Association of a High Healthy Eating Index Diet with Long-Term Visceral Fat Loss in a Large Longitudinal Study
Abstract
1. Introduction
2. Methods
2.1. Setting and Recruitment
2.2. Definition of Abdominal Obesity Based on Waist Circumference
2.3. Demographic, Anthropometric, and Biochemical Measurements
2.4. Food and Nutrient Intake Assessments, Dietary Patterns, and Dietary Inflammatory Index
2.5. Modified Healthy Eating Index (MHEI) Definition
2.6. Genetic Factors Related to the Risk of Abdominal Obesity
2.7. Experimental Design for the Machine Learning (ML) Approach for Predicting WC Reduction
2.8. Prediction Model for WC Reduction
2.9. Statistical Analysis
3. Results
3.1. Characteristics of the Participants in the Follow-Up Study
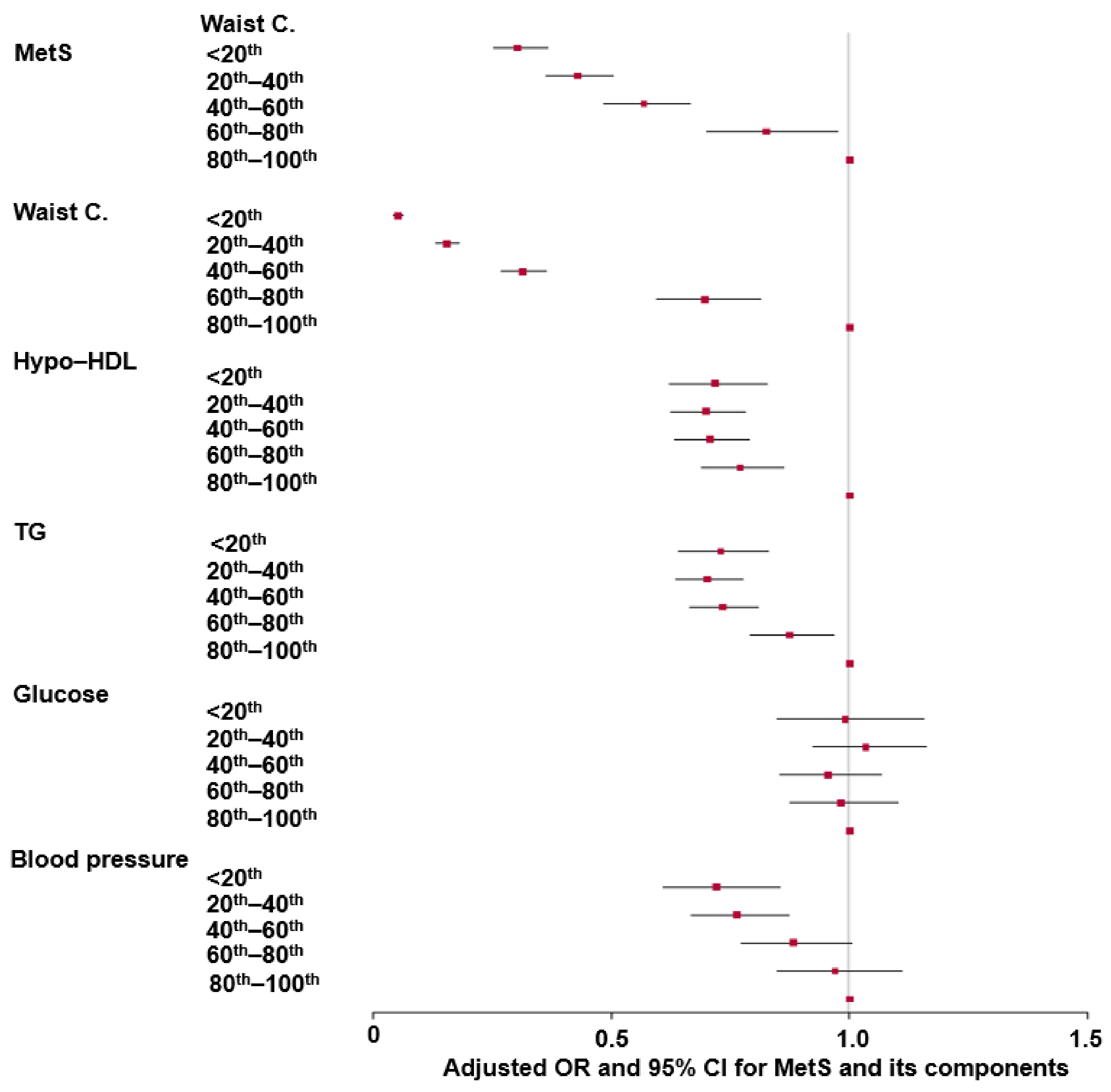
3.2. Association of WC Reduction with Metabolic Syndrome (MetS) and Its Components at the Follow-Up Study
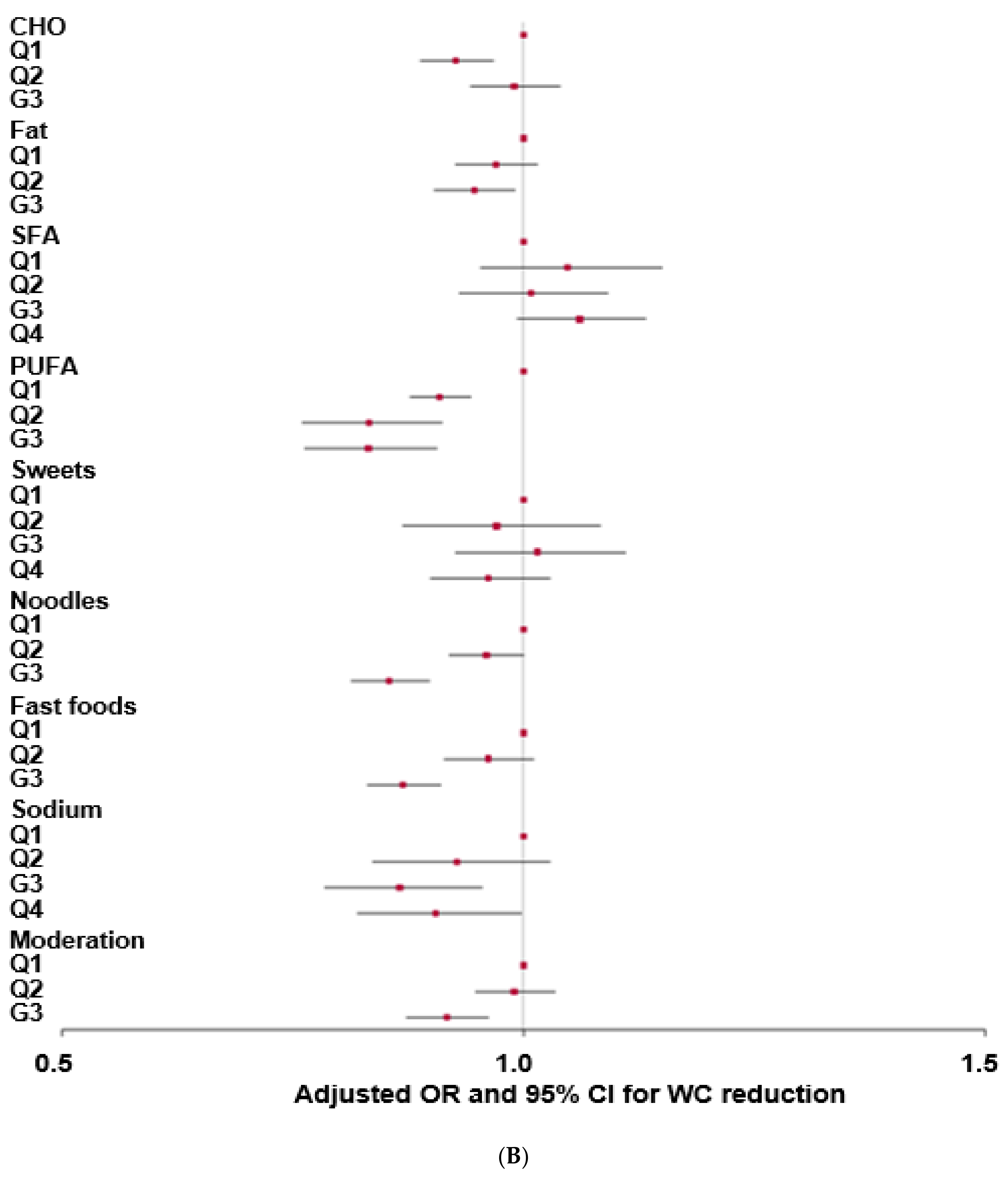
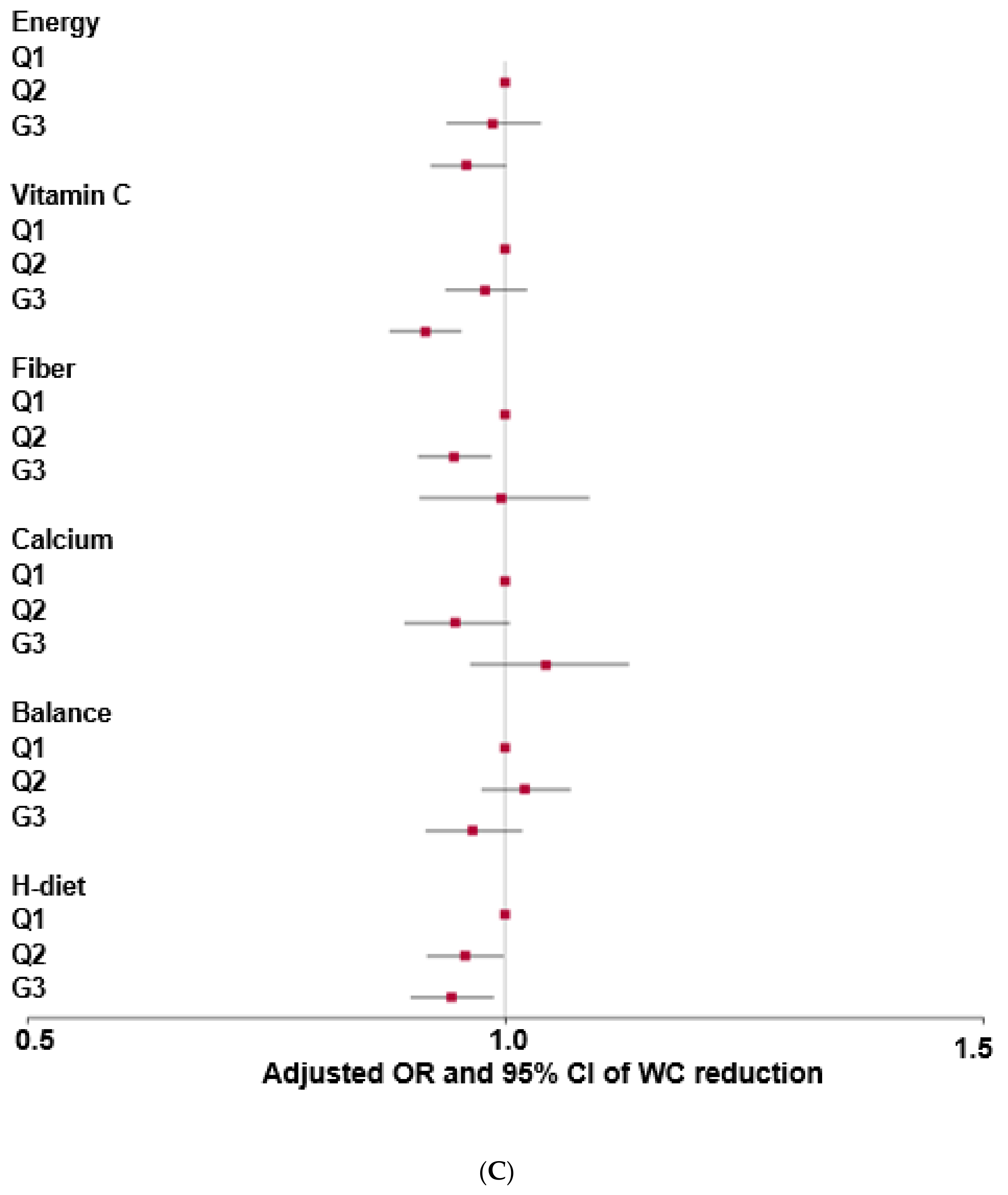
3.3. Effects of Dietary Nutrients on WC Reduction in the Follow-Up Study
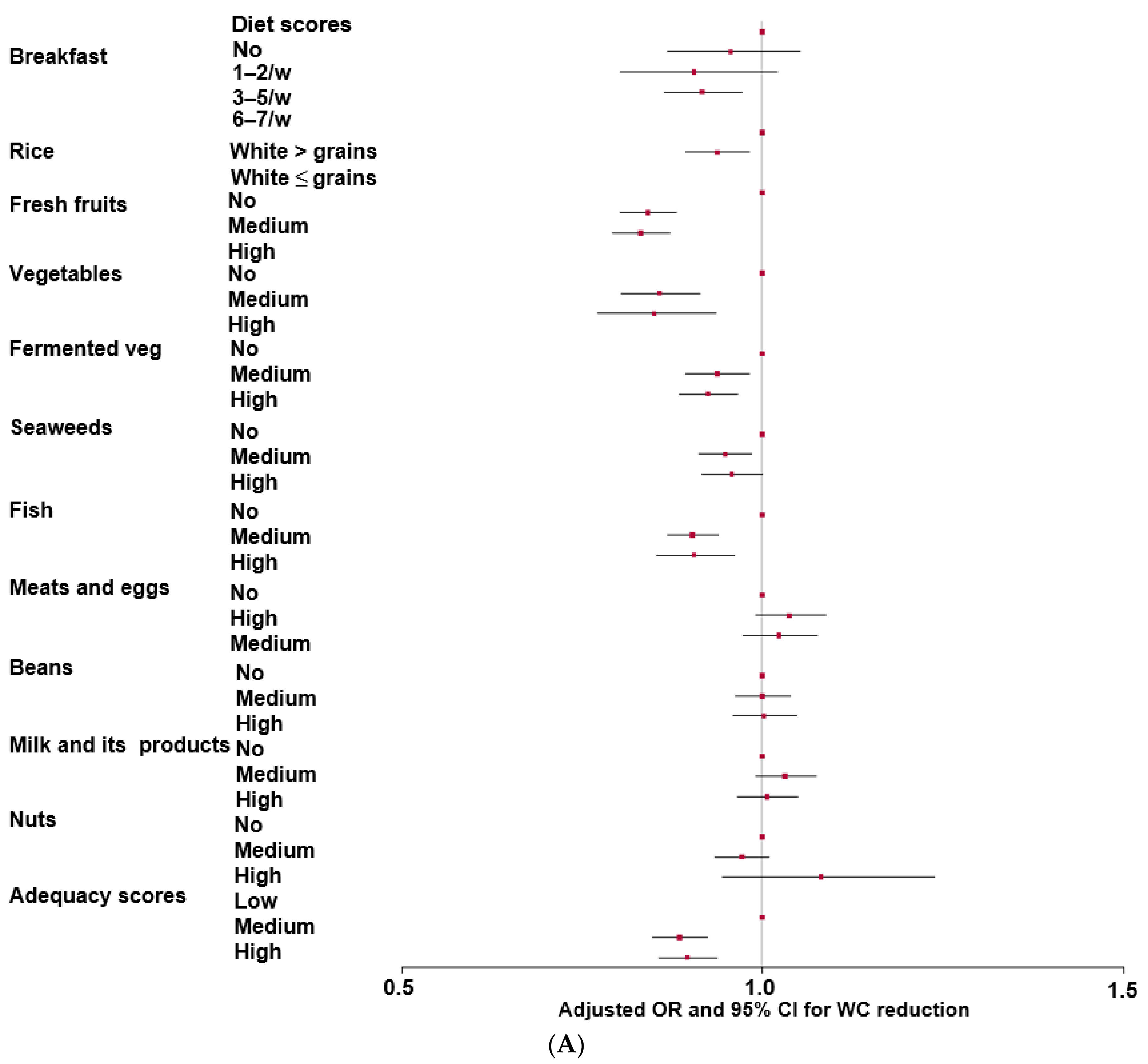
3.4. Impact of MHEI Scores on Decreasing WC in the Follow-Up Study
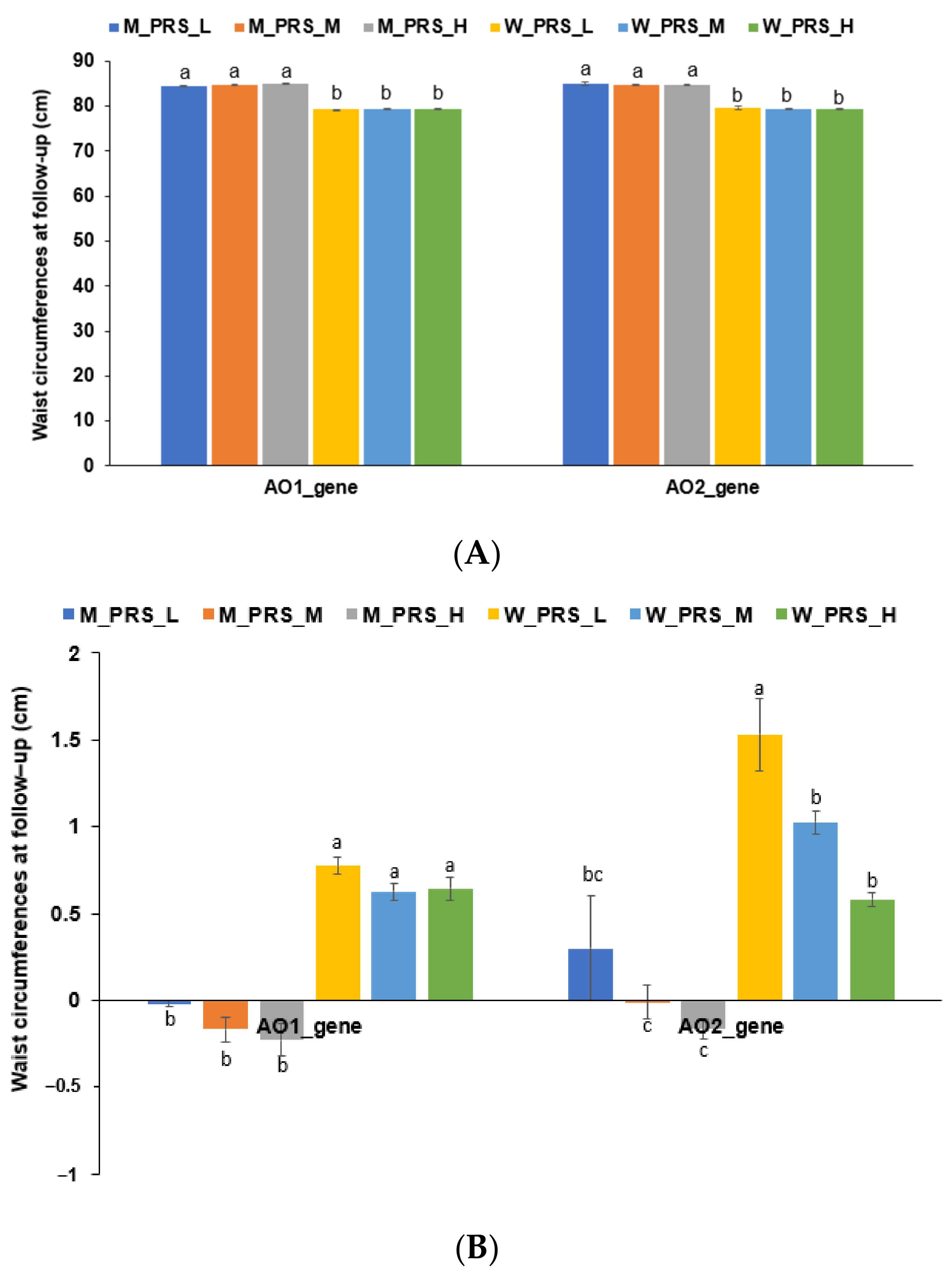
3.5. Genetic Factors
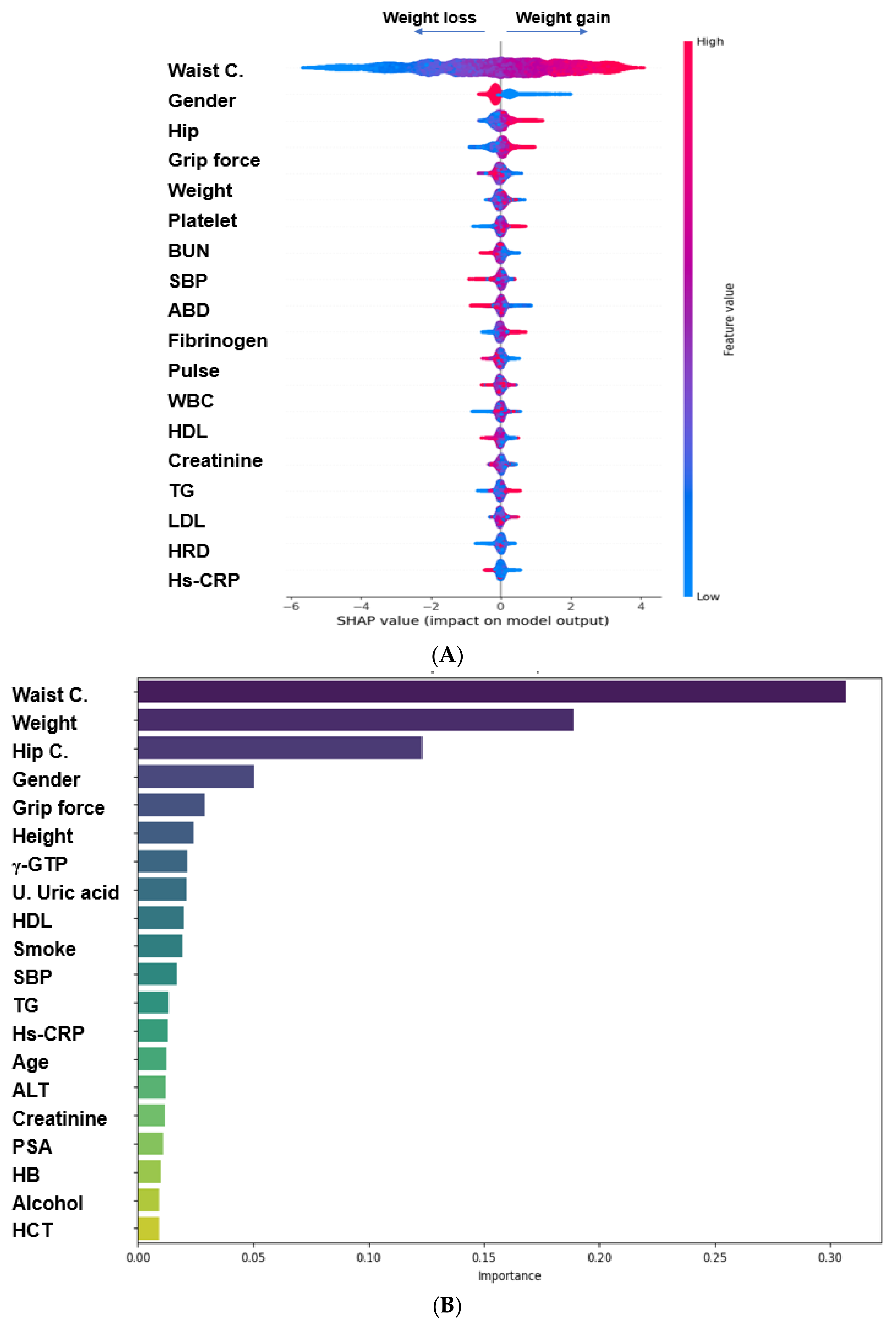
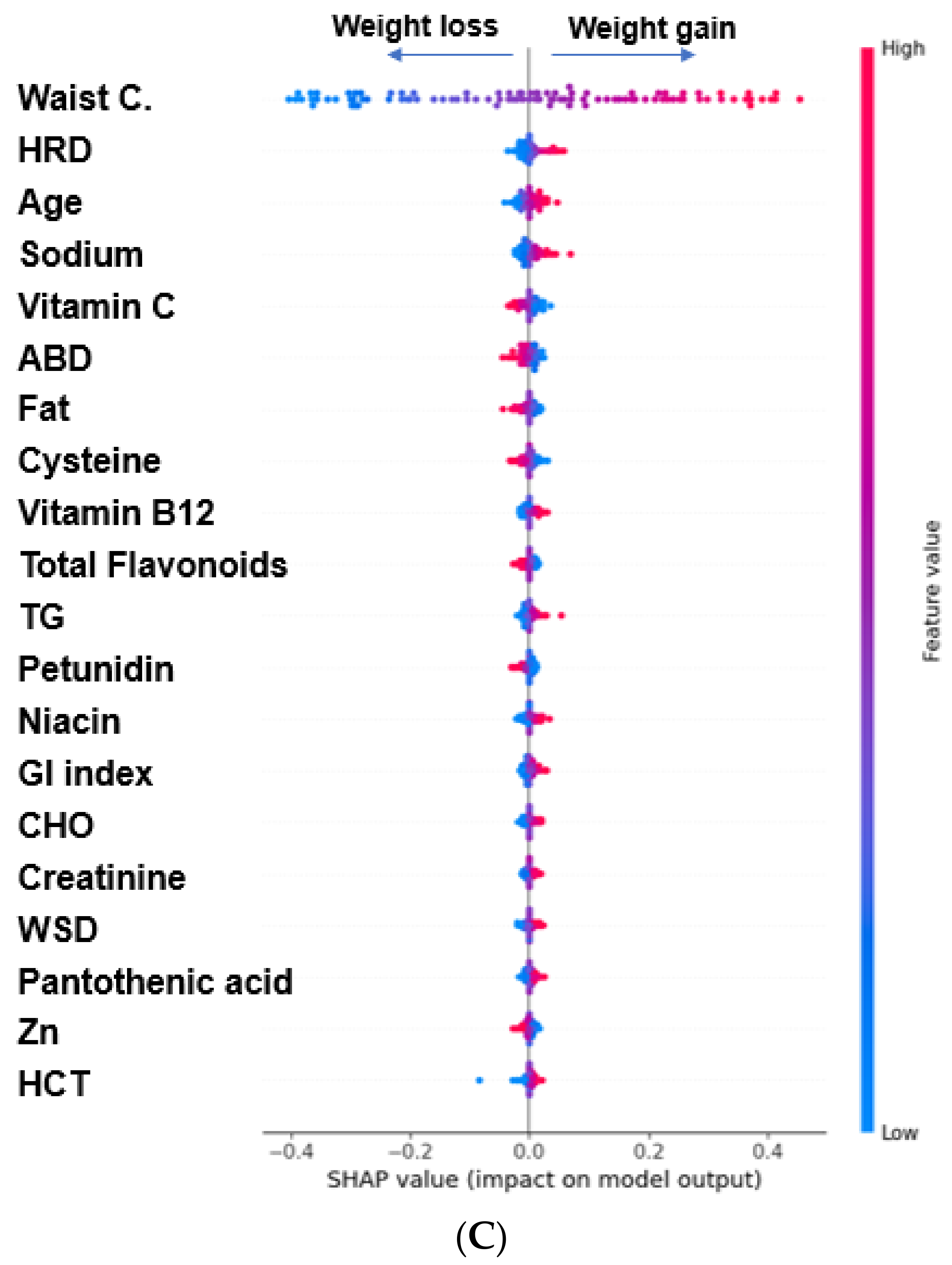
3.6. Prediction of Biomarkers Associated with WC Reductions Using the ML Approach during the Follow-Up Study
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tham, K.W.; Abdul Ghani, R.; Cua, S.C.; Deerochanawong, C.; Fojas, M.; Hocking, S.; Lee, J.; Nam, T.Q.; Pathan, F.; Saboo, B.; et al. Obesity in South and Southeast Asia—A new consensus on care and management. Obes. Rev. 2023, 24, e13520. [Google Scholar] [CrossRef] [PubMed]
- Chait, A.; den Hartigh, L.J. Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front. Cardiovasc. Med. 2020, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Kim, Y.J.; Oh, S.-W.; Lee, C.M.; Choi, H.C.; Joh, H.-K.; Oh, B.; Hwang, S.-S.; Kim, S.J.; Kwon, O.D. Cut-Off Values for Visceral Fat Area Identifying Korean Adults at Risk for Metabolic Syndrome. Korean J. Fam. Med. 2018, 39, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Salas-Salvadó, J.; Ros, E.; Estruch, R.; Corella, D.; Fitó, M.; Martínez-González, M.A. The PREDIMED trial, Mediterranean diet and health outcomes: How strong is the evidence? Nutr. Metab. Cardiovasc. Dis. 2017, 27, 624–632. [Google Scholar] [CrossRef] [PubMed]
- Ellinger, S.; Amini, A.M.; Haardt, J.; Lehmann, A.; Schmidt, A.; Bischoff-Ferrari, H.A.; Buyken, A.E.; Kroke, A.; Kühn, T.; Louis, S.; et al. Protein intake and body weight, fat mass and waist circumference: An umbrella review of systematic reviews for the evidence-based guideline on protein intake of the German Nutrition Society. Eur. J. Nutr. 2024, 63, 3–32. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Kim, M.J.; Hur, H.J.; Lee, B.K.; Kim, M.S.; Park, S. Association between Korean-Style Balanced Diet and Risk of Abdominal Obesity in Korean Adults: An Analysis Using KNHANES-VI (2013–2016). Front. Nutr. 2021, 8, 772347. [Google Scholar] [CrossRef] [PubMed]
- Zamanillo-Campos, R.; Chaplin, A.; Romaguera, D.; Abete, I.; Salas-Salvadó, J.; Martín, V.; Estruch, R.; Vidal, J.; Ruiz-Canela, M.; Babio, N.; et al. Longitudinal association of dietary carbohydrate quality with visceral fat deposition and other adiposity indicators. Clin. Nutr. 2022, 41, 2264–2274. [Google Scholar] [CrossRef]
- Chen, Y.; Kang, M.; Kim, H.; Xu, W.; Lee, J.E. Associations of dietary patterns with obesity and weight change for adults aged 18–65 years: Evidence from the China Health and Nutrition Survey (CHNS). PLoS ONE 2023, 18, e0279625. [Google Scholar] [CrossRef]
- Kim, M.J.; Park, S.; Yang, H.J.; Shin, P.K.; Hur, H.J.; Park, S.J.; Lee, K.H.; Hong, M.; Kim, J.H.; Choi, S.W.; et al. Alleviation of Dyslipidemia via a Traditional Balanced Korean Diet Represented by a Low Glycemic and Low Cholesterol Diet in Obese Women in a Randomized Controlled Trial. Nutrients 2022, 14, 235. [Google Scholar] [CrossRef]
- Jeon, J.; Jung, K.J.; Jee, S.H. Waist circumference trajectories and risk of type 2 diabetes mellitus in Korean population: The Korean genome and epidemiology study (KoGES). BMC Public Health 2019, 19, 741. [Google Scholar] [CrossRef]
- Kim, Y.; Han, B.G. Cohort Profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int. J. Epidemiol. 2017, 46, e20. [Google Scholar] [CrossRef] [PubMed]
- Ahn, Y.; Park, S.J.; Kwack, H.K.; Kim, M.K.; Ko, K.P.; Kim, S.S. Rice-eating pattern and the risk of metabolic syndrome especially waist circumference in Korean Genome and Epidemiology Study (KoGES). BMC Public Health 2013, 13, 61. [Google Scholar] [CrossRef] [PubMed]
- Van Woudenbergh, G.J.; Theofylaktopoulou, D.; Kuijsten, A.; Ferreira, I.; van Greevenbroek, M.M.; van der Kallen, C.J.; Schalkwijk, C.G.; Stehouwer, C.D.; Ocké, M.C.; Nijpels, G.; et al. Adapted dietary inflammatory index and its association with a summary score for low-grade inflammation and markers of glucose metabolism: The Cohort study on Diabetes and Atherosclerosis Maastricht (CODAM) and the Hoorn study. Am. J. Clin. Nutr. 2013, 98, 1533–1542. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.B.; Leak, T.M. Healthy Eating Index Scores, Body Mass Index and Abdominal Obesity Among Asian Americans: NHANES 2011–2018. Front. Epidemiol. 2022, 2, 879264. [Google Scholar] [CrossRef]
- Park, S.; Kang, S. Alcohol, Carbohydrate, and Calcium Intakes and Smoking Interactions with APOA5 rs662799 and rs2266788 were Associated with Elevated Plasma Triglyceride Concentrations in a Cross-Sectional Study of Korean Adults. J. Acad. Nutr. Diet. 2020, 120, 1318–1329.e1311. [Google Scholar] [CrossRef]
- Konikowska, K.; Bombała, W.; Szuba, A.; Różańska, D.; Regulska-Ilow, B. Metabolic Syndrome Is Associated with Low Diet Quality Assessed by the Healthy Eating Index-2015 (HEI-2015) and Low Concentrations of High-Density Lipoprotein Cholesterol. Biomedicines 2022, 10, 2487. [Google Scholar] [CrossRef]
- Kim, H.; Hwang, J.Y.; Kwon, O. Dietary Reference Intakes for Koreans with special consideration to older adults. Nutr. Res. Pract. 2022, 16, S1–S10. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Kwon, H.K.; Park, S. Polygenic Variants Linked to Oxidative Stress and the Antioxidant System Are Associated with Type 2 Diabetes Risk and Interact with Lifestyle Factors. Antioxidants 2023, 12, 1280. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Carvalho, B.; Cutler, D.J.; Arking, D.E.; Chakravarti, A.; Irizarry, R.A. Validation and extension of an empirical Bayes method for SNP calling on Affymetrix microarrays. Genome Biol. 2008, 9, R63. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; He, J.; Lu, X.; Yuan, Y.; Jiang, D.; Xiao, H.; Lin, S.; Xu, L.; Chen, Y. Association of Myopia and Genetic Variants of TGFB2-AS1 and TGFBR1 in the TGF-β Signaling Pathway: A Longitudinal Study in Chinese School-Aged Children. Front. Cell Dev. Biol. 2021, 9, 628182. [Google Scholar] [CrossRef] [PubMed]
- Uma Jyothi, K.; Reddy, B.M. Gene-gene and gene-environment interactions in the etiology of type 2 diabetes mellitus in the population of Hyderabad, India. Meta Gene 2015, 5, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Park, S. Interaction of polygenic variants specific for abdominal obesity risk with energy metabolism in large Korean cohorts. Nutr. Bull. 2022, 47, 307–321. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Park, S. An Inverse Relation between Hyperglycemia and Skeletal Muscle Mass Predicted by Using a Machine Learning Approach in Middle-Aged and Older Adults in Large Cohorts. J. Clin. Med. 2021, 10, 2133. [Google Scholar] [CrossRef] [PubMed]
- Rhee, E.J. The Influence of Obesity and Metabolic Health on Vascular Health. Endocrinol. Metab. 2022, 37, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.J.; Min, K.W. Response: The effects of low-calorie diets on abdominal visceral fat, muscle mass, and dietary quality in obese type 2 diabetic subjects. Korean Diabetes J. 2010, 34, 68–69. [Google Scholar] [CrossRef]
- Kim, J.Y. Optimal Diet Strategies for Weight Loss and Weight Loss Maintenance. J. Obes. Metab. Syndr. 2021, 30, 20–31. [Google Scholar] [CrossRef]
- Witjaksono, F.; Jutamulia, J.; Annisa, N.G.; Prasetya, S.I.; Nurwidya, F. Comparison of low calorie high protein and low calorie standard protein diet on waist circumference of adults with visceral obesity and weight cycling. BMC Res. Notes 2018, 11, 674. [Google Scholar] [CrossRef]
- Salman, H.B.; Salman, M.A.; Yildiz Akal, E. The effect of omega-3 fatty acid supplementation on weight loss and cognitive function in overweight or obese individuals on weight-loss diet. Nutr. Hosp. 2022, 39, 803–813. [Google Scholar] [CrossRef]
- Oliveira, L.D.C.; Morais, G.P.; de Oliveira, F.P.; Mata, M.M.; Veras, A.S.C.; da Rocha, A.L.; Elias, L.L.K.; Teixeira, G.R.; de Moraes, C.; Cintra, D.E.; et al. Intermittent fasting combined with exercise training reduces body mass and alleviates hypothalamic disorders induced by high-fat diet intake. J. Nutr. Biochem. 2023, 119, 109372. [Google Scholar] [CrossRef] [PubMed]
- Kong, Z.; Sun, S.; Shi, Q.; Zhang, H.; Tong, T.K.; Nie, J. Short-Term Ketogenic Diet Improves Abdominal Obesity in Overweight/Obese Chinese Young Females. Front. Physiol. 2020, 11, 856. [Google Scholar] [CrossRef] [PubMed]
- Schutte, S.; Esser, D.; Siebelink, E.; Michielsen, C.J.R.; Daanje, M.; Matualatupauw, J.C.; Boshuizen, H.C.; Mensink, M.; Afman, L.A. Diverging metabolic effects of 2 energy-restricted diets differing in nutrient quality: A 12-week randomized controlled trial in subjects with abdominal obesity. Am. J. Clin. Nutr. 2022, 116, 132–150. [Google Scholar] [CrossRef]
- Akhlaghi, M. Dietary Approaches to Stop Hypertension (DASH): Potential mechanisms of action against risk factors of the metabolic syndrome. Nutr. Res. Rev. 2020, 33, 1–18. [Google Scholar] [CrossRef]
- Tapsell, L.C.; Neale, E.P.; Satija, A.; Hu, F.B. Foods, Nutrients, and Dietary Patterns: Interconnections and Implications for Dietary Guidelines. Adv. Nutr. 2016, 7, 445–454. [Google Scholar] [CrossRef]
- Kim, S.A.; Shin, S.; Ha, K.; Hwang, Y.; Park, Y.H.; Kang, M.S.; Joung, H. Effect of a balanced Korean diet on metabolic risk factors among overweight/obese Korean adults: A randomized controlled trial. Eur. J. Nutr. 2020, 59, 3023–3035. [Google Scholar] [CrossRef] [PubMed]
- Low, D.; Tee, K.X.; Meldrum, O.; D’Agostino, G.; Kim, H.J.; Kang, A.; Yang, Y.; Cheon, B.; Pink, A.; Fong, L.; et al. Four Dietary Patterns Observed within an Elderly Asian Cohort. Curr. Dev. Nutr. 2022, 6, 923. [Google Scholar] [CrossRef]
- Oh, H.Y.; Kim, M.K.; Lee, M.; Kim, Y.O. Macronutrient Composition and Sodium Intake of Diet Are Associated with Risk of Metabolic Syndrome and Hypertension in Korean Women. PLoS ONE 2013, 8, e78088. [Google Scholar] [CrossRef] [PubMed]
- Woo, H.; Han, A.; Park, J.E.; Cha, Y.S. Korean fermented soybean paste (Doenjang) has anti-obesity and anti-hypertensive effects via the renin-angiotensin system (RAS) in high-fat diet-induced obese rats. PLoS ONE 2023, 18, e0291762. [Google Scholar] [CrossRef] [PubMed]
- Kwak, C.S.; Park, S.C.; Song, K.Y. Doenjang, a fermented soybean paste, decreased visceral fat accumulation and adipocyte size in rats fed with high fat diet more effectively than nonfermented soybeans. J. Med. Food 2012, 15, 1–9. [Google Scholar] [CrossRef]

| Men (n = 22,290) | Women (n = 43,321) | |||
|---|---|---|---|---|
| WC-Loss (n = 11,670) | WC-Gain (n = 10,620) | WC-Loss (n = 20,527) | WC-Gain (n = 22,794) | |
| Age (years) | 61.8 ± 0.08 a | 61.2 ± 0.08 b | 57.4 ± 0.06 c | 57.1 ± 0.05 d***+++# |
| Gender [N (%)] 1 | 11,670 (36.3) 1 | 10,620 (31.8) | 20,527 (63.8) | 22,794 (68.2) +++ |
| Duration (years) | 4.87 ± 0.12 | 4.82 ± 0.23 | 4.87 ± 0.22 | 4.80 ± 0.21 |
| Education [N (%)] 1 | ||||
| ≤Middle school | 2754 (23.6) | 2007 (18.9) | 4559 (22.2) | 3899 (17.1) |
| High school | 8182 (70.1) | 7880 (74.2) | 14,584 (71.0) | 17,189 (75.4) |
| ≥Collage | 710 (6.36) | 728 (6.86) +++ | 1383 (6.73) | 1706 (7.48) ++ |
| Waist C changes (cm) | −4.0 ± 0.04 d | 4.18 ± 0.04 b | −4.32 ± 0.03 c | 5.08 ± 0.03 a***+++### |
| Height (cm) | 168.6 ± 0.06 a | 168.5 ± 0.06 a | 156.5 ± 0.04 b | 156.5 ± 0.04 b*** |
| Waist C (cm) | 82.5 ± 0.08 b | 87.2 ± 0.09 a | 76.6 ± 0.06 d | 81.8 ± 0.05 c***+++### |
| Hip C (cm) | 94 ± 0.06 b | 96.2 ± 0.06 a | 91.7 ± 0.04 c | 93.9 ± 0.04 b***+++ |
| BMI (kg/m2) | 23.9 ± 0.03 c | 24.5 ± 0.03 a | 23.4 ± 0.02 d | 24 ± 0.02 b***+++ |
| Hemoglobin (g/dL) | 14.95 ± 0.01 d | 15.08 ± 0.01 c | 13.32 ± 0.01 b | 13.35 ± 0.01 a***+++### |
| Hematocrit (%) | 44.3 ± 0.03 b | 44.6 ± 0.03 a | 40.2 ± 0.02 d | 40.3 ± 0.02 c***+++### |
| MetS [N (%)] 1 | 8770 (45.7) | 1850 (59.7) +++ | 19,931 (51.4) | 2863 (63.2) +++ |
| Glucose (mg/dL) | 103 ± 0.21 a | 102.7 ± 0.22 a | 99 ± 0.15 b | 99.1 ± 0.14 b*** |
| HbA1c (%) | 5.64 ± 0.01 b | 5.64 ± 0.01 b | 5.69 ± 0.01 a | 5.69 ± 0.01 a*** |
| Total cholesterol (mg/dL) | 189 ± 0.4 d | 192 ± 0.42 c | 203 ± 0.28 b | 205 ± 0.27 a***+++ |
| HDL (mg/dL) | 53.8 ± 0.16 c | 52.5 ± 0.17 d | 61 ± 0.11 a | 60.1 ± 0.11 b***+++ |
| LDL (mg/dL) | 111 ± 0.37 d | 113 ± 0.38 c | 118 ± 0.26 b | 120 ± 0.25 a***+++ |
| Triglyceride (mg/dL) | 122 ± 0.77 b | 132 ± 0.81 a | 120 ± 0.54 c | 124 ± 0.52 b***+++### |
| SBP (mmHg) | 124 ± 0.16 b | 126 ± 0.16 a | 121 ± 0.11 d | 123 ± 0.11 c***+++## |
| DBP (mmHg) | 75.9 ± 0.1 b | 77.1 ± 0.11 a | 73.3 ± 0.07 d | 74.1 ± 0.07 c***+++ |
| Creatinine | 0.97 ± 0.003 a | 0.98 ± 0.003 a | 0.7 ± 0.002 b | 0.7 ± 0.002 b***++ |
| BUN (mg/dL) | 16 ± 0.05 a | 15.9 ± 0.05 a | 14.7 ± 0.03 b | 14.7 ± 0.03 b*** |
| eGFR (mL/min/1.73 m2) | 82.8 ± 0.17 c | 82.3 ± 0.18 c | 88.9 ± 0.12 a | 88.5 ± 0.12 b***++ |
| γ-GTP (mg/dL) | 35.4 ± 0.42 b | 37.1 ± 0.44 a | 26.3 ± 0.3 d | 27.4 ± 0.29 c***+++ |
| Fibrinogen (mg/dL) | 305 ± 0.65 b | 302.7 ± 0.67 c | 327.2 ± 0.46 a | 326.3 ± 0.44 a***++ |
| Platelet (Thous/uL) | 232.1 ± 0.64 a | 232.4 ± 0.67 a | 259.6 ± 0.45 c | 262.9 ± 0.43 b |
| Hs-CRP (ng/mL) | 0.13 ± 0.004 a | 0.117 ± 0.004 b | 0.115 ± 0.003 c | 0.114 ± 0.003 c*+# |
| Grip force (N) | 35.4 ± 0.07 a | 35.7 ± 0.07 a | 21.3 ± 0.05 b | 21.3 ± 0.04 b***# |
| MI [N (%)] 1 | 263 (2.25) 1 | 209 (1.97) | 194 (0.95) | 244 (1.07) |
| Stroke [N (%)] 1 | 96 (0.81) 1 | 73 (0.69) | 74 (0.36) | 75 (0.33) |
| CVD [N (%)] 1 | 619 (5.33) 1 | 504 (4.75) + | 542 (2.65) | 507 (2.23) ++ |
| Men (n = 22,290) | Women (n = 43,321) | |||
|---|---|---|---|---|
| WC-Loss (n = 11,670) | WC-Gain (n = 10,620) | WC-Loss (n = 20,527) | WC-Gain (n = 22,794) | |
| Energy intake (EER %) | 85.5 ± 0.3 b | 84.8 ± 0.32 b | 93.5 ± 0.21 a | 94 ± 0.2 a***## |
| Carbohydrate (En%) | 71.4 ± 0.08 a | 71.3 ± 0.08 a | 71 ± 0.05 b | 70.9 ± 0.05 b*** |
| Fat (En%) | 14.3 ± 0.06 b | 14.4 ± 0.06 b | 14.7 ± 0.04 a | 14.8 ± 0.04 a***+ |
| SFA (En%) | 8.04 ± 0.06 a | 8.06 ± 0.06 a | 7.39 ± 0.04 b | 7.44 ± 0.04 b*** |
| MUFA (En%) | 10.3 ± 0.07 a | 10.3 ± 0.08 a | 9.16 ± 0.05 b | 9.3 ± 0.05 b*** |
| PUFA (En%) | 4.87 ± 0.03 a | 4.89 ± 0.03 a | 4.33 ± 0.02 b | 4.38 ± 0.02 b*** |
| Protein (%) | 13.2 ± 0.03 b | 13.1 ± 0.03 b | 13.5 ± 0.02 a | 13.5 ± 0.02 a***+ |
| Fiber (mg/day) | 11.6 ± 0.05 b | 11.6 ± 0.05 b | 12.3 ± 0.03 a | 12.2 ± 0.03 a*** |
| Calcium (mg/day) | 353 ± 1.82 b | 352 ± 1.91 b | 421 ± 1.28 a | 420 ± 1.23 a*** |
| Sodium (g/day) | 1.92 ± 0.01 b | 1.93 ± 0.01 b | 1.97 ± 0.01 a | 1.96 ± 0.01 a*** |
| Potassium (g/day) | 1.88 ± 0.01 b | 1.87 ± 0.01 b | 2.08 ± 0.01 a | 2.08 ± 0.01 a*** |
| Zinc (mg/day) | 7.20 ± 0.02 c | 7.12 ± 0.02 d | 7.53 ± 0.02 a | 7.40 ± 0.01 b***+++ |
| Vitamin C (mg/day) | 84.3 ± 0.52 c | 81.8 ± 0.54 d | 98.9 ± 0.37 a | 97.2 ± 0.35 b***+++ |
| Vitamin B6 (mg/day) | 1.37 ± 0.004 b | 1.36 ± 0.004 b | 1.47 ± 0.002 a | 1.46 ± 0.002 a***++ |
| Niacin (mg/day) | 13.2 ± 0.03 b | 13.1 ± 0.03 b | 13.6 ± 0.02 a | 13.5 ± 0.02 a*** |
| Folate (ug/day) | 177 ± 0.82 c | 175 ± 0.85 d | 199 ± 0.58 a | 197 ± 0.56 b***+++ |
| Vitamin B12 (ug/day) | 6.87 ± 0.05 b | 6.91 ± 0.05 b | 7.89 ± 0.04 a | 7.99 ± 0.04 a*** |
| Pantothenic acid (mg/day) | 2.54 ± 0.01 b | 2.53 ± 0.01 b | 2.92 ± 0.01 a | 2.90 ± 0.01 a*** |
| Vitamin A (RE ug/day) | 396 ± 2.54 c | 390 ± 2.66 c | 445 ± 1.80 a | 438 ± 1.73 b***++ |
| Vitamin D (ug/day) | 29.4 ± 0.27 c | 28.8 ± 0.28 c | 36.8 ± 0.19 a | 36 ± 0.18 b***++ |
| Vitamin K (ug/day) | 53.3 ± 0.62 b | 51.4 ± 0.65 c | 61.1 ± 0.44 a | 60.3 ± 0.42 a***++ |
| DII | −14.3 ± 0.94 a | −14.5 ± 0.82 a | −18.6 ± 0.7 b | −18 ± 0.62 b*** |
| Total flavonoids (ug/day) | 35.4 ± 0.28 b | 34.2 ± 0.29 c | 43.1 ± 0.19 a | 43 ± 0.19 a***++# |
| Glycemic index | 49.2 ± 0.1 b | 49.8 ± 0.1 a | 46.3 ± 0.07 d | 46.8 ± 0.07 c***+++ |
| ABD [N (%)] 1 | 6267 (48.5) | 4059 (46.9) + | 15215 (53.3) | 6480 (51.4) +++ |
| WSD [N (%)] 1 | 5231 (45.4) | 5095 (50.6) +++ | 15537 (52.2) | 6158 (54.2) +++ |
| PBD [N (%)] 1 | 8293 (48.2) | 2033 (46.3) + | 12936 (52.6) | 8759 (52.9) |
| HRD [N (%)] 1 | 6753 (46.2) | 3573 (50.7) +++ | 13998 (52.0) | 7697 (54.1) +++ |
| Coffee (g/day) | 3.95 ± 0.04 b | 4.09 ± 0.04 a | 3.65 ± 0.03 d | 3.84 ± 0.03 c***+++ |
| Alcohol (g/week) | 2.33 ± 0.03 b | 2.65 ± 0.03 a | 0.58 ± 0.02 c | 0.61 ± 0.02 c***+++### |
| Exercise [N (%)] 1 | 7259 (62.2) | 6328 (59.6) +++ | 12,052 (58.7) | 12,780 (56.1) +++ |
| Former smoking | 4994 (44.0) | 4313 (41.4) | 195 (0.97) | 258 (1.16) |
| Smoking [N (%)] 1 | 2788 (24.6) | 2870 (27.6) +++ | 324 (1.61) | 384 (1.72) |
| Classification | Men (n = 22,290) | Women (n = 43,321) | p Value for WC Changes * | p Value for Gender + | ||
|---|---|---|---|---|---|---|
| WC-Loss (n = 11,670) | WC-Gain (n = 10,620) | WC-Loss (n = 20,527) | WC-Gain (n = 22,794) | |||
| Having breakfast | 9.18 (9.11–9.24) a | 9.10 (9.03–9.16) b | 8.63 (8.59–8.68) c | 8.56 (8.52–8.50) c | 0.0025 | <0.0001 |
| Mixed grains intake | 4.14 (4.11–4.18) b | 4.07 (4.03–4.11) c | 4.43 (4.41–4.46) a | 4.41 (4.39–4.44) a | 0.0022 | <0.0001 |
| Total fruit intake | 2.81 (2.77–2.84) c | 2.62 (2.58–2.66) d | 3.76 (3.74–3.79) a | 3.71 (3.69–3.74) b | <0.0001 | <0.0001 |
| Vegetable intake, excluding kimchi and pickled vegetables | 2.57 (2.55–2.59) b | 2.48 (2.46–2.50) c | 3.07 (3.06–3.08) a | 3.07 (3.06–3.08) a | <0.0001 | <0.0001 |
| Fermented vegetable intake | 3.57 (3.53–3.61) a | 3.52 (3.48–3.57) a | 3.38 (3.35–3.41) b | 3.32 (3.30–3.35) c | 0.0013 | <0.0001 |
| Seaweed intake | 2.39 (2.35–2.43) b | 2.33 (2.28–2.37) b | 2.88 (2.86–2.91) a | 2.88 (2.85–2.90) a | 0.0348 | <0.0001 |
| Fish intake | 0.744 (0.708–0.779) c | 0.707 (0.669–0.744) c | 1.613 (1.588–1.638) a | 1.530 (1.506–1.555) b | <0.0001 | <0.0001 |
| Meat and eggs | 2.94 (2.91–2.98) b | 2.94 (2.90–2.97) b | 3.49 (3.47–3.52) a | 3.50 (3.48–3.52) a | 0.8825 | <0.0001 |
| Beans, including fermented beans | 1.01 (0.97–1.05) b | 1.02 (0.98–1.07) b | 2.13 (2.11–2.16) a | 2.13 (2.11–2.16) a | 0.6649 | <0.0001 |
| Milk and milk products | 1.33 (1.29–1.38) b | 1.36 (1.31–1.40) b | 1.94 (1.91–1.97) a | 1.95 (1.92–1.98) a | 0.2577 | <0.0001 |
| Nuts | 2.28 (2.25–2.31) b | 2.25 (2.22–2.28) b | 2.39 (2.37–2.41) a | 2.39 (2.38–2.41) a | 0.1686 | <0.0001 |
| Total MHEI for adequacy | 30.8 (30.7–31.0) c | 30.3 (30.2–30.5) d | 35.2 (35.1–35.3) a | 35.0 (34.9–35.1) b | <0.0001 | <0.0001 |
| Saturated fatty acids (En%) | 8.69 (8.63–8.75) | 8.73 (8.66–8.79) | 8.76 (8.71–8.80) | 8.78 (8.74–8.82) | 0.1890 | 0.0633 |
| Polyunsaturated fatty acids (En%) | 4.31 (4.28–4.33) | 4.29 (4.27–4.32) | 4.26 (4.24–4.28) | 4.26 (4.24–4.27) | 0.3638 | 0.0047 |
| Sodium intake | 8.29 (8.24–8.34) a | 8.26 (8.21–8.31) a | 8.21 (8.17–8.24) b | 8.19 (8.16–8.22) b | 0.2584 | 0.0023 |
| Sweets and beverages (En%) | 6.16 (6.12–6.19) a | 6.12 (6.09–6.16) a | 5.97 (5.95–6.00) b | 5.96 (5.93–5.98) b | 0.0906 | <0.0001 |
| Fast foods (En%) | 3.67 (3.63–3.71) a | 3.54 (3.50–3.58) b | 3.63 (3.60–3.66) a | 3.56 (3.54–3.59) b | <0.0001 | 0.6953 |
| Noodles (En%) | 2.72 (2.69–2.76) c | 2.64 (2.60–2.68) d | 3.01 (2.99–3.04) a | 2.94 (2.92–2.97) b | <0.0001 | <0.0001 |
| Total MHEI for moderation | 45.2 (45.1–45.3) a | 44.9 (44.8–45.1) b | 45.0 (44.9–45.1) a | 44.9 (44.8–45.0) b | <0.0001 | 0.1369 |
| Energy intake | 3.65 (3.61–3.69) a | 3.58 (3.54–3.63) a | 3.49 (3.45–3.52) b | 3.49 (3.46–3.52) b | 0.0579 | <0.001 |
| Vitamin C intake | 2.05 (2.01–2.10) b | 1.96 (1.91–2.00) c | 2.55 (2.52–2.58) a | 2.51 (2.48–2.54) a | <0.0001 | <0.0001 |
| Fiber intake | 0.56 (0.53–0.59) c | 0.58 (0.55–0.61) c | 1.99 (1.97–2.01) a | 1.95 (1.93–1.97) b | 0.4450 | <0.0001 |
| Calcium intake | 0.196 (0.170–0.223) b | 0.211 (0.183–0.239) b | 0.762 (0.743–0.781) a | 0.770 (0.752–0.788) a | 0.2808 | <0.0001 |
| Carbohydrates (En%) | 1.32 (1.28–1.36) b | 1.30 (1.25–1.34) b | 1.55 (1.52–1.58) a | 1.54 (1.51–1.57) a | 0.3171 | <0.0001 |
| Fat (En%) | 3.06 (3.02–3.10) b | 3.09 (3.05–3.13) b | 3.23 (3.21–3.26) a | 3.26 (3.24–3.29) a | 0.0814 | <0.0001 |
| Total MHEI for balance | 10.8 (10.7–10.9) b | 10.7 (10.5–10.8) b | 13.6 (13.6–13.7) a | 13.6 (13.5–13.7) a | 0.0586 | <0.0001 |
| Total MHEI | 86.8 (86.6–87.1) c | 85.9 (85.6–86.1) d | 93.9 (93.7–94.0) a | 93.5 (93.3–93.6) b | <0.0001 | <0.0001 |
| Logistic Regression | XGBoost | Random Forest | DNN | |
|---|---|---|---|---|
| AUROC | 0.793 (0.792–0.794) | 0.866 (0.864–0.867) | 0.795 (0.794–0.795) | 0.811 |
| Accuracy | 0.721 (0.721–0.722) | 0.828 (0.827–0.828) | 0.735 (0.735–0.736) | 0.805 |
| k-fold | 0.721 (0.717–0.725) | 0.845 (0.831–0.860) | 0.766 (0.763–0.770) | 0.78 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S. Association of a High Healthy Eating Index Diet with Long-Term Visceral Fat Loss in a Large Longitudinal Study. Nutrients 2024, 16, 534. https://doi.org/10.3390/nu16040534
Park S. Association of a High Healthy Eating Index Diet with Long-Term Visceral Fat Loss in a Large Longitudinal Study. Nutrients. 2024; 16(4):534. https://doi.org/10.3390/nu16040534
Chicago/Turabian StylePark, Sunmin. 2024. "Association of a High Healthy Eating Index Diet with Long-Term Visceral Fat Loss in a Large Longitudinal Study" Nutrients 16, no. 4: 534. https://doi.org/10.3390/nu16040534
APA StylePark, S. (2024). Association of a High Healthy Eating Index Diet with Long-Term Visceral Fat Loss in a Large Longitudinal Study. Nutrients, 16(4), 534. https://doi.org/10.3390/nu16040534






