Socioeconomic and Health-Related Determinants of Eating Habits in Polish Caucasian Older Population—The Nationwide PolSenior2 Study Results
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Protocol and Participants
2.2. Evaluation of Dietary Habits
- Vegetables: daily frequency of consumption ≥ 3;
- Fruit: daily frequency ≥ 2;
- Protein (meat, dairy, eggs, fish): daily frequency ≥ 3;
- Fish: weekly frequency ≥ 1;
- Low-fat dairy: daily frequency ≥ 3;
- Wholegrain carbohydrates: daily frequency ≥ 3;
- Free sugars: daily frequency 1;
- Fats: 100% unsaturated; no saturated fats consumed;
- Fluids: ≥1500 mL per day;
- Alcohol: weekly frequency ≤ 1.
2.3. Data Analysis and Covariates
2.4. Statistical Analysis
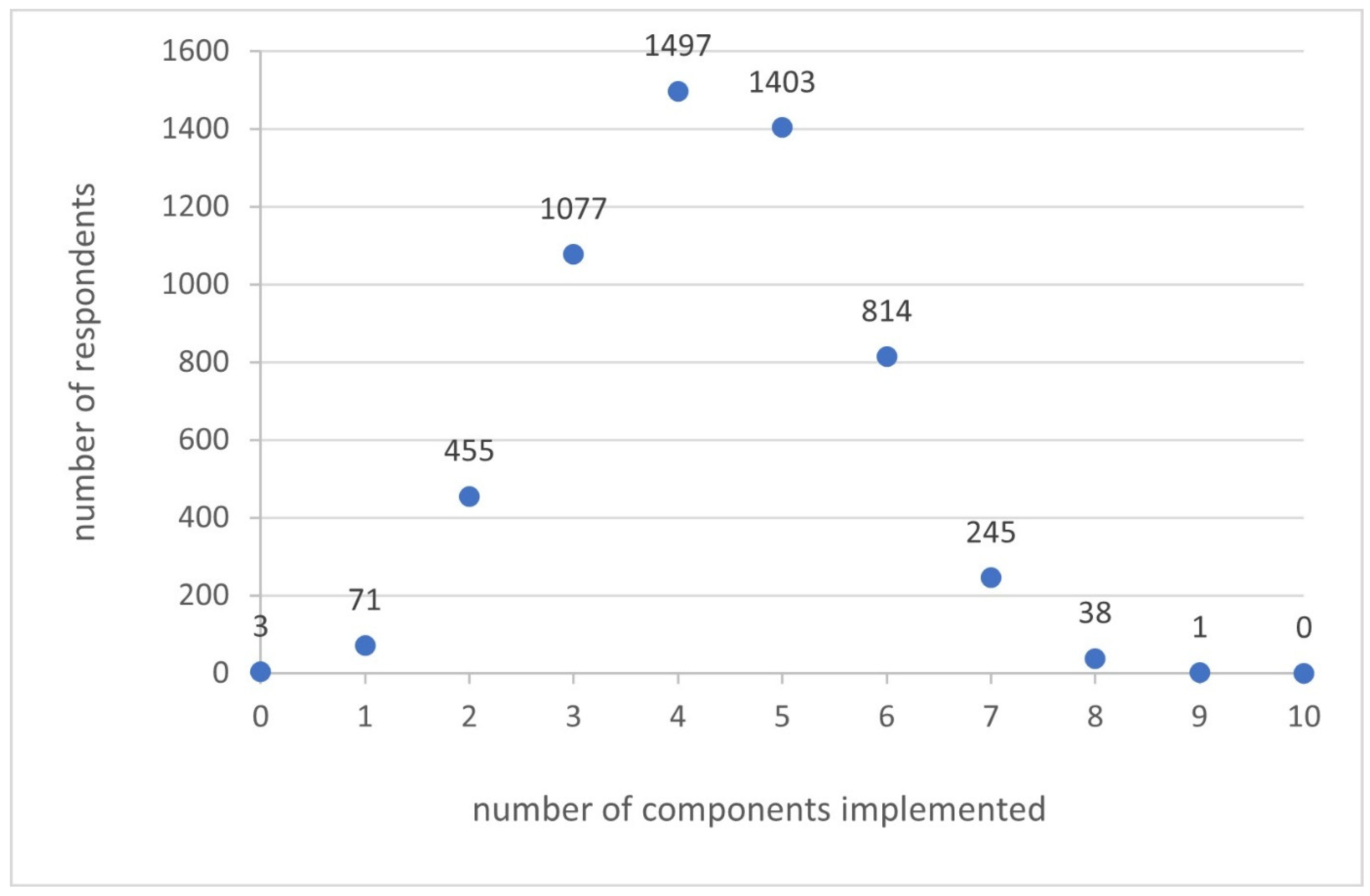
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Govindaraju, T.; Sahle, B.W.; McCaffrey, T.A.; McNeil, J.J.; Owen, A.J. Dietary patterns and quality of life in older adults: A Systematic Review. Nutrients 2018, 10, 971. [Google Scholar] [CrossRef]
- Clegg, M.E.; Williams, E.A. Optimizing nutrition in older people. Maturitas 2018, 112, 34–38. [Google Scholar] [CrossRef]
- Vega-Cabello, V.; Struijk, E.A.; Caballero, F.F.; Yévenes-Briones, H.; Ortolá, R.; Calderón-Larrañaga, A.; Lana, A.; Rodríguez-Artalejo, F.; Lopez-Garcia, E. Diet quality and multimorbidity in older adults: A Prospective Cohort Study. J. Gerontol. Ser. A 2024, 79, glad285. [Google Scholar] [CrossRef] [PubMed]
- Gajda, R.; Raczkowska, E.; Sobieszczańska, M.; Noculak, Ł.; Szymala-Pędzik, M.; Godyla-Jabłoński, M. Diet quality variation among Polish older adults: Association with selected metabolic diseases, demographic characteristics and socioeconomic status. Int. J. Environ. Res. Public Health 2023, 20, 2878. [Google Scholar] [CrossRef] [PubMed]
- Dorrington, N.; Fallaize, R.; Hobbs, D.; Weech, M.; Lovegrove, J.A. Diet Quality Index for older adults (DQI-65): Development and use in predicting adherence to dietary recommendations and health markers in the UK National Diet and Nutrition Survey. Br. J. Nutr. 2022, 128, 2193–2207. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Shams-White, M.M.; Pannucci, T.E.; Lerman, J.L.; Herrick, K.A.; Zimmer, M.; Mathieu, K.M.; Stoody, E.E.; Reedy, J. Healthy Eating Index-2020: Review and update process to reflect the dietary guidelines for Americans, 2020–2025. J. Acad. Nutr. Diet. 2023, 123, 1280–1288. [Google Scholar] [CrossRef]
- Kourlaba, G.; Polychronopoulos, E.; Zampelas, A.; Lionis, C.; Panagiotakos, D.B. Development of a diet index for older adults and its relation to cardiovascular disease risk factors: The Elderly Dietary Index. J. Am. Diet. Assoc. 2009, 109, 1022–1030. [Google Scholar] [CrossRef]
- Jeruszka-Bielak, M.; Hamulka, J.; Czarniecka-Skubina, E.; Hoffmann, M.; Kostyra, E.; Stasiewicz, B.; Jeszka, J.; Wadolowska, L. Dietary-Physical Activity Patterns in the Health Context of Older Polish Adults: The ‘ABC of Healthy Eating’ Project. Nutrients 2022, 14, 3757. [Google Scholar] [CrossRef]
- Hamulka, J.; Frackiewicz, J.; Stasiewicz, B.; Jeruszka-Bielak, M.; Piotrowska, A.; Leszczynska, T.; Niedzwiedzka, E.; Brzozowska, A.; Wadolowska, L. Socioeconomic, Eating- and Health-Related Limitations of Food Consumption among Polish Women 60+ Years: The ‘ABC of Healthy Eating’ Project. Nutrients 2021, 14, 51. [Google Scholar] [CrossRef]
- Dardzińska, J.A.; Małgorzewicz, S.; Szupryczyńska, N.; Gładyś, K.; Śliwińska, A.; Kaczkan, M.; Pieszko, M.; Wojda, A.; Wernio, E.; Gogga, P.; et al. Adherence to the 2021 dietary guidelines of the European Society of Cardiology on cardiovascular disease prevention in residents of the Pomeranian Voivodeship with increased cardiovascular risk. Pol. Arch. Intern. Med. 2023, 133, 16418. [Google Scholar] [CrossRef]
- Schroll, K.; Carbajal, A.; Decarli, B.; Martins, I.; Grunenberger, F.; Blauw, Y.H.; de Groot, C.P. Food patterns of elderly Europeans—SENECA Investigators. Eur. J. Clin. Nutr. 1996, 50, S86–S100. [Google Scholar] [PubMed]
- Leung, C.W.; Epel, E.S.; Ritchie, L.D.; Crawford, P.B.; Laraia, B.A. Food insecurity is inversely associated with diet quality of lower-income adults. J. Acad. Nutr. Diet. 2014, 114, 1943–1953. [Google Scholar] [CrossRef]
- Stefler, D.; Yi, X.; Malyutina, S.; Kubinova, R.; Pajak, A.; Hrezova, E.; Pikhart, H.; Peasey, A.; Bobak, M. Socioeconomic determinants of traditional diet in Eastern Europe: Result from the HAPIEE study. Eur. J. Public Health 2021, 31, piii318. [Google Scholar] [CrossRef]
- Wierucki, Ł.; Kujawska-Danecka, H.; Mossakowska, M.; Grodzicki, T.; Błędowski, P.; Chudek, J.; Kostka, T.; Więcek, A.; Hajduk, A.; Bandosz, P.; et al. Health status and its socio-economic covariates in the older population in Poland–the assumptions and methods of the nationwide, cross-sectional PolSenior2 survey. Arch. Med. Sci. 2022, 18, 92. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Sheikh, J.I.; Yesavage, J.A.; Brooks, J.O.; Friedman, L.; Gratzinger, P.; Hill, R.D.; Zadeik, A.; Crook, T. Proposed factor structure of the Geriatric Depression Scale. Int. Psychogeriatr. 1991, 3, 23–28. [Google Scholar] [CrossRef]
- Vellas, B.; Guigoz, Y.; Garry, P.J.; Nourhashemi, F.; Bennahum, D.; Lauque, S.; Albarede, J.-L. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 1999, 15, 116–122. [Google Scholar] [CrossRef]
- Niedzwiedzka, E.; Wadolowska, L.; Kowalkowska, J. Reproducibility of a Non-Quantitative Food Frequency Questionnaire (62-Item FFQ-6) and PCA-Driven Dietary Pattern Identification in 13–21-Year-Old Females. Nutrients 2019, 11, 2183. [Google Scholar] [CrossRef]
- Bledowski, P.; Mossakowska, M.; Chudek, J.; Grodzicki, T.; Milewicz, A.; Szybalska, A.; Zdrojewski, T. Medical, psychological and socioeconomic aspects of aging in Poland: Assumptions and objectives of the PolSenior project. Exp. Gerontol. 2011, 46, 1003–1009. [Google Scholar] [CrossRef] [PubMed]
- Institute of Food and Nutrition. Healthy Eating and Physical Activity Pyramid for Older Adults. Ministry of Health. Available online: https://www.gov.pl/attachment/e91f7a31-0196-4c57-a6d5-d28d4bace1b1 (accessed on 22 March 2025).
- Sheiham, A.; Steele, J.G.; Marcenes, W.; Finch, S.; Walls, A.W. The impact of oral health on stated ability to eat certain foods; findings from the National Diet and Nutrition Survey of Older People in Great Britain. Gerodontology 1999, 16, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic—Report of a WHO Consultation; WHO Technical Report Series No. 894; World Health Organization: Geneva, Italy, 2000; Available online: https://apps.who.int/iris/handle/10665/42330 (accessed on 11 March 2025).
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Moradell, A.; Casajús, J.A.; Moreno, L.A.; Vicente-Rodríguez, G. Perspectives on diet and exercise interaction for healthy aging: Opportunities to reduce malnutrition risk and optimize fitness. Nutrients 2025, 17, 596. [Google Scholar] [CrossRef]
- World Health Organization. Decade of Healthy Ageing: Baseline Report; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Eilat-Adar, S.; Sinai, T.; Yosefy, C.; Henkin, Y. Nutritional recommendations for cardiovascular disease prevention. Nutrients 2013, 5, 3646–3683. [Google Scholar] [CrossRef]
- Chareonrungrueangchai, K.; Wongkawinwoot, K.; Anothaisintawee, T.; Reutrakul, S. Dietary factors and risks of cardiovascular diseases: An Umbrella Review. Nutrients 2020, 12, 1088. [Google Scholar] [CrossRef]
- X World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective; World Cancer Research Fund International: London, UK, 2018. [Google Scholar]
- X World Health Organization/Food and Agricultural Organization. Diet, Nutrition and the Prevention of Chronic Diseases; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Madini, N.; Vincenti, A.; Beretta, A.; Santero, S.; Viroli, G.; Cena, H. Addressing inflammaging and disease-related malnutrition: Adequacy of oral nutritional supplements in clinical care. Nutrients 2024, 16, 4141. [Google Scholar] [CrossRef]
- Lesourd, B. Nutrition: A major factor influencing immunity in the elderly. J. Nutr. Health Aging 2004, 8, 28–37. [Google Scholar]
- Verlaan, S.; Ligthart-Melis, G.C.; Wijers, S.L.J.; Cederholm, T.; Maier, A.B.; de van der Schueren, M.A.E. High prevalence of physical frailty among community-dwelling malnourished older adults- a systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2017, 18, 374–382. [Google Scholar] [CrossRef]
- Wei, K.; Nyunt, M.S.Z.; Gao, Q.; Wee, S.L.; Ng, T.P. Frailty and malnutrition: Related and distinct syndrome prevalence and association among community-dwelling older adults: Singapore Longitudinal Ageing Studies. J. Am. Med. Dir. Assoc. 2017, 18, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Borda, M.G.; Ayala Copete, A.M.; Tovar-Rios, D.A.; Jaramillo-Jimenez, A.; Giil, L.M.; Soennesyn, H.; Gómez-Arteaga, C.; Venegas-Sanabria, L.C.; Kristiansen, I.; Chavarro-Carvajal, D.A.; et al. Association of malnutrition with functional and cognitive trajectories in people living with dementia: A Five-Year Follow-Up Study. J. Alzheimers Dis. 2021, 79, 1713–1722. [Google Scholar] [CrossRef] [PubMed]
- Feng, W.; Wang, J.; Zhang, H.; Wang, Y.; Sun, Z.; Chen, Y. Association between malnutrition and cognitive frailty in older adults: A systematic review and meta-analysis. Geriatr. Nurs. 2024, 58, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Mañas, L.; Murray, R.; Glencorse, C.; Sulo, S. Good nutrition across the lifespan is foundational for healthy aging and sustainable development. Front. Nutr. 2023, 9, 1113060. [Google Scholar] [CrossRef]
- de Souza Fernandes, D.P.; Duarte, M.S.L.; Pessoa, M.C.; Franceschini, S.D.C.C.; Ribeiro, A.Q. Evaluation of diet quality of the elderly and associated factors. Arch. Gerontol. Geriatr. 2017, 72, 174–180. [Google Scholar] [CrossRef]
- Irz, X.; Fratiglioni, L.; Kuosmanen, N.; Mazzocchi, M.; Modugno, L.; Nocella, G.; Shakersain, B.; Traill, W.B.; Xu, W.; Zanello, G. Sociodemographic determinants of diet quality of the EU elderly: A comparative analysis in four countries. Public Health Nutr. 2014, 17, 1177–1189. [Google Scholar] [CrossRef]
- Jomaa, L.; Hwalla, N.; Itani, L.; Chamieh, M.C.; Mehio-Sibai, A.; Naja, F. A Lebanese dietary pattern promotes better diet quality among older adults: Findings from a national cross-sectional study. BMC Geriatr. 2016, 16, 85. [Google Scholar] [CrossRef]
- Zhao, H.; Andreyeva, T. Diet quality and health in older Americans. Nutrients 2022, 14, 1198. [Google Scholar] [CrossRef]
- Agarwal, P.; Wang, Y.; Buchman, A.S.; Bennett, D.A.; Morris, M.C. Dietary patterns and self-reported incident disability in older adults. J. Gerontol. Ser. A 2019, 74, 1331–1337. [Google Scholar] [CrossRef]
- Puzianowska-Kuznicka, M.; Kurylowicz, A.; Walkiewicz, D.; Borkowska, J.; Owczarz, M.; Olszanecka-Glinianowicz, M.; Wieczorowska-Tobis, K.; Skalska, A.; Szybalska, A.; Mossakowska, M. Obesity paradox in Caucasian seniors: Results of the PolSenior Study. J. Nutr. Health Aging 2019, 23, 796–804. [Google Scholar] [CrossRef]
- Puzianowska-Kuznicka, M.; Kurylowicz, A.; Wierucki, L.; Owczarek, A.J.; Jagiello, K.; Mossakowska, M.; Zdrojewski, T.; Chudek, J. Obesity in Caucasian seniors on the rise: Is it truly harmful? Results of the PolSenior2 Study. Nutrients 2022, 14, 4621. [Google Scholar] [CrossRef] [PubMed]
- Krzyminska-Siemaszko, R.; Chudek, J.; Suwalska, A.; Lewandowicz, M.; Mossakowska, M.; Kroll-Balcerzak, R. Health status correlates of malnutrition in the polish elderly population—Results of the Polsenior Study. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 4565–4573. [Google Scholar] [PubMed]
- Quirk, S.; Williams, L.; O’Neil, A.; Pasco, J.; Jacka, F.; Housden, S.; Berk, M.; Brennan, S.L. The association between diet quality, dietary patterns and depression in adults: A systematic review. BMC Psychiatry 2013, 13, 175. [Google Scholar] [CrossRef] [PubMed]
- Masana, M.F.; Haro, J.M.; Mariolis, A.; Piscopo, S.; Valacchi, G.; Bountziouka, V.; Panagiotakos, D.B. Mediterranean diet and depression among older individuals: The multinational MEDIS study. Exp. Gerontol. 2018, 110, 67–72. [Google Scholar] [CrossRef]
- Ljungberg, T.; Bondza, E.; Lethin, C. Evidence of the importance of dietary habits regarding depressive symptoms and depression. Int. J. Environ. Res. Public Health 2020, 17, 1616. [Google Scholar] [CrossRef]
- Lai, J.S.; Hiles, S.; Bisquera, A.; Hure, A.J.; McEvoy, M.; Attia, J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am. J. Clin. Nutr. 2014, 99, 181–197. [Google Scholar] [CrossRef]
- Gomes, A.P.; Bierhals, I.O.; Hellwig, N.; Tomasi, E.; Assunção, M.F. Interrelationship between diet quality and depressive symptoms in elderly. J. Nutr. Health Aging 2018, 22, 387–392. [Google Scholar] [CrossRef]
- Jacka, F.N.; Cherbuin, N.; Anstey, K.J.; Butterworth, P. Does reverse causality explain the relationship between diet and depression? J. Affect. Disord. 2015, 175, 248–250. [Google Scholar] [CrossRef]
- Payne, M.E.; Steck, S.E.; George, R.R.; Steffens, D.C. Fruit, vegetable, and antioxidant intakes are lower in older adults with depression. J. Acad. Nutr. Diet. 2012, 112, 2022–2027. [Google Scholar] [CrossRef]
- Elstgeest, L.E.; Winkens, L.H.; Penninx, B.W.; Brouwer, I.A.; Visser, M. Associations of depressive symptoms and history with three a priori diet quality indices in middle-aged and older adults. J. Affect. Disord. 2019, 249, 394–403. [Google Scholar] [CrossRef]
- Fostinelli, S.; De Amicis, R.; Leone, A.; Giustizieri, V.; Binetti, G.; Bertoli, S.; Cappa, S.F. Eating behavior in aging and dementia: The need for a comprehensive assessment. Front. Nutr. 2020, 7, 604488. [Google Scholar] [CrossRef] [PubMed]
- Buchman, A.S.; Wilson, R.S.; Bienias, J.L.; Shah, R.C.; Evans, D.A.; Bennett, D.A. Change in body mass index and risk of incident Alzheimer disease. Neurology 2005, 65, 892–897. [Google Scholar] [CrossRef] [PubMed]
- Bamford, S.M.; Walker, T. Women and dementia—Not forgotten. Maturitas 2012, 73, 121–126. [Google Scholar] [CrossRef]
- Fletcher, J.R. Structuring unequal relations: Role trajectories in informal dementia care. Sociol. Health Illn. 2021, 43, 65–81. [Google Scholar] [CrossRef]
- Kodama, S.; Hoshi, T.; Kurimori, S. Decline in independence after three years and its association with dietary patterns and IADL-related factors in community-dwelling older people: An analysis by age stage and sex. BMC Geriatr. 2021, 21, 385. [Google Scholar] [CrossRef]
- Hsiao, F.Y.; Peng, L.N.; Lee, W.J.; Chen, L.K. Higher dietary diversity and better healthy aging: A 4-year study of community-dwelling middle-aged and older adults from the Taiwan Longitudinal Study of Aging. Exp. Gerontol. 2022, 168, 111929. [Google Scholar] [CrossRef] [PubMed]
- Laclaustra, M.; Rodriguez-Artalejo, F.; Guallar-Castillon, P.; Banegas, J.R.; Graciani, A.; Garcia-Esquinas, E.; Lopez-Garcia, E. The inflammatory potential of diet is related to incident frailty and slow walking in older adults. Clin. Nutr. 2020, 39, 185–191. [Google Scholar] [CrossRef]
- Kiesswetter, E.; Poggiogalle, E.; Migliaccio, S.; Donini, L.M.; Sulmont-Rossé, C.; Feart, C.; Volkert, D. Functional determinants of dietary intake in community-dwelling older adults: A DEDIPAC (DEterminants of DIet and Physical ACtivity) systematic literature review. Public Health Nutr. 2018, 21, 1886–1903. [Google Scholar] [CrossRef]
- Zelig, R.; Goldstein, S.; Touger-Decker, R.; Firestone, E.; Golden, A.; Johnson, Z.; Kaseta, A.; Sackey, J.; Tomesko, J.; Parrott, J. Tooth loss and nutritional status in older adults: A systematic review and meta-analysis. JDR Clin. Trans. Res. 2020, 7, 4–15. [Google Scholar] [CrossRef]
- Iwasaki, M.; Yoshihara, A.; Ogawa, H.; Sato, M.; Muramatsu, K.; Watanabe, R.; Ansai, T.; Miyazaki, H. Longitudinal association of dentition status with dietary intake in Japanese adults aged 75 to 80 years. J. Oral Rehab. 2016, 43, 737–744. [Google Scholar] [CrossRef]
- Kotronia, E.; Brown, H.; Papacosta, A.O.; Lennon, L.T.; Weyant, R.J.; Whincup, P.H.; Wannamethee, S.G.; Ramsay, S.E. Poor oral health and the association with diet quality and intake in older people in two studies in the UK and USA. Br. J. Nutr. 2021, 126, 118–130. [Google Scholar] [CrossRef] [PubMed]
- Ervin, R.B.; Dye, B.A. The effect of functional dentition on Healthy Eating Index scores and nutrient intakes in a nationally representative sample of older adults. J. Public Health Dent. 2009, 69, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Gaewkhiew, P.; Sabbah, W.; Bernabé, E. Functional dentition and changes in dietary patterns among older adults in Thailand. Public Health Nutr. 2021, 24, 4556–4563. [Google Scholar] [CrossRef] [PubMed]
| Index Component | Components for Maximum Score (i.e., 10) | Mean Score (95% CI) | Proportion Meeting Recommendation (%, 95% CI) | |
|---|---|---|---|---|
| 1. | Vegetables | daily frequency of consumption ≥ 3 | 6.4 (6.3–6.6) | 26.7 (24.4–29) |
| 2. | Fruit | daily frequency of consumption ≥ 2 | 6.0 (5.9–6.2) | 32.9 (30.3–35.5) |
| 3. | Protein | daily frequency of consumption ≥ 3 | 8.3 (8.2–8.4) | 50.2 (48.2–52.2) |
| 4. | Fish | weekly frequency of consumption ≥ 1 | 7.2 (7.1–7.4) | 62.2 (59.9–64.6) |
| 5. | Low-fat dairy | daily frequency of consumption ≥ 3 | 2.5 (2.4–2.6) | 1.0 (0.7–1.3) |
| 6. | Wholegrain carbohydrates | daily frequency of consumption ≥ 3 | 2.1 (2–2.2) | 1.9 (1.4–2.5) |
| 7. | Free sugars | daily frequency of consumption ≤ 1 | - * | 36.1 (33.6–38.5) |
| 8. | Fats | 100% unsaturated consumed | 3.1 (2.9–3.2) | 0.9 (0.5–1.4) |
| 9. | Fluids | ≥1500 mL per day | 9.4 (9.3–9.5) | 75.8 (73.7–77.9) |
| 10. | Alcohol | weekly frequency of consumption ≤ 1 | - * | 93.6 (92.6–94.5) |
| Total (N = 5604) | Adherence to SHDI | p-Value | ||
|---|---|---|---|---|
| Lower (0–4 Components) (n = 3103) | Higher (≥5 Components) (n = 2501) | |||
| Total, % | 55.4 | 44.6 | ||
| Women, % | 50.7 | 48.0 | 54.1 | <0.001 |
| Men, % | 49.3 | 52.0 | 45.9 | |
| Age, years | 74.8 ± 9.4 | 75.7 ± 9.7 | 73.6 ± 8.9 | <0.001 |
| Age category, % | ||||
| 60–79 years | 67.9 | 63.8 | 73.0 | <0.001 |
| 80 and more years | 32.1 | 36.2 | 27.0 | |
| Living alone, % | 21.1 | 21.5 | 20.6 | <0.05 |
| Marital status, % | ||||
| In a relationship | 61.0 | 59.2 | 63.3 | <0.01 |
| Single (divorced, widower, never married) | 39.0 | 40.8 | 36.7 | |
| Place of residence, % | ||||
| Rural | 35.2 | 38.1 | 31.7 | <0.001 |
| Urban | 64.8 | 61.9 | 68.3 | |
| Education, % | ||||
| Primary or less/basic vocational | 53.0 | 57.3 | 47.8 | <0.001 |
| Secondary/post-secondary/higher | 47.0 | 42.7 | 52.2 | |
| Type of work, % | ||||
| Blue collar/farmer | 63.2 | 66.3 | 59.4 | <0.001 |
| White collar | 34.8 | 31.9 | 38.4 | |
| Economic status, % | ||||
| Can afford everything without saving money | 18.9 | 18.1 | 19.9 | <0.05 |
| Living modestly to be able to afford daily expenses | 74.0 | 74.2 | 73.8 | |
| Money is only enough for the cheapest food, or even less | 7.1 | 7.7 | 6.3 | |
| Current or past smoker, % | 50.9 | 52.0 | 49.6 | 0.074 |
| Physical activity, % | ||||
| Meets ACSM criteria | 33.7 | 31.2 | 36.9 | <0.001 |
| Total (N = 5604) | Adherence to SHDI | p-Value | ||
|---|---|---|---|---|
| Lower (0–4 Components) (n = 3103) | Higher (≥5 Components) (n = 2501) | |||
| IADL, % | ||||
| Highly functional (24 pts) | 34.2 | 61.6 | 71.0 | <0.001 |
| Partially disabled or disabled (≤23 pts) | 65.8 | 38.4 | 29.0 | |
| Depression, % | 26.2 | 29.7 | 22.1 | <0.001 |
| Cognitive impairment, % | ||||
| Without | 52.7 | 48.2 | 58.2 | <0.001 |
| MCI | 22.7 | 23.0 | 22.5 | |
| Dementia | 24.6 | 28.8 | 19.3 | |
| Falls, % | 19.0 | 20.4 | 17.3 | <0.01 |
| Frailty, % | 22.6 | 21.5 | 19.5 | <0.001 |
| Vision impairment, % | 46.4 | 48.1 | 44.3 | <0.01 |
| Constipation, % | 9.4 | 10.2 | 8.4 | <0.05 |
| Dentition, % | ||||
| Functional dentition (≥20 teeth) | 15.4 | 13.1 | 18.3 | <0.001 |
| Partial edentulism (1–19 teeth) | 48.2 | 47.9 | 48.7 | |
| Complete edentulism | 36.4 | 39.0 | 33.1 | |
| Dentures, % (only in the group with <20 teeth) | ||||
| Used | 81.7 | 80.6 | 83.2 | <0.05 |
| Not used | 18.3 | 19.4 | 16.8 | |
| BMI category, % | ||||
| Normal/overweight (18.5–29.9 kg/m2) | 63.3 | 64.7 | 61.6 | <0.01 |
| Obesity (≥30 kg/m2) | 35.8 | 34.2 | 37.8 | |
| MNA nutritional status, % | ||||
| Good | 71.7 | 69.9 | 73.9 | <0.001 |
| Risk of malnutrition or malnutrition | 28.3 | 30.1 | 26.1 | |
| Heart failure, % | 21.0 | 20.7 | 21.2 | 0.661 |
| Hypertension, % | 77.2 | 76.4 | 78.2 | 0.089 |
| Past stroke, % | 9.0 | 9.3 | 8.7 | 0.475 |
| Diabetes, % | 25.7 | 23.4 | 28.5 | <0.001 |
| Hypercholesterolemia, % | 75.8 | 75.2 | 76.5 | 0.265 |
| Women Adherence to SHDI | Men Adherence to SHDI | |||||
|---|---|---|---|---|---|---|
| Lower (0–4 Components) (n= 1488) | Higher (≥5 Components) (n = 1353) | p-Value | Lower (0–4 Components) (n= 1615) | Higher (≥5 Components) (n = 1148) | p-Value | |
| Age, years | 75.9 ± 9.7 | 72.9 ± 8.7 | <0.001 | 75.5 ± 9.6 | 74.2 ± 9.4 | <0.001 |
| Age category, % | ||||||
| 60–79 years | 61.8 | 75.1 | <0.001 | 65.8 | 70.6 | <0.01 |
| 80 and more years | 38.2 | 24.9 | 34.2 | 29.4 | ||
| Living alone, % | 30.5 | 27.8 | 0.121 | 13.2 | 12.1 | 0.417 |
| Marital status, % | ||||||
| In a relationship | 39.5 | 49.5 | <0.001 | 77.4 | 79.4 | 0.200 |
| Single (divorced, widower, never married) | 60.5 | 50.5 | 22.6 | 20.6 | ||
| Place of residence, % | ||||||
| Rural | 39.2 | 31.5 | <0.001 | 37.0 | 32.0 | <0.01 |
| Urban | 60.8 | 68.5 | 63.0 | 68.0 | ||
| Education, % | ||||||
| Primary or less/basic vocational | 57.1 | 45.5 | <0.001 | 57.2 | 50.4 | <0.001 |
| Secondary/post-secondary/higher | 42.9 | 54.5 | 42.5 | 49.6 | ||
| Type of work, % | ||||||
| Blue collar/farmer | 60.3 | 53.4 | <0.01 | 71.7 | 66.4 | <0.05 |
| White collar | 37.7 | 44.2 | 26.7 | 31.8 | ||
| Economic status, % | ||||||
| Can afford everything without saving money | 14.7 | 16.6 | 0.137 | 21.2 | 23.8 | 0.108 |
| Living modestly to be able to afford daily expenses | 75.9 | 75.7 | 72.7 | 71.5 | ||
| Money is only enough for the cheapest food, or even less | 9.4 | 7.7 | 6.1 | 4.7 | ||
| IADL, % | ||||||
| Highly functional (24 pts) | 59.7 | 72.5 | <0.001 | 36.6 | 30.8 | <0.01 |
| Partially disabled or disabled (23 and less pts) | 40.3 | 27.5 | 63.4 | 69.2 | ||
| Depression, % | 34.4 | 24.3 | <0.001 | 25.5 | 19.6 | <0.001 |
| Cognitive impairment, % | ||||||
| Without | 45.3 | 58.7 | <0.001 | 50.9 | 57.5 | <0.001 |
| MCI | 23.2 | 22.4 | 22.7 | 22.6 | ||
| Dementia | 31.5 | 18.8 | 26.4 | 19.9 | ||
| Falls, % | 24.8 | 21.0 | <0.05 | 16.3 | 12.9 | <0.05 |
| Frailty, % | 27.3 | 17.6 | <0.001 | 23.0 | 21.8 | 0.761 |
| Vision impairment, % | 49.8 | 42.5 | <0.001 | 46.6 | 46.5 | 0.934 |
| Constipation, % | 13.1 | 10.6 | <0.001 | 7.5 | 9.1 | 0.128 |
| Dentition, % | ||||||
| Functional dentition (≥20 teeth) | 11.6 | 18.2 | <0.001 | 14.4 | 18.4 | <0.01 |
| Partial edentulism (1–19 teeth) | 45.5 | 46.5 | 50.2 | 51.3 | ||
| Complete edentulism | 42.9 | 35.3 | 35.4 | 30.4 | ||
| Dentures (only in group with less than 20 teeth), % | ||||||
| Used | 86.0 | 88.2 | 0.131 | 75.4 | 77.1 | 0.376 |
| Not used | 14.0 | 11.8 | 24.6 | 22.9 | ||
| BMI category, % | ||||||
| Normal/overweight 18.5–29.9 kg/m2) | 60.0 | 59.1 | 0.102 | 69.1 | 64.6 | <0.05 |
| Obesity (≥30 kg/m2) | 38.7 | 40.4 | 30.1 | 34.7 | ||
| Nutritional status—MNA, % | ||||||
| Good | 65.5 | 72.1 | <0.001 | 74.0 | 76.1 | 0.213 |
| Risk of malnutrition/malnutrition | 34.5 | 27.9 | 26.0 | 23.9 | ||
| Heart failure, % | 19.0 | 17.3 | 0.250 | 22.4 | 25.9 | <0.05 |
| Hypertension, % | 77.5 | 77.3 | 0.856 | 75.3 | 79.5 | <0.01 |
| Past stroke, % | 8.8 | 6.8 | <0.05 | 9.7 | 11.0 | 0.267 |
| Diabetes, % | 21.8 | 24.9 | 0.154 | 24.9 | 32.8 | <0.001 |
| Hypercholesterolemia, % | 79.4 | 80.0 | 0.705 | 71.4 | 72.4 | 0.553 |
| Current or past smoker, % | 33.0 | 35.8 | 0.119 | 69.4 | 65.8 | <0.05 |
| Physical activity, % | ||||||
| who meet ACSM criteria | 26.7 | 34.3 | <0.001 | 35.3 | 40.0 | <0.05 |
| OR * | Lower CI | Higher CI | p-Value | |
|---|---|---|---|---|
| Men | 0.67 | 0.58 | 0.78 | <0.001 |
| Age 60–79 | 1.13 | 0.95 | 1.36 | 0.18 |
| In relationship | 1.06 | 0.91 | 1.24 | 0.45 |
| Living in an urban area | 1.15 | 0.99 | 1.33 | 0.07 |
| Education (secondary/higher) | 1.32 | 1.09 | 1.60 | <0.01 |
| White collar | 0.86 | 0.71 | 1.05 | 0.14 |
| Highly independent (IADL 24 pts) | 1.07 | 0.88 | 1.29 | 0.48 |
| BMI 18.5–29.9 kg/m2 | 0.92 | 0.79 | 1.06 | 0.24 |
| Malnutrition/ at risk of malnutrition | 1.26 | 1.04 | 1.53 | 0.02 |
| Depression | 0.67 | 0.56 | 0.81 | <0.001 |
| Mild cognitive impairment | 1.12 | 0.90 | 1.40 | 0.30 |
| Dementia | 0.75 | 0.61 | 0.93 | 0.01 |
| No falls | 1.06 | 0.88 | 1.29 | 0.52 |
| Pre-frail | 0.91 | 0.73 | 1.14 | 0.42 |
| Robust | 0.87 | 0.66 | 1.13 | 0.28 |
| Good vision | 0.99 | 0.86 | 1.13 | 0.85 |
| No constipation | 1.18 | 0.91 | 1.52 | 0.21 |
| Partial edentulism | 1.08 | 0.93 | 1.26 | 0.33 |
| Functional dentition | 1.45 | 1.16 | 1.80 | <0.01 |
| Prediabetes | 0.73 | 0.60 | 0.89 | <0.01 |
| Diabetes | 1.47 | 1.25 | 1.75 | <0.001 |
| Meets ACSM criteria | 1.22 | 1.06 | 1.42 | <0.01 |
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | Lower CI | Higher CI | p-Value | OR | Lower CI | Higher CI | p-Value | |
| Age 60–79 | 1.25 | 0.96 | 1.64 | 0.10 | 0.99 | 0.78 | 1.26 | 0.93 |
| In relationship | 1.11 | 0.90 | 1.36 | 0.33 | ||||
| Living in an urban area | 1.15 | 0.92 | 1.42 | 0.21 | 1.27 | 1.04 | 1.56 | 0.02 |
| Education (secondary/higher) | 1.62 | 1.19 | 2.20 | <0.01 | 1.19 | 0.94 | 1.51 | 0.16 |
| White collar | 0.66 | 0.49 | 0.90 | <0.01 | 0.96 | 0.75 | 1.24 | 0.75 |
| Highly independent (IADL 24 pts) | 1.08 | 0.82 | 1.42 | 0.59 | 0.98 | 0.77 | 1.24 | 0.86 |
| BMI 18.5–29.9 kg/m2 | NI * | 0.82 | 0.67 | 1.00 | 0.05 | |||
| Malnutrition/at risk of malnutrition | 1.49 | 1.14 | 1.96 | <0.01 | ||||
| Depression | 0.65 | 0.51 | 0.84 | <0.01 | 0.79 | 0.63 | 1.00 | 0.05 |
| Mild cognitive impairment | 1.09 | 0.80 | 1.49 | 0.60 | 1.02 | 0.76 | 1.37 | 0.90 |
| Dementia | 0.72 | 0.53 | 0.98 | 0.03 | 0.89 | 0.67 | 1.18 | 0.43 |
| No falls | 0.93 | 0.73 | 1.19 | 0.56 | 1.27 | 0.95 | 1.70 | 0.11 |
| Pre-frail | 1.15 | 0.85 | 1.57 | 0.36 | NI * | |||
| Robust | 1.16 | 0.80 | 1.69 | 0.44 | NI * | |||
| Good vision | 1.18 | 0.96 | 1.43 | 0.11 | NI * | |||
| No constipation | 1.82 | 1.29 | 2.58 | <0.001 | NI * | |||
| Partial edentulism | 0.97 | 0.78 | 1.21 | 0.80 | 1.19 | 0.96 | 1.47 | 0.11 |
| Functional dentition | 1.40 | 1.02 | 1.93 | 0.04 | 1.36 | 1.01 | 1.82 | 0.04 |
| Prediabetes | 0.75 | 0.56 | 1.01 | 0.06 | 0.75 | 0.58 | 0.96 | 0.02 |
| Diabetes | 1.33 | 1.05 | 1.69 | 0.02 | 1.47 | 1.16 | 1.85 | <0.01 |
| Heart failure | NI * | 1.30 | 1.04 | 1.61 | 0.02 | |||
| Hypertension | NI * | 1.28 | 1.61 | 1.02 | 0.03 | |||
| Meets ACSM criteria | 1.15 | 0.93 | 1.42 | 0.21 | 1.26 | 1.04 | 1.52 | 0.02 |
| No smoking (present or past) | NI * | 1.23 | 1.00 | 1.50 | 0.05 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kujawska-Danecka, H.; Dardzińska, J.A.; Mossakowska, M.; Puzianowska-Kuźnicka, M.; Kaluźniak-Szymanowska, A.; Małgorzewicz, S.; Wernio, E.; Chudek, J. Socioeconomic and Health-Related Determinants of Eating Habits in Polish Caucasian Older Population—The Nationwide PolSenior2 Study Results. Nutrients 2025, 17, 1640. https://doi.org/10.3390/nu17101640
Kujawska-Danecka H, Dardzińska JA, Mossakowska M, Puzianowska-Kuźnicka M, Kaluźniak-Szymanowska A, Małgorzewicz S, Wernio E, Chudek J. Socioeconomic and Health-Related Determinants of Eating Habits in Polish Caucasian Older Population—The Nationwide PolSenior2 Study Results. Nutrients. 2025; 17(10):1640. https://doi.org/10.3390/nu17101640
Chicago/Turabian StyleKujawska-Danecka, Hanna, Jolanta A. Dardzińska, Małgorzata Mossakowska, Monika Puzianowska-Kuźnicka, Aleksandra Kaluźniak-Szymanowska, Sylwia Małgorzewicz, Edyta Wernio, and Jerzy Chudek. 2025. "Socioeconomic and Health-Related Determinants of Eating Habits in Polish Caucasian Older Population—The Nationwide PolSenior2 Study Results" Nutrients 17, no. 10: 1640. https://doi.org/10.3390/nu17101640
APA StyleKujawska-Danecka, H., Dardzińska, J. A., Mossakowska, M., Puzianowska-Kuźnicka, M., Kaluźniak-Szymanowska, A., Małgorzewicz, S., Wernio, E., & Chudek, J. (2025). Socioeconomic and Health-Related Determinants of Eating Habits in Polish Caucasian Older Population—The Nationwide PolSenior2 Study Results. Nutrients, 17(10), 1640. https://doi.org/10.3390/nu17101640






