Assessing Discriminant Validity through Structural Equation Modeling: The Case of Eating Compulsivity
Abstract
1. Introduction
1.1. Food Addiction
1.2. Measures of FA: Overlap and Differences
1.3. Discriminant Validity
1.4. On the Importance of Discriminant Validity
1.5. Assessing Discriminant Validity
1.6. Research Gap
1.7. Aim and Research Hypotheses
2. Materials and Methods
2.1. Measures
2.2. Data Analysis Strategy
2.2.1. Preliminary Analysis
2.2.2. Discriminant Validity
2.3. Sample Size Determination
3. Results
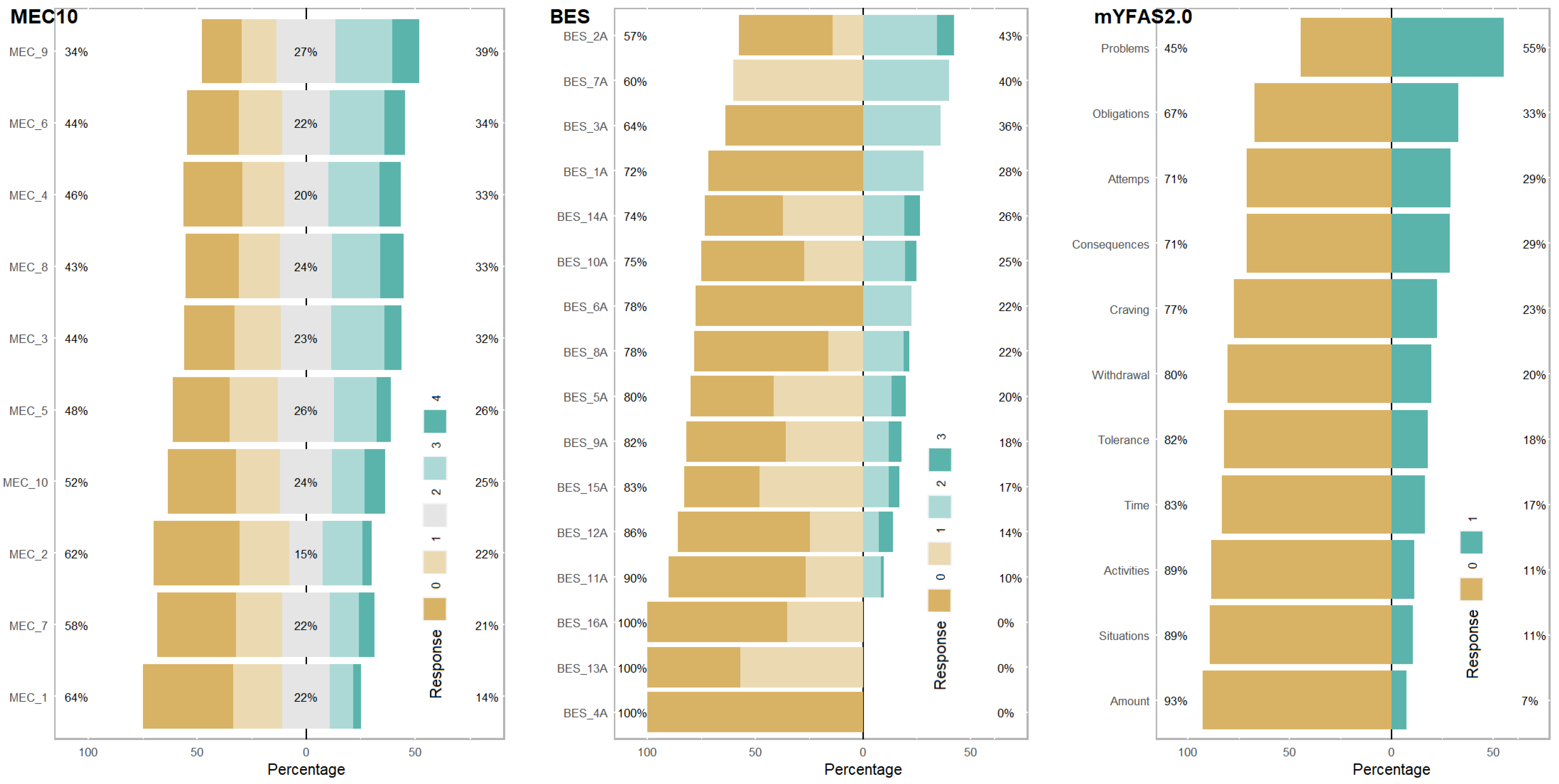
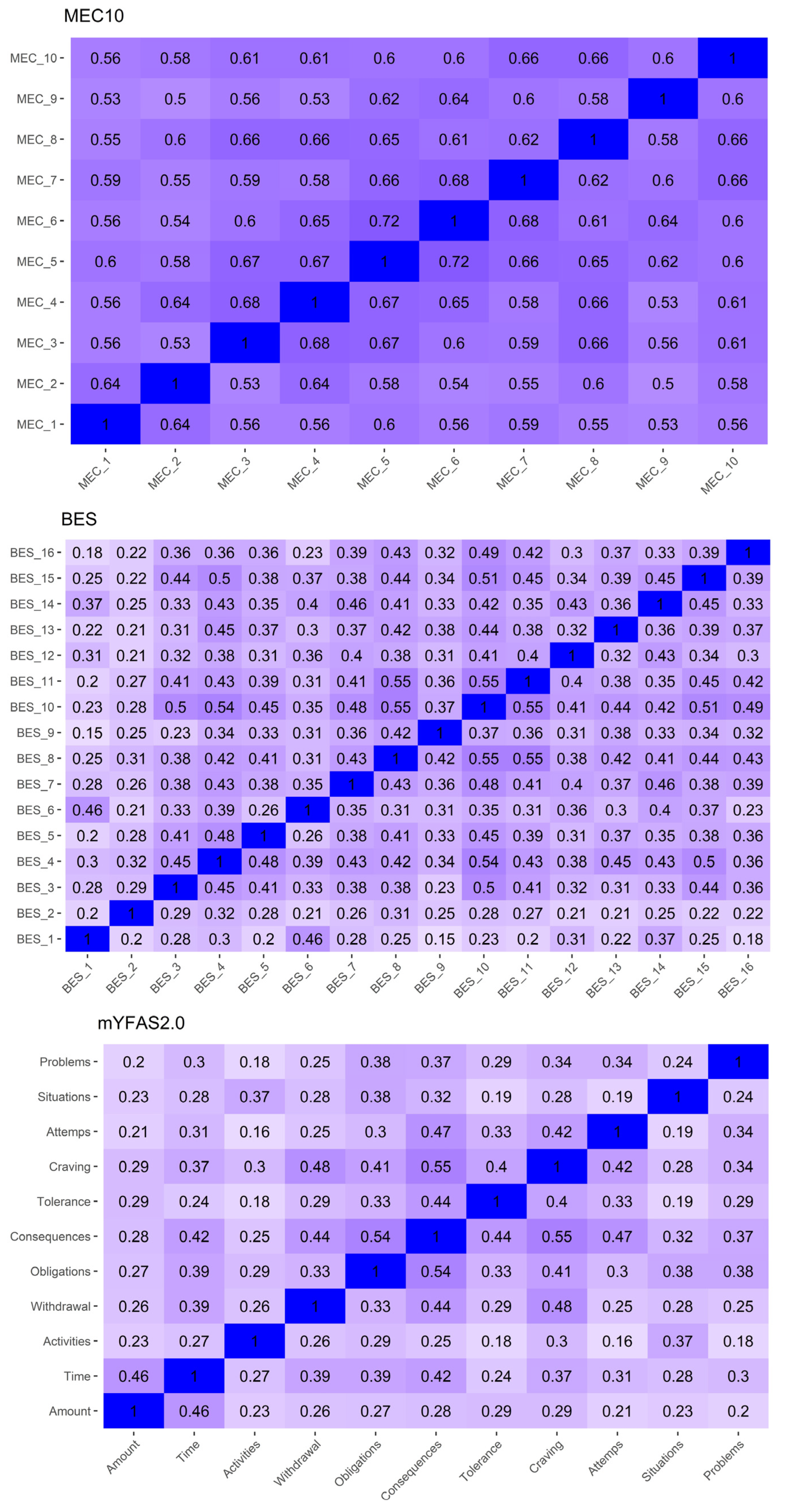
3.1. Preliminary Analysis
3.1.1. Participants
3.1.2. Item Properties
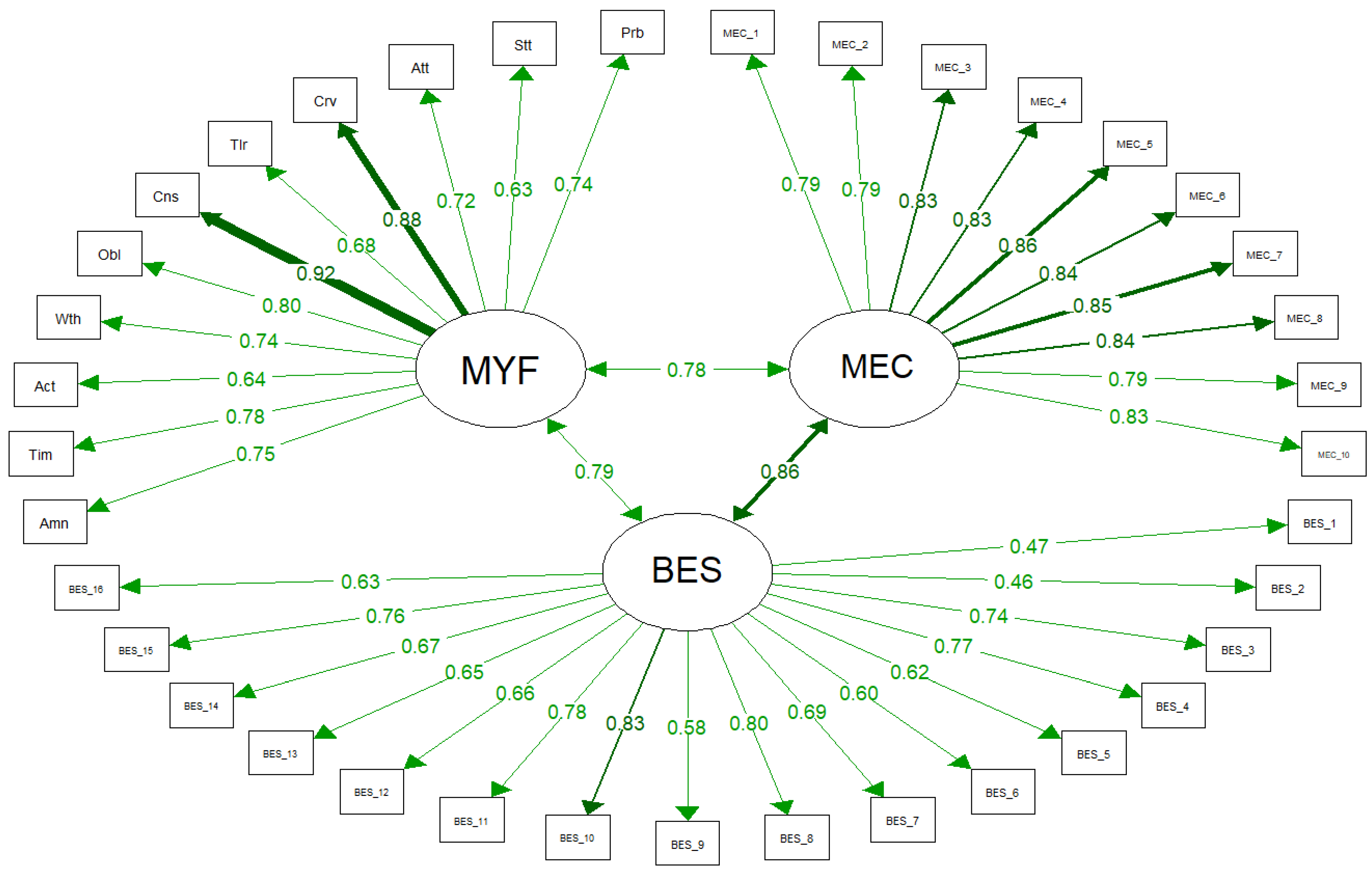
3.2. Assessing Discriminant Validity through SEM
3.2.1. Unconstrained Model: ρxx(Cut) and CIxx(Cut)
MEC10 and BES
mYFAS2.0 and MEC10
mYFAS2.0 and BES
3.2.2. Comparison of the Unconstrained and Constrained Models: χ2(cut) and CFI(cut)
MEC10 and BES
mYFAS2.0 and MEC10
mYFAS2.0 and BES
4. Discussions
4.1. FA and BED: Constructs Differences
4.2. MEC10 or BES?
4.3. Limitations
4.4. Strengths
4.5. Future Research
4.6. Further Methodological Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global Nutrition Transition and the Pandemic of Obesity in Developing Countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef]
- GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef]
- Davis, C.; Curtis, C.; Levitan, R.D.; Carter, J.C.; Kaplan, A.S.; Kennedy, J.L. Evidence That ‘Food Addiction’ Is a Valid Phenotype of Obesity. Appetite 2011, 57, 711–717. [Google Scholar] [CrossRef]
- Yau, Y.H.C.; Leeman, R.F.; Potenza, M.N. Biological Underpinning of Behavioural Addictions and Management Implications. In Textbook of Addiction Treatment: International Perspectives; el-Guebaly, N., Carrà, G., Galanter, M., Eds.; Springer: Milan, Italy, 2015; pp. 1411–1442. ISBN 978-88-470-5322-9. [Google Scholar]
- Gearhardt, A.N.; White, M.A.; Masheb, R.M.; Morgan, P.T.; Crosby, R.D.; Grilo, C.M. An Examination of the Food Addiction Construct in Obese Patients with Binge Eating Disorder. Int. J. Eat. Disord. 2012, 45, 657–663. [Google Scholar] [CrossRef]
- Linardon, J.; Messer, M. Assessment of Food Addiction Using the Yale Food Addiction Scale 2.0 in Individuals with Binge-Eating Disorder Symptomatology: Factor Structure, Psychometric Properties, and Clinical Significance. Psychiatry Res. 2019, 279, 216–221. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Rossi, A.; Pietrabissa, G.; Mannarini, S.; Fabbricatore, M.; Imperatori, C.; Innamorati, M.; Gearhardt, A.N.; Castelnuovo, G. Structural Validity, Measurement Invariance, Reliability and Diagnostic Accuracy of the Italian Version of the Yale Food Addiction Scale 2.0 in Patients with Severe Obesity and the General Population. Eat. Weight Disord. 2021, 26, 345–366. [Google Scholar] [CrossRef]
- Murphy, C.M.; Stojek, M.K.; MacKillop, J. Interrelationships among Impulsive Personality Traits, Food Addiction, and Body Mass Index. Appetite 2014, 73, 45–50. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Rossi, A.; Pietrabissa, G.; Varallo, G.; Molinari, E.; Poggiogalle, E.; Donini, L.M.; Tarrini, G.; Melchionda, N.; Piccione, C.; et al. Validation of the Italian Yale Food Addiction Scale in Postgraduate University Students. Eat. Weight Disord. 2018, 23, 167–176. [Google Scholar] [CrossRef]
- Meule, A.; Hermann, T.; Kübler, A. Food Addiction in Overweight and Obese Adolescents Seeking Weight-Loss Treatment. Eur. Eat. Disord. Rev. 2015, 23, 193–198. [Google Scholar] [CrossRef]
- Meule, A.; Gearhardt, A.N. Food Addiction in the Light of DSM-5. Nutrients 2014, 6, 3653–3671. [Google Scholar] [CrossRef]
- Pursey, K.M.; Stanwell, P.; Gearhardt, A.N.; Collins, C.E.; Burrows, T.L. The Prevalence of Food Addiction as Assessed by the Yale Food Addiction Scale: A Systematic Review. Nutrients 2014, 6, 4552–4590. [Google Scholar] [CrossRef]
- Schulte, E.M.; Smeal, J.K.; Gearhardt, A.N. Foods Are Differentially Associated with Subjective Effect Report Questions of Abuse Liability. PLoS ONE 2017, 12, e0184220. [Google Scholar] [CrossRef]
- MacLean, P.S.; Blundell, J.E.; Mennella, J.A.; Batterham, R.L. Biological Control of Appetite: A Daunting Complexity. Obesity 2017, 25, S8–S16. [Google Scholar] [CrossRef]
- Jiménez-Murcia, S.; Granero, R.; Wolz, I.; Baño, M.; Mestre-Bach, G.; Steward, T.; Agüera, Z.; Hinney, A.; Diéguez, C.; Casanueva, F.F.; et al. Food Addiction in Gambling Disorder: Frequency and Clinical Outcomes. Front. Psychol. 2017, 8, 473. [Google Scholar] [CrossRef]
- Rogers, P.J. Food and Drug Addictions: Similarities and Differences. Pharmacol. Biochem. Behav. 2017, 153, 182–190. [Google Scholar] [CrossRef]
- Brewerton, T.D. Food Addiction as a Proxy for Eating Disorder and Obesity Severity, Trauma History, PTSD Symptoms, and Comorbidity. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2017, 22, 241–247. [Google Scholar] [CrossRef]
- Nolan, L.J. Is It Time to Consider the “Food Use Disorder?”. Appetite 2017, 115, 16–18. [Google Scholar] [CrossRef]
- Bastianelli, A.; Vicentini, M.; Spoto, A.; Vidotto, G. Un modello di equazioni strutturali per lo studio dei fattori di rischio nel mantenimento del disturbo da alimentazione incontrollata. G. Ital. Med. Lav. Ergon. 2007, 29, B50–B55. [Google Scholar]
- di Giacomo, E.; Aliberti, F.; Pescatore, F.; Santorelli, M.; Pessina, R.; Placenti, V.; Colmegna, F.; Clerici, M. Disentangling Binge Eating Disorder and Food Addiction: A Systematic Review and Meta-Analysis. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2022, 27, 1963–1970. [Google Scholar] [CrossRef]
- Imperatori, C.; Innamorati, M.; Lamis, D.A.; Contardi, A.; Continisio, M.; Castelnuovo, G.; Manzoni, G.M.; Fabbricatore, M. Factor Structure of the Binge Eating Scale in a Large Sample of Obese and Overweight Patients Attending Low Energy Diet Therapy. Eur. Eat. Disord. Rev. 2016, 24, 174–178. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Preliminary Validation of the Yale Food Addiction Scale. Appetite 2009, 52, 430–436. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Development of the Yale Food Addiction Scale Version 2.0. Psychol. Addict. Behav. 2016, 30, 113–121. [Google Scholar] [CrossRef]
- Schulte, E.M.; Gearhardt, A.N. Development of the Modified Yale Food Addiction Scale Version 2.0. Eur. Eat. Disord. Rev. 2017, 25, 302–308. [Google Scholar] [CrossRef]
- Meule, A.; Gearhardt, A.N. Ten Years of the Yale Food Addiction Scale: A Review of Version 2.0. Curr. Addict. Rep. 2019, 6, 218–228. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Schroder, R.; Sellman, J.D.; Adamson, S. Development and Validation of a Brief Measure of Eating Compulsivity (MEC). Subst. Use Misuse 2017, 52, 1918–1924. [Google Scholar] [CrossRef]
- Rossi, A.A.; Pietrabissa, G.; Gearhardt, A.N.; Musetti, A.; Castelnuovo, G.; Mannarini, S. Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Version of the Measure of Eating Compulsivity (MEC10-IT). Nutrients 2023, 15, 1378. [Google Scholar] [CrossRef]
- Netemeyer, R.G.; Bearden, W.O.; Sharma, S. Scaling Procedures: Issues and Applications; SAGE Publications: Newbury Park, CA, USA, 2003; ISBN 978-1-5063-2018-2. [Google Scholar]
- Campbell, D.T.; Fiske, D.W. Convergent and Discriminant Validation by the Multitrait-Multimethod Matrix. Psychol. Bull. 1959, 56, 81–105. [Google Scholar] [CrossRef]
- Roemer, E.; Schuberth, F.; Henseler, J. HTMT2–an Improved Criterion for Assessing Discriminant Validity in Structural Equation Modeling. Ind. Manag. Data Syst. 2021, 121, 2637–2650. [Google Scholar] [CrossRef]
- McDonald, R.P. Factor Analysis and Related Methods; Erlbaum: Hillsdale, NJ, USA, 1985; Volume 12, p. 308. [Google Scholar]
- Rönkkö, M.; Cho, E. An Updated Guideline for Assessing Discriminant Validity. Organ. Res. Methods 2022, 25, 6–14. [Google Scholar] [CrossRef]
- Gelman, A. More on Replication Crisis. Available online: https://statmodeling.stat.columbia.edu/2016/03/03/more-on-replication-crisis/ (accessed on 22 September 2023).
- Loken, E.; Gelman, A. Measurement Error and the Replication Crisis. Science 2017, 355, 584–585. [Google Scholar] [CrossRef]
- Flake, J.K.; Fried, E.I. Measurement Schmeasurement: Questionable Measurement Practices and How to Avoid Them. Adv. Methods Pract. Psychol. Sci. 2020, 3, 456–465. [Google Scholar] [CrossRef]
- Gonzalez, O.; MacKinnon, D.P.; Muniz, F.B. Extrinsic Convergent Validity Evidence to Prevent Jingle and Jangle Fallacies. Multivar. Behav. Res. 2021, 56, 3–19. [Google Scholar] [CrossRef]
- Shaffer, J.A.; DeGeest, D.; Li, A. Tackling the Problem of Construct Proliferation: A Guide to Assessing the Discriminant Validity of Conceptually Related Constructs. Organ. Res. Methods 2016, 19, 80–110. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A New Criterion for Assessing Discriminant Validity in Variance-Based Structural Equation Modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Rossi, A.; Mannarini, S.; Castelnuovo, G.; Pietrabissa, G. Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT). Nutrients 2023, 15, 104. [Google Scholar] [CrossRef] [PubMed]
- Ricca, V.; Mannucci, E.; Moretti, S.; Di Bernardo, M.; Zucchi, T.; Cabras, P.L.; Rotella, C.M. Screening for Binge Eating Disorder in Obese Outpatients. Compr. Psychiatry 2000, 41, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Marcus, M.D.; Wing, R.R.; Hopkins, J. Obese Binge Eaters: Affect, Cognitions, and Response to Behavioral Weight Control. J. Consult. Clin. Psychol. 1988, 56, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Duarte, C.; Pinto-Gouveia, J.; Ferreira, C. Expanding Binge Eating Assessment: Validity and Screening Value of the Binge Eating Scale in Women from the General Population. Eat. Behav. 2015, 18, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Gormally, J.; Black, S.; Daston, S.; Rardin, D. The Assessment of Binge Eating Severity among Obese Persons. Addict. Behav. 1982, 7, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Freitas, S.R.; Lopes, C.S.; Appolinario, J.C.; Coutinho, W. The Assessment of Binge Eating Disorder in Obese Women: A Comparison of the Binge Eating Scale with the Structured Clinical Interview for the DSM-IV. Eat. Behav. 2006, 7, 282–289. [Google Scholar] [CrossRef]
- Grupski, A.E.; Hood, M.M.; Hall, B.J.; Azarbad, L.; Fitzpatrick, S.L.; Corsica, J.A. Examining the Binge Eating Scale in Screening for Binge Eating Disorder in Bariatric Surgery Candidates. Obes. Surg. 2013, 23, 1–6. [Google Scholar] [CrossRef]
- Imperatori, C.; Fabbricatore, M.; Lester, D.; Manzoni, G.M.; Castelnuovo, G.; Raimondi, G.; Innamorati, M. Psychometric Properties of the Modified Yale Food Addiction Scale Version 2.0 in an Italian Non-Clinical Sample. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2019, 24, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Pursey, K.M.; Gearhardt, A.N.; Burrows, T.L. The Relationship between “Food Addiction” and Visceral Adiposity in Young Females. Physiol. Behav. 2016, 157, 9–12. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2023. [Google Scholar]
- RStudio Team. RStudio: Integrated Development for R; RStudio Team: Boston, MA, USA, 2023. [Google Scholar]
- Revelle, W. Package “psych”—Procedures for Psychological, Psychometric and Personality Research; R Package: Vienna, Austria, 2015; pp. 1–358. [Google Scholar]
- Wickham, H.; Francois, R.; Henry, L.; Müller, K.; Vaughan, D. Dplyr: A Grammar of Data Manipulation; R Package: Vienna, Austria, 2023. [Google Scholar]
- Wickham, H. Reshaping Data with the Reshape Package. J. Stat. Softw. 2007, 21, 1–20. [Google Scholar] [CrossRef]
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016; ISBN 978-3-319-24277-4. [Google Scholar]
- Heinzen, E.; Sinnwell, J.; Atkinson, E.; Gunderson, T.; Dougherty, G.; Votruba, P.; Lennon, R.; Hanson, A.; Goergen, K.; Lundt, E.; et al. Arsenal: An Arsenal of “R” Functions for Large-Scale Statistical Summaries; R Package: Vienna, Austria, 2021. [Google Scholar]
- Rosseel, Y. Lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Jorgensen, T.D. Package “semTools”. Useful Tools for Structural Equation Modeling; R Package: Vienna, Austria, 2018. [Google Scholar]
- Epskamp, S. semPlot: Unified Visualizations of Structural Equation Models. Struct. Equ. Model. Multidiscip. J. 2015, 22, 474–483. [Google Scholar] [CrossRef]
- Bryer, J.; Speerschneider, K. Likert: Analysis and Visualization Likert Items; R Package: Vienna, Austria, 2016. [Google Scholar]
- Flora, D.B. Your Coefficient Alpha Is Probably Wrong, but Which Coefficient Omega Is Right? A Tutorial on Using R to Obtain Better Reliability Estimates. Adv. Methods Pract. Psychol. Sci. 2020, 3, 484–501. [Google Scholar] [CrossRef]
- Lord, F.M.; Novick, M.R.; Birnbaum, A. Statistical Theories of Mental Test Scores; Statistical theories of mental test scores; Addison-Wesley: Oxford, UK, 1968. [Google Scholar]
- Sijtsma, K. On the Use, the Misuse, and the Very Limited Usefulness of Cronbach’s Alpha. Psychometrika 2009, 74, 107–120. [Google Scholar] [CrossRef]
- Woodhouse, B.; Jackson, P.H. Lower Bounds for the Reliability of the Total Score on a Test Composed of Non-Homogeneous Items: II: A Search Procedure to Locate the Greatest Lower Bound. Psychometrika 1977, 42, 579–591. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Hoyle, R.H. Handbook of Structural Equation Modeling; Guilford Press: New York, NY, USA, 2012; ISBN 978-1-60918-230-4. [Google Scholar]
- Kline, P. Introduction to Psychometric Design; Routledge: London, UK, 2015; ISBN 978-1-315-69599-0. [Google Scholar]
- Lionetti, F.; Keijsers, L.; Dellagiulia, A.; Pastore, M. Evidence of Factorial Validity of Parental Knowledge, Control and Solicitation, and Adolescent Disclosure Scales: When the Ordered Nature of Likert Scales Matters. Front. Psychol. 2016, 7, 941. [Google Scholar] [CrossRef] [PubMed]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 1998. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Muthén, B.O.; Asparouhov, T. Latent Variable Analysis with Categorical Outcomes: Multiple-Group And Growth Modeling In Mplus. Mplus Web Notes 2002, 4, 1–22. [Google Scholar]
- Rossi, A.A.; Pietrabissa, G.; Tagliagambe, A.; Scuderi, A.; Montecchiani, L.; Castelnuovo, G.; Mannarini, S.; Dalla Ragione, L. Many Facets of Eating Disorders: Profiling Key Psychological Features of Anorexia Nervosa and Binge Eating Disorder. Behav. Sci. 2023, 13, 276. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, R. Measurement Issues in Health-Related Quality of Life: Challenges for Health Psychology. Psychol. Health 2000, 15, 99–108. [Google Scholar] [CrossRef]
- Bottesi, G.; Spoto, A.; Freeston, M.H.; Sanavio, E.; Vidotto, G. Beyond the Score: Clinical Evaluation through Formal Psychological Assessment. J. Pers. Assess. 2015, 97, 252–260. [Google Scholar] [CrossRef]
- Panzeri, A.; Komici, K.; Cerutti, P.; Sacco, D.; Pistono, M.; Ferrario, S.R. Gender Differences and Long-Term Outcome of over 75 Elderlies in Cardiac Rehabilitation: Highlighting the Role of Psychological and Physical Factors through a Secondary Analysis of a Cohort Study. Eur. J. Phys. Rehabil. Med. 2021, 57, 288–297. [Google Scholar] [CrossRef]
- Bastianelli, A.; Spoto, A.; Vidotto, G. Social Network Analysis and Eating Disorders: A Study Concerning Blogs. G. Ital. Med. Lav. Ergon. 2011, 33, B5–B13. [Google Scholar]
- Panzeri, A.; Bettinardi, O.; Bottesi, G.; Bertolotti, G.; Brambatti, L.; Monfredo, M.; Mignemi, G.; Bruno, G.; Vidotto, G.; Spoto, A.; et al. Assessment of Perceived Support in the Context of Emergency: Development and Validation of the Psycho-Social Support Scale. Curr. Psychol. 2022, 12, 22514–22525. [Google Scholar] [CrossRef]
- Bennett, K.M.; Panzeri, A.; Derrer-Merk, E.; Butter, S.; Hartman, T.K.; Mason, L.; McBride, O.; Murphy, J.; Shevlin, M.; Gibson-Miller, J.; et al. Predicting Resilience during the COVID-19 Pandemic in the United Kingdom: Cross-Sectional and Longitudinal Results. PLoS ONE 2023, 18, e0283254. [Google Scholar] [CrossRef]
- Flake, J.K.; Pek, J.; Hehman, E. Construct Validation in Social and Personality Research: Current Practice and Recommendations. Soc. Psychol. Personal. Sci. 2017, 8, 370–378. [Google Scholar] [CrossRef]
- Beleigoli, A.M.; Andrade, A.Q.; Cançado, A.G.; Paulo, M.N.; Diniz, M.D.F.H.; Ribeiro, A.L. Web-Based Digital Health Interventions for Weight Loss and Lifestyle Habit Changes in Overweight and Obese Adults: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2019, 21, e9609. [Google Scholar] [CrossRef] [PubMed]
- Moghimi, E.; Davis, C.; Rotondi, M. The Efficacy of eHealth Interventions for the Treatment of Adults Diagnosed with Full or Subthreshold Binge Eating Disorder: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2021, 23, e17874. [Google Scholar] [CrossRef] [PubMed]
- Moravcová, K.; Karbanová, M.; Bretschneider, M.P.; Sovová, M.; Ožana, J.; Sovová, E. Comparing Digital Therapeutic Intervention with an Intensive Obesity Management Program: Randomized Controlled Trial. Nutrients 2022, 14, 2005. [Google Scholar] [CrossRef]
- Panzeri, A.; Rossi Ferrario, S. Supporting Rehabilitation Patients with COVID-19 during the Pandemic: Experiences from a Technology-Based Psychological Approach. In Proceedings of the CEUR Workshop Proceedings: Second Symposium on Psychology-Based Technologies—Psychobit, Naples, Italy, 28–29 September 2020; Volume 2730. [Google Scholar]
- Rossi Ferrario, S.; Panzeri, A.; Pistono, M.; Ferrario, S.R.; Panzeri, A.; Pistono, M. Psychological Difficulties of LVAD Patients and Caregivers: A Follow up over 1 Year from Discharge. Artif. Organs 2021, 46, 479–490. [Google Scholar] [CrossRef]
- Heggestad, E.D.; Banks George, C.; Monroe Hausfeld, M.; Tonidandel, S.; Williams, E.B. Scale Adaptation in Organizational Science Research: A Review and Best-Practice Recommendations. J. Manag. 2019, 45, 2596–2627. [Google Scholar] [CrossRef]
| Males (n 314) | Females (n 403) | Total (n = 717) | |
|---|---|---|---|
| Age | |||
| Mean (SD) | 54.557 (12.401) | 52.924 (13.138) | 53.628 (12.842) |
| Range | 18–87 | 18–80 | 18–87 |
| Weight in kg | |||
| Mean (SD) | 130.872 (24.523) | 110.288 (19.471) | 118.876 (23.963) |
| Range | 82.600–270 | 70–220.200 | 70–270 |
| Height in meters | |||
| Mean (SD) | 1.736 (0.074) | 1.594 (0.075) | 1.653 (0.102) |
| Range | 1.500–1.950 | 1.400–1.830 | 1.400–1.950 |
| Body Mass Index | |||
| Mean (SD) | 43.345 (7.132) | 43.332 (6.395) | 43.337 (6.707) |
| Range | 35.077–86.182 | 35.156–83.210 | 35.077–86.182 |
| MEC10 | |||
| Mean (SD) | 14.571 (9.834) | 16.649 (10.595) | 15.745 (10.315) |
| Range | 0–37 | 0–40 | 0–40 |
| BES | |||
| Mean (SD) | 25.667 (7.626) | 28.536 (8.849) | 27.287 (8.454) |
| Range | 15–52 | 15–57 | 15–57 |
| mYFAS2.0 | |||
| Mean (SD) | 2.231 (2.449) | 2.756 (2.889) | 2.527 (2.717) |
| Range | 0–11 | 0–11 | 0–11 |
| n (%) | Males (n 314) | Females (n 403) | Total (n = 717) |
| FA diagnosis | |||
| No FA | 241 (77.2%) | 287 (70.9%) | 528 (73.6%) |
| FA | 71 (22.8%) | 118 (29.1%) | 189 (26.4%) |
| Severity of FA diagnosis | |||
| Mild FA | 17 (23.9%) | 21 (17.8%) | 38 (20.1%) |
| Moderate FA | 22 (31.0%) | 30 (25.4%) | 52 (27.5%) |
| Severe FA | 32 (45.1%) | 67 (56.8%) | 99 (52.4%) |
| Only FA diagnosis | |||
| Not only FA | 276 (88.5%) | 369 (91.1%) | 645 (90.0%) |
| Only FA | 36 (11.5%) | 36 (8.9%) | 72 (10.0%) |
| BED diagnosis | |||
| No BED | 248 (79.5%) | 280 (69.1%) | 528 (73.6%) |
| BED | 64 (20.5%) | 125 (30.9%) | 189 (26.4%) |
| Only BED diagnosis | |||
| Not only BED | 283 (90.7%) | 362 (89.4%) | 645 (90.0%) |
| Only BED | 29 (9.3%) | 43 (10.6%) | 72 (10.0%) |
| MEC10 | Mean | sd | Median | Min | Max | Range | Skew | Kurtosis |
|---|---|---|---|---|---|---|---|---|
| MEC_1 | 1.126 | 1.172 | 1 | 0 | 4 | 4 | 0.698 | −0.562 |
| MEC_2 | 1.250 | 1.260 | 1 | 0 | 4 | 4 | 0.561 | −0.995 |
| MEC_3 | 1.725 | 1.278 | 2 | 0 | 4 | 4 | 0.081 | −1.163 |
| MEC_4 | 1.700 | 1.349 | 2 | 0 | 4 | 4 | 0.135 | −1.262 |
| MEC_5 | 1.582 | 1.244 | 2 | 0 | 4 | 4 | 0.220 | −1.042 |
| MEC_6 | 1.766 | 1.313 | 2 | 0 | 4 | 4 | 0.060 | −1.212 |
| MEC_7 | 1.344 | 1.289 | 1 | 0 | 4 | 4 | 0.544 | −0.862 |
| MEC_8 | 1.756 | 1.328 | 2 | 0 | 4 | 4 | 0.099 | −1.183 |
| MEC_9 | 1.985 | 1.286 | 2 | 0 | 4 | 4 | −0.137 | −1.059 |
| MEC_10 | 1.512 | 1.322 | 1 | 0 | 4 | 4 | 0.380 | −1.024 |
| BES | mean | sd | median | min | max | range | skew | kurtosis |
| BES_1 | 2.384 | 0.987 | 2 | 1 | 4 | 3 | 0.020 | −1.068 |
| BES_2 | 2.071 | 1.049 | 2 | 1 | 4 | 3 | 0.279 | −1.388 |
| BES_3 | 1.639 | 0.936 | 1 | 1 | 4 | 3 | 1.416 | 0.953 |
| BES_4 | 2.059 | 0.936 | 2 | 1 | 4 | 3 | 0.587 | −0.523 |
| BES_5 | 1.877 | 0.877 | 2 | 1 | 4 | 3 | 0.822 | −0.008 |
| BES_6 | 1.722 | 0.683 | 2 | 1 | 3 | 2 | 0.413 | −0.849 |
| BES_7 | 1.636 | 0.940 | 1 | 1 | 4 | 3 | 1.385 | 0.815 |
| BES_8 | 1.619 | 0.884 | 1 | 1 | 4 | 3 | 1.062 | −0.251 |
| BES_9 | 1.773 | 0.876 | 2 | 1 | 4 | 3 | 0.979 | 0.187 |
| BES_10 | 1.827 | 0.928 | 2 | 1 | 4 | 3 | 0.757 | −0.565 |
| BES_11 | 1.473 | 0.704 | 1 | 1 | 4 | 3 | 1.368 | 1.185 |
| BES_12 | 1.589 | 0.883 | 1 | 1 | 4 | 3 | 1.459 | 1.203 |
| BES_13 | 1.778 | 0.980 | 1 | 1 | 4 | 3 | 1.121 | 0.158 |
| BES_14 | 1.971 | 0.919 | 2 | 1 | 4 | 3 | 0.608 | −0.546 |
| BES_15 | 1.870 | 0.809 | 2 | 1 | 4 | 3 | 0.808 | 0.332 |
| BES_16 | 1.749 | 0.768 | 2 | 1 | 4 | 3 | 0.497 | −1.033 |
| mYFAS2.0 | mean | sd | median | min | max | range | skew | kurtosis |
| Amount | 0.074 | 0.262 | 0 | 0 | 1 | 1 | 3.250 | 8.576 |
| Time | 0.167 | 0.374 | 0 | 0 | 1 | 1 | 1.778 | 1.164 |
| Activities | 0.114 | 0.318 | 0 | 0 | 1 | 1 | 2.418 | 3.854 |
| Withdrawal | 0.197 | 0.398 | 0 | 0 | 1 | 1 | 1.523 | 0.321 |
| Obligations | 0.329 | 0.470 | 0 | 0 | 1 | 1 | 0.726 | −1.475 |
| Consequences | 0.289 | 0.453 | 0 | 0 | 1 | 1 | 0.931 | −1.136 |
| Tolerance | 0.179 | 0.383 | 0 | 0 | 1 | 1 | 1.675 | 0.808 |
| Craving | 0.226 | 0.418 | 0 | 0 | 1 | 1 | 1.308 | −0.290 |
| Attempts | 0.291 | 0.455 | 0 | 0 | 1 | 1 | 0.916 | −1.163 |
| Situations | 0.107 | 0.310 | 0 | 0 | 1 | 1 | 2.531 | 4.411 |
| Problems | 0.554 | 0.497 | 1 | 0 | 1 | 1 | −0.216 | −1.956 |
| MEC10 Loadings | BES Loadings | mYFAS2.0 Loadings | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item | MEC10 | BES | mYFAS2.0 | r2 | Item | MEC10 | BES | mYFAS2.0 | r2 | Item | MEC10 | BES | mYFAS2.0 | r2 |
| MEC_1 | 0.793 | 0 | 0 | 0.629 | BES_1 | 0 | 0.465 | 0 | 0.217 | Amount | 0 | 0 | 0.752 | 0.566 |
| MEC_2 | 0.789 | 0 | 0 | 0.622 | BES_2 | 0 | 0.460 | 0 | 0.211 | Time | 0 | 0 | 0.780 | 0.608 |
| MEC_3 | 0.831 | 0 | 0 | 0.690 | BES_3 | 0 | 0.741 | 0 | 0.549 | Activities | 0 | 0 | 0.642 | 0.412 |
| MEC_4 | 0.833 | 0 | 0 | 0.694 | BES_4 | 0 | 0.772 | 0 | 0.596 | Withdrawal | 0 | 0 | 0.740 | 0.547 |
| MEC_5 | 0.855 | 0 | 0 | 0.731 | BES_5 | 0 | 0.624 | 0 | 0.390 | Obligations | 0 | 0 | 0.802 | 0.644 |
| MEC_6 | 0.838 | 0 | 0 | 0.703 | BES_6 | 0 | 0.602 | 0 | 0.363 | Consequences | 0 | 0 | 0.917 | 0.842 |
| MEC_7 | 0.853 | 0 | 0 | 0.728 | BES_7 | 0 | 0.686 | 0 | 0.471 | Tolerance | 0 | 0 | 0.685 | 0.469 |
| MEC_8 | 0.836 | 0 | 0 | 0.698 | BES_8 | 0 | 0.803 | 0 | 0.644 | Craving | 0 | 0 | 0.881 | 0.777 |
| MEC_9 | 0.787 | 0 | 0 | 0.620 | BES_9 | 0 | 0.579 | 0 | 0.335 | Attempts | 0 | 0 | 0.721 | 0.520 |
| MEC_10 | 0.829 | 0 | 0 | 0.687 | BES_10 | 0 | 0.834 | 0 | 0.696 | Situations | 0 | 0 | 0.633 | 0.400 |
| BES_11 | 0 | 0.782 | 0 | 0.612 | Problems | 0 | 0 | 0.739 | 0.546 | |||||
| BES_12 | 0 | 0.657 | 0 | 0.432 | ||||||||||
| BES_13 | 0 | 0.652 | 0 | 0.426 | ||||||||||
| BES_14 | 0 | 0.671 | 0 | 0.450 | ||||||||||
| BES_15 | 0 | 0.758 | 0 | 0.575 | ||||||||||
| BES_16 | 0 | 0.630 | 0 | 0.396 | ||||||||||
| Unconstrained Model | ||||||
|---|---|---|---|---|---|---|
| Point Std. Estimate | 95% CI | |||||
| Latent Factors | Lower | Upper | Std. Err. | z-Value | p-Value | |
| MEC10 ~~ | - | - | - | - | - | - |
| mYFAS2.0 | 0.783 | 0.766 | 0.799 | 0.008 | 93.394 | <0.001 |
| BES | 0.856 | 0.844 | 0.867 | 0.006 | 148.023 | <0.001 |
| BES ~~ | - | - | - | - | - | - |
| mYFAS2.0 | 0.786 | 0.768 | 0.804 | 0.009 | 85.595 | <0.001 |
| MEC10 ~~ BES Point est. 0.856 95% CI [0.844, 0.867] | Model fit | Model comparison | ||||||||||
| X2 | df | p | CFI | RMSEA | SRMR | ΔX2 | Δdf | p | ΔCFI | ΔRMSEA | DV | |
| Unconstrained model | 940.048 | 626 | <0.001 | 0.998 | 0.026 | 0.048 | - | - | - | - | - | - |
| Constrained at 0.85 | 941.040 | 627 | <0.001 | 0.998 | 0.026 | 0.048 | 0.992 | 1 | 0.319 | 0 | 0 | No |
| Constrained at 0.90 | 996.47 | 627 | <0.001 | 0.997 | 0.029 | 0.049 | 56.425 | 1 | <0.001 | −0.001 | 0.003 | - |
| Constrained at 0.95 | 1184.57 | 627 | <0.001 | 0.996 | 0.035 | 0.051 | 244.53 | 1 | <0.001 | −0.002 | 0.090 | - |
| mYFAS2.0 ~~ MEC10 point est. 0.783 95% CI [0.766, 0.799] | Model fit | Model comparison | ||||||||||
| X2 | df | p | CFI | RMSEA | SRMR | ΔX2 | Δdf | p | ΔCFI | ΔRMSEA | DV | |
| Unconstrained model | 940.048 | 626 | <0.001 | 0.998 | 0.026 | 0.048 | - | - | - | - | - | - |
| Model constr. 0.85 | 999.793 | 627 | <0.001 | 0.997 | 0.029 | 0.050 | 59.745 | 1 | <0.001 | −0.001 | 0.003 | Yes |
| mYFAS2.0 ~~ BES point est. 0.786 95% CI [0.768, 0.804] | Model fit | Model comparison | ||||||||||
| X2 | df | p | CFI | RMSEA | SRMR | ΔX2 | Δdf | p | ΔCFI | ΔRMSEA | DV | |
| Model unconstrained | 940.048 | 626 | <0.001 | 0.998 | 0.026 | 0.048 | - | - | - | - | - | - |
| Constrained at 0.85 | 986.373 | 627 | <0.001 | 0.997 | 0.028 | 0.049 | 46.325 | 1 | <0.001 | −0.001 | 0.002 | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panzeri, A.; Castelnuovo, G.; Spoto, A. Assessing Discriminant Validity through Structural Equation Modeling: The Case of Eating Compulsivity. Nutrients 2024, 16, 550. https://doi.org/10.3390/nu16040550
Panzeri A, Castelnuovo G, Spoto A. Assessing Discriminant Validity through Structural Equation Modeling: The Case of Eating Compulsivity. Nutrients. 2024; 16(4):550. https://doi.org/10.3390/nu16040550
Chicago/Turabian StylePanzeri, Anna, Gianluca Castelnuovo, and Andrea Spoto. 2024. "Assessing Discriminant Validity through Structural Equation Modeling: The Case of Eating Compulsivity" Nutrients 16, no. 4: 550. https://doi.org/10.3390/nu16040550
APA StylePanzeri, A., Castelnuovo, G., & Spoto, A. (2024). Assessing Discriminant Validity through Structural Equation Modeling: The Case of Eating Compulsivity. Nutrients, 16(4), 550. https://doi.org/10.3390/nu16040550






