Personalized Hydration Strategy to Improve Fluid Balance and Intermittent Exercise Performance in the Heat
Abstract
1. Introduction
2. Materials and Methods
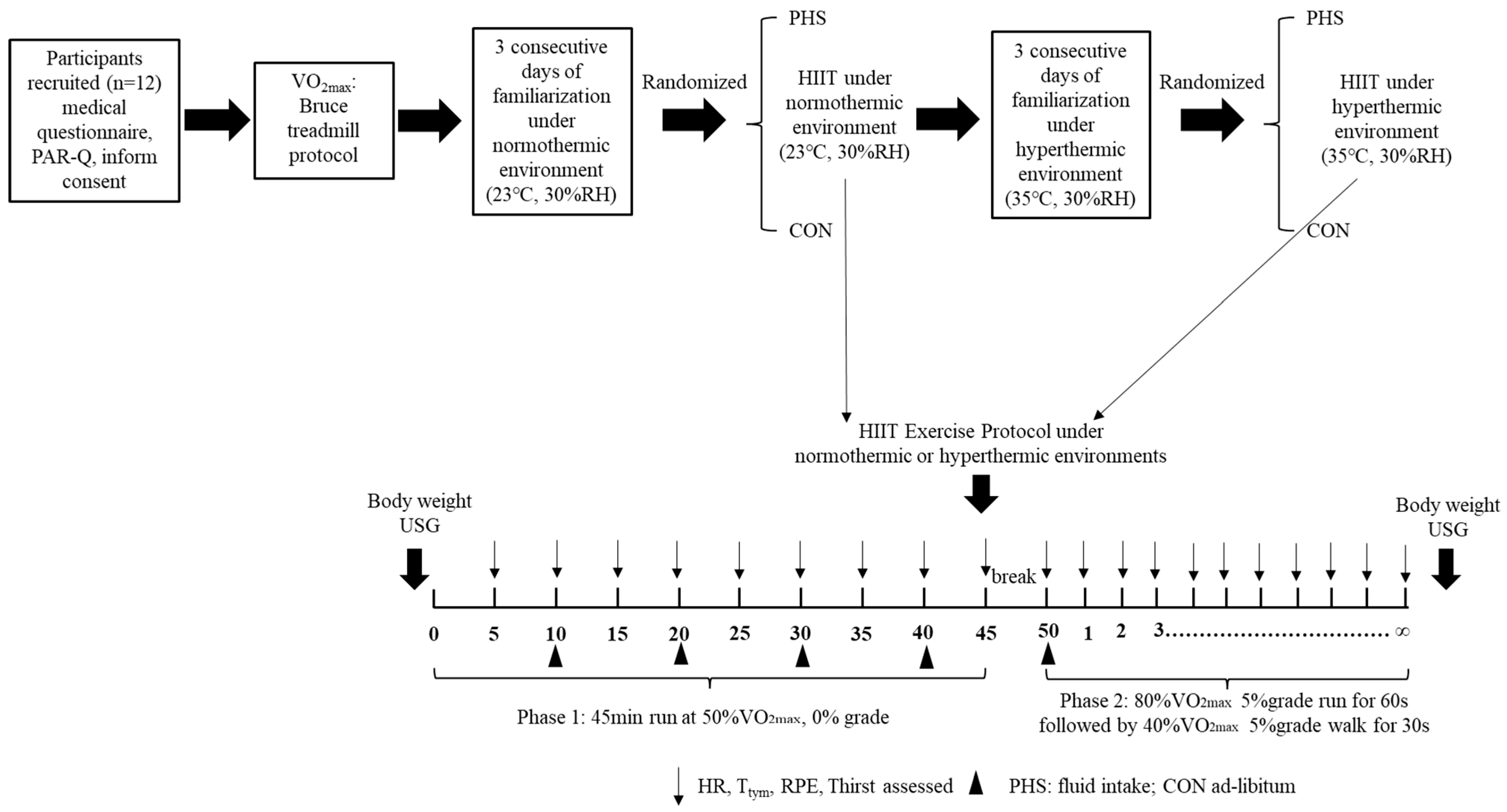
2.1. Experimental Design
2.2. Participants
2.3. Familiarization Exercise Phase
2.4. Hydration Strategies
2.5. Exercise Trials
2.6. Outcome Measures
2.7. Statistical Analysis
3. Results
3.1. Fluid Balance
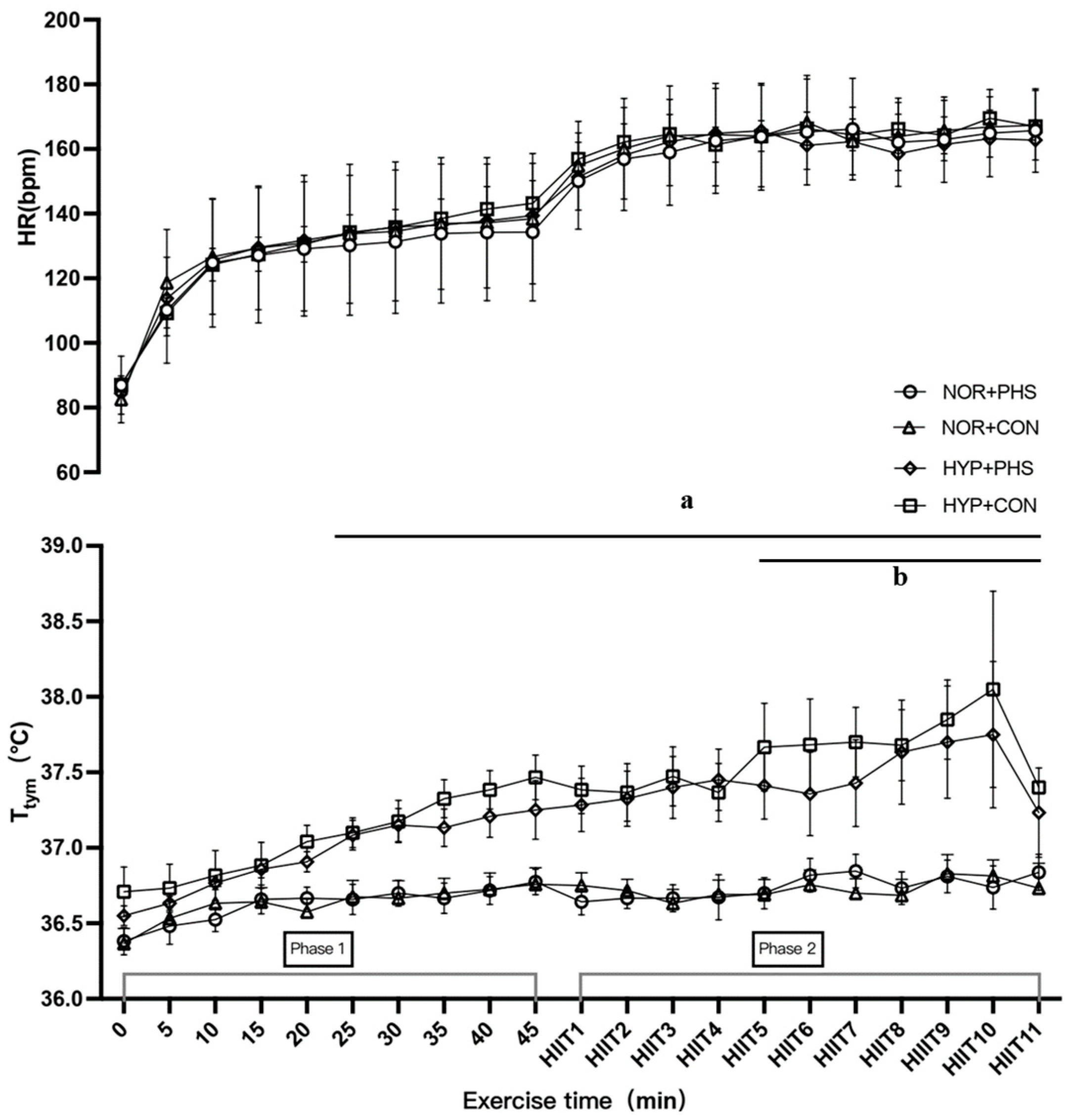
3.2. Physiological Responses
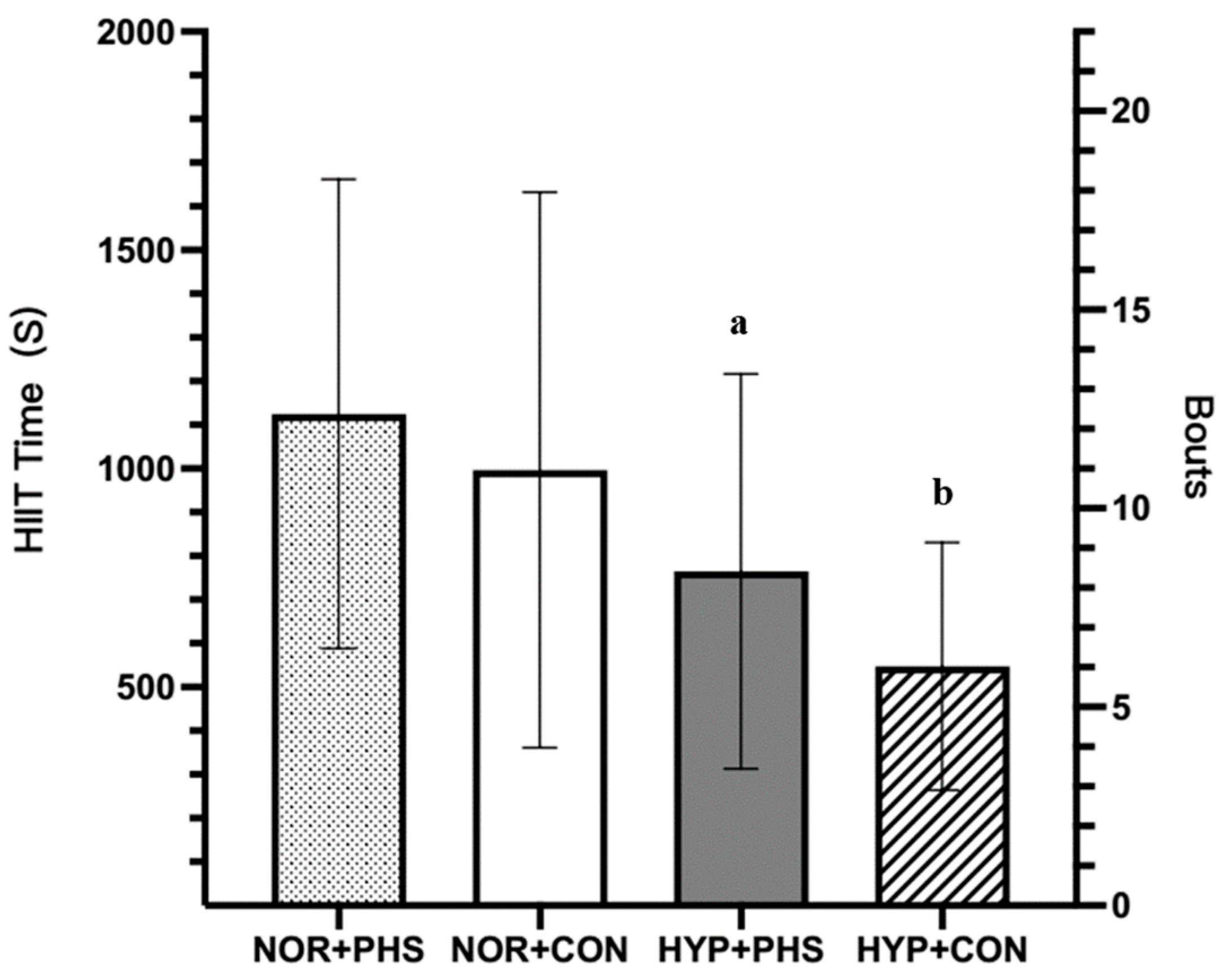
3.3. Exercise Performance
4. Discussion
4.1. Fluid Balance
4.2. Exercise Performance
4.3. Strengths and Limitations
4.4. Practical Applications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gerrett, N.; Kingma, B.R.M.; Sluijter, R.; Daanen, H.A.M. Ambient Conditions Prior to Tokyo 2020 Olympic and Paralympic Games: Considerations for Acclimation or Acclimatization Strategies. Front. Physiol. 2019, 10, 414. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; Clarkson, P.M.; Roberts, W.O. American College of Sports Medicine roundtable on hydration and physical activity: Consensus statements. Curr. Sports Med. Rep. 2005, 4, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Racinais, S.; Mohr, M.; Buchheit, M.; Voss, S.C.; Gaoua, N.; Grantham, J.; Nybo, L. Individual responses to short-term heat acclimatisation as predictors of football performance in a hot, dry environment. Br. J. Sports Med. 2012, 46, 810–815. [Google Scholar] [CrossRef] [PubMed]
- Tatterson, A.J.; Hahn, A.G.; Martin, D.T.; Febbraio, M.A. Effects of heat stress on physiological responses and exercise performance in elite cyclists. J. Sci. Med. Sport 2000, 3, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Convertino, V.A.; Armstrong, L.E.; Coyle, E.F.; Mack, G.W.; Sawka, M.N.; Senay, L.C., Jr.; Sherman, W.M. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 1996, 28, i–vii. [Google Scholar] [CrossRef] [PubMed]
- McDermott, B.P.; Anderson, S.A.; Armstrong, L.E.; Casa, D.J.; Cheuvront, S.N.; Cooper, L.; Kenney, W.L.; O’Connor, F.G.; Roberts, W.O. National Athletic Trainers’ Association Position Statement: Fluid Replacement for the Physically Active. J. Athl. Train. 2017, 52, 877–895. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; Armstrong, L.E.; Hillman, S.K.; Montain, S.J.; Reiff, R.V.; Rich, B.S.; Roberts, W.O.; Stone, J.A. National athletic trainers’ association position statement: Fluid replacement for athletes. J. Athl. Train. 2000, 35, 212–224. [Google Scholar] [PubMed]
- Savoie, F.A.; Kenefick, R.W.; Ely, B.R.; Cheuvront, S.N.; Goulet, E.D. Effect of Hypohydration on Muscle Endurance, Strength, Anaerobic Power and Capacity and Vertical Jumping Ability: A Meta-Analysis. Sports Med. 2015, 45, 1207–1227. [Google Scholar] [CrossRef]
- Sawka, M.N.; Burke, L.M.; Eichner, E.R.; Maughan, R.J.; Montain, S.J.; Stachenfeld, N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007, 39, 377–390. [Google Scholar]
- Pence, J.; Bloomer, R.J. Impact of Nuun Electrolyte Tablets on Fluid Balance in Active Men and Women. Nutrients 2020, 12, 3030. [Google Scholar] [CrossRef]
- Chryssanthopoulos, C.; Dallas, G.; Arnaoutis, G.; Ragkousi, E.C.; Kapodistria, G.; Lambropoulos, I.; Papassotiriou, I.; Philippou, A.; Maridaki, M.; Theos, A. Young Artistic Gymnasts Drink Ad Libitum Only Half of Their Fluid Lost during Training, but More Fluid Intake Does Not Influence Performance. Nutrients 2023, 15, 2667. [Google Scholar] [CrossRef] [PubMed]
- Wijering, L.A.J.; Cotter, J.D.; Rehrer, N.J. A randomized, cross-over trial assessing effects of beverage sodium concentration on plasma sodium concentration and plasma volume during prolonged exercise in the heat. Eur. J. Appl. Physiol. 2023, 123, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Ranchordas, M.K.; Tiller, N.B.; Ramchandani, G.; Jutley, R.; Blow, A.; Tye, J.; Drury, B. Normative data on regional sweat-sodium concentrations of professional male team-sport athletes. J. Int. Soc. Sports Nutr. 2017, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Shirreffs, S.M.; Aragon-Vargas, L.F.; Chamorro, M.; Maughan, R.J.; Serratosa, L.; Zachwieja, J.J. The sweating response of elite professional soccer players to training in the heat. Int. J. Sports Med. 2005, 26, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Belval, L.N.; Hosokawa, Y.; Casa, D.J.; Adams, W.M.; Armstrong, L.E.; Baker, L.B.; Burke, L.; Cheuvront, S.; Chiampas, G.; González-Alonso, J.; et al. Practical Hydration Solutions for Sports. Nutrients 2019, 11, 1550. [Google Scholar] [CrossRef] [PubMed]
- Wingo, J.E. Exercise intensity prescription during heat stress: A brief review. Scand. J. Med. Sci. Sports 2015, 25 (Suppl. S1), 90–95. [Google Scholar] [CrossRef] [PubMed]
- Perez-Suarez, I.; Martin-Rincon, M.; Gonzalez-Henriquez, J.J.; Fezzardi, C.; Perez-Regalado, S.; Galvan-Alvarez, V.; Juan-Habib, J.W.; Morales-Alamo, D.; Calbet, J.A.L. Accuracy and Precision of the COSMED K5 Portable Analyser. Front. Physiol. 2018, 9, 1764. [Google Scholar] [CrossRef]
- Morris, N.B.; Cramer, M.N.; Hodder, S.G.; Havenith, G.; Jay, O. A comparison between the technical absorbent and ventilated capsule methods for measuring local sweat rate. J. Appl. Physiol. (1985) 2013, 114, 816–823. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B.; De Chavez, P.J.D.; Ungaro, C.T.; Sopena, B.C.; Nuccio, R.P.; Reimel, A.J.; Barnes, K.A. Exercise intensity effects on total sweat electrolyte losses and regional vs. whole-body sweat [Na(+)], [Cl(-)], and [K(+)]. Eur. J. Appl. Physiol. 2019, 119, 361–375. [Google Scholar] [CrossRef]
- Passe, D.; Horn, M.; Stofan, J.; Horswill, C.; Murray, R. Voluntary dehydration in runners despite favorable conditions for fluid intake. Int. J. Sport Nutr. Exerc. Metab. 2007, 17, 284–295. [Google Scholar] [CrossRef]
- Emerson, D.M.; Torres-McGehee, T.M.; Emerson, C.C.; LaSalle, T.L. Individual fluid plans versus ad libitum on hydration status in minor professional ice hockey players. J. Int. Soc. Sports Nutr. 2017, 14, 25. [Google Scholar] [CrossRef] [PubMed]
- de Melo-Marins, D.; Souza-Silva, A.A.; da Silva-Santos, G.L.L.; Freire-Junior, F.A.; Lee, J.K.W.; Laitano, O. Personalized Hydration Strategy Attenuates the Rise in Heart Rate and in Skin Temperature Without Altering Cycling Capacity in the Heat. Front. Nutr. 2018, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Bardis, C.N.; Kavouras, S.A.; Adams, J.D.; Geladas, N.D.; Panagiotakos, D.B.; Sidossis, L.S. Prescribed Drinking Leads to Better Cycling Performance than Ad Libitum Drinking. Med. Sci. Sports Exerc. 2017, 49, 1244–1251. [Google Scholar] [CrossRef] [PubMed]
- Lopez, R.M.; Casa, D.J.; Jensen, K.A.; Stearns, R.L.; DeMartini, J.K.; Pagnotta, K.D.; Roti, M.W.; Armstrong, L.E.; Maresh, C.M. Comparison of Two Fluid Replacement Protocols During a 20-km Trail Running Race in the Heat. J. Strength Cond. Res. 2016, 30, 2609–2616. [Google Scholar] [CrossRef] [PubMed]
- Ayotte, D., Jr.; Corcoran, M.P. Individualized hydration plans improve performance outcomes for collegiate athletes engaging in in-season training. J. Int. Soc. Sports Nutr. 2018, 15, 27. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B.; De Chavez, P.J.D.; Nuccio, R.P.; Brown, S.D.; King, M.A.; Sopena, B.C.; Barnes, K.A. Explaining variation in sweat sodium concentration: Effect of individual characteristics and exercise, environmental, and dietary factors. J. Appl. Physiol. (1985) 2022, 133, 1250–1259. [Google Scholar] [CrossRef] [PubMed]
- Buono, M.J.; Claros, R.; Deboer, T.; Wong, J. Na+ secretion rate increases proportionally more than the Na+ reabsorption rate with increases in sweat rate. J. Appl. Physiol. (1985) 2008, 105, 1044–1048. [Google Scholar] [CrossRef] [PubMed]
- Bates, G.P.; Miller, V.S. Sweat rate and sodium loss during work in the heat. J. Occup. Med. Toxicol. 2008, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- McCubbin, A.J.; Lopez, M.B.; Cox, G.R.; Caldwell Odgers, J.N.; Costa, R.J.S. Impact of 3-day high and low dietary sodium intake on sodium status in response to exertional-heat stress: A double-blind randomized control trial. Eur. J. Appl. Physiol. 2019, 119, 2105–2118. [Google Scholar] [CrossRef]
- Hamouti, N.; Fernandez-Elias, V.E.; Ortega, J.F.; Mora-Rodriguez, R. Ingestion of sodium plus water improves cardiovascular function and performance during dehydrating cycling in the heat. Scand. J. Med. Sci. Sports 2014, 24, 507–518. [Google Scholar] [CrossRef]
- Johannsen, N.M.; Sullivan, Z.M.; Warnke, N.R.; Smiley-Oyen, A.L.; King, D.S.; Sharp, R.L. Effect of preexercise soup ingestion on water intake and fluid balance during exercise in the heat. Int. J. Sport Nutr. Exerc. Metab. 2013, 23, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Cheung, S.S.; McGarr, G.W.; Mallette, M.M.; Wallace, P.J.; Watson, C.L.; Kim, I.M.; Greenway, M.J. Separate and combined effects of dehydration and thirst sensation on exercise performance in the heat. Scand. J. Med. Sci. Sports 2015, 25 (Suppl. S1), 104–111. [Google Scholar] [CrossRef] [PubMed]
- Berkulo, M.A.; Bol, S.; Levels, K.; Lamberts, R.P.; Daanen, H.A.; Noakes, T.D. Ad libitum drinking and performance during a 40-km cycling time trial in the heat. Eur. J. Sport Sci. 2016, 16, 213–220. [Google Scholar] [CrossRef] [PubMed]

| NOR+PHS | NOR+CON | HYP+PHS | HYP+CON | p Value | |
|---|---|---|---|---|---|
| %BML | −0.49 ± 0.40 ab | −1.19 ± 0.57 | −0.69 ± 0.40 ab | −1.28 ± 0.34 | <0.001 |
| Fluid Intake (g) | 734.2 ± 144.9 ab | 272.3 ± 143.0 | 831.7 ± 166.4 ab | 369.8 ± 221.7 | <0.001 |
| Sodium Intake (g) | 0.92 ± 0.27 ab | 0.19 ± 0.10 | 1.18 ± 0.29 abc | 0.26 ± 0.15 | <0.001 |
| WBSR (L/h) | 0.89 ± 0.44 | 0.89 ± 0.34 | 1.07 ± 0.20 | 1.12 ± 0.22 | 0.16 |
| LSR (mg/cm2/min) | 3.69 ± 1.10 | 3.61 ± 1.34 | 3.86 ± 0.98 | 4.09 ± 0.80 | 0.52 |
| Sweat Na+ (mmol/L) | 67.8 ± 14.3 | 71.3 ± 16.3 | 62.7 ± 9.6 ab | 56.2 ± 9.0 a | <0.001 |
| ΔUrine Na+ (mmol/L) | 10.0 ± 17.2 | 13.9 ± 16.5 | 5.0 ± 13.6 | 5.6 ± 16.1 | 0.36 |
| ΔUrine K+ (mmol/L) | −4.3 ± 4.8 | −6.0 ± 5.7 | −4.8 ± 4.8 | −0.5 ± 5.9 | 0.10 |
| Phase 1 (0–45 min) | |||||
| NOR+PHS | NOR+CON | HYP+PHS | HYP+CON | p Value | |
| HR (bpm) | 124 ± 24 | 127 ± 24 | 127 ± 26 | 127 ± 25 | 0.50 |
| Ttym (°C) | 36.6 ± 0.3 | 36.6 ± 0.4 | 37.0 ± 0.4 abc | 37.1 ± 0.5 ab | <0.001 |
| RPE | 9 ± 2 c | 9 ± 2 c | 9 ± 3 c | 10 ± 3 | 0.003 |
| ΔThirst | 0.5 ± 1.2 | 0.8 ± 1.0 a | 0.6 ± 0.8 | 0.7 ± 0.7 a | 0.03 |
| Phase 2 (HIIT-Fatigue) | |||||
| HR (bpm) | 163 ± 14 | 167 ± 13 a | 166 ± 16 | 165 ± 16 | 0.04 |
| Ttym (°C) | 36.8 ± 0.4 | 36.8 ± 0.3 | 37.5 ± 0.6 ab | 37.6 ± 0.6 ab | <0.001 |
| RPE | 16 ± 3 | 16 ± 3 | 17 ± 3 | 16 ± 4 | <0.001 |
| ΔThirst | 2.2 ± 2.0 bc | 2.8 ± 2.1 | 2.0 ± 2.2 bc | 2.9 ± 2.1 | 0.002 |
| HIIT Time (s) | 1125 ± 537 | 1005 ± 627 | 765 ± 452 abc | 548 ± 283 ab | <0.001 |
| Bouts (#) | 13 ± 6 | 11 ± 7 | 9 ± 5 abc | 6 ± 3 ab | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, H.; Early, K.S.; Zhang, G.; Ma, P.; Wang, H. Personalized Hydration Strategy to Improve Fluid Balance and Intermittent Exercise Performance in the Heat. Nutrients 2024, 16, 1341. https://doi.org/10.3390/nu16091341
Li H, Early KS, Zhang G, Ma P, Wang H. Personalized Hydration Strategy to Improve Fluid Balance and Intermittent Exercise Performance in the Heat. Nutrients. 2024; 16(9):1341. https://doi.org/10.3390/nu16091341
Chicago/Turabian StyleLi, Haicheng, Kate S. Early, Guangxia Zhang, Pengwei Ma, and Haoyan Wang. 2024. "Personalized Hydration Strategy to Improve Fluid Balance and Intermittent Exercise Performance in the Heat" Nutrients 16, no. 9: 1341. https://doi.org/10.3390/nu16091341
APA StyleLi, H., Early, K. S., Zhang, G., Ma, P., & Wang, H. (2024). Personalized Hydration Strategy to Improve Fluid Balance and Intermittent Exercise Performance in the Heat. Nutrients, 16(9), 1341. https://doi.org/10.3390/nu16091341





