRef]
- Marcone, M.F.; Madan, P.; Grodzinski, B. An overview of the sociological and environmental factors influencing eating food behavior in Canada. Front. Nutr. 2020, 7, 77. [Google Scholar] [CrossRef]
- Hu, Y.; Xiao, J.; Li, X. The impact of living arrangements on dietary patterns among older adults: The mediating effects of loneliness and anxiety. Front. Public Health 2025, 13, 1519564. [Google Scholar] [CrossRef]
- Zhu, Y.; Duan, M.-J.; Riphagen, I.J.; Minovic, I.; Mierau, J.O.; Carrero, J.J.; Bakker, S.J.; Navis, G.J.; Dekker, L.H. Separate and combined effects of individual and neighbourhood socio-economic disadvantage on health-related lifestyle risk factors: A multilevel analysis. Int. J. Epidemiol. 2022, 50, 1959–1969. [Google Scholar] [CrossRef]
- Kim, C.-O. Food choice patterns among frail older adults: The associations between social network, food choice values and diet quality. Appetite 2016, 96, 116–121. [Google Scholar] [CrossRef]
- Urzędy centralne. Koniec Stanu Zagrożenia Epidemiologicznego. Available online: https://www.gov.pl/web/rpp/koniec-stanu-zagrozenia-epidemicznego (accessed on 30 May 2025).
- Lee, J.J.; Sultana, N.; Nishita, C. Participants assessment of a alternative flexible congregate nutrition meal program for older adults. J. Nutr. Gerontol. Geriatr. 2024, 43, 134–150. [Google Scholar] [CrossRef]
- Leroux, J.; Morrison, K.; Rosenberg, M. Prevalence and predictors of food insecurity among older people in Canada. Int. J. Environ. Res. Public Health 2018, 15, 2511. [Google Scholar] [CrossRef]
- Olejniczak, T. Uwarunkowania zmian zachowań zakupowych konsumentów seniorów. Stud. Ekon. 2018, 357, 207–216. [Google Scholar]
- Gutkowska, K.; Ozimek, I.; Górska-Warsewicz, H. Czynniki ekonomiczne warunkujące sposób żywienia populacji. In Żywienie Człowieka a Zdrowie Publiczne, 3rd ed.; Gawęcki, J., Roszkowski, W.F., Eds.; PWN: Warszawa, Poland, 2023; pp. 162–178. [Google Scholar]
- Mills, S.; Adams, J.; Wrieden, W.; White, M.; Brown, H. Sociodemographic characteristics and frequency of consuming home-cooked meals and meals from out-of-home sources: Cross-sectional analysis of a population-based cohort study. Public Health Nutr. 2018, 21, 2255–2266. [Google Scholar] [CrossRef]
- Ishida, A.; Ishida, E. Which Japanese older adults are least likely to enjoy favorable dietary practices. Int. J. Gerontol. 2019, 13, 330–334. [Google Scholar] [CrossRef]
- Kwan, Y.; Hong, K.H.; Park, Y.-K.; Kim, S. How does the frequency of eating-alone among older people in Korea affect their health and dietary behaviour. Nutrients 2023, 15, 2085. [Google Scholar] [CrossRef]
- Minagawa-Watanabe, Y.; Ukawa, S.; Fukumura, T.; Okabayashi, S.; Audo, M.; Wakai, K.; Tsushita, K.; Tamakoshi, A. The association of dining companionship with Energy and nutrient intake among community-dwelling Japanese older adults. Nutrients 2025, 17, 37. [Google Scholar] [CrossRef]
- Maynard, L.M.; Serdula, M.K.; Galuska, D.A.; Gillespie, C.; Mokdad, A.H. Secular trends in desired weight of adults. Int. J. Obes. 2006, 30, 1375–1381. [Google Scholar] [CrossRef]
- Langellier, B.A.; Glik, D.; Ortega, A.N.; Prelip, M.L. Trends in racial/ethnic disparities in overweight self-perception among US adults, 1988–1994 and 1999–2008. Public Health Nutr. 2015, 18, 2115–2125. [Google Scholar] [CrossRef][Green Version]
- Johnson, F.; Cooke, L.; Croker, H.; Wardle, J. Changing perceptions of weight in Great Britain: Comparison of two population surveys. BMJ 2008, 337, a494. [Google Scholar] [CrossRef]
- Johnson-Taylor, W.L.; Fisher, R.A.; Hubbard, V.S.; Starke-Reed, P.; Eggers, P.S. The change in weight perception of weight status among the overweight: Comparison of NHANES III (1988–1994) and 1999–2004 NHANES. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 9. [Google Scholar] [CrossRef]
- Burke, M.A.; Heiland, F.W.; Nadler, C.M. From “overweight” to “about right”: Evidence of a generational shift in body weight norms. Obesity 2010, 18, 1226–1234. [Google Scholar] [CrossRef]
- Sarah, E.J.; Lee, S.; Andrew, S. Weight perceptions in older adults: Findings from the English longitudinal study of ageing. BMJ Open 2020, 10, e033773. [Google Scholar] [CrossRef]
- Lee, K. Trends in prevalence of overweight and obesity, and weight loss efforts among older adults in South Korea, 2005–2021. Prev. Med. 2024, 180, 107854. [Google Scholar] [CrossRef]
- Joh, H.K.; Oh, J.; Lee, H.J.; Kawachi, I. Gender and socioeconomic status in relation to weight perception and weight control behavior in Korean adults. Obes. Facts 2013, 6, 17–27. [Google Scholar] [CrossRef]
- Fang, K.; Li, H.; Ma, A.; Dong, J.; Xie, J.; Zhou, Y.; Qi, K.; Wei, Y.; Li, G.; Cao, J.; et al. Weight underestimation for adults in Beijing and its association with chronic disease awareness and weight management. Lipids Health Dis. 2018, 17, 225. [Google Scholar] [CrossRef]
- Kim, S.; So, W.-Y. Secular trends in the prevalence of weight misperception among Korean adults, 2001–2013. Obes. Res. Clin. Pract. 2018, 12, 346–350. [Google Scholar] [CrossRef]
- Muttarak, R. Normalization of plus size and the danger of unseen overweight and obesity in England. Obesity 2018, 26, 1125–1129. [Google Scholar] [CrossRef]
- Smith, M.P. Self-estimated BMI, but not self-perceived body size, accurately identifies unhealthy weight in US adults. BMC Public Health 2021, 21, 253. [Google Scholar] [CrossRef]
- Yook, S.-J.; Jung, J.-G.; Ahn, S.-K.; Kim, J.-S.; Hong, J.-H. Non-linear relationship between body mass index and self-rated health in olser Korean adults: Body image and sex considerations. Epidemiol. Health 2023, 45, e2023061. [Google Scholar] [CrossRef]
- Dijkstra, T.K.; Henseler, J. Consistent and asymptotically normal PLS estimators for linear structural equations. Comput. Stat. Data Anal. 2015, 81, 10–23. [Google Scholar] [CrossRef]
- Jyrkkä, J.; Enlund, H.; Lavikainen, P.; Sulkava, R.; Hartikainen, S. Association of polypharmacy with nutritional status, functional ability and cognitive capacity over a three-year period in an elderly population. Pharmacoepidemiol. Drug Saf. 2011, 20, 514–522. [Google Scholar] [CrossRef]
- Phillips, M.B.; Foley, A.L.; Barnard, R.; Isenring, E.A.; Miller, M.D. Nutritional screening in community-dwelling older adults: A systematic literature review. Asia Pac. J. Clin. Nutr. 2010, 19, 440–449. [Google Scholar]
| Place of Study | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wrocław City | Świdnica District | Wrocław District | Trzebnica District | Sieradz District | |||||||
| Senior organisations participating in the study in each place | |||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| Number of people participating in each place | |||||||||||
| 36 | 31 | 31 | 30 | 28 | 27 | 34 | 30 | 18 | 14 | 13 | 10 |
| Number of people excluded from the study in each place | |||||||||||
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Final number of people in the study (N = 301) | |||||||||||
| Variables | N | % | |
|---|---|---|---|
| Total | 301 | 100.0 | |
| Gender | women | 241 | 80.1 |
| men | 60 | 19.9 | |
| Age (in years) | 60–74 | 219 | 72.8 |
| 75 and over | 82 | 27.2 | |
| Place of residence | village | 60 | 19.9 |
| city < 100,000 inhabitants | 58 | 19.3 | |
| city > 100,000 inhabitants | 183 | 60.8 | |
| Region of residence | City of Wrocław | 183 | 60.8 |
| Świdnica district | 64 | 21.2 | |
| Wrocław district | 32 | 10.6 | |
| Trzebnica district | 12 | 4.0 | |
| Sieradz district | 10 | 3.4 | |
| Education | primary | 27 | 9.0 |
| basic vocational | 49 | 16.3 | |
| secondary | 152 | 50.5 | |
| higher | 73 | 24.2 | |
| Financial situation | below average | 26 | 8.6 |
| average | 241 | 80.1 | |
| above average | 34 | 11.3 | |
| Financial assistance from family | There is no need | 245 | 81.4 |
| No, despite financial problems | 22 | 7.3 | |
| Yes, due to financial problems | 13 | 4.3 | |
| Yes, despite no financial problems | 21 | 7.0 | |
| Social financial assistance | There is no need | 259 | 86.0 |
| No, despite financial problems | 33 | 11.0 | |
| Yes, due to financial problems | 3 | 1.0 | |
| Yes, despite no financial problems | 6 | 2.0 | |
| Factors (F) | Item Number * | Content of Test Items |
|---|---|---|
| Unhealthy eating (F1) | 13 | I usually limit or omit healthy foods from my meals |
| 14 | Usually my meals have little variety (I usually eat the same thing every day) | |
| 15 | Usually my meals are not healthy (e.g., I eat fast food). | |
| 24 | I eat raw vegetables and fruits less than twice a day | |
| 25 | Any vegetables or fruits I eat less than twice during the day (e.g., raw, cooked, pickled) | |
| 49 | Prepared store-bought foods (refrigerated or frozen, e.g., soups, dumplings, croquettes, potato noodles, dumplings, etc., which can be quickly cooked or reheated in the microwave) I eat every day | |
| 50 | I eat powdered soups or canned or jarred foods, etc., every day | |
| 76 | I have trouble choosing healthy foods when shopping | |
| Irregularities related to meals (F2) | 7 | I eat three or fewer meals a day |
| 8 | I eat six or more meals a day | |
| 9 | Breaks between my meals are less than two hours | |
| 10 | Breaks between my meals are longer than four hours | |
| Perception of body weight (F3) | 3 | I would like to increase my body weight |
| 4 | I would like to reduce my body weight | |
| 5 | I think my body weight is too high | |
| 6 | I think my body weight is too low |
| Measures of Fit * | Factor Model |
|---|---|
| χ2/df | 3.34 |
| CFI | 0.93 |
| TLI | 0.92 |
| IFI | 0.93 |
| RMSEA | 0.06 |
| SRMR | 0.09 |
| GFI | 0.95 |
| AGFI | 0.94 |
| Factors (F) | Influence Direction | Item Number | Factor Model |
|---|---|---|---|
| Unhealthy eating (F1) | → | 13 | 0.36 * |
| 14 | 0.32 | ||
| 15 | 0.23 | ||
| 24 | 0.43 | ||
| 25 | 0.31 | ||
| 49 | 0.24 | ||
| 50 | 0.25 | ||
| 76 | 0.24 | ||
| Irregularities related to meals (F2) | → | 7 | 0.55 |
| 8 | 0.52 | ||
| 9 | 0.26 | ||
| 10 | 0.40 | ||
| Perception of body weight (F3) | → | 3 | 0.28 |
| 4 | 0.37 | ||
| 5 | 0.69 | ||
| 6 | 0.73 |
| Factors (F) | Factor Model | ||
|---|---|---|---|
| α | CR | AVE | |
| Unhealthy eating (F1) | 0.77 | 0.77 | 0.30 |
| Irregularities related to meals (F2) | 0.75 | 0.75 | 0.43 |
| Perception of body weight (F3) | 0.79 | 0.80 | 0.52 |
| Factors (F) | Factor Model | ||
|---|---|---|---|
| Unhealthy Eating (F1) | Irregularities Related to Meals (F2) | Perception of Body Weight (F3) | |
| Unhealthy eating (F1) | 1.00 * | 0.16 | 0.14 |
| Irregularities related to meals (F2) | 0.16 | 1.00 | 0.06 |
| Perception of body weight (F3) | 0.14 | 0.06 | 1.00 |
| Variables | Response Categories | Total | Nutritional Risk Factors | |||||
|---|---|---|---|---|---|---|---|---|
| F1 | F2 | F3 | ||||||
| Intensity | ||||||||
| Low (N = 149) | High (N = 152) | Low (N = 149) | High (N = 152) | Low (N = 178) | High (N = 123) | |||
| Gender | woman | 80.1 (241) | 88.6 (132) | 71.7 (109) | 82.6 (123) | 77.6 (118) | 69.7 (124) | 95.1 (117) |
| men | 19.9 (60) | 11.4 (17) | 24.3 (43) | 17.4 (26) | 22.4 (34) | 30.3 (54) | 4.9 (6) | |
| p-value (chi2 test) | p = 0.015 | p = 0.736 | p < 0.001 | |||||
| Education | primary | 9.0 (27) | 6.1 (9) | 11.8 (18) | 8.1 (12) | 9.9 (15) | 12.5 (22) | 4.6 (5) |
| basic vocational | 16.3 (49) | 14.1 (21) | 18.4 (28) | 15.3 (23) | 17.1 (26) | 24.7 (44) | 4.1 (5) | |
| secondary | 50.4 (152) | 48.3 (72) | 52.6 (80) | 49.2 (75) | 50.6 (77) | 49.4 (88) | 52.0 (64) | |
| higher | 24.3 (73) | 31.5 (47) | 17.1 (26) | 25.4 (38) | 23.4 (35) | 13.4 (24) | 39.3 (49) | |
| p-value (chi2 test) | p < 0.001 | p = 0.844 | p < 0.001 | |||||
| Social activity 1 | often | 33.6 (101) | 30.9 (46) | 36.2 (55) | 16.1(24) | 50.7 (77) | 27.5(49) | 42.3 (52) |
| sometimes | 38.2 (115) | 38.3 (57) | 38.1 (58) | 35.6 (53) | 40.8 (62) | 34.3 (61) | 43.9 (54) | |
| never | 28.2 (85) | 26.8 (40) | 29.7 (45) | 48.3 (72) | 8.5 (13) | 38.2 (68) | 13.8 (17) | |
| p-value (chi2 test) | p = 0.549 | p < 0.001 | p = 0.049 | |||||
| Family relations 2 | very good | 46.2 (139) | 52.3 (78) | 40.1 (61) | 49.0 (73) | 43.4 (66) | 50.6 (90) | 39.8 (49) |
| good | 39.2 (118) | 42.9 (64) | 35.5 (54) | 43.6 (65) | 34.7 (53) | 38.2 (68) | 40.6 (50) | |
| average or worse | 14.6 (44) | 4.7 (7) | 24.3 (37) | 7.4 (11) | 21.7 (33) | 11.2 (20) | 19.5 (24) | |
| p-value (chi2 test) | p = 0.039 | p = 0.043 | p = 0.009 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gajda, R.; Jeżewska-Zychowicz, M.; Rak, K.; Maćków, M. Nutritional Risk Factors Model of Community-Dwelling Older People in Poland–Pilot Study. Nutrients 2025, 17, 2150. https://doi.org/10.3390/nu17132150
Gajda R, Jeżewska-Zychowicz M, Rak K, Maćków M. Nutritional Risk Factors Model of Community-Dwelling Older People in Poland–Pilot Study. Nutrients. 2025; 17(13):2150. https://doi.org/10.3390/nu17132150
Chicago/Turabian StyleGajda, Robert, Marzena Jeżewska-Zychowicz, Karolina Rak, and Monika Maćków. 2025. "Nutritional Risk Factors Model of Community-Dwelling Older People in Poland–Pilot Study" Nutrients 17, no. 13: 2150. https://doi.org/10.3390/nu17132150
APA StyleGajda, R., Jeżewska-Zychowicz, M., Rak, K., & Maćków, M. (2025). Nutritional Risk Factors Model of Community-Dwelling Older People in Poland–Pilot Study. Nutrients, 17(13), 2150. https://doi.org/10.3390/nu17132150








