Choline in Pediatric Nutrition: Assessing Formula, Fortifiers and Supplements Across Age Groups and Clinical Indications
Abstract
1. Introduction
1.1. Essential Nature of Choline
1.2. Choline Concentrations and Metabolism
1.3. Choline Function and Organotypic Metabolism
1.4. Choline in Nutrition
1.5. Aim of Study
2. Materials and Methods
2.1. Study Design
2.2. Sample Collection
2.3. Sample Characterization
2.4. Statistics
3. Results
3.1. Energy
3.2. Macronutrients
3.3. Choline
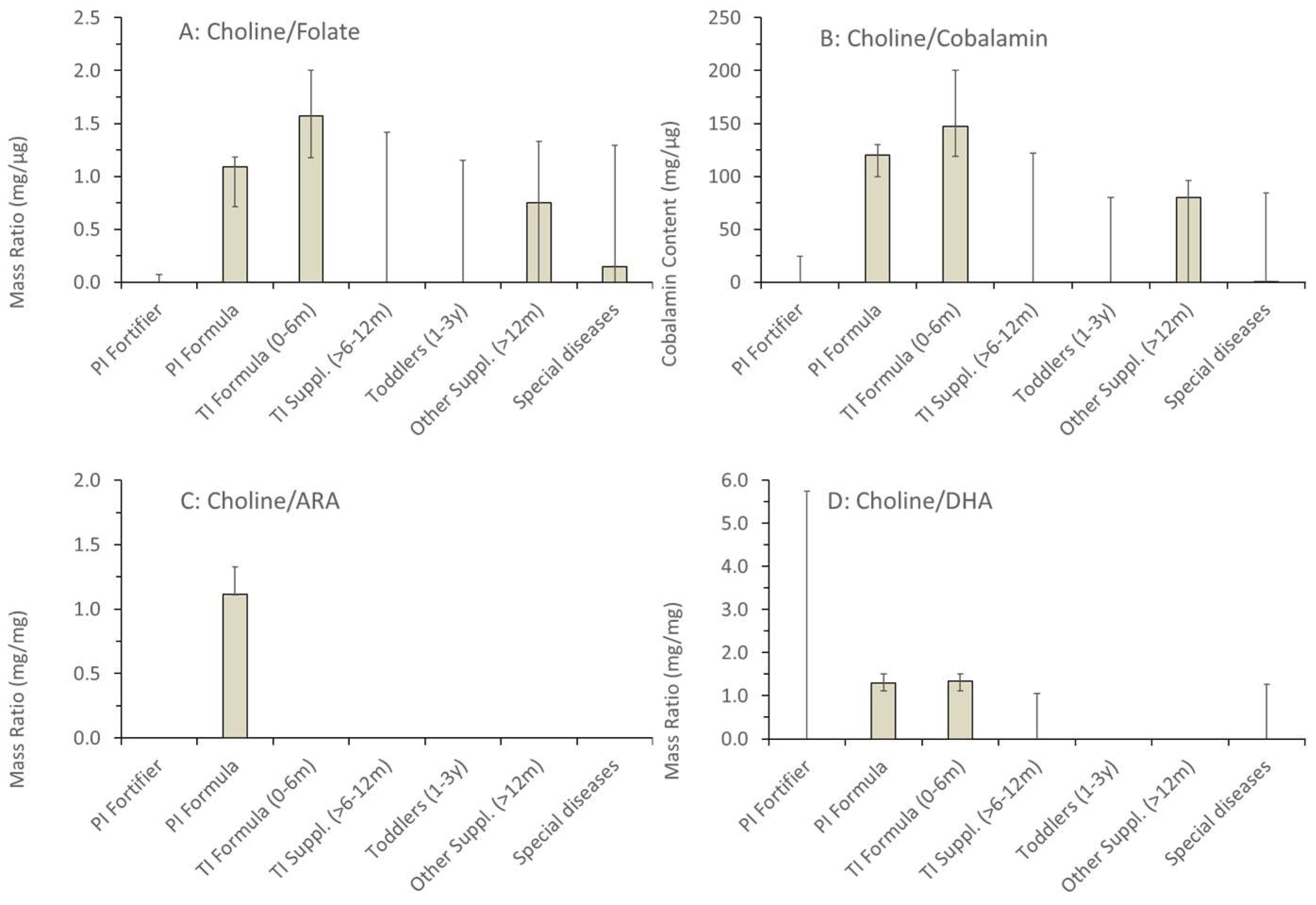
3.4. Choline Related Nutrients: Folate, Cobalamin and Long-Chain Polyunsaturated Fatty Acids
4. Discussion
4.1. Balance and Imbalance of Choline Compared to Other Nutrients
4.2. The Indicated Choline Content May Not Match the Actual Amount in the Products
4.3. Clinical Suggestions for Product Choice
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
Appendix A
| Product Name, Producer | Choline Concentration (mg/100 kcal) | Added Choline Compound |
|---|---|---|
| Preterm Infant Fortifier | ||
| BEBA FM 85, Nestlé * | 17.3 | Not specified |
| Humavant+4, Prolacta | 0 | ∅ |
| Aptamil FMS, Nutricia | 0 | ∅ |
| Preterm Infant Formula | ||
| 0-HP-1 Expert, Humana | 38.6 | Choline bitartrate |
| 0-HP-2, Humana | 46.8 | Choline bitartrate |
| Alphare HMO, Nestlé | 29.9 | Choline bitartrate |
| BEBA expert pro Comfort, Nestlé | 33.3 | Choline bitartrate |
| BEBA FG 1, Nestlé | 25.0 | Choline bitartrate |
| Nestlé | 20.5 | Choline bitartrate |
| Aptamil HA Pre, Nutricia | 33.3 | Choline chloride |
| Aptamil PDF, Nutricia | 31.9 | Choline chloride |
| Aptamil Prematil, Nutricia | 32.5 | Choline chloride |
| Aptamil Prematil HA, Nutricia | 32.5 | Choline chloride |
| Monogen, Nutricia | 23.0 | Choline chloride |
| Term Infant Formula 0–6 months | ||
| Bebivita-PRE HA, Bebivita | 37.9 | Not specified |
| Bebivita 1 Anfangsmilch, Bebivita | 38.8 | Not specified |
| Bio Combiotic PRE, Hipp | 37.9 | Not specified |
| HA Combiotic PRE-HA, Hipp | 37.9 | Not specified |
| Bio Combiotic 1, Hipp | 38.8 | Not specified |
| HiPP Comfort, Hipp | 37.9 | Not specified |
| Humana Anfangsmilch pre, Humana | 30.8 | Choline bitartrate |
| Humana Anfangsmilch 1, Humana | 37.3 | Choline bitartrate |
| kendamil first instant milk, Kendamil | 32.8 | Choline bitartrate |
| Kendamil first organic, Kendamil | 30.3 | Choline bitartrate |
| Kendamil first goat, Kendamil | 32.8 | Choline bitartrate |
| Milumil Pre Anfangsmilch, Milupa | 36.4 | Choline chloride |
| Milumil 1 Anfangsmilch, Milupa | 32.4 | Choline chloride |
| Alfaré, Nestlé | 29.9 | Choline bitartrate |
| Alphare HMO, Nestlé | 29.9 | Choline bitartrate |
| BEBA EXPERT HA 1, Nestlé | 35.2 | Choline bitartrate |
| BEBA Optipro PRE, Nestlé | 30.8 | Choline bitartrate |
| BEBA Optipro 1, Nestlé | 30.7 | Choline bitartrate |
| BEBA Supreme Pre, Nestlé | 34.3 | Choline bitartrate |
| BEBA Supreme 1, Nestlé | 34.2 | Choline bitartrate |
| Aptamil Care Pre, Nutricia | 34.8 | Choline chloride |
| Aptamil Comfort, Nutricia | 33.3 | Choline chloride |
| Aptamil Organic PRE, Nutricia | 33.3 | Not specified |
| Aptamil Pronutra Pre, Nutricia | 33.3 | Choline chloride |
| Aptamil Pregomin, Nutricia | 28.8 | Choline chloride |
| Aptamil Pregomin AS, Nutricia | 28.0 | Choline bitartrate |
| Aptamil FMS, Nutricia | 0 | ∅ |
| Aptamil Anti Reflux, Nutricia | 33.3 | Choline chloride |
| Aptamil Care Pre, Nutricia | 34.8 | Choline chloride |
| Aptamil Bio PRE, Nutricia | 33.3 | Choline chloride |
| Aptamil Organic PRE, Nutricia | 33.3 | Not specified |
| Aptamil Organic 1, Nutricia | 33.3 | Choline chloride |
| Monogen, Nutricia | 23.0 | Choline chloride |
| Neocate Syneo, Nutricia | 27.9 | Not specified |
| Neocate Infant, Nutricia | 27.6 | Not specified |
| Holle Bio Pre, Holle | 33.3 | Choline bitartrate |
| Bio-Anfangsmilch, Holle | 33.8 | Choline bitartrate |
| Bio-Anfangsmilch 1, Holle | 33.3 | Choline bitartrate |
| Bio-Anfangsmilch 1 (from goat milk) | 32.4 | Choline bitartrate |
| Term Infants 6–12 months | ||
| Bebivita 2 Folgemilch, Bebivita | 0 | ∅ |
| Bio Combiotic 2, Hipp | 0 | ∅ |
| HiPP Bio Ziegenmilch 2, Hipp | 0 | ∅ |
| Humana Folgemilch 2, Humana | 37.3 | Choline bitartrate |
| Humana Folgemilch 3, Humana | 37.3 | Choline bitartrate |
| Follow-on milk, Kendamil | 32.8 | Choline bitartrate |
| kendamil goat, Kendamil | 24.2 | Choline bitartrate |
| Milumil 2 Folgemilch, Milupa | 25.0 | Choline chloride |
| Milumil 3 Folgemilch, Milupa | 25.0 | Choline chloride |
| BEBA Optipro 2, Nestlé | 0 | ∅ |
| BEBA Supreme 2, Nestlé | 0 | ∅ |
| BEBA Supreme 3, Nestlé | 0 | ∅ |
| BEBA EXPERT HA 2, Nestlé | 0 | ∅ |
| Aptamil Bio 2, Nutricia | 0 | ∅ |
| Humana Kindergetränk 1+, Humana | 0 | ∅ |
| Toddler milk, Kendamil | 0 | ∅ |
| Toddler milk Organic, Kendamil | 0 | ∅ |
| BEBA EXPERT HA 3, Nestlé | 0 | ∅ |
| BEBA Junior 12–36, Nestlé | 0 | ∅ |
| Aptamil Profutura DUOADVANCE 2, Nutricia | 22.1 | Choline chloride |
| Neocate Junior, Nutricia | 20.0 | Not specified |
| Nutrini Multi Fibre, Nutricia | 20.0 | Not specified |
| Product Name, Producer | Choline Concentration (mg/100 kcal) | Added Choline Compound |
|---|---|---|
| RCF, Abbott * | 12 | Not specified |
| Calshake, Fresenius KABI | 0 | ∅ |
| Fresubin 5kcal Shot, Fresenius KABI | 0 | ∅ |
| Comfort Spezialnahrung (Opstipation, lactose intolerance of infants) | 37.9 | Not specified |
| Energea Pkid, MetaX | 0 | ∅ |
| Energea P, MetaX | 0 | ∅ |
| Maltocal 19, MetaX | 0 | ∅ |
| Nephea Infant (Kidney Disease), MetaX | 0 | ∅ |
| Nephea Kid (Kidney Disease), MetaX | 0 | ∅ |
| Alphamino, Nestlé | 34.3 | Choline bitartrate |
| Althera (Cow milk allergie), Nestlé | 28.8 | Choline bitartrate |
| Beba Anti Reflux, Nestlé | 31.3 | Choline bitartrate |
| Modulen IBD (Crohn’s Disease), Nestlé | 7.1 | Choline bitartrate |
| Peptamen (Tube feeding), Nestlé | 21 | Choline chloride |
| Peptamen Junior Advance (high energy tube feed), Nestlé | 16 | Choline chloride |
| Aptamil Eiweiß +, Nutricia | 0 | ∅ |
| Aptamil PDF, Nutricia | 31.9 | Choline chloride |
| Duocal, Nutricia (Cachexia) | 0 | ∅ |
| Heparon Junior, Nutricia (Liver disease) | 24.7 | Choline chloride |
| Fortimel Joghurt style, Nutricia | 36.7 | Choline chloride |
| Fortimel Pulver Neutral, Nutricia | 33.1 | Choline chloride |
| Neocate® Junior, Nutricia | 20 | Choline bitartrate |
| Infatrini 125 mL, Nutricia | 31.3 | Choline chloride |
| Infatrini Peptisorb, Nutricia | 32.1 | Choline chloride |
| Nutrini Multi Fibre, Nutricia | 20 | Choline chloride |
| NutriniDrink Smoothie, Nutricia | 19.8 | Choline chloride |
| NutriniDrink Compact Multi Fibre, Nutricia | 20 | Choline chloride |
| Nutrini creamy, Nutricia | 20 | Choline chloride |
| restoric® nephro prae, Vitasyn medical | 0 | ∅ |
| restoric® supportiv S (Malnutrition), Vitasyn medical | 0 | ∅ |
Appendix B
References
- Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes and its Panel on Folate, Other B Vitamins, and Choline. In Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline; National Academies Press: Washington, DC, USA, 1998. [PubMed]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Dietary Reference Values for choline. EFSA J. 2016, 14, 4484. [Google Scholar] [CrossRef]
- Pynn, C.J.; Henderson, N.G.; Clark, H.; Koster, G.; Bernhard, W.; Postle, A.D. Specificity and rate of human and mouse liver and plasma phosphatidylcholine synthesis analyzed in vivo. J. Lipid Res. 2011, 52, 399–407. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bernhard, W. Choline in cystic fibrosis: Relations to pancreas insufficiency, enterohepatic cycle, PEMT and intestinal microbiota. Eur. J. Nutr. 2021, 60, 1737–1759. [Google Scholar] [CrossRef] [PubMed]
- Böckmann, K.A.; Bernhard, W.; Minarski, M.; Shunova, A.; Wiechers, C.; Poets, C.F.; Franz, A.R. Choline supplementation for preterm infants: Metabolism of four Deuterium-labeled choline compounds. Eur. J. Nutr. 2023, 62, 1195–1205. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bernhard, W.; Shunova, A.; Boriga, J.; Graepler-Mainka, U.; Hilberath, J. Low Plasma Choline in Cystic Fibrosis Patients Is Linked to Exocrine Pancreatic Insufficiency and Small Intestinal Bacterial Overgrowth. Nutrients 2025, 17, 868. [Google Scholar] [CrossRef]
- Song, J.; da Costa, K.A.; Fischer, L.M.; Kohlmeier, M.; Kwock, L.; Wang, S.; Zeisel, S.H. Polymorphism of the PEMT gene and susceptibility to nonalcoholic fatty liver disease (NAFLD). FASEB J. 2005, 19, 1266–1271. [Google Scholar] [CrossRef]
- EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA). Choline and contribution to normal liver function of the foetus and exclusively breastfed infants: Evaluation of a health claim pursuant to Article 14 of Regulation (EC) No 1924/2006. EFSA J. 2023, 21, 8115. [Google Scholar]
- Bernhard, W.; Lange, R.; Graepler-Mainka, U.; Engel, C.; Machann, J.; Hund, V.; Shunova, A.; Hector, A.; Riethmüller, J. Choline Supplementation in Cystic Fibrosis-The Metabolic and Clinical Impact. Nutrients 2019, 11, 656. [Google Scholar] [CrossRef]
- Buchman, A.L.; Dubin, M.; Jenden, D.; Moukarzel, A.; Roch, M.H.; Rice, K.; Gornbein, J.; Ament, M.E.; Eckhert, C.D. Lecithin increases plasma free choline and decreases hepatic steatosis in long-term total parenteral nutrition patients. Gastroenterology 1992, 102, 1363–1370. [Google Scholar] [CrossRef]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) Scientific Opinion on the substantiation of health claims related to betaine and contribution to normal homocysteine metabolism (ID 4325) pursuant to Article 13(1) of Regulation (EC) No 1924/2006. EFSA J. 2011, 9, 2052. [CrossRef]
- Bernhard, W.; Böckmann, K.A.; Minarski, M.; Wiechers, C.; Busch, A.; Bach, D.; Poets, C.F.; Franz, A.R. Evidence and Perspectives for Choline Supplementation during Parenteral Nutrition-A Narrative Review. Nutrients 2024, 16, 1873. [Google Scholar] [CrossRef] [PubMed]
- Buchman, A. The addition of choline to parenteral nutrition. Gastroenterology 2009, 137 (Suppl. 5), S119–S128. [Google Scholar] [CrossRef] [PubMed]
- Kumpf, V.J. Parenteral nutrition-associated liver disease in adult and pediatric patients. Nutr. Clin. Pract. 2006, 21, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Obeid, R.; Schön, C.; Derbyshire, E.; Jiang, X.; Mellott, T.J.; Blusztajn, J.K.; Zeisel, S.H. A Narrative Review on Maternal Choline Intake and Liver Function of the Fetus and the Infant; Implications for Research, Policy, and Practice. Nutrients 2024, 16, 260. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jaiswal, A.; Dewani, D.; Reddy, L.S.; Patel, A. Choline Supplementation in Pregnancy: Current Evidence and Implications. Cureus 2023, 15, e48538. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bernhard, W.; Böckmann, K.; Maas, C.; Mathes, M.; Hövelmann, J.; Shunova, A.; Hund, V.; Schleicher, E.; Poets, C.F.; Franz, A.R. Combined choline and DHA supplementation: A randomized controlled trial. Eur. J. Nutr. 2020, 59, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Innis, S.M.; Davidson, A.G.; Bay, B.N.; Slack, P.J.; Hasman, D. Plasma choline depletion is associated with decreased peripheral blood leukocyte acetylcholine in children with cystic fibrosis. Am. J. Clin. Nutr. 2011, 93, 564–568. [Google Scholar] [CrossRef]
- Bernhard, W.; Poets, C.F.; Franz, A.R. Choline and choline-related nutrients in regular and preterm infant growth. Eur. J. Nutr. 2019, 58, 931–945. [Google Scholar] [CrossRef]
- Böckmann, K.A.; Franz, A.R.; Minarski, M.; Shunova, A.; Maiwald, C.A.; Schwarz, J.; Gross, M.; Poets, C.F.; Bernhard, W. Differential metabolism of choline supplements in adult volunteers. Eur. J. Nutr. 2022, 61, 219–230. [Google Scholar] [CrossRef]
- Grothe, J.; Riethmüller, J.; Tschürtz, S.M.; Raith, M.; Pynn, C.J.; Stoll, D.; Bernhard, W. Plasma phosphatidylcholine alterations in cystic fibrosis patients: Impaired metabolism and correlation with lung function and inflammation. Cell Physiol. Biochem. 2015, 35, 1437–1453. [Google Scholar] [CrossRef]
- Cohen, D.E. Hepatocellular transport and secretion of biliary phospholipids. Semin. Liver Dis. 1996, 16, 191–200. [Google Scholar] [CrossRef]
- Schmitz, G.; Muller, G. Structure and function of lamellar bodies, lipid-protein complexes involved in storage and secretion of cellular lipids. J. Lipid Res. 1991, 32, 1539–1570. [Google Scholar] [CrossRef] [PubMed]
- Mason, T.M. The role of factors that regulate the synthesis and secretion of very-low-density lipoprotein by hepatocytes. Crit. Rev. Clin. Lab. Sci. 1998, 35, 461–487. [Google Scholar] [CrossRef] [PubMed]
- Goss, K.C.W.; Goss, V.M.; Townsend, J.P.; Koster, G.; Clark, H.W.; Postle, A.D. Postnatal adaptations of phosphatidylcholine metabolism in extremely preterm infants: Implications for choline and PUFA metabolism. Am. J. Clin. Nutr. 2020, 112, 1438–1447. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, Z.; Agellon, L.B.; Allen, T.M.; Umeda, M.; Jewell, L.; Mason, A.; Vance, D.E. The ratio of phosphatidylcholine to phosphatidylethanolamine influences membrane integrity and steatohepatitis. Cell Metab. 2006, 3, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Hollenbeck, C.B. An introduction to the nutrition and metabolism of choline. Cent. Nerv. Syst. Agents Med. Chem. 2012, 12, 100–113. [Google Scholar] [CrossRef]
- Bernhard, W.; Raith, M.; Shunova, A.; Lorenz, S.; Böckmann, K.; Minarski, M.; Poets, C.F.; Franz, A.R. Choline Kinetics in Neonatal Liver, Brain and Lung-Lessons from a Rodent Model for Neonatal Care. Nutrients 2022, 14, 720. [Google Scholar] [CrossRef]
- Grassmé, H.; Carpinteiro, A.; Edwards, M.J.; Gulbins, E.; Becker, K.A. Regulation of the inflammasome by ceramide in cystic fibrosis lungs. Cell Physiol. Biochem. 2014, 34, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Mashimo, M.; Moriwaki, Y.; Misawa, H.; Ono, S.; Horiguchi, K.; Kawashima, K. Expression and function of the cholinergic system in immune cells. Front. Immunol. 2017, 8, 1085. [Google Scholar] [CrossRef]
- Zeisel, S.H. Choline: Critical role during fetal development and dietary requirements in adults. Annu. Rev. Nutr. 2006, 26, 229–250. [Google Scholar] [CrossRef]
- Li, Z.; Agellon, L.B.; Vance, D.E. Phosphatidylcholine homeostasis and liver failure. J. Biol. Chem. 2005, 280, 37798–37802. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Agellon, L.B.; Vance, D.E. Choline redistribution during adaptation to choline deprivation. J. Biol. Chem. 2007, 282, 10283–10289. [Google Scholar] [CrossRef]
- Bernhard, W.; Maas, C.; Shunova, A.; Mathes, M.; Böckmann, K.; Bleeker, C.; Vek, J.; Poets, C.F.; Schleicher, E.; Franz, A.R. Transport of long-chain polyunsaturated fatty acids in preterm infant plasma is dominated by phosphatidylcholine. Eur. J. Nutr. 2018, 57, 2105–2112. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, Å.; Duan, R.D. Pancreatic and mucosal enzymes in choline phospholipid digestion. Am. J. Physiol. Gastrointest. Liver Physiol. 2019, 316, G425–G445. [Google Scholar] [CrossRef] [PubMed]
- Northfield, T.C.; Hofmann, A.F. Biliary lipid output during three meals and an overnight fast. I. Relationship to bile acid pool size and cholesterol saturation of bile in gallstone and control subjects. Gut 1975, 16, 1–11. [Google Scholar] [CrossRef]
- Chen, A.H.; Innis, S.M.; Davidson, A.G.; James, S.J. Phosphatidylcholine and lysophosphatidylcholine excretion is increased in children with cystic fibrosis and is associated with plasma homocysteine, S-adenosylhomocysteine, and S-adenosylmethionine. Am. J. Clin. Nutr. 2005, 81, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Bernhard, W.; Shunova, A.; Machann, J.; Grimmel, M.; Haack, T.B.; Utz, P.; Graepler-Mainka, U. Resolution of severe hepatosteatosis in a cystic fibrosis patient with multifactorial choline deficiency: A case report. Nutrition 2021, 89, 111348. [Google Scholar] [CrossRef] [PubMed]
- Patterson, K.Y.; Bhagwat, S.A.; Williams, J.R.; Howe, J.C.; Holden, J.M. USDA Database for the Choline Content of Common Foods-Release Two. 2008. Available online: https://data.nal.usda.gov/system/files/Choln02.pdf (accessed on 11 June 2020).
- Shunova, A.; Böckmann, K.A.; Minarski, M.; Franz, A.R.; Wiechers, C.; Poets, C.F.; Bernhard, W. Choline Content of Term and Preterm Infant Formulae Compared to Expressed Breast Milk-How Do We Justify the Discrepancies? Nutrients 2020, 12, 3815. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Commission Delegated Regulation (EU) 2016/127 of 25 September 2015 Supplementing Regulation (EU) No 609/2013 of the European Parliament and of the Council as Regards the Specific Compositional and Information Requirements for Infant Formula and Follow-on Formula and as Regards Requirements on Information Relating to Infant and Young Child Feeding. 2016. Available online: https://eur-lex.europa.eu/legal-content/EN/ALL/?uri=CELEX%3A32016R0127 (accessed on 14 February 2025).
- Cho, C.E.; Aardema, N.D.J.; Bunnel, M.L.; Larson, D.P.; Aguilar, S.S.; Bergeson, J.R.; Malysheva, O.V.; Caudill, M.A.; Lefevre, M. Effect of Choline Forms and Gut Microbiota Composition on Trimethylamine-N-Oxide Response in Healthy Men. Nutrients 2020, 12, 2220. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Agostoni, C.; Buonocore, G.; Carnielli, V.P.; De Curtis, M.; Darmaun, D.; Decsi, T.; Domellöf, M.; Embleton, N.D.; Fusch, C.; Genzel-Boroviczeny, O.; et al. Enteral nutrient supply for preterm infants: Commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Embleton, N.D.; Jennifer Moltu, S.; Lapillonne, A.; van den Akker, C.H.P.; Carnielli, V.; Fusch, C.; Gerasimidis, K.; van Goudoever, J.B.; Haiden, N.; Iacobelli, S.; et al. Enteral Nutrition in Preterm Infants: A Position Paper from the ESPGHAN Committee on Nutrition and Invited Experts. J. Pediatr. Gastroenterol. Nutr. 2023, 76, 248–268. [Google Scholar] [CrossRef] [PubMed]
- Wilschanski, M.; Munck, A.; Carrion, E.; Cipolli, M.; Collins, S.; Colombo, C.; Declercq, D.; Hatziagorou, E.; Hulst, J.; Kalnins, D.; et al. ESPEN-ESPGHAN-ECFS guideline on nutrition care for cystic fibrosis. Clin. Nutr. 2024, 43, 413–445. [Google Scholar] [CrossRef] [PubMed]
- Maas, C.; Franz, A.R.; Shunova, A.; Mathes, M.; Bleeker, C.; Poets, C.F.; Schleicher, E.; Bernhard, W. Choline and polyunsaturated fatty acids in preterm infants’ maternal milk. Eur. J. Nutr. 2017, 56, 1733–1742. [Google Scholar] [CrossRef] [PubMed]
- Nierle, W.; el Wahab el Bayâ, A. Untersuchung und Zusammensetzung einiger Leguminosen [Examination and composition of some legume seeds (author’s transl)]. Z. Lebensm. Unters. Forsch. 1977, 164, 23–27. (In German) [Google Scholar] [CrossRef] [PubMed]




| Patient Group | Preterm Infant Fortifier Preterm Infant Formula Term Infant Formula (0–6 months) Term Infant Supplementary Food (>6–12 months) Toddler Supplementary Food (12 months to 3 years;) Supplements in Cystic Fibrosis (>12 m) Products with other Indications |
| Macronutrients | Energy (kcal/100 mL) | |
| Protein (Energy-%) | ||
| Fat (Energy-%) | ||
| Carbohydrates (Energy-%) | ||
| Micronutrients | (mg/100 mL) | (mg/100 kcal) |
| Choline | Choline | |
| Folate | Folate | |
| B12 | B12 | |
| ARA | ARA | |
| DHA | DHA | |
| Micronutrient Ratios | Choline/Folate; Choline/B12; Choline/ARA; Choline/DHA | |
| Product | Choline Added (mg/100 kcal) | Choline Component | Choline Containing Emulsifiers | Water Soluble Choline Components from Milk |
|---|---|---|---|---|
| Preterm Infant Fortifier | ||||
| BEBA FM 85, Nestlé * | 17.3 | No specification | Soya Lecithin | ∅ |
| Humavant+4, Prolacta | 0 | ∅ | Milk Lipids | Human Milk |
| Aptamil FMS, Nutricia | 0 | ∅ | Egg and Milk Lipids | ∅ |
| Preterm Infant Formula | ||||
| Aptamil HA Pre, Nutricia | 33.3 | Choline chloride | egg lipids | ∅ |
| Aptamil PDF, Nutricia | 31.9 | Choline chloride | egg lipids | Skimmed milk |
| Aptamil Prematil, Nutricia | 32.5 | Choline chloride | egg lipids | Skimmed milk |
| Aptamil Prematil HA, Nutricia | 32.5 | Choline chloride | egg lipids, soya lecithin | ∅ |
| Monogen, Nutricia | 23.0 | Choline chloride | ∅ | Skimmed milk |
| Term Infant Formula (0–6 months) | ||||
| Aptamil HA Pre, Nutricia | 33.3 | Choline chloride | egg lipids | ∅ |
| Aptamil PDF, Nutricia | 31.9 | Choline chloride | egg lipids | ∅ |
| Aptamil Prematil, Nutricia | 33.3 | Choline chloride | egg lipids | ∅ |
| Aptamil Prematil HA, Nutricia | 31.9 | Choline chloride | egg lipids, soya lecithin | ∅ |
| Bebita 1, Bebivita | 38.8 | No specification | ∅ | Skimmed milk |
| Bio Combiotic PRE, Hipp | 37.9 | No specification | ∅ | Skimmed milk |
| Bio Combiotic 1, Hipp | 38.8 | No specification | ∅ | Skimmed milk |
| Humana Anfangsmilch pre, Humana | 30.8 | Choline bitartrate | ∅ | Skimmed Milk, whey powder |
| Humana Anfangsmilch 1, Humana | 37.3 | Choline bitartrate | ∅ | Skimmed Milk, whey powder |
| kendamil first instant milk, Kendamil | 32.8 | Choline bitartrate | Whole milk lipids | skimmed milk, whey powder |
| Kendamil first organic, Kendamil | 30.3 | Choline bitartrate | Whole milk lipids | skimmed milk, whey powder |
| Kendamil first goat, Kendamil | 32.8 | Choline bitartrate | Whole goat milk lipids | skimmed goat milk, whey powder |
| Milumil Pre Anfangsmilch, Milupa | 36.4 | Choline chloride | Soya lecithin | Skimmed milk, whey components |
| Milumil 1 Anfangsmilch, Milupa | 32.4 | Choline chloride | Soya lecithin | Skimmed milk |
| Alfaré, Nestlé | 29.9 | Choline bitartrate | Soya lecithin | ∅ |
| BEBA Optipro PRE, Nestlé | 30.8 | Choline bitartrate | Soya lecithin | Skimmed milk, whey |
| BEBA Optipro 1, Nestlé | 30.7 | Choline bitartrate | Soya lecithin | Skimmed milk, whey |
| Aptamil Care Pre, Nutricia | 34.8 | Choline chloride | Soya lecithin | Skimmed milk |
| Aptamil Comfort, Nutricia | 33.3 | Choline chloride | Soya lecithin | ∅ |
| Aptamil Pronutra Pre, Nutricia | 33.3 | Choline chloride | Soya lecithin | Skimmed milk |
| Aptamil FMS, Nutricia | 0 | ∅ | Egg lipids | ∅ |
| Aptamil Anti Reflux, Nutricia | 33.3 | Choline chloride | Soya lecithin | Skimmed milk, whey |
| Aptamil Care Pre, Nutricia | 34.8 | Choline chloride | Soya lecithin | Skimmed milk, whey |
| Aptamil Bio PRE, Nutricia | 33.3 | Choline chloride | Lecithin, not specified | Skimmed milk, whey |
| Aptamil Organic PRE, Nutricia | 33.3 | Choline chloride | ∅ | Skimmed milk, whey |
| Aptamil Organic 1, Nutricia | 33.3 | Choline chloride | Soya lecithin | Skimmed milk, whey |
| Holle Bio Pre, Holle | 33.3 | Choline bitartrate | ∅ | Skimmed milk, whey |
| Bio-Anfangsmilch, Holle | 33.8 | Choline bitartrate | ∅ | Skimmed milk, whey |
| Bio-Anfangsmilch 1, Holle | 33.3 | Choline bitartrate | ∅ | Skimmed milk, whey |
| Bio-Anfangsmilch 1 aus Ziegenmilch, Holle | 32.4 | Choline bitartrate | Goat milk lipids | Whey |
| Term Infant Supplements (6–12 months) | ||||
| Bebivita 2 Folgemilch, Bebivita | 0 | ∅ | Lecithins, not specified | Skimmed milk |
| Bio Combiotic 2, Hipp | 0 | ∅ | ∅ | Skimmed milk, whey |
| HiPP Bio Ziegenmilch 2, Hipp | 0 | ∅ | ∅ | Skimmed goat milk |
| Humana Folgemilch 2, Humana | 37.3 | Choline bitartrate | ∅ | Skimmed milk, whey |
| Humana Folgemilch 3, Humana | 37.3 | Choline bitartrate | ∅ | Skimmed milk, whey |
| Follow-on milk, Kendamil | 32.8 | Choline bitartrate | Whole Milk lipids | Skimmed milk, whey |
| kendamil goat, Kendamil | 24.2 | Choline bitartrate | Whole Goat Milk Lipids | Skimmed Goat Milk, Whey |
| Milumil 2 Folgemilch, Milupa | 25.0 | Choline chloride | Soya lecithin | Skimmed milk, whey |
| Milumil 3 Folgemilch, Milupa | 25.0 | Choline chloride | Soya lecithin | Skimmed milk, whey |
| BEBA Optipro 2, Nestlé | 0 | ∅ | Soya lecithin | Skimmed milk, whey |
| Aptamil Bio 2, Nutricia | 0 | ∅ | Lecithins, not specified | Skimmed milk, whey |
| Monogen, Nutricia | 23.0 | Choline chloride | ∅ | Skimmed milk |
| BEBA Optipro 2, Nestlé | 0 | ∅ | Soya lecithin | ∅ |
| Toddler Milk (12–36 Months) | ||||
| Humana Kindergetränk 1+, Humana | 0 | ∅ | ∅ | Skimmed milk |
| Toddler milk, Kendamil | 0 | ∅ | Whole milk lipids | Skimmed milk |
| Toddler milk Organic, Kendamil | 0 | ∅ | Whole milk lipids | Water soluble Milk Components, Whey |
| BEBA Junior 12–36, Nestlé | 0 | ∅ | Milk fat, soya lecithin | Skimmed milk, whey |
| Special Indications | ||||
| Aptamil Profutura DUOADVANCE 2, Nutricia | 22.1 | Choline chloride | Milk fat, soya lecithin | Skimmed milk, whey |
| Energea Pkid, MetaX | 0 | ∅ | Sunflower lecithin | Skimmed milk |
| Energea P, MetaX | 0 | ∅ | Sunflower lecithin | Skimmed milk |
| Nephea Kid (Kidney Disease), MetaX | 0 | ∅ | Soya lecithin | ∅ |
| Nephea Infant (Kidney Disease), MetaX | 0 | ∅ | Soya lecithin | ∅ |
| Peptamen (Tube feeding), Nestlé | 21 | Choline chloride | Soya lecithin | ∅ |
| Peptamen Junior Advance (high energy tube feed), Nestlé | 16 | Choline chloride | Soya lecithin | ∅ |
| Aptamil PDF, Nutricia | 31.9 | Choline chloride | Egg lipids | Skimmed milk |
| Fortimel Joghurt Style | 36.7 | Choline chloride | Skimmed milk | |
| Fortimel Pulver Neutral, | 33.1 | Choline chloride | Soya lecithin | ∅ |
| Infatrini 125 mL, Nutricia | 31.3 | Choline chloride | Soya lecithin | Skimmed milk |
| Nutrini Multi Fibre, Nutricia | 20 | Choline chloride | Soya lecithin | ∅ |
| NutriniDrink Compact Multi Fibre, Nutricia | 20 | Choline chloride | Soya lecithin | ∅ |
| Nutrini creamy, Nutricia | 20 | Choline chloride | Soya lecithin, milk lipids | Skimmed milk |
| restoric® nephro prae, Vitasyn medical | 0 | ∅ | Soya lecithin | ∅ |
| restoric® supportiv S (Malnutrition), Vitasyn medical | 0 | ∅ | Soya lecithin | ∅ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernhard, W.; Shunova, A.; Graepler-Mainka, U.; Hilberath, J.; Wiechers, C.; Poets, C.F.; Franz, A.R. Choline in Pediatric Nutrition: Assessing Formula, Fortifiers and Supplements Across Age Groups and Clinical Indications. Nutrients 2025, 17, 1632. https://doi.org/10.3390/nu17101632
Bernhard W, Shunova A, Graepler-Mainka U, Hilberath J, Wiechers C, Poets CF, Franz AR. Choline in Pediatric Nutrition: Assessing Formula, Fortifiers and Supplements Across Age Groups and Clinical Indications. Nutrients. 2025; 17(10):1632. https://doi.org/10.3390/nu17101632
Chicago/Turabian StyleBernhard, Wolfgang, Anna Shunova, Ute Graepler-Mainka, Johannes Hilberath, Cornelia Wiechers, Christian F. Poets, and Axel R. Franz. 2025. "Choline in Pediatric Nutrition: Assessing Formula, Fortifiers and Supplements Across Age Groups and Clinical Indications" Nutrients 17, no. 10: 1632. https://doi.org/10.3390/nu17101632
APA StyleBernhard, W., Shunova, A., Graepler-Mainka, U., Hilberath, J., Wiechers, C., Poets, C. F., & Franz, A. R. (2025). Choline in Pediatric Nutrition: Assessing Formula, Fortifiers and Supplements Across Age Groups and Clinical Indications. Nutrients, 17(10), 1632. https://doi.org/10.3390/nu17101632







