How Did the Dietary Behavior of Older Korean Adults Change During the COVID-19 Pandemic?
Abstract
1. Introduction
2. Materials and Methods
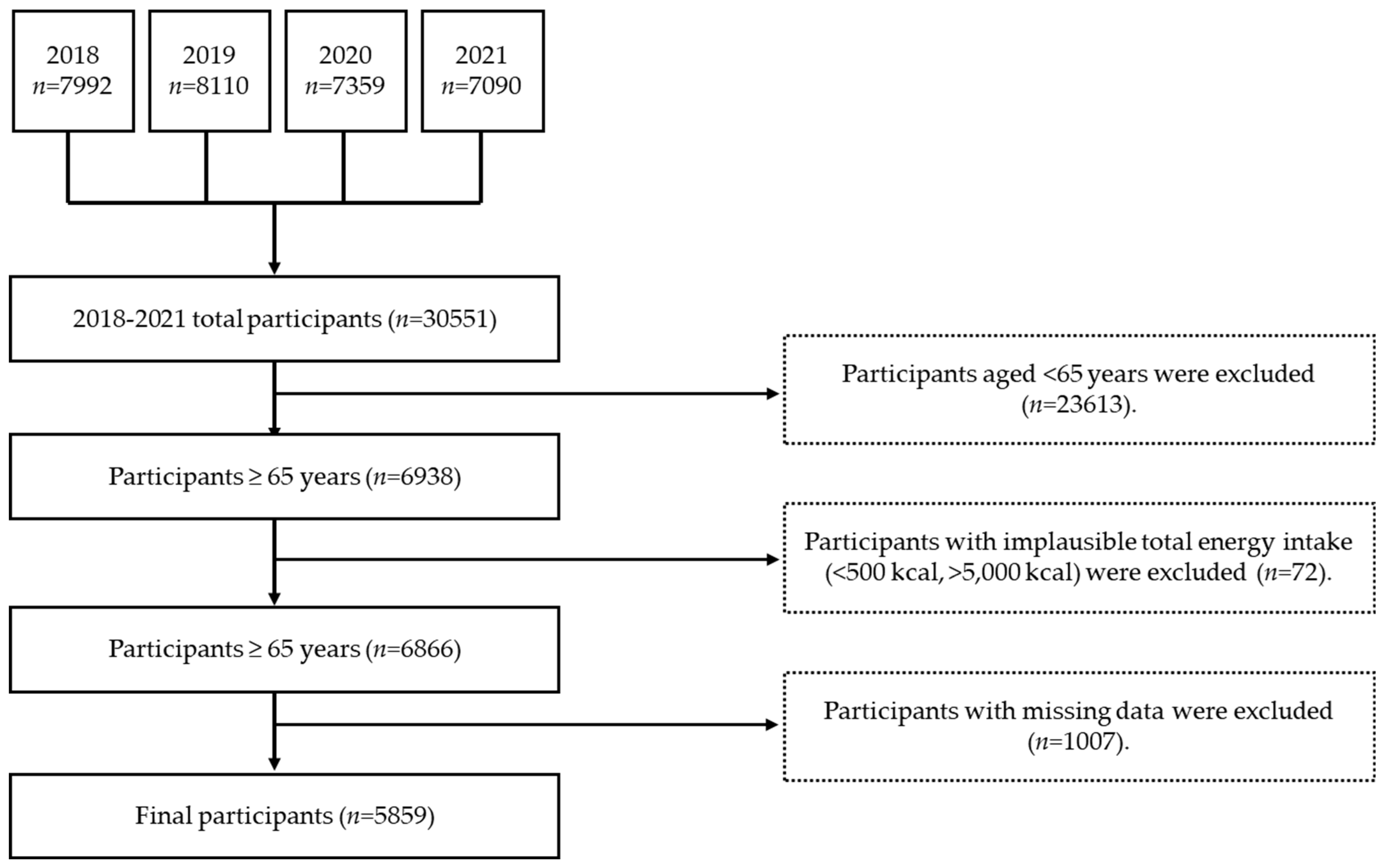
2.1. Study Population and Design
2.2. General Characteristics
2.3. Health Behavior
2.4. Dietary Habits
2.5. Food and Nutrient Intake
2.6. Statistical Analysis
3. Results
3.1. General Characteristics
3.2. Health-Related Behaviors Before vs. During COVID-19
3.3. Dietary Behaviors Before vs. During COVID-19
3.4. Food Group Intake Before vs. During COVID-19
3.5. Plant Food Intake Before vs. During COVID-19
3.6. Nutrient Intake Before vs. During COVID-19
3.7. Effects of the Pre- and During-COVID-19 Pandemic Periods on Nutritional Insufficiency
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 25 November 2023).
- Choi, J.H. Food Insecurity Is Associated with Dietary Consumption during the COVID-19 Pandemic: Data from the Korea National Health and Nutrition Examination Survey 2019–2020. Nutrients 2023, 15, 772. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Park, S.; Yoon, T.Y.; Ryoo, J.H.; Park, S.K.; Jung, J.Y.; Lee, J.H.; Oh, C.M. Nationwide changes in physical activity, nutrient intake, and obesity in South Korea during the COVID-19 pandemic era. Front. Endocrinol. 2022, 13, 965842. [Google Scholar] [CrossRef]
- Kwon, S.L.; Oh, J. COVID-19 vaccination program in South Korea: A long journey toward a new normal. Health Policy Technol. 2022, 11, 100601. [Google Scholar] [CrossRef] [PubMed]
- Onyeaka, H.; Anumudu, C.K.; Al-Sharify, Z.T.; Egele-Godswill, E.; Mbaegbu, P. COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Sci. Prog. 2021, 104, 00368504211019854. [Google Scholar] [CrossRef]
- Dighe, A.; Cattarino, L.; Cuomo-Dannenburg, G.; Skarp, J.; Imai, N.; Bhatia, S.; Gaythorpe, K.A.M.; Ainslie, K.E.C.; Baguelin, M.; Bhatt, S.; et al. Response to COVID-19 in South Korea and implications for lifting stringent interventions. BMC Med. 2020, 18, 321. [Google Scholar] [CrossRef] [PubMed]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Lee, S. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide effect of COVID-19 on physical activity: A descriptive study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Y.; Bennell, K.; White, D.K.; Wei, J.; Wu, Z.; He, H.; Liu, S.; Luo, X.; Hu, S.; et al. Physical distancing measures and walking activity in middle-aged and older residents in changsha, China, during the COVID-19 epidemic period: Longitudinal observational study. J. Med. Internet Res. 2020, 22, e21632. [Google Scholar] [CrossRef]
- Pryor, S.; Dietz, W. The COVID-19, obesity, and food insecurity syndemic. Curr. Obes. Rep. 2022, 11, 70–79. [Google Scholar] [CrossRef]
- Błaszczyk-Bebenek, E.; Jagielski, P.; Bolesławska, I.; Jagielska, A.; Nitsch-Osuch, A.; Kawalec, P. Nutrition behaviors in polish adults before and during COVID-19 lockdown. Nutrients 2020, 12, 3084. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Lopez, V. Global impact of COVID-19 on weight and weight-related behaviors in the adult population: A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 1876. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, K.M.; Harris, C.; Drawve, G.; Willis, D.E. Assessing food insecurity among US adults during the COVID-19 pandemic. J. Hunger Environ. Nutr. 2021, 16, 1–18. [Google Scholar] [CrossRef]
- Koltai, J.; Toffolutti, V.; McKee, M.; Stuckler, D. Prevalence and changes in food-related hardships by socioeconomic and demographic groups during the COVID-19 pandemic in the UK: A longitudinal panel study. Lancet Reg. Health Eur. 2021, 6, 100125. [Google Scholar] [CrossRef] [PubMed]
- Litton, M.M.; Beavers, A.W. The relationship between food security status and fruit and vegetable intake during the COVID-19 pandemic. Nutrients 2021, 13, 712. [Google Scholar] [CrossRef]
- Picchioni, F.; Goulao, L.F.; Roberfroid, D. The impact of COVID-19 on diet quality, food security and nutrition in low and middle income countries: A systematic review of the evidence. Clin. Nutr. 2021, 41, 2955–2964. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.; Mills, S.; Albani, V. Socioeconomic risks of food insecurity during the COVID-19 pandemic in the UK: Findings from the Understanding Society Covid Survey. BMC Public Health 2022, 22, 590. [Google Scholar] [CrossRef]
- Choi, S.; Ki, M. Estimating the reproductive number and the outbreak size of COVID-19 in Korea. Epidemiol. Health 2020, 42, e2020011. [Google Scholar] [CrossRef]
- Kim, S.W.; Lee, K.S.; Kim, K.; Lee, J.J.; Kim, J.Y. A brief telephone severity scoring system and therapeutic living centers solved acute hospital-bed shortage during the COVID-19 outbreak in daegu, Korea. J. Korean Med. Sci. 2020, 35, e152. [Google Scholar] [CrossRef]
- Ryu, S.K.; Chung, S.G. Korea’s early COVID-19 response: Findings and implications. Int. J. Environ. Res. Public Health 2021, 18, 8316. [Google Scholar] [CrossRef]
- Task Force for Tackling COVID-19. All About Korea’s Response to COVID-19. South Korea. Available online: http://www.kdca.go.kr/upload_comm/syview/doc.html?fn=160276224199800.pdf&rs=/upload_comm/docu/0030/ (accessed on 25 November 2023).
- Kim, S.Y.; Yoo, D.M.; Min, C.; Choi, H.G. Changes in Dietary Habits and Exercise Pattern of Korean Adolescents from Prior to during the COVID-19 Pandemic. Nutrients 2021, 13, 3314. [Google Scholar] [CrossRef]
- Kim, C.; Kim, E. Comparative study on the health and dietary habits of Korean male and female adults before and after the coronavirus disease 2019 pandemic: Utilizing data from the 8th Korea National Health and Nutrition Examination Survey (2019–2021). Korean J. Community Nutr. 2024, 29, 65–80. [Google Scholar] [CrossRef]
- Na, H.M.; Jung, B.M. Dietary behavior and diet quality in the Korean adult population by income level before and after the COVID-19 pandemic: Using the Korean National Health and Nutrition Examination Survey (2019–2020). Korean J. Community Living Sci. 2022, 33, 397–413. [Google Scholar] [CrossRef]
- Suh, B.D.; Kwon, K.H. Impacts of the depression among the elderly in the South Korea community in COVID-19 pandemic. J. Health Inform. Stat. 2021, 46, 54–63. [Google Scholar] [CrossRef]
- Kim, J.Y.; Jung, B.M. Comparison of the Health Behavior and Nutrient Intake of the Korean Elderly Before and After the Start of the COVID-19 Pandemic: Data from the 8th Korea National Health and Nutrition Examination Survey. Korean J. Community Living Sci. 2023, 34, 353–364. [Google Scholar] [CrossRef]
- Hur, Y.I.; Huh, Y.; Lee, J.H.; Lee, C.B.; Kim, B.; Yu, S.H.; Kim, J.H.; Kim, J.; Kim, H.M.; Lee, M.; et al. Factors Associated with Body Weight Gain among Korean Adults during the COVID-19 Pandemic. J. Obes. Metab. Syndr. 2022, 31, 51–60. [Google Scholar] [CrossRef]
- Lee, Y.S.; Lee, Y. Changes in nutritional status of Korean older adults during COVID-19 Pandemic by household income and demographic factors-using the Korea National Health and Nutrition Examination Survey (2019–2020): A cross-sectional study. Korean J. Community Nutr. 2023, 28, 302–316. [Google Scholar] [CrossRef]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Kang, M.S.; Jang, K.-A.; Kim, H.R.; Song, S. Association of Dietary Resistant Starch Intake with Obesity and Metabolic Syndrome in Korean Adults. Nutrients 2024, 16, 158. [Google Scholar] [CrossRef]
- Sung, H.; Park, J.M.; Oh, S.U.; Ha, K.; Joung, H. Consumption of ultra-processed foods increases the likelihood of having obesity in Korean women. Nutrients 2021, 13, 698. [Google Scholar] [CrossRef]
- Kwon, Y.S.; Ryu, J.H.; Yang, Y.; Park, Y.K.; Kim, S.H. Trends and Dietary Assessment According to Fruit and Vegetable Intake in Korean Elderly People: Analysis Based on the Korea National Health and Nutrition Examination Survey 1998, 2008, and 2018. Foods 2020, 9, 1712. [Google Scholar] [CrossRef]
- Bae, A.; Yoon, J.; Yun, S.-Y.; Asano, K. Dietary and health characteristics of the young-old and the old-old by food security status: Analysis of data from the 6th (2013~2015) Korea National Health and Nutrition Examination Survey. J. Nutr. Health 2019, 52, 104–117. [Google Scholar] [CrossRef]
- Jung, K.H.; Oh, Y.H.; Kang, E.N.; Kim, K.R.; Lee, Y.K.; Oh, M.A.; Hwang, N.H.; Kim, S.J.; Lee, S.H.; Lee, S.G.; et al. 2017 Investigation of Elderly Conditions; Korea Institute for Health and Social Affairs: Sejong, Republic of Korea, 2017.
- Korean Society for the Study of Obesity. Available online: https://general.kosso.or.kr/html/?pmode=obesityDiagnosis (accessed on 21 November 2024).
- World Health Organization, Regional Office for the Western Pacific. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; World Health Organization: Geneva, Switzerland, 2000.
- Shim, J.S.; Oh, K.W.; Nam, C.M. Association of Household Food Security with Dietary Intake; Based on the Third (2005) Korea National Health and Nutrition Examination Survey (KNHANES III). J. Nutr. Health 2008, 41, 174–183. [Google Scholar]
- Lee, S.J.; Lee, K.W.; Oh, J.E.; Cho, M.S. Nutritional and health consequences are associated with food insecurity among Korean elderly: Based on the fifth (2010) Korea National Health and Nutrition Examination Survey (KNHANES V-1). J. Nutr. Health 2015, 48, 519–529. [Google Scholar] [CrossRef]
- Kwon, J.; Shim, J.; Park, M.; Paik, H. Evaluation of fruits and vegetables intake for prevention of chronic disease in Korean adults aged 30 years and over: Using the Third Korea National Health and Nutrition Examination Survey (KNHANES III), 2005. J. Nutr. Health 2009, 42, 146–157. [Google Scholar] [CrossRef]
- World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation; World Health Organization: Geneva, Switzerland, 2003.
- World Cancer Research Fund. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. A Summary of the Third Expert Report; World Cancer Research Fund: London, UK, 2018. [Google Scholar]
- National Institute of Agricultural Sciences of Korea. Food Composition Table, 9.1 Revision; Rural Development Administration: Wanju, Republic of Korea, 2016.
- Kim, S.; Kwon, Y.S.; Hong, K.H. What Is the Relationship between the Chewing Ability and Nutritional Status of the Elderly in Korea? Nutrients 2023, 15, 2042. [Google Scholar] [CrossRef]
- Korea Disease Control and Prevention Agency. Korea Health Statistics 2022; Korea Disease Control and Prevention Agency: Cheongju, Republic of Korea, 2022.
- Korea Disease Control and Prevention Agency. Guideline for 8th Korea National Health and Nutrition Examination Survey (KNHANES VIII); Korea Disease Control and Prevention Agency: Cheongju, Republic of Korea, 2018.
- Yun, S.H.; Oh, K.W. Dietary habits among Korean population. Public Health Wkly. Rep. 2022, 15, 1623–1632. [Google Scholar]
- Chung, S.R. Changes in food security before and after the COVID-19 pandemic: Comparing rural and urban areas. In Proceedings of the Korean Society of Community Nutrition Fall Conference, Seoul, Republic of Korea, 27 October 2023. [Google Scholar]
- Acton, R.B.; Vanderlee, L.; Cameron, A.J.; Goodman, S.; Jáuregui, A.; Sacks, G.; White, C.M.; White, M.; Hammond, D. Selfreported impacts of the COVID-19 pandemic on diet-related behaviors and food security in 5 countries: Results from the International Food Policy Study 2020. J. Nutr. 2022, 152, 35s–46s. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 14 November 2023).
- Dietz, W.H.; Douglas, C.; Brownson, R.C. Chronic Disease Prevention: Tobacco Avoidance, Physical Activity, and Nutrition for a Healthy Start. JAMA 2016, 316, 1645–1646. [Google Scholar] [CrossRef] [PubMed]
- Kimokoti, R.W.; Millen, B.E. Nutrition for the Prevention of Chronic Diseases. Med. Clin. 2016, 100, 1185–1198. [Google Scholar] [CrossRef]
- Sachdeva, S.; Sachdev, T.R.; Sachdeva, R. Increasing fruit and vegetable consumption: Challenges and opportunities. Indian J. Community Med. 2013, 38, 192–197. [Google Scholar] [CrossRef]
- Larson, E.A.; Bader-Larsen, K.S.; Magkos, F. The Effect of COVID-19-related Lockdowns on Diet and Physical Activity in Older Adults: A Systematic Review. Aging and Dis. 2021, 12, 1935–1947. [Google Scholar]
- Wang, J.; Yeoh, E.K.; Yung, T.K.C.; Wong, M.C.S.; Dong, D.; Chen, X.; Chan, M.K.Y.; Wong, E.L.Y.; Wu, Y.; Guo, Z.; et al. Change in eating habits and physical activities before and during the COVID-19 pandemic in Hong Kong: A cross-sectional study via random telephone survey. J. Int. Soc. Sports Nutr. 2021, 18, 33. [Google Scholar] [CrossRef] [PubMed]
- Liday, D.M. Eating behavior and physical activity of senior citizens during the COVID-19 lockdown. Int. J. Public Health Sci. 2021, 10, 493–499. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare; The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2020; Ministry of Health and Welfare: Sejong, Republic of Korea, 2021.
- Cutler, J.A.; Follmann, D.; Allender, P.S. Randomized trials of sodium reduction: An overview. Am. J. Clin. Nutr. 1997, 65, 643S–651S. [Google Scholar] [CrossRef]
- Karppanen, H.; Mervaala, E. Sodium intake and hypertension. Prog. Cardiovasc. Dis. 2006, 49, 59–75. [Google Scholar] [CrossRef]
- Hoffmann, I.S.; Cubeddu, L.X. Salt and the metabolic syndrome. Nutr. Metab. Cardiovasc. Dis. 2009, 19, 123–128. [Google Scholar] [CrossRef]
- Ju, S.; Kwon, Y.; Yeum, K.J. Persistent Calcium Inadequacy in Korean Adults over 20 Years: Analysis of the 1998–2018 Korea National Health and Nutrition Examination Survey. Foods 2024, 13, 3568. [Google Scholar] [CrossRef]
- Jeong, C.E.; Lee, H.; Lee, J.E. Intake of energy and macronutrients according to household income among elementary, middle, and high school students before and during the COVID-19 pandemic: A cross-sectional study. Korean J. Community Nutr. 2024, 29, 234–252. [Google Scholar] [CrossRef]
| Variables | Before COVID-19 (n = 2943) | During COVID-19 (n = 2916) | Total (n = 5859) | p-Value (1) | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Total | 2943 | 47.07 | 2916 | 52.93 | 5859 | 100.00 | - |
| Sex | 0.331 | ||||||
| Male | 1234 | 44.76 | 1252 | 46.01 | 2486 | 45.43 | |
| Female | 1709 | 55.24 | 1664 | 53.99 | 3373 | 54.57 | |
| Age (years) | 0.919 | ||||||
| 65–74 | 1688 | 58.98 | 1672 | 59.16 | 3360 | 59.07 | |
| ≥75 | 1255 | 41.02 | 1244 | 40.84 | 2499 | 40.93 | |
| Marital status | 0.878 | ||||||
| Married | 2919 | 99.17 | 2890 | 99.21 | 5809 | 99.19 | |
| Single | 24 | 0.83 | 26 | 0.79 | 50 | 0.81 | |
| Education level | 0.605 | ||||||
| High school graduate or lower | 1919 | 66.12 | 1685 | 64.16 | 3604 | 65.12 | |
| High school diploma | 513 | 20.95 | 524 | 22.45 | 1037 | 21.72 | |
| College degree or higher | 309 | 12.93 | 315 | 13.39 | 624 | 13.17 | |
| Region | 0.317 | ||||||
| City | 2132 | 78.57 | 1995 | 74.19 | 4127 | 76.26 | |
| Rural area | 811 | 21.43 | 921 | 25.81 | 1732 | 23.74 | |
| Employment status | 0.003 | ||||||
| Employed | 934 | 33.20 | 1002 | 38.86 | 1936 | 36.09 | |
| Unemployed | 1810 | 66.80 | 1525 | 61.14 | 3335 | 63.91 | |
| Household income | 0.557 | ||||||
| Low | 1411 | 44.87 | 1323 | 42.23 | 2734 | 43.48 | |
| Middle-low | 812 | 28.15 | 837 | 29.62 | 1649 | 28.93 | |
| Middle-high | 445 | 16.86 | 450 | 16.87 | 895 | 16.87 | |
| High | 266 | 10.12 | 280 | 11.27 | 546 | 10.73 | |
| Variables | Before COVID-19 (n = 2943) | During COVID-19 (n = 2916) | Total (n = 5859) | p-Value (1) | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Smoking status | |||||||
| Current smoker | 249 | 9.22 | 267 | 9.73 | 516 | 9.49 | 0.675 |
| Past smoker | 825 | 29.65 | 796 | 30.47 | 1621 | 30.08 | |
| Non-smoker | 1830 | 61.13 | 1795 | 59.80 | 3625 | 60.43 | |
| Drinking frequency | |||||||
| <1 time/month | 1910 | 63.91 | 2000 | 68.69 | 3910 | 66.43 | 0.006 |
| 1–4 times/month | 527 | 19.19 | 465 | 16.48 | 992 | 17.76 | |
| 2–3 times/week | 252 | 9.03 | 233 | 8.89 | 485 | 8.96 | |
| ≥4 times/week | 219 | 7.86 | 163 | 5.94 | 382 | 6.85 | |
| Stress level | |||||||
| Severe stress | 106 | 3.21 | 96 | 3.17 | 202 | 3.19 | 0.287 |
| Moderate stress | 407 | 13.92 | 388 | 13.18 | 795 | 13.53 | |
| Mild stress | 1478 | 52.35 | 1538 | 55.37 | 3016 | 53.94 | |
| No stress | 913 | 30.52 | 830 | 28.29 | 1743 | 29.34 | |
| Exercise | |||||||
| <1 day/week | 2244 | 80.18 | 1977 | 76.91 | 4221 | 78.51 | 0.057 |
| 1–2 days/week | 88 | 3.58 | 100 | 3.99 | 188 | 3.79 | |
| 3–4 days/week | 134 | 5.34 | 136 | 5.41 | 270 | 5.37 | |
| ≥5 days/week | 282 | 10.90 | 315 | 13.69 | 597 | 12.33 | |
| Obesity status | |||||||
| Underweight (BMI < 18.5) | 77 | 2.46 | 91 | 3.15 | 168 | 2.82 | 0.164 |
| Normal (18.5 ≤ BMI < 23) | 1000 | 35.20 | 940 | 33.83 | 1940 | 34.49 | |
| Overweight (23 ≤ BMI < 25) | 765 | 26.78 | 712 | 25.09 | 1477 | 25.90 | |
| Obesity (BMI ≥ 25) | 1055 | 35.56 | 1054 | 37.93 | 2109 | 36.80 | |
| Chewing ability | |||||||
| Very inconvenient | 288 | 8.41 | 276 | 9.39 | 564 | 8.92 | 0.063 |
| Inconvenient | 827 | 27.92 | 698 | 24.20 | 1525 | 25.96 | |
| Normal | 533 | 18.19 | 510 | 18.69 | 1043 | 18.45 | |
| Not inconvenient | 529 | 18.98 | 603 | 21.22 | 1132 | 20.16 | |
| Not inconvenient at all | 725 | 26.50 | 770 | 26.51 | 1495 | 26.51 | |
| Variables | Before COVID-19 (n = 2943) | During COVID-19 (n = 2916) | Total (n = 5859) | p–Value (1) | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Breakfast | <0.001 | ||||||
| 5–7 times/week | 2741 | 93.00 | 2693 | 91.56 | 5434 | 92.24 | |
| 3–4 times/week | 85 | 3.21 | 61 | 2.18 | 146 | 2.66 | |
| 1–2 times/week | 40 | 1.27 | 66 | 2.55 | 106 | 1.95 | |
| Rarely (<1 time/week) | 77 | 2.52 | 96 | 3.72 | 173 | 3.15 | |
| Snack | 0.6492 | ||||||
| Yes | 2672 | 91.27 | 2641 | 90.87 | 5313 | 91.06 | |
| No | 271 | 8.73 | 275 | 9.13 | 546 | 8.94 | |
| Daily meal pattern (2) | 0.2935 | ||||||
| B + L | 108 | 3.53 | 107 | 3.81 | 215 | 3.68 | |
| B + D | 201 | 6.99 | 228 | 8.24 | 429 | 7.65 | |
| L + D | 120 | 4.21 | 144 | 5.28 | 264 | 4.78 | |
| B + L + D | 2485 | 84.41 | 2412 | 81.92 | 4897 | 83.09 | |
| Others | 26 | 0.86 | 23 | 0.74 | 49 | 0.80 | |
| Home | 0.6488 | ||||||
| Eating | 2823 | 95.82 | 2815 | 96.10 | 5638 | 95.97 | |
| Not eating | 120 | 4.18 | 101 | 3.90 | 221 | 4.03 | |
| Commercial location | 0.0715 | ||||||
| Eating | 1276 | 45.60 | 1192 | 42.34 | 2468 | 43.88 | |
| Not eating | 1667 | 54.40 | 1724 | 57.66 | 3391 | 56.12 | |
| Institutional location | <0.001 | ||||||
| Eating | 209 | 7.01 | 94 | 3.28 | 303 | 5.04 | |
| Not eating | 2734 | 92.99 | 2822 | 96.72 | 5859 | 94.96 | |
| Frequency of eating–out | <0.001 | ||||||
| ≥1 time/day | 130 | 5.13 | 97 | 3.91 | 227 | 4.49 | |
| 5–6 times/week | 203 | 7.13 | 155 | 5.49 | 358 | 6.26 | |
| 3–4 times/week | 249 | 8.97 | 180 | 6.21 | 429 | 7.51 | |
| 1–2 times/week | 819 | 28.33 | 515 | 18.91 | 1334 | 23.34 | |
| 1–3 times/month | 938 | 31.54 | 1027 | 34.46 | 1965 | 33.08 | |
| Rarely | 604 | 18.90 | 942 | 31.03 | 1546 | 25.32 | |
| Food security | 0.0056 | ||||||
| Sufficiently food secure | 1395 | 48.57 | 1585 | 54.88 | 2980 | 51.91 | |
| Mildly food insecure | 1377 | 46.29 | 1180 | 40.18 | 2557 | 43.06 | |
| Moderately/Severe food insecure | 168 | 5.14 | 150 | 4.94 | 318 | 5.03 | |
| Food Group | Before COVID-19 (n = 2943) | During COVID-19 (n = 2916) | Total (n = 5859) | Unadjusted p-Value (1) | Adjusted p-Value (2) |
|---|---|---|---|---|---|
| Total food (g) | 1243.00 ± 16.14 (3) | 1255.33 ± 19.24 | 1249.53 ± 12.47 | 0.2805 | 0.0065 |
| Cereals and grains (g) | 260.13 ± 2.74 | 241.30 ± 2.77 | 250.16 ± 1.91 | <0.0001 | 0.0002 |
| Potatoes and starches (g) | 33.62 ± 2.25 | 41.24 ± 2.33 | 37.65 ± 1.62 | 0.0539 | 0.0137 |
| Sugars and sweets (g) | 5.85 ± 0.30 | 5.52 ± 0.26 | 5.68 ± 0.20 | 0.6031 | 0.7364 |
| Legumes (g) | 43.90 ± 1.99 | 51.31 ± 2.08 | 47.82 ± 1.44 | 0.0070 | 0.0023 |
| Seeds and nuts (g) | 7.96 ± 0.70 | 8.04 ± 0.70 | 8.00 ± 0.49 | 0.9801 | 0.8785 |
| Vegetables (4) (g) | 304.28 ± 5.08 | 327.82 ± 5.67 | 316.74 ± 3.85 | 0.0005 | <0.0001 |
| Mushrooms (g) | 4.64 ± 0.56 | 4.45 ± 0.48 | 4.54 ± 0.37 | 0.9127 | 0.8652 |
| Fruits (5) (g) | 166.20 ± 5.99 | 160.91 ± 6.15 | 163.40 ± 4.28 | 0.9100 | 0.7176 |
| Seaweed (g) | 29.63 ± 2.33 | 32.36 ± 2.60 | 31.08 ± 1.74 | 0.2324 | 0.2009 |
| Meat and poultry (g) | 60.64 ± 2.72 | 61.60 ± 2.57 | 61.15 ± 1.86 | 0.9837 | 0.7465 |
| Eggs (g) | 22.18 ± 0.94 | 25.42 ± 0.99 | 23.90 ± 0.67 | 0.0149 | 0.0091 |
| Fishes and shell fishes (g) | 100.62 ± 4.07 | 90.60 ± 3.86 | 95.32 ± 2.75 | 0.1433 | 0.1565 |
| Milks and dairy products (g) | 63.72 ± 3.03 | 73.11 ± 3.40 | 68.69 ± 2.29 | 0.0206 | 0.0060 |
| Oils and fats (g) | 3.82 ± 0.14 | 4.15 ± 0.17 | 4.00 ± 0.11 | 0.0267 | 0.0043 |
| Beverages (g) | 59.48 ± 3.60 | 59.92 ± 3.76 | 59.71 ± 2.59 | 0.9569 | 0.9265 |
| Seasonings (g) | 26.60 ± 0.61 | 26.73 ± 0.77 | 26.67 ± 0.50 | 0.9501 | 0.6483 |
| Other food (g) | 0.91 ± 0.43 | 0.74 ± 0.15 | 0.82 ± 0.22 | 0.6863 | 0.6749 |
| Plant Food (g/day) | Before COVID-19 (n = 2943) | During COVID-19 (n = 2916) | Total (n = 5859) | Unadjusted p-Value (1) | Adjusted p-Value (2),(3) |
|---|---|---|---|---|---|
| Fresh fruits (5) | 165.46 ± 5.95 (4) | 157.33 ± 6.10 | 161.16 ± 4.25 | 0.4041 | 0.6372 |
| Non-starchy vegetables (6) | 184.91 ± 4.43 | 199.37 ± 4.81 | 192.56 ± 3.26 | 0.0233 | 0.0040 |
| Fresh fruits and non-starchy vegetables | 350.37 ± 8.42 | 356.70 ± 8.64 | 353.72 ± 5.95 | 0.5279 | 0.2004 |
| Nutrients | Before COVID-19 (n = 2943) | During COVID-19 (n = 2916) | Total (n = 5859) | Unadjusted p-Value (1) | Adjusted p-Value (2),(3) |
|---|---|---|---|---|---|
| Energy (kcal) | 1617.70 ± 14.24 (4) | 1579.98 ± 16.77 | 1597.73 ± 11.08 | <0.0001 | 0.0497 |
| Carbohydrate (g) | 272.43 ± 2.34 | 258.98 ± 2.44 | 265.31 ± 1.67 | 0.0015 | 0.0003 |
| Protein (g) | 55.51 ± 0.67 | 56.58 ± 0.82 | 56.08 ± 0.53 | 0.1332 | 0.0001 |
| Fat (g) | 28.60 ± 0.52 | 31.54 ± 0.68 | 30.15 ± 0.43 | 0.0003 | <0.0001 |
| Fiber (g) | 25.77 ± 0.37 | 27.27 ± 0.39 | 26.56 ± 0.27 | 0.0009 | <0.0001 |
| Calcium (mg) | 457.98 ± 8.13 | 471.91 ± 7.93 | 465.35 ± 5.66 | 0.0906 | 0.0067 |
| Phosphorus (mg) | 911.70 ± 10.61 | 938.87 ± 12.39 | 926.08 ± 8.16 | 0.0192 | <0.0001 |
| Iron (mg) | 9.79 ± 0.16 | 8.54 ± 0.16 | 9.13 ± 0.11 | <0.0001 | <0.0001 |
| Sodium (mg) | 2816.22 ± 38.77 | 2885.60 ± 45.64 | 2852.95 ± 30.48 | 0.1247 | 0.6253 |
| Magnesium (mg) | 300.07 ± 3.52 | 301.57 ± 3.96 | 300.87 ± 2.66 | 0.3785 | 0.0117 |
| Potassium (mg) | 2524.38 ± 34.25 | 2599.63 ± 36.18 | 2564.22 ± 24.85 | 0.0457 | <0.0001 |
| Zinc (mg) | 9.19 ± 0.10 | 9.25 ± 0.12 | 9.22 ± 0.08 | 0.3771 | 0.0059 |
| Vitamin A (μg RAE) | 323.49 ± 12.08 | 342.88 ± 10.00 | 333.75 ± 7.68 | 0.2692 | 0.1063 |
| Carotene (μg) | 2725.37 ± 82.73 | 2874.32 ± 86.64 | 2804.22 ± 59.59 | 0.2205 | 0.0967 |
| Retinol (μg) | 96.40 ± 9.27 | 103.34 ± 5.61 | 100.08 ± 5.22 | 0.6583 | 0.4892 |
| Thiamine (mg) | 1.06 ± 0.01 | 0.95 ± 0.01 | 1.00 ± 0.01 | <0.0001 | <0.0001 |
| Riboflavin (mg) | 1.18 ± 0.02 | 1.22 ± 0.02 | 1.20 ± 0.01 | 0.0408 | 0.0004 |
| Niacin (mg) | 9.99 ± 0.14 | 9.72 ± 0.16 | 9.85 ± 0.10 | 0.6609 | 0.8147 |
| Vitamin D (μg) | 2.72 ± 0.17 | 2.58 ± 0.11 | 2.65 ± 0.10 | 0.7035 | 0.8619 |
| Vitamin E (mg α-TE) | 5.33 ± 0.09 | 5.78 ± 0.09 | 5.57 ± 0.07 | 0.0001 | <0.0001 |
| Vitamin C (mg) | 55.76 ± 1.73 | 62.71 ± 1.83 | 59.44 ± 1.25 | 0.0083 | 0.0010 |
| Folic acid (μg DFE) | 309.50 ± 4.21 | 320.65 ± 4.71 | 315.41 ± 3.17 | 0.0315 | 0.0002 |
| Energy distribution (%) | |||||
| Carbohydrate | 71.02 ± 0.26 | 68.79 ± 0.30 | 69.84 ± 0.19 | <0.0001 | <0.0001 |
| Protein | 13.62 ± 0.09 | 14.10 ± 0.10 | 13.87 ± 0.07 | <0.0001 | 0.0003 |
| Fat | 15.36 ± 0.20 | 17.11 ± 0.23 | 16.29 ± 0.15 | <0.0001 | <0.0001 |
| Total (1) | Energy | Calcium | Iron | Vitamin A | Riboflavin | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Before COVID-19 | 503 | 16.45 | 947 | 31.57 | 2312 | 77.72 | 859 | 28.10 | 2383 | 81.00 | 1393 | 46.67 |
| During COVID-19 | 619 | 20.76 | 1037 | 35.59 | 2195 | 73.82 | 1164 | 39.34 | 2263 | 77.12 | 1299 | 43.24 |
| p-value (2) | 0.0012 | 0.014 | 0.0184 | <0.0001 | 0.0103 | 0.0822 | ||||||
| Model 1 | 1.350 (1.121–1.626) ** (3) | 1.198 (1.026–1.399) * | 0.781 (0.652–0.936) ** | 1.652 (1.398–1.952) *** | 0.809 (0.675–0.970) ** | 0.859 (0.727–1.014) | ||||||
| Model 2 | 1.375 (1.142–1.655) *** | 1.221 (1.046–1.426) * | 0.796 (0.663–0.956) * | 1.676 (1.420–1.978) *** | 0.821 (0.686–0.984) * | 0.875 (0.742–1.031) | ||||||
| Model 3 | 1.314 (1.092–1.580) ** | 1.171 (1.003–1.360) * | 0.797 (0.663–0.959) * | 1.632 (1.384–1.926) *** | 0.818 (0.683–0.978) * | 0.851 (0.721–1.003) | ||||||
| Model 4 | 1.419 (1.170–1.721) *** | 1.172 (0.998–1.376) | 0.783 (0.647–0.947) * | 1.697 (1.429–2.016) *** | 0.834 (0.692–1.005) | 0.841 (0.712–0.995) * | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, Y.-S.; Kim, D.; Lim, H.-S. How Did the Dietary Behavior of Older Korean Adults Change During the COVID-19 Pandemic? Nutrients 2025, 17, 1973. https://doi.org/10.3390/nu17121973
Kwon Y-S, Kim D, Lim H-S. How Did the Dietary Behavior of Older Korean Adults Change During the COVID-19 Pandemic? Nutrients. 2025; 17(12):1973. https://doi.org/10.3390/nu17121973
Chicago/Turabian StyleKwon, Yong-Seok, Dasol Kim, and Hee-Sook Lim. 2025. "How Did the Dietary Behavior of Older Korean Adults Change During the COVID-19 Pandemic?" Nutrients 17, no. 12: 1973. https://doi.org/10.3390/nu17121973
APA StyleKwon, Y.-S., Kim, D., & Lim, H.-S. (2025). How Did the Dietary Behavior of Older Korean Adults Change During the COVID-19 Pandemic? Nutrients, 17(12), 1973. https://doi.org/10.3390/nu17121973





