Relationship of Composite Dietary Antioxidant Index vs. Alcohol Consumption with Mild Cognitive Impairment in the Elderly
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
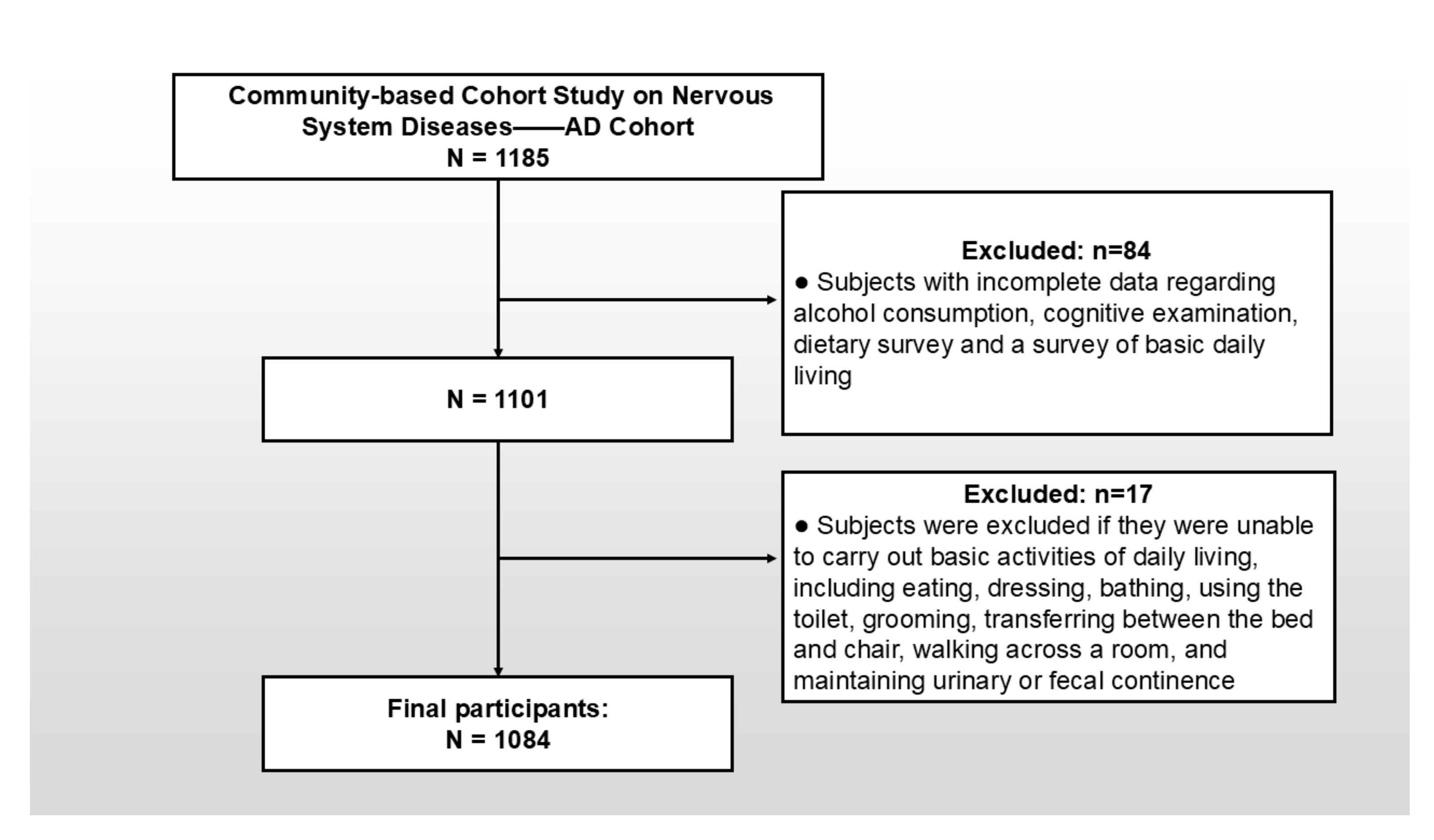
2.2. Study Population and Sampling Method
2.3. Data Collection
2.4. Assessment of Cognitive Function
2.5. Assessment of Composite Dietary Antioxidant Index and Energy
2.6. Assessment of Alcohol Consumption and Other Covariates
2.7. Statistical Analyses
3. Results
3.1. Basic Information
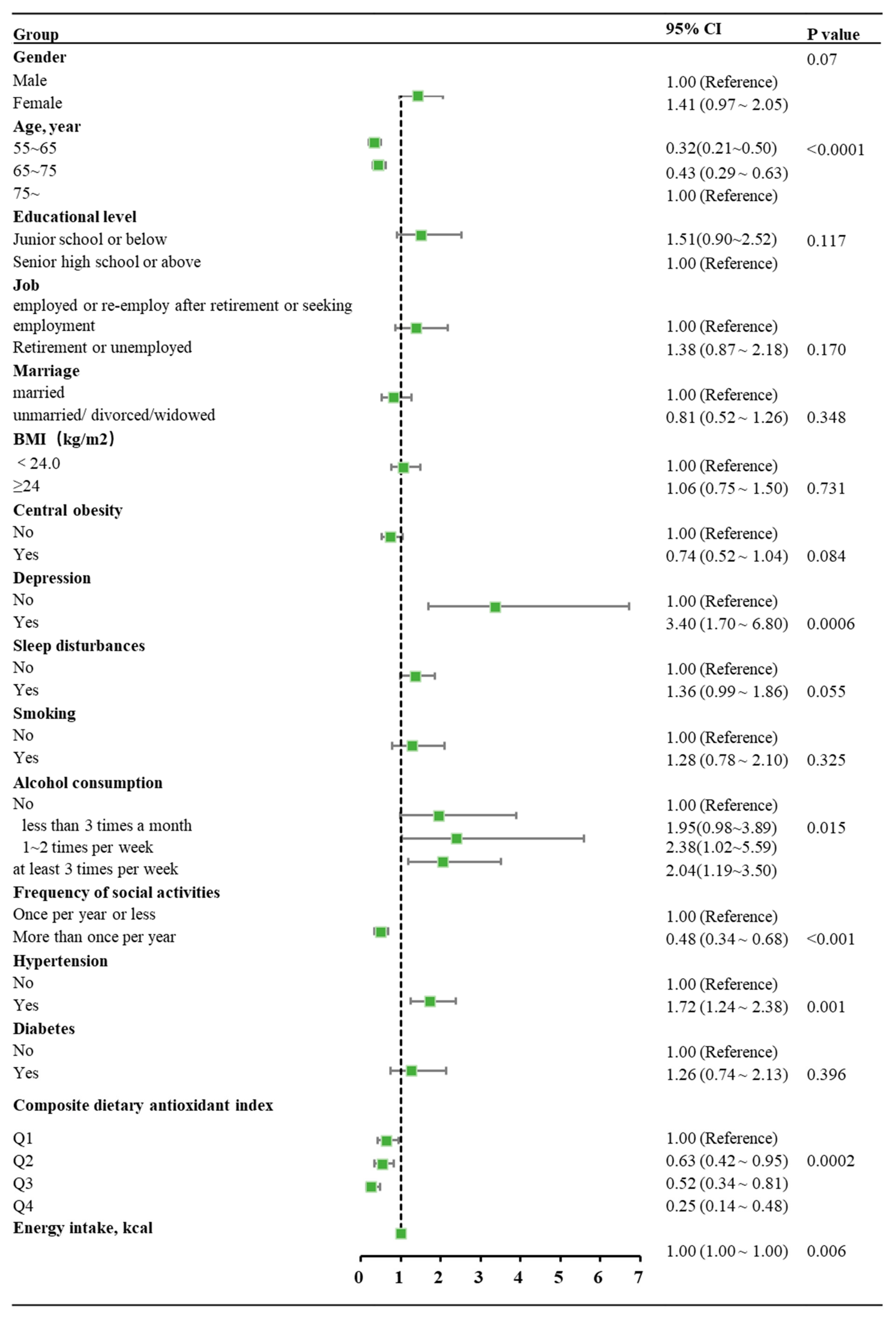
3.2. Analysis of the Association Between Composite Dietary Antioxidant Index and MCI
3.3. Analysis of the Association Between Alcohol Consumption and MCI
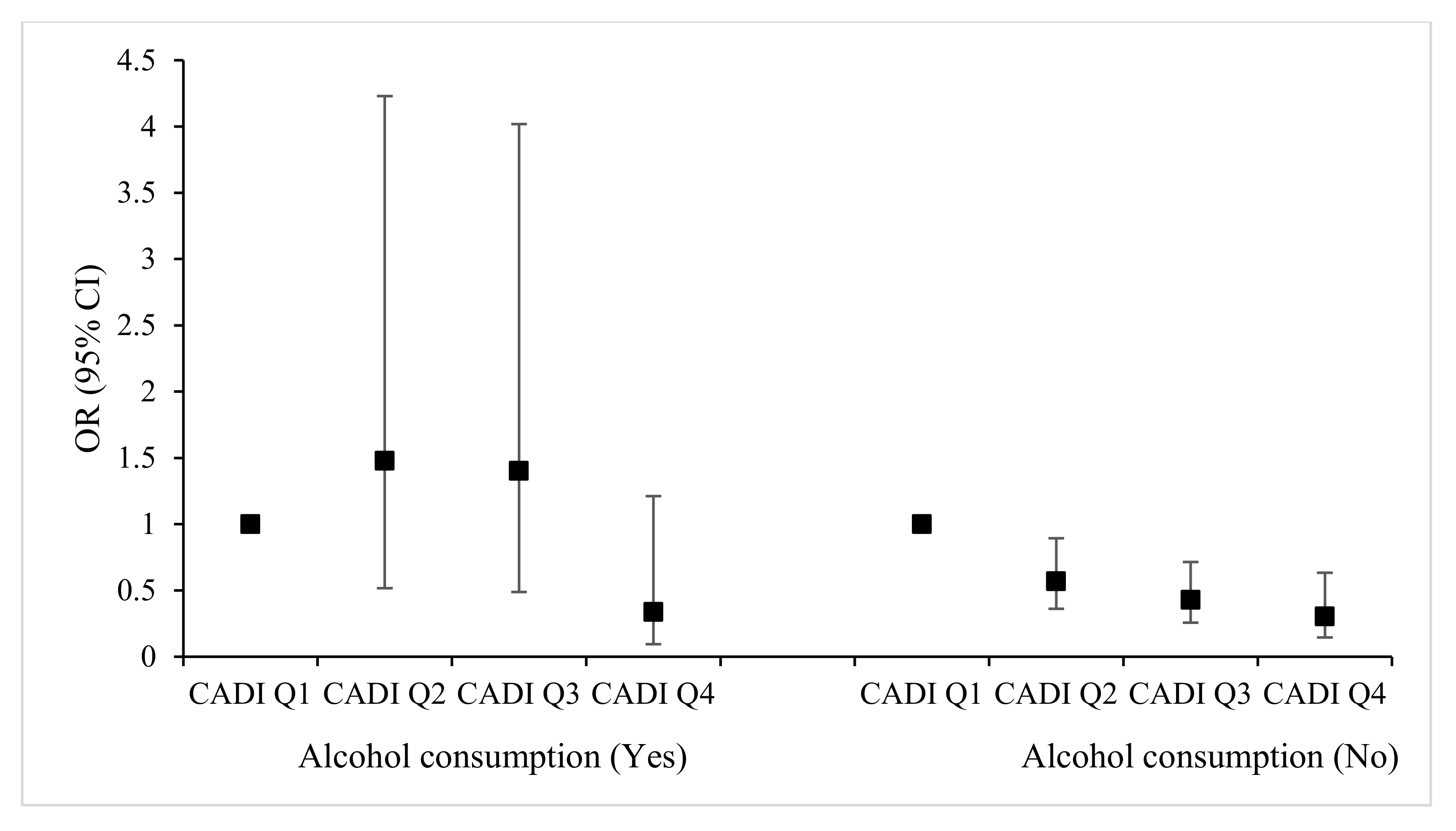
3.4. Interactive Effect of CDAI and Alcohol Consumption on MCI
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AD | Alzheimer’s disease |
| BMI | Body Mass Index |
| CDAI | Composite dietary antioxidant index |
| CI | Confidence interval |
| DRIs | Dietary Reference Intakes |
| FCTs | Converted FFQ Food Composition Tables |
| FFQ | Food Frequency Questionnaire |
| GDS | Geriatric Depression Scale |
| MCI | Mild cognitive impairment |
| MOCA | Montreal Cognitive Assessment |
| MMSE | Mini-Mental State Examination |
| OR | Odds Ratio |
| PSQI | Pittsburgh Sleep Quality Index |
| RNI | Recommended Nutrient Intake |
| WFCT | Weighted Food Composition Table method |
| WHO | World Health Organization |
| 24HRs | 24 h dietary recall |
References
- United Nations. World Population Prospects 2024; United Nations: New York, NY, USA, 2024. [Google Scholar]
- National Bureau of Statistics of China. Statistical Bulletin of the People’s Republic of China on National Economic and Social Development; National Bureau of Statistics of China: Beijing, China, 2024. [Google Scholar]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Dementia; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Cao, Y.; Yu, F.; Lyu, Y.; Lu, X. Promising candidates from drug clinical trials: Implications for clinical treatment of Alzheimer’s disease in China. Front. Neurol. 2022, 13, 1034243. [Google Scholar] [CrossRef]
- Gifford, K.A.; Liu, D.; Romano, R.R.; Jones, R.N.; Jefferson, A.L. Development of a subjective cognitive decline questionnaire using item response theory: A pilot study. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2015, 1, 429–439. [Google Scholar] [CrossRef] [PubMed]
- Petersen, R.C.; Roberts, R.O.; Knopman, D.S.; Boeve, B.F.; Geda, Y.E.; Ivnik, R.J.; Smith, G.E.; Jack, C.R.J. Mild cognitive impairment: Ten years later. Arch. Neurol. 2009, 66, 1447–1455. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.; Liu, X.; Yin, Q.; Zhu, W.; Zhang, R.; Fan, X. Alcohol consumption and transition of mild cognitive impairment to dementia. Psychiatry Clin. Neurosci. 2009, 63, 43–49. [Google Scholar] [CrossRef]
- Cui, Y.; Si, W.; Zhu, C.; Zhao, Q. Alcohol Consumption and Mild Cognitive Impairment: A Mendelian Randomization Study from Rural China. Nutrients 2022, 14, 3596. [Google Scholar] [CrossRef]
- Lao, Y.; Hou, L.; Li, J.; Hui, X.; Yan, P.; Yang, K. Association between alcohol intake, mild cognitive impairment and progression to dementia: A dose–response meta-analysis. Aging Clin. Exp. Res. 2021, 33, 1175–1185. [Google Scholar] [CrossRef]
- Koch, M.; Fitzpatrick, A.L.; Rapp, S.R.; Nahin, R.L.; Williamson, J.D.; Lopez, O.L.; DeKosky, S.T.; Kuller, L.H.; Mackey, R.H.; Mukamal, K.J.; et al. Alcohol Consumption and Risk of Dementia and Cognitive Decline Among Older Adults With or Without Mild Cognitive Impairment. JAMA Netw. Open 2019, 2, e1910319. [Google Scholar] [CrossRef]
- Nallapu, B.T.; Petersen, K.K.; Lipton, R.B.; Grober, E.; Sperling, R.A.; Ezzati, A. Association of Alcohol Consumption with Cognition in Older Population: The A4 Study. J. Alzheimer’s Dis. 2023, 93, 1381–1393. [Google Scholar] [CrossRef]
- Kim, J.W.; Lee, D.Y.; Lee, B.C.; Jung, M.H.; Kim, H.; Choi, Y.S.; Choi, I. Alcohol and Cognition in the Elderly: A Review. Psychiatry Investig. 2012, 9, 8. [Google Scholar] [CrossRef]
- Etgen, T.; Sander, D.; Bickel, H.; Förstl, H. Mild Cognitive Impairment and Dementia. Dtsch. Arztebl. Int. 2011, 44, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, E.; Lamport, D.; Brennan, L.; Burnet, P.; Calabrese, V.; Cunnane, S.C.; de Wilde, M.C.; Dye, L.; Farrimond, J.A.; Emerson Lombardo, N.; et al. Nutrition and the ageing brain: Moving towards clinical applications. Ageing Res. Rev. 2020, 62, 101079. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Tang, W.; Li, H.; Lv, J.; Chang, L.; Chen, S. Composite dietary antioxidant index negatively correlates with osteoporosis among middle-aged and older US populations. Am. J. Transl. Res. 2023, 15, 1300–1308. [Google Scholar]
- Wright, M.E.; Mayne, S.T.; Stolzenberg-Solomon, R.Z.; Li, Z.; Pietinen, P.; Taylor, P.R.; Virtamo, J.; Albanes, D. Development of a comprehensive dietary antioxidant index and application to lung cancer risk in a cohort of male smokers. Am. J. Epidemiol. 2004, 160, 68–76. [Google Scholar] [CrossRef]
- Wang, R.; Tao, W.; Cheng, X. Association of composite dietary antioxidant index with cardiovascular disease in adults: Results from 2011 to 2020 NHANES. Front. Cardiovasc. Med. 2024, 11, 1379871. [Google Scholar] [CrossRef]
- Zhao, S.; Su, Y.; Yang, H. Associations of dietary inflammation index and composite dietary antioxidant index with all-cause mortality in COPD patients. Front. Nutr. 2025, 12, 1514430. [Google Scholar] [CrossRef]
- Huang, Q.; Jia, X.; Zhang, J.; Huang, F.; Wang, H.; Zhang, B.; Wang, L.; Jiang, H.; Wang, Z. Diet–Cognition Associations Differ in Mild Cognitive Impairment Subtypes. Nutrients 2021, 13, 1341. [Google Scholar] [CrossRef]
- He, M.; Su, D.; Zhang, R.; Xu, P.; Han, D.; Huang, L.; Zou, Y. Sex Disparity in the Nutrition-Related Determinants of Mild Cognitive Impairment: A Case–Control Study. Nutrients 2025, 17, 248. [Google Scholar] [CrossRef]
- Jia, X.; Wang, Z.; Huang, F.; Su, C.; Du, W.; Jiang, H.; Wang, H.; Wang, J.; Wang, F.; Su, W.; et al. A comparison of the Mini-Mental State Examination (MMSE) with the Montreal Cognitive Assessment (MoCA) for mild cognitive impairment screening in Chinese middle-aged and older population: A cross-sectional study. BMC Psychiatry 2021, 21, 485. [Google Scholar] [CrossRef]
- Lu, J.; Li, D.; Li, F.; Zhou, A.; Wang, F.; Zuo, X.; Jia, X.; Song, H.; Jia, J. Montreal Cognitive Assessment in Detecting Cognitive Impairment in Chinese Elderly Individuals: A Population-Based Study. J. Geriatr. Psychiatry. Neurol. 2011, 24, 184–190. [Google Scholar] [CrossRef]
- Winblad, B.; Palmer, K.; Kivipelto, M.; Jelic, V.; Fratiglioni, L.; Wahlund, L.O.; Nordberg, A.; Bäckman, L.; Albert, M.; Almkvist, O.; et al. Mild cognitive impairment–beyond controversies, towards a consensus: Report of the International Working Group on Mild Cognitive Impairment. J. Intern. Med. 2004, 256, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Julayanont, P.; Brousseau, M.; Chertkow, H.; Phillips, N.; Nasreddine, Z.S. Montreal Cognitive Assessment Memory Index Score (MoCA-MIS) as a Predictor of Conversion from Mild Cognitive Impairment to Alzheimer’s Disease. J. Am. Geriatr. Soc. 2014, 62, 679–684. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Zou, Y.; Huang, L.; Zhao, D.; Han, D.; Su, D.; Zhang, R. The Nutritional Status of Vitamin D and Its Influencing Factors among Adults in Zhejiang Province in 2018. J. Hyg. Res. 2022, 51, 844–848. [Google Scholar]
- Zhao, D.; Gong, Y.; Huang, L.; Lv, R.; Gu, Y.; Ni, C.; Zhu, D.; Yang, M.; Rong, S.; Zhang, R.; et al. Validity of food and nutrient intakes assessed by a food frequency questionnaire among Chinese adults. Nutr. J. 2024, 23, 23. [Google Scholar] [CrossRef]
- Yang, Y. China Food Composition Tables Standard Edition; Peking University Medical Press: Beijing, China, 2019. [Google Scholar]
- Huang, F.; Wang, H.; Wang, Z.; Zhang, J.; Du, W.; Jia, X.; Wang, L.; Zhang, B. Is geriatric depression scale a valid instrument to screen depression in Chinese community-dwelling elderly? BMC Geriatr. 2021, 21, 310. [Google Scholar] [CrossRef]
- Chen, C. Guidelines for the Prevention and Control of Overweight and Obesity in Chinese Adults; People’s Medical Publishing House: Beijing, China, 2006. [Google Scholar]
- National Health and Family Planning Commission of the People’s Republic of China. Adult Weight Assessment WS/T 428-2013; Standards Press of China: Beijing, China, 2013. [Google Scholar]
- Liu, X.; Tang, M.; Hu, L.; Wang, A.; Wu, H.; Zhao, G.; Gao, C.; Li, W. Reliability and validity of the Pittsburgh sleep quality index. Chin. J. Psychiatry 1996, 29, 103–107. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.R.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Weinstein, A.; Sesso, H.; Lee, I.; Cook, N.; Manson, J.; Buring, J.; Gaziano, J. Relationship of physical activity vs body mass index with type 2 diabetes in women. JAMA 2004, 292, 1188–1194. [Google Scholar] [CrossRef]
- Luo, L.; Li, H.; Luo, J. Detection of cognitive impairment and its relationship with physical activity levels in Chinese elderly: A cross-sectional analysis based on data from the 2018 China Health and Retirement Longitudinal Study. J. Math. Med. 2025, 38, 90–97. [Google Scholar]
- Zhao, C.; Pu, M.; Wu, C.; Ding, J.; Guo, J.; Zhang, G. Association between composite dietary antioxidant index and cognitive function impairment among the US older adults: A cross-sectional study based on the NHANES 2011–2014. Front. Nutr. 2024, 11, 1471981. [Google Scholar] [CrossRef]
- Mao, J.; Hu, H.; Zhao, Y.; Zhou, M.; Yang, X. Association Between Composite Dietary Antioxidant Index and Cognitive Function Among Aging Americans from NHANES 2011–2014. J. Alzheimer’s Dis. 2024, 98, 1377–1389. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Chen, J.; Liu, P.; Huang, Y. The role of composite dietary antioxidants in elderly cognitive function: Insights from NHANES. Front. Nutr. 2024, 11, 1455975. [Google Scholar] [CrossRef] [PubMed]
- Tsermpini, E.E.; Ilješ, A.P.; Dolžan, V. Alcohol-Induced Oxidative Stress and the Role of Antioxidants in Alcohol Use Disorder: A Systematic Review. Antioxidants 2022, 11, 1374. [Google Scholar] [CrossRef] [PubMed]
- Mann, R.E.; Vogel-Sprott, M.; Genest, M. Alcohol and cognition; some preliminary observations. J. Stud. Alcohol 1983, 44, 900–905. [Google Scholar] [CrossRef]
- Kryscio, R.J.; Abner, E.L.; Caban-Holt, A.; Lovell, M.; Goodman, P.; Darke, A.K.; Yee, M.; Crowley, J.; Schmitt, F.A. Association of Antioxidant Supplement Use and Dementia in the Prevention of Alzheimer’s Disease by Vitamin E and Selenium Trial (PREADViSE). JAMA Neurol. 2017, 74, 567–573. [Google Scholar] [CrossRef]
- Sharma, Y.; Popescu, A.; Horwood, C.; Hakendorf, P.; Thompson, C. Relationship between Vitamin C Deficiency and Cognitive Impairment in Older Hospitalised Patients: A Cross-Sectional Study. Antioxidants 2022, 11, 463. [Google Scholar] [CrossRef]
- Goveas, J.S.; Espeland, M.A.; Woods, N.F.; Wassertheil-Smoller, S.; Kotchen, J.M. Depressive symptoms and incidence of mild cognitive impairment and probable dementia in elderly women: The Women’s Health Initiative Memory Study. J. Am. Geriatr. Soc. 2011, 59, 57–66. [Google Scholar] [CrossRef]
- Chen, Y.; Grodstein, F.; Capuano, A.W.; Wang, T.; Bennett, D.A.; James, B.D. Late-life social activity and subsequent risk of dementia and mild cognitive impairment. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2025, 21, e14316. [Google Scholar] [CrossRef]
- Sachdev, P.S.; Lipnicki, D.M.; Crawford, J.; Reppermund, S.; Kochan, N.A.; Trollor, J.N.; Draper, B.; Slavin, M.J.; Kang, K.; Lux, O.; et al. Risk profiles for mild cognitive impairment vary by age and sex: The Sydney Memory and Ageing study. Am. J. Geriatr. Psychiatr. 2012, 20, 854–865. [Google Scholar] [CrossRef]
- Song, M.; Wang, Y.; Wang, R.; Xu, S.; Yu, L.; Wang, L.; Zhao, X.; Wang, X. Prevalence and risks of mild cognitive impairment of Chinese community-dwelling women aged above 60 years: A cross-sectional study. Arch. Womens Ment. Health 2021, 24, 903–911. [Google Scholar] [CrossRef]
- Wei, C.; Zhao, J.; Hu, R.; Wei, X. Association between depressive status and mild cognitive impairment in middle-aged and elderly Chinese adults from CHARLS study. Front. Psychiatry 2025, 16, 1516341. [Google Scholar] [CrossRef] [PubMed]
- Shajahan, S.; Peters, R.; Carcel, C.; Woodward, M.; Harris, K.; Anderson, C.S. Hypertension and Mild Cognitive Impairment: State-of-the-Art Review. Am. J. Hypertens. 2024, 37, 385–393. [Google Scholar] [CrossRef]
- Bao, Y.; Han, Y.; Ma, J.; Wang, R.; Le, S.; Wang, T.; He, J.; Yue, J.; Shi, J.; Tang, X.; et al. Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: Meta-analysis and systematic review. Neurosci. Biobehav. Rev. 2017, 75, 257–273. [Google Scholar] [CrossRef] [PubMed]
- Zafar, J.; Malik, N.I.; Atta, M.; Makhdoom, I.F.; Ullah, I.; Manzar, M.D. Loneliness may mediate the relationship between depression and the quality of life among elderly with mild cognitive impairment. Psychogeriatrics 2021, 21, 805–812. [Google Scholar] [CrossRef]
- Aiken-Morgan, A.T.; Capuano, A.W.; Wilson, R.S.; Barnes, L.L. Changes in Body Mass Index and Incident Mild Cognitive Impairment Among African American Older Adults. J. Gerontol. 2024, 79, glad263. [Google Scholar] [CrossRef]
- Qiu, T.; Zeng, Q.; Luo, X.; Xu, T.; Shen, Z.; Xu, X.; Wang, C.; Li, K.; Huang, P.; Li, X.; et al. Effects of Cigarette Smoking on Resting-State Functional Connectivity of the Nucleus Basalis of Meynert in Mild Cognitive Impairment. Front. Aging Neurosci. 2021, 13, 755630. [Google Scholar] [CrossRef]
| Variables | Total, n | MCI, n (%) | Normal, n (%) | χ2 | p | |
|---|---|---|---|---|---|---|
| Total | 1084 | 267 (24.6) | 817 (75.4) | |||
| Composite dietary antioxidant index | 8.96 | 0.030 | ||||
| Q1 | 311 (28.7) | 91 (34.1) | 220 (26.9) | |||
| Q2 | 279 (25.7) | 74 (27.7) | 205 (25.1) | |||
| Q3 | 258 (23.8) | 57 (21.4) | 201 (24.6) | |||
| Q4 | 236 (21.8) | 45 (16.9) | 191 (23.4) | |||
| Alcohol consumption | 12.40 | 0.006 | ||||
| No | 874 (80.6) | 197 (73.8) | 677 (82.9) | |||
| Less than 3 times a month | 59 (5.4) | 17 (6.4) | 42 (5.1) | |||
| 1~2 times per week | 34 (3.1) | 14 (5.2) | 20 (2.5) | |||
| At least 3 times per week | 117 (10.8) | 39 (14.6) | 78 (9.6) | |||
| Region | 3.13 | 0.077 | ||||
| Urban | 554 (51.1) | 149 (55.8) | 405 (49.6) | |||
| Rural | 530 (48.9) | 118 (44.2) | 412 (50.4) | |||
| Gender | 0.01 | 0.932 | ||||
| Male | 514 (47.4) | 126 (47.2) | 388 (47.5) | |||
| Female | 570 (52.6) | 141 (52.8) | 429 (52.5) | |||
| Age, year | 43.57 | <0.001 | ||||
| 55~65 | 372 (34.3) | 63 (23.6) | 309 (37.8) | |||
| 65~75 | 479 (44.2) | 110 (41.2) | 369 (45.2) | |||
| 75~ | 233 (21.5) | 94 (35.2) | 139 (17.0) | |||
| Educational level | 4.6 | 0.032 | ||||
| Junior school or below | 927 (86.5) | 236 (90.4) | 691 (85.2) | |||
| Senior high school or above | 145 (13.5) | 25 (9.6) | 120 (14.8) | |||
| Occupation | 0.14 | 0.710 | ||||
| Employed or re-employed after retirement or seeking employment | 166 (15.3) | 39 (14.6) | 127 (15.5) | |||
| Retired or unemployed | 918 (84.7) | 228 (85.4) | 690 (84.5) | |||
| Marriage | 1.11 | 0.293 | ||||
| Married | 919 (84.8) | 221 (82.8) | 698 (85.4) | |||
| Unmarried/divorced/widowed | 165 (15.2) | 46 (17.2) | 119 (14.6) | |||
| BMI (kg/m2) | 0.46 | 0.498 | ||||
| <24.0 | 614 (56.6) | 156 (58.4) | 458 (56.1) | |||
| ≥24 | 470 (43.4) | 111 (41.6) | 359 (43.9) | |||
| Central obesity | 1.04 | 0.308 | ||||
| No | 582 (55.0) | 150 (57.7) | 432 (54.1) | |||
| Yes | 477 (45.0) | 110 (42.3) | 367 (45.9) | |||
| Frequency of social activities | 24.04 | <0.001 | ||||
| Once per year or less | 275 (25.4) | 98 (36.7) | 177 (21.7) | |||
| More than once per year | 809 (74.6) | 169 (63.3) | 640 (78.3) | |||
| Depression | 20.09 | <0.001 | ||||
| No | 1041 (96.0) | 244 (91.4) | 797 (97.6) | |||
| Yes | 43 (4.0) | 23 (8.6) | 20 (2.5) | |||
| Sleep disturbances | 6.10 | 0.014 | ||||
| No | 585 (54.1) | 126 (47.6) | 459 (56.3) | |||
| Yes | 496 (45.9) | 139 (52.5) | 357 (43.8) | |||
| Smoking | 2.58 | 0.108 | ||||
| No | 882 (81.5) | 208 (78.2) | 674 (82.6) | |||
| Yes | 200 (18.5) | 58 (21.8) | 142 (17.4) | |||
| Hypertension | 15.58 | <0.001 | ||||
| No | 499 (46.0) | 95 (35.6) | 404 (49.5) | |||
| Yes | 585 (54.0) | 172 (64.4) | 413 (50.6) | |||
| Diabetes | 2.71 | 0.100 | ||||
| No | 988 (91.6) | 238 (89.1) | 750 (92.4) | |||
| Yes | 91 (8.4) | 29 (10.9) | 62 (7.6) | |||
| Energy intake, kcal * | 1517.5 ± 1282.4 | 1528.8 ± 1495 | 1513.8 ± 1205.8 | −0.15 | 0.882 | |
| Variables | CADI (Q1) | CADI (Q2) | CADI (Q3) | CADI (Q4) | |
|---|---|---|---|---|---|
| Alcohol consumption | No | 1.00 | 0.57 (0.37~0.90) | 0.44 (0.27~0.73) | 0.32 (0.16~0.63) |
| Yes | 1.43 (0.62~3.32) | 1.60 (0.77~3.31) | 1.53 (0.74~3.15) | 0.35 (0.15~0.81) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, M.; Zou, Y.; Su, D.; Zhao, D.; Zhou, M.; Xu, P.; Zhang, R. Relationship of Composite Dietary Antioxidant Index vs. Alcohol Consumption with Mild Cognitive Impairment in the Elderly. Nutrients 2025, 17, 2111. https://doi.org/10.3390/nu17132111
He M, Zou Y, Su D, Zhao D, Zhou M, Xu P, Zhang R. Relationship of Composite Dietary Antioxidant Index vs. Alcohol Consumption with Mild Cognitive Impairment in the Elderly. Nutrients. 2025; 17(13):2111. https://doi.org/10.3390/nu17132111
Chicago/Turabian StyleHe, Mengjie, Yan Zou, Danting Su, Dong Zhao, Mengyi Zhou, Peiwei Xu, and Ronghua Zhang. 2025. "Relationship of Composite Dietary Antioxidant Index vs. Alcohol Consumption with Mild Cognitive Impairment in the Elderly" Nutrients 17, no. 13: 2111. https://doi.org/10.3390/nu17132111
APA StyleHe, M., Zou, Y., Su, D., Zhao, D., Zhou, M., Xu, P., & Zhang, R. (2025). Relationship of Composite Dietary Antioxidant Index vs. Alcohol Consumption with Mild Cognitive Impairment in the Elderly. Nutrients, 17(13), 2111. https://doi.org/10.3390/nu17132111







