Effects of a Novel Applet-Based Personalized Dietary Intervention on Dietary Intakes: A Randomized Controlled Trial in a Real-World Scenario
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Randomization and Blinding
2.4. Run-In Phase and Baseline Assessment
2.5. Interventions
2.5.1. Pre-Meal Intervention: Figure 2b
2.5.2. Post-Meal Intervention: Figure 2c
2.6. Measures and Follow-Up
2.6.1. Online Questionnaire Survey
2.6.2. Dietary Records
2.6.3. Anthropometric Measurements
2.7. Statistical Analysis
3. Results
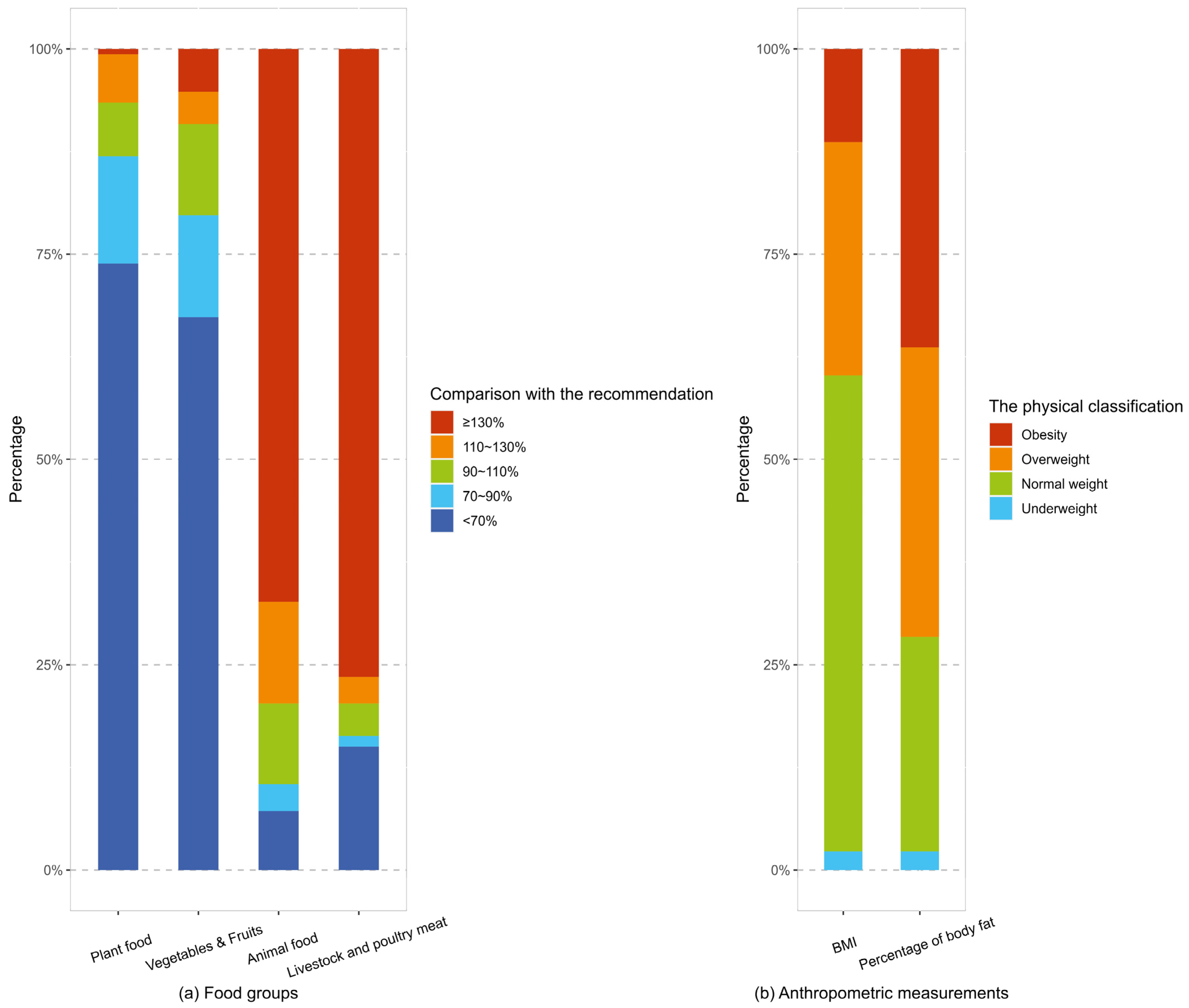
3.1. Participants’ Characteristics
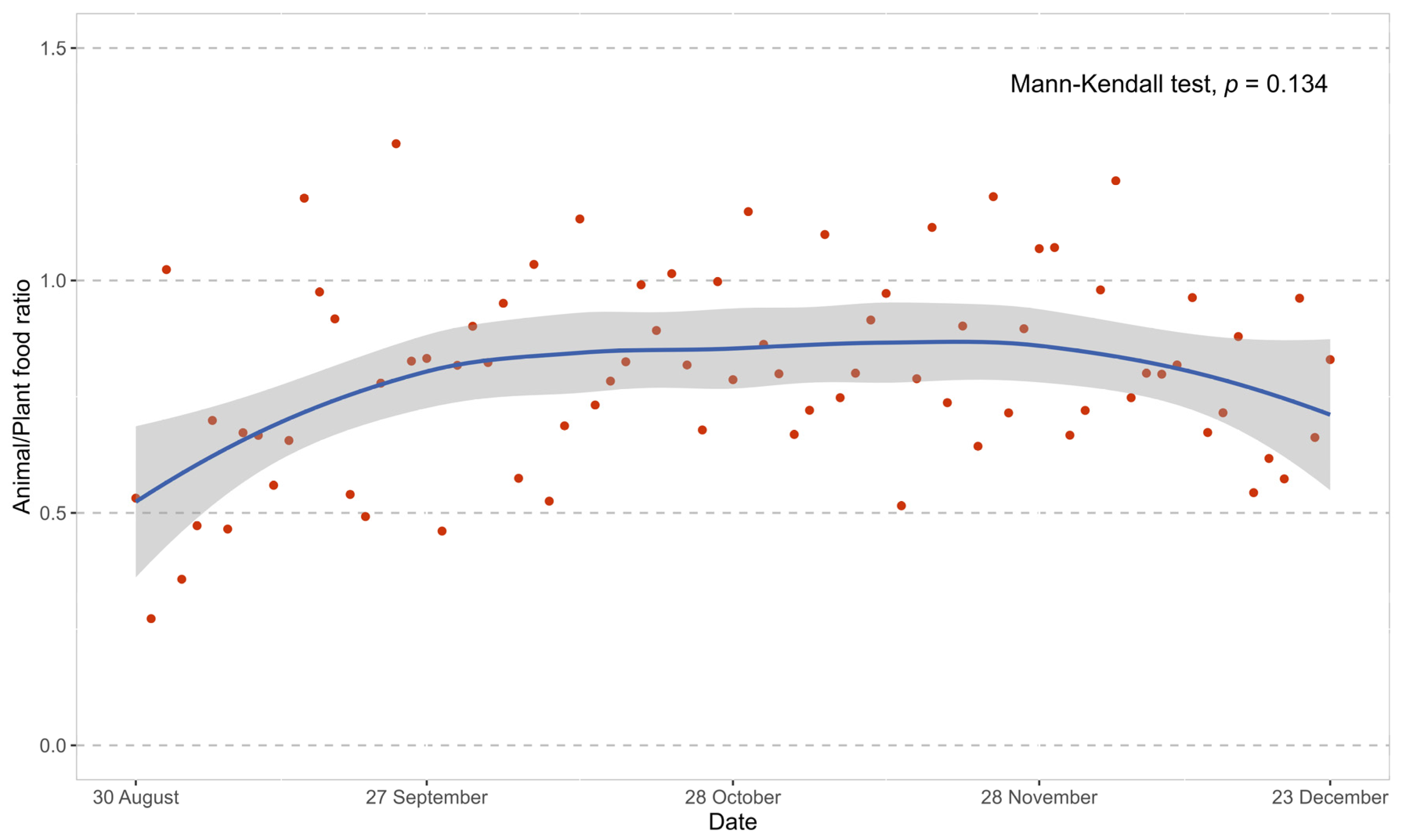
3.2. Canteen Meal Supply
3.3. Effects of the Intervention on Dietary Intakes
3.4. Effects of the Intervention on Anthropometric Indicators
3.5. Additional Analysis for Ease and Understandability of the Applet
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Huang, L.; Wang, Z.; Wang, H.; Zhao, L.; Jiang, H.; Zhang, B.; Ding, G. Nutrition transition and related health challenges over decades in China. Eur. J. Clin. Nutr. 2021, 75, 247–252. [Google Scholar] [CrossRef]
- Chlebowski, R.T.; Aragaki, A.K.; Anderson, G.L.; Pan, K.; Neuhouser, M.L.; Manson, J.E.; Thomson, C.A.; Mossavar-Rahmani, Y.; Lane, D.S.; Johnson, K.C.; et al. Dietary Modification and Breast Cancer Mortality: Long-Term Follow-Up of the Women’s Health Initiative Randomized Trial. J. Clin. Oncol. 2020, 38, 1419–1428. [Google Scholar] [CrossRef]
- Luna-Castillo, K.P.; Olivares-Ochoa, X.C.; Hernandez-Ruiz, R.G.; Llamas-Covarrubias, I.M.; Rodriguez-Reyes, S.C.; Betancourt-Nunez, A.; Vizmanos, B.; Martinez-Lopez, E.; Munoz-Valle, J.F.; Marquez-Sandoval, F.; et al. The Effect of Dietary Interventions on Hypertriglyceridemia: From Public Health to Molecular Nutrition Evidence. Nutrients 2022, 14, 1104. [Google Scholar] [CrossRef]
- Prentice, R.L.; Aragaki, A.K.; Van Horn, L.; Thomson, C.A.; Beresford, S.A.; Robinson, J.; Snetselaar, L.; Anderson, G.L.; Manson, J.E.; Allison, M.A.; et al. Low-fat dietary pattern and cardiovascular disease: Results from the Women’s Health Initiative randomized controlled trial. Am. J. Clin. Nutr. 2017, 106, 35–43. [Google Scholar] [CrossRef]
- Ali, M.K.; Echouffo-Tcheugui, J.; Williamson, D.F. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff. 2012, 31, 67–75. [Google Scholar] [CrossRef]
- Lim, S.L.; Ong, K.W.; Johal, J.; Han, C.Y.; Yap, Q.V.; Chan, Y.H.; Zhang, Z.P.; Chandra, C.C.; Thiagarajah, A.G.; Khoo, C.M. A Smartphone App-Based Lifestyle Change Program for Prediabetes (D’LITE Study) in a Multiethnic Asian Population: A Randomized Controlled Trial. Front. Nutr. 2021, 8, 780567. [Google Scholar] [CrossRef]
- Barry, E.; Roberts, S.; Oke, J.; Vijayaraghavan, S.; Normansell, R.; Greenhalgh, T. Efficacy and effectiveness of screen and treat policies in prevention of type 2 diabetes: Systematic review and meta-analysis of screening tests and interventions. BMJ 2017, 356, i6538. [Google Scholar] [CrossRef] [PubMed]
- Van Lippevelde, W.; Vangeel, J.; De Cock, N.; Lachat, C.; Goossens, L.; Beullens, K.; Vervoort, L.; Braet, C.; Maes, L.; Eggermont, S.; et al. Using a gamified monitoring app to change adolescents’ snack intake: The development of the REWARD app and evaluation design. BMC Public Health 2016, 16, 725. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Mitchell, E.S.; Ho, A.S.; DeLuca, L.; Behr, H.; Michaelides, A. Cross-National Outcomes of a Digital Weight Loss Intervention in the United States, Canada, United Kingdom and Ireland, and Australia and New Zealand: A Retrospective Analysis. Front. Public Health 2021, 9, 604937. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wang, X.; Gao, F.; Liao, J.; Zeng, J.; Fan, L. Mobile nutrition and health management platform for perioperative recovery: An interdisciplinary research achievement using WeChat Applet. Front. Med. 2023, 10, 1201866. [Google Scholar] [CrossRef]
- Feng, J.; Liu, H.; Mai, S.; Su, J.; Sun, J.; Zhou, J.; Zhang, Y.; Wang, Y.; Wu, F.; Zheng, G.; et al. Protocol of a parallel, randomized controlled trial on the effects of a novel personalized nutrition approach by artificial intelligence in real world scenario. BMC Public Health 2023, 23, 1700. [Google Scholar] [CrossRef]
- Zhu, Z.; Zang, J.; Wang, Z.; Zou, S.; Jia, X.; Guo, C.; Ma, L.; Xu, D.; Wu, F. Dietary pattern and its seasonal characteristic in residents of Shanghai, 2012–2014. Chin. J. Epidemiol. 2018, 39, 880–885. [Google Scholar] [CrossRef]
- YueXin, Y. China Food Composition Tables Standard Edition, 6th ed.; Peking University Medical Press: Beijing, China, 2018. [Google Scholar]
- Zhu, Z.; Yang, X.; Fang, Y.; Zhang, J.; Yang, Z.; Wang, Z.; Liu, A.; He, L.; Sun, J.; Lian, Y.; et al. Trends and Disparities of Energy Intake and Macronutrient Composition in China: A Series of National Surveys, 1982–2012. Nutrients 2020, 12, 2168. [Google Scholar] [CrossRef]
- Chinese Nutrition Society. Chinese Dietary Guidelines (2022); People’s Medical Publishing House: Beijing, China, 2022. [Google Scholar]
- Carlsohn, A.; Scharhag-Rosenberger, F.; Cassel, M.; Weber, J.; de Guzman Guzman, A.; Mayer, F. Physical activity levels to estimate the energy requirement of adolescent athletes. Pediatr. Exerc. Sci. 2011, 23, 261–269. [Google Scholar] [CrossRef]
- Schofield, W.N. Predicting basal metabolic rate, new standards and review of previous work. Hum. Nutr. Clin. Nutr. 1985, 39 (Suppl. 1), 5–41. [Google Scholar]
- McLean, S.A.; Paxton, S.J.; Wertheim, E.H. A body image and disordered eating intervention for women in midlife: A randomized controlled trial. J. Consult. Clin. Psychol. 2011, 79, 751–758. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Li, Q.; Yang, M.; Jiao, J.; Ma, X.; Zhou, Y.; Song, A.; Heymsfield, S.B.; Zhang, S.; Zhu, S. Lower BMI cutoffs to define overweight and obesity in China. Obesity 2015, 23, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, D.; Heymsfield, S.B.; Heo, M.; Jebb, S.A.; Murgatroyd, P.R.; Sakamoto, Y. Healthy percentage body fat ranges: An approach for developing guidelines based on body mass index. Am. J. Clin. Nutr. 2000, 72, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Ho-Pham, L.T.; Campbell, L.V.; Nguyen, T.V. More on body fat cutoff points. Mayo Clin. Proc. 2011, 86, 584–585. [Google Scholar] [CrossRef]
- Ahmad, S.R. Plant-based diet for obesity treatment. Front. Nutr. 2022, 9, 952553. [Google Scholar] [CrossRef]
- Balk, E.M.; Earley, A.; Raman, G.; Avendano, E.A.; Pittas, A.G.; Remington, P.L. Combined Diet and Physical Activity Promotion Programs to Prevent Type 2 Diabetes Among Persons at Increased Risk: A Systematic Review for the Community Preventive Services Task Force. Ann. Intern. Med. 2015, 163, 437–451. [Google Scholar] [CrossRef]
- Xu, H.; Li, X.; Adams, H.; Kubena, K.; Guo, S. Etiology of Metabolic Syndrome and Dietary Intervention. Int. J. Mol. Sci. 2018, 20, 128. [Google Scholar] [CrossRef]
- Casas, R.; Castro-Barquero, S.; Estruch, R.; Sacanella, E. Nutrition and Cardiovascular Health. Int. J. Mol. Sci. 2018, 19, 3988. [Google Scholar] [CrossRef]
- Glechner, A.; Keuchel, L.; Affengruber, L.; Titscher, V.; Sommer, I.; Matyas, N.; Wagner, G.; Kien, C.; Klerings, I.; Gartlehner, G. Effects of lifestyle changes on adults with prediabetes: A systematic review and meta-analysis. Prim. Care Diabetes 2018, 12, 393–408. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E. The role of the Mediterranean diet on weight loss and obesity-related diseases. Rev. Endocr. Metab. Disord. 2020, 21, 315–327. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Feng, L.; Zeng, G.; Zhu, H.; Sun, J.; Gao, P.; Yuan, J.; Lan, X.; Li, S.; Zhao, Y.; et al. Effects of Cuisine-Based Chinese Heart-Healthy Diet in Lowering Blood Pressure Among Adults in China: Multicenter, Single-Blind, Randomized, Parallel Controlled Feeding Trial. Circulation 2022, 146, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Popp, C.J.; Hu, L.; Kharmats, A.Y.; Curran, M.; Berube, L.; Wang, C.; Pompeii, M.L.; Illiano, P.; St-Jules, D.E.; Mottern, M.; et al. Effect of a Personalized Diet to Reduce Postprandial Glycemic Response vs a Low-fat Diet on Weight Loss in Adults With Abnormal Glucose Metabolism and Obesity: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2233760. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Zang, J.; Luo, B.; Wang, Y.; Zhu, Z.; Wang, Z.; He, X.; Wang, W.; Guo, Y.; Chen, X.; Wang, C.; et al. Eating Out-of-Home in Adult Residents in Shanghai and the Nutritional Differences among Dining Places. Nutrients 2018, 10, 951. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, A.; Finkelstein, E.A.; Levine, E.; Foley, P.; Askew, S.; Steinberg, D.; Bennett, G.G. A Digital Behavioral Weight Gain Prevention Intervention in Primary Care Practice: Cost and Cost-Effectiveness Analysis. J. Med. Internet Res. 2019, 21, e12201. [Google Scholar] [CrossRef] [PubMed]
- Mogensen, C.S.; Faerch, K.; Bruhn, L.; Amadid, H.; Tetens, I.; Quist, J.S.; Clemmensen, K.K.B. Timing and Frequency of Daily Energy Intake in Adults with Prediabetes and Overweight or Obesity and Their Associations with Body Fat. Nutrients 2020, 12, 3484. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Wang, J.; Sun, L.; Gu, W.; Zong, G.; Song, B.; Shen, C.; Zhou, P.; Chen, Y.; Wu, Y.; et al. Isocaloric-restricted Mediterranean Diet and Chinese Diets High or Low in Plants in Adults With Prediabetes. J. Clin. Endocrinol. Metab. 2022, 107, 2216–2227. [Google Scholar] [CrossRef] [PubMed]


| Item (/100 g b) | I | II | III |
|---|---|---|---|
| Fat (g) | <8 | 8–20 | >20 |
| Sodium (mg) | <500 | 500–1000 | >1000 |
| Sugar (g) | <4.5 | 4.5–9.0 | >9.0 |
| ALL | Control | Intervention | p Value | |
|---|---|---|---|---|
| n | 153 | 77 | 76 | |
| Age, years, mean (SD) | 32.7 (7.5) | 32.7 (7.3) | 32.6 (7.8) | 0.963 |
| Sex, n (%) | ||||
| Female | 97 (63.4) | 51 (66.2) | 46 (60.5) | 0.572 |
| Male | 56 (36.6) | 26 (33.8) | 30 (39.5) | |
| Smoking status, n (%) | ||||
| Non-smoker | 136 (88.9) | 69 (89.6) | 67 (88.2) | 0.945 |
| Ex-smoker | 11 (7.2) | 5 (6.5) | 6 (7.9) | |
| current Smoker | 6 (3.9) | 3 (3.9) | 3 (3.9) | |
| Alcohol consumption, n (%) | ||||
| Lifetime abstainer | 67 (43.8) | 34 (44.2) | 33 (43.4) | 0.865 |
| Non-heavy drinker | 68 (44.4) | 35 (45.4) | 33 (43.4) | |
| Heavy drinker | 18 (11.8) | 8 (10.4) | 10 (13.2) | |
| Daily physical activity level, n (%) | ||||
| Low | 134 (87.6) | 70 (90.9) | 64 (84.2) | 0.341 |
| Moderate | 18 (11.8) | 7 (9.1) | 11 (14.5) | |
| Vigorous | 1 (0.6) | 0 (0.0) | 1 (1.3) | |
| Intentional physical exercise, n (%) | ||||
| No | 118 (77.1) | 58 (75.3) | 60 (78.9) | 0.733 |
| Yes | 35 (22.9) | 19 (24.7) | 16 (21.1) | |
| Enrollment sequence, n (%) | ||||
| September | 23 (15.0) | 10 (13.0) | 13 (17.1) | 0.535 |
| October | 86 (56.2) | 42 (54.5) | 44 (57.9) | |
| November | 44 (28.8) | 25 (32.5) | 19 (25.0) | |
| Lunch consumption, mean (SD) | ||||
| Food group, g/meal | ||||
| Plant foods | 222.9 (98.0) | 225.9 (94.8) | 219.8 (101.6) | 0.701 |
| Cereals and Tubers | 52.0 (35.6) | 51.4 (35.7) | 52.63 (35.7) | 0.827 |
| Vegetables and Fruits | 161.0 (94.7) | 163.9 (94.0) | 158.0 (96.0) | 0.698 |
| Soybeans and soybean products | 8.5 (12.4) | 8.3 (12.2) | 8.7 (12.7) | 0.830 |
| Animal foods | 126.6 (55.9) | 124.8 (51.4) | 128.4 (60.4) | 0.691 |
| Livestock and poultry meat | 84.2 (57.9) | 79.4 (56.3) | 89.0 (59.5) | 0.308 |
| Aquatic products | 32.9 (50.3) | 35.8 (50.2) | 30.0 (50.6) | 0.475 |
| Eggs | 9.6 (23.6) | 9.7 (24.9) | 9.5 (22.4) | 0.969 |
| Animal/plant food ratio | 0.7 (0.6) | 0.7 (0.7) | 0.7 (0.5) | 0.679 |
| Energy, kcal/meal | 676.1 (223.7) | 666.3 (207.3) | 685.9 (240.1) | 0.589 |
| Percentage of energy intake from fat | 0.5 (0.1) | 0.5 (0.1) | 0.5(0.1) | 0.616 |
| Nutrients | ||||
| Protein, g/meal | 31.9 (11.8) | 31.8 (12.2) | 32.0 (11.5) | 0.929 |
| Fat, g/meal | 35.9 (15.5) | 35.1 (14.5) | 36.7 (16.4) | 0.525 |
| Carbohydrate, g/meal | 51.2 (21.8) | 51.0 (21.9) | 51.3 (21.9) | 0.921 |
| Cholesterol, mg/meal | 163.4 (168.1) | 164.7 (176.0) | 162.1 (160.8) | 0.925 |
| Sodium, mg/meal | 2017.4 (925.1) | 1954.2 (916.9) | 2081.5 (935.0) | 0.396 |
| Calcium, mg/meal | 189.6 (119.4) | 199.2 (122.5) | 179.9 (116.2) | 0.321 |
| Iron, mg/meal | 6.7 (4.7) | 6.3 (2.6) | 7.1 (6.1) | 0.311 |
| Zinc, mg/meal | 5.0 (2.6) | 5.0 (2.8) | 5.0 (2.5) | 0.936 |
| Vitamin C, mg/meal | 37.6 (31.6) | 39.7 (33.6) | 35.6 (29.5) | 0.420 |
| Anthropometric measurement, mean (SD) | ||||
| Body Weight, kg | 64.5 (14.0) | 62.9 (14.0) | 66.2 (14.0) | 0.151 |
| BMI, kg/m2 | 23.2 (3.7) | 22.6 (3.8) | 23.9 (3.6) | 0.033 |
| Blood pressure, mmHg | ||||
| Systolic pressure | 115.6 (16.1) | 114.8 (15.4) | 116.3 (16.9) | 0.575 |
| Diastolic pressure | 75.8 (11.2) | 75.2 (10.8) | 76.5 (11.6) | 0.488 |
| Body composition | ||||
| Percentage of body fat, % | 28.3 (6.5) | 27.8 (6.8) | 28.9 (6.1) | 0.276 |
| Percentage of torso fat, % | 28.9 (6.6) | 28.0 (7.0) | 29.7 (6.0) | 0.112 |
| Visceral fat rank | 6.7 (3.8) | 6.2 (3.7) | 7.2 (3.8) | 0.105 |
| Missing, n (%) | 2 (1.3) | 2 (2.6) | 0 (0.0) |
| Time × Group a | ||||
|---|---|---|---|---|
| Model 1 b | Model 2 c | |||
| β d | p | β d | p | |
| Food group, g/meal | ||||
| Plant foods | 3.23 | 0.061 | 3.26 | 0.057 |
| Cereals and Tubers | 0.08 | 0.847 | 0.07 | 0.870 |
| Vegetables and fruits | 3.26 | 0.054 | 3.22 | 0.055 |
| Soybeans and soybean products | 0.02 | 0.933 | 0.03 | 0.881 |
| Animal foods | −1.32 | 0.183 | −1.26 | 0.199 |
| Livestock and poultry meat | −1.75 | 0.046 | −1.80 | 0.035 |
| Aquatic products | 0.60 | 0.405 | 0.63 | 0.378 |
| Eggs | −0.53 | 0.184 | −0.51 | 0.202 |
| Animal/plant food ratio | −0.03 | 0.025 | −0.03 | 0.024 |
| Energy, kcal/meal | −3.92 | 0.143 | −4.06 | 0.130 |
| Percentage of energy intake from fat, % | 0.00 | 0.180 | 0.00 | 0.152 |
| Nutrients | ||||
| Protein, g/meal | −0.14 | 0.340 | −0.15 | 0.296 |
| Fat, g/meal | −0.36 | 0.054 | −0.38 | 0.041 |
| Carbohydrate, g/meal | −0.07 | 0.746 | −0.07 | 0.748 |
| Cholesterol, mg/meal | −3.87 | 0.053 | −3.97 | 0.048 |
| Sodium, mg/meal | −3.62 | 0.765 | −4.40 | 0.718 |
| Calcium, mg/meal | 2.29 | 0.125 | 2.37 | 0.115 |
| Iron, mg/meal | −0.03 | 0.539 | −0.04 | 0.431 |
| Zinc, mg/meal | 0.00 | 0.894 | −0.01 | 0.818 |
| Vitamin C, mg/meal | 0.14 | 0.653 | 0.03 | 0.933 |
| Time × Group a | ||||
|---|---|---|---|---|
| Model 1 b | Model 2 c | |||
| β d | p | β d | p | |
| Body weight, kg | −0.40 | 0.099 | −0.43 | 0.074 |
| BMI, kg/m2 | −0.16 | 0.142 | −0.19 | 0.091 |
| Blood pressure, mmHg | ||||
| Systolic pressure | 0.26 | 0.847 | −0.08 | 0.955 |
| Diastolic pressure | 1.38 | 0.118 | 1.32 | 0.135 |
| Body composition | ||||
| Percentage of body fat, % | −0.31 | 0.371 | −0.31 | 0.375 |
| Percentage of torso fat, % | −0.20 | 0.633 | −0.25 | 0.542 |
| Visceral fat index | −0.16 | 0.350 | −0.14 | 0.402 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, H.; Feng, J.; Shi, Z.; Su, J.; Sun, J.; Wu, F.; Zhu, Z. Effects of a Novel Applet-Based Personalized Dietary Intervention on Dietary Intakes: A Randomized Controlled Trial in a Real-World Scenario. Nutrients 2024, 16, 565. https://doi.org/10.3390/nu16040565
Liu H, Feng J, Shi Z, Su J, Sun J, Wu F, Zhu Z. Effects of a Novel Applet-Based Personalized Dietary Intervention on Dietary Intakes: A Randomized Controlled Trial in a Real-World Scenario. Nutrients. 2024; 16(4):565. https://doi.org/10.3390/nu16040565
Chicago/Turabian StyleLiu, Hongwei, Jingyuan Feng, Zehuan Shi, Jin Su, Jing Sun, Fan Wu, and Zhenni Zhu. 2024. "Effects of a Novel Applet-Based Personalized Dietary Intervention on Dietary Intakes: A Randomized Controlled Trial in a Real-World Scenario" Nutrients 16, no. 4: 565. https://doi.org/10.3390/nu16040565
APA StyleLiu, H., Feng, J., Shi, Z., Su, J., Sun, J., Wu, F., & Zhu, Z. (2024). Effects of a Novel Applet-Based Personalized Dietary Intervention on Dietary Intakes: A Randomized Controlled Trial in a Real-World Scenario. Nutrients, 16(4), 565. https://doi.org/10.3390/nu16040565






