Healthy Dietary Pattern Cycling Affects Gut Microbiota and Cardiovascular Disease Risk Factors: Results from a Randomized Controlled Feeding Trial with Young, Healthy Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Participant Recruitment
2.2. Experimental Design
2.3. Outcome Assessments
2.4. Statistics
3. Results
3.1. Participant Recruitment and Baseline Characteristics
3.2. Dietary Intakes
3.3. Gut Microbiota Composition
3.3.1. Community-Level Characteristics
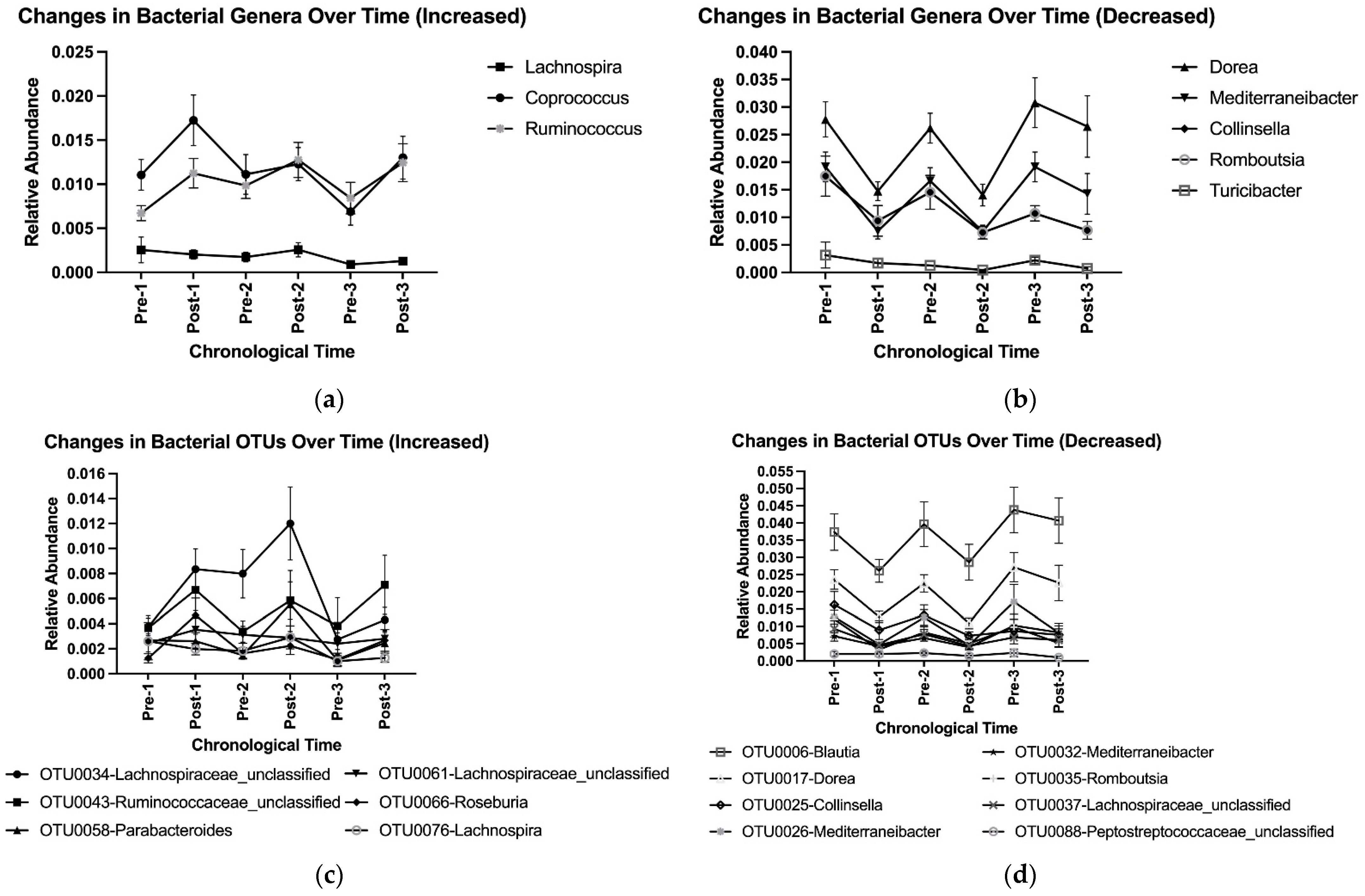
3.3.2. Taxonomic-Level Characteristics
3.4. CVD Risk Factors
3.5. Individuality and Reproducibility
3.6. Correlations Between Changes in Bacterial Taxa and CVD Risk Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025, 9th ed.; U.S. Department of Agriculture; U.S. Department of Health and Human Services: Washington, DC, USA, 2020. Available online: http://www.dietaryguidelines.gov/ (accessed on 1 May 2022).
- Rashidipour-Fard, N.; Karimi, M.; Saraf-Bank, S.; Baghaei, M.H.; Haghighatdoost, F.; Azadbakht, L. Healthy Eating Index and Cardiovascular Risk Factors among Iranian Elderly Individuals. ARYA Atheroscler. 2017, 13, 56–65. [Google Scholar] [PubMed]
- Motamedi, A.; Ekramzadeh, M.; Bahramali, E.; Farjam, M.; Homayounfar, R. Diet Quality in Relation to the Risk of Hypertension among Iranian Adults: Cross-Sectional Analysis of Fasa PERSIAN Cohort Study. Nutr. J. 2021, 20, 57. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Steffen, L.M.; Selvin, E.; Rebholz, C.M. Diet Quality, Change in Diet Quality and Risk of Incident CVD and Diabetes. Public Health Nutr. 2020, 23, 329–338. [Google Scholar] [CrossRef] [PubMed]
- NHANES—What We Eat in America. Available online: https://www.cdc.gov/nchs/nhanes/wweia.htm (accessed on 13 May 2022).
- CDC Heart Disease Facts|Cdc.Gov. Available online: https://www.cdc.gov/heart-disease/data-research/facts-stats/index.html (accessed on 13 May 2022).
- Wang, Y.; Lindemann, S.R.; Cross, T.-W.L.; Tang, M.; Clark, C.M.; Campbell, W.W. Effects of Adding Lean Red Meat to a U.S.-Style Healthy Vegetarian Dietary Pattern on Gut Microbiota and Cardiovascular Risk Factors in Young Adults: A Crossover Randomized Controlled Trial. J. Nutr. 2023, 153, 1439–1452. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Wang, X.; Feng, W.; Liu, Q.; Zhou, S.; Liu, Q.; Cai, L. The Gut Microbiota and Its Interactions with Cardiovascular Disease. Microb. Biotechnol. 2020, 13, 637. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.H.W.; Kitai, T.; Hazen, S.L. Gut Microbiota in Cardiovascular Health and Disease. Circ. Res. 2017, 120, 1183–1196. [Google Scholar] [CrossRef] [PubMed]
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A.; et al. Diet Rapidly and Reproducibly Alters the Human Gut Microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Sommer, F.; Anderson, J.M.; Bharti, R.; Raes, J.; Rosenstiel, P. The Resilience of the Intestinal Microbiota Influences Health and Disease. Nat. Rev. Microbiol. 2017, 15, 630–638. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, L.E.; Li, J.; Sayer, R.D.; Hennessy, J.E.; Campbell, W.W. Short-Term Effects of Healthy Eating Pattern Cycling on Cardiovascular Disease Risk Factors: Pooled Results from Two Randomized Controlled Trials. Nutrients 2018, 10, 1725. [Google Scholar] [CrossRef] [PubMed]
- Schofield, W.N. Predicting Basal Metabolic Rate, New Standards and Review of Previous Work. Hum. Nutr. Clin. Nutr. 1985, 39 (Suppl. S1), 5–41. [Google Scholar] [PubMed]
- Black, A. Critical Evaluation of Energy Intake Using the Goldberg Cut-off for Energy Intake:Basal Metabolic Rate. A Practical Guide to Its Calculation, Use and Limitations. Int. J. Obes. 2000, 24, 1119–1130. [Google Scholar] [CrossRef] [PubMed]
- NCC—Nutrition Coordinating Center. NDSR Software Food and Nutrient Database; NCC—Nutrition Coordinating Center: Minneapolis, MN, USA, 2013. [Google Scholar]
- Kozich, J.J.; Westcott, S.L.; Baxter, N.T.; Highlander, S.K.; Schloss, P.D. Development of a Dual-Index Sequencing Strategy and Curation Pipeline for Analyzing Amplicon Sequence Data on the MiSeq Illumina Sequencing Platform. Appl. Environ. Microbiol. 2013, 79, 5112–5120. [Google Scholar] [CrossRef] [PubMed]
- Segata, N.; Izard, J.; Waldron, L.; Gevers, D.; Miropolsky, L.; Garrett, W.S.; Huttenhower, C. Metagenomic Biomarker Discovery and Explanation. Genome Biol. 2011, 12, R60. [Google Scholar] [CrossRef] [PubMed]
- Bray, J.R.; Curtis, J.T. An Ordination of the Upland Forest Communities of Southern Wisconsin. Ecol. Monogr. 1957, 27, 326–349. [Google Scholar] [CrossRef]
- Jaccard, P. Étude Comparative de La Distribution Florale Dans Une Portion Des Alpes et Du Jura. Bull. Soc. Vaud. Sci. Nat. 1901, 37, 547. [Google Scholar] [CrossRef]
- Yue, J.C.; Clayton, M.K. A Similarity Measure Based on Species Proportions. Commun. Stat.-Theory Methods 2005, 34, 2123–2131. [Google Scholar] [CrossRef]
- Montani, J.-P.; Schutz, Y.; Dulloo, A.G. Dieting and Weight Cycling as Risk Factors for Cardiometabolic Diseases: Who Is Really at Risk? Obes. Rev. 2015, 16 (Suppl. S1), 7–18. [Google Scholar] [CrossRef] [PubMed]
- Vourakis, M.; Mayer, G.; Rousseau, G. The Role of Gut Microbiota on Cholesterol Metabolism in Atherosclerosis. Int. J. Mol. Sci. 2021, 22, 8074. [Google Scholar] [CrossRef] [PubMed]
- Leeming, E.R.; Johnson, A.J.; Spector, T.D.; Le Roy, C.I. Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients 2019, 11, 2862. [Google Scholar] [CrossRef] [PubMed]
- Rothschild, D.; Weissbrod, O.; Barkan, E.; Kurilshikov, A.; Korem, T.; Zeevi, D.; Costea, P.I.; Godneva, A.; Kalka, I.N.; Bar, N.; et al. Environment Dominates over Host Genetics in Shaping Human Gut Microbiota. Nature 2018, 555, 210–215. [Google Scholar] [CrossRef] [PubMed]
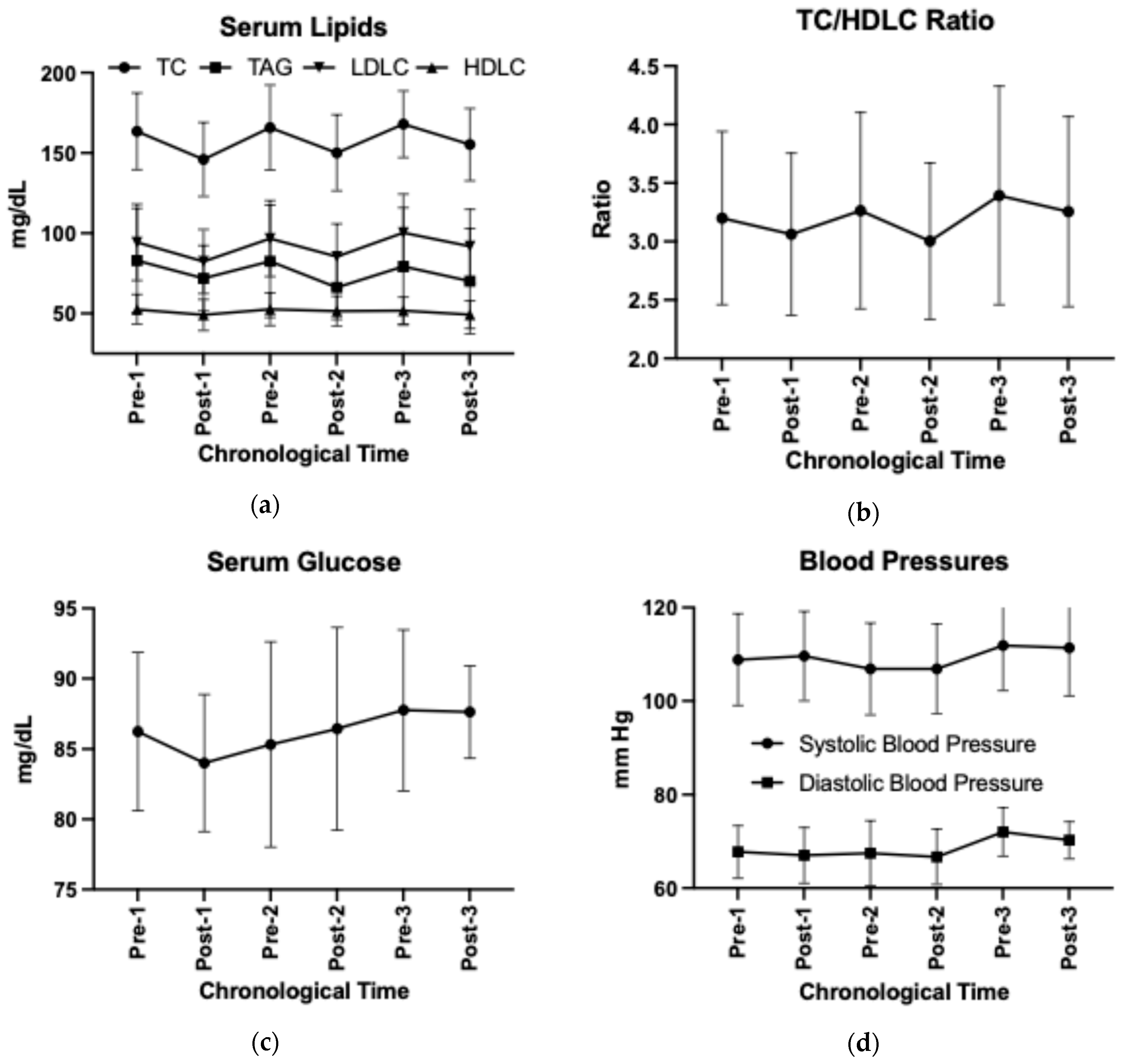
| Outcomes | |
|---|---|
| Anthropometrics | |
| Sample size N (F/M) | N = 17 (7/10) |
| Age (y) | 26 ± 4 |
| Weight (kg) | 69 ± 15 |
| BMI (kg/m2) | 23 ± 3 |
| Waist-to-hip circumference (cm) | 0.87 ± 0.05 |
| Sagittal abdominal diameter (cm) | 19.0 ± 2.4 |
| Systolic blood pressure (mm Hg) | 109 ± 9.8 |
| Diastolic blood pressure (mm Hg) | 68 ± 5.6 |
| Serum biomarkers | |
| Total cholesterol (mg/dL) | 164 ± 23.9 |
| Triglycerides (mg/dL) | 83 ± 32.5 |
| HDL cholesterol (mg/dL) | 53 ± 9.2 |
| LDL cholesterol (mg/dL) | 94 ± 23.8 |
| Cholesterol/HDL-C ratio | 3.2 ± 0.7 |
| Glucose (mg/dL) | 86.2 ± 5.6 |
| Blood Urea Nitrogen (mg/dL) | 13.1 ± 2.8 |
| Creatinine (mg/dL) | 0.9 ± 0.1 |
| Level | OTUs | Genera | ||||
|---|---|---|---|---|---|---|
| Comparisons | Mothur Output | LEfSe Output | RA > 0.1% | Mothur Output | LEfSe Output | RA > 0.1% |
| HDP 1, Post-1 vs. Pre-1 | Total: 292 RA > 0.1%: 49 | 6 | 5 | Total: 2152 RA > 0.1%: 90 | 10 | 8 |
| Washout 1, Pre-2 vs. Post-1 | 9 | 4 | 7 | 6 | ||
| HDP 2, Post-2 vs. Pre-2 | 7 | 4 | 5 | 4 | ||
| Washout 2, Pre-3 vs. Post-2 | 25 | 13 | 17 | 10 | ||
| HDP 3, Post-3 vs. Pre-3 | 6 | 3 | 1 | 1 | ||
| All HDP, Post vs. Pre | 17 | 8 | 18 | 14 | ||
| All Washouts, Post vs. Pre | 22 | 10 | 21 | 15 | ||
| Post, Post-1 vs. Post 2 | 2 | 1 | 0 | 0 | ||
| Post, Post-1 vs. Post-3 | 4 | 2 | 4 | 3 | ||
| Post, Post-2 vs. Post-3 | 5 | 3 | 5 | 4 | ||
| Pre, Pre-1 vs. Pre-2 | 3 | 1 | 2 | 0 | ||
| Pre, Pre-1 vs. Pre-3 | 3 | 2 | 6 | 3 | ||
| Pre, Pre-2 vs. Pre-3 | 3 | 1 | 4 | 2 | ||
| Comparisons | Increased | Decreased |
|---|---|---|
| HDP 1, Post-1 vs. Pre-1 | Genus: None OTUs: OTU0066-Roseburia OTU0071-Ruminococcaceae_unclassified | Genera: Dorea, Mediterraneibacter, Collinsella, Romboutsia, Lachnospira OTUs: OTU0017-Dorea OTU0025-Collinsella OTU0026-Mediterraneibacter OTU0035-Romboutsia OTU0057-Dorea OTU0076-Lachnospira |
| Washout 1, Pre-2 vs. Post-1 | Genera: Dorea, Mediterraneibacter, Collinsella, Romboutsia OTUs: OTU0017-Dorea OTU0026-Mediterraneibacter OTU0032-Mediterraneibacter OTU0035-Romboutsia OTU0056-Roseburia OTU0057-Dorea | None |
| HDP 2, Post-2 vs. Pre-2 | Genera: None OTUs: None | Genera: Anaerostipes, Dorea, Mediterraneibacter, Romboutsia, Collinsella OTUs: OTU0017-Dorea OTU0026-Mediterraneibacter OTU0032-Mediterraneibacter OTU0035-Romboutsia |
| Washout 2, Pre-3 vs. Post-2 | Genera: Blautia, Dorea, Mediterraneibacter, Streptococcus, Collinsella, Romboutsia, Faecalibacillus, Turicibacter OTUs: OTU0006-Blautia OTU0017-Dorea OTU0026-Mediterraneibacter OTU0035-Romboutsia OTU0038-Faecalibacillus OTU0110-Turicibacter | Genera: Clostridiales_unclassified, Parabacteroides, Bacteria_unclassified, Lachnospira, Bacteroidetes_unclassified OTUs: OTU0034-Lachnospiraceae_unclassified OTU0044-Ruminococcaceae_unclassified OTU0058-Parabacteroides OTU0076-Lachnospira |
| HDP 3, Post-3 vs. Pre-3 | Genus: Lachnospira OTUs: None | Genera: Collinsella, Turicibacter OTUs: OTU0026-Mediterraneibacter |
| All HDPs, Post vs. Pre | Genera: Coprococcus, Ruminococcus, Lachnospira OTUs: OTU0034-Lachnospiraceae_unclassified OTU0043-Ruminococcaceae_unclassified OTU0058-Parabacteroides OTU0061-Lachnospiraceae_unclassified OTU0066-Roseburia OTU0076-Lachnospira | Genera: Dorea, Mediterraneibacter, Collinsella, Romboutsia, Turicibacter OTUs: OTU0006-Blautia OTU0017-Dorea OTU0025-Collinsella OTU0026-Mediterraneibacter OTU0032-Mediterraneibacter OTU0035-Romboutsia OTU0037-Lachnospiraceae_unclassified OTU0088-Peptostreptococcaceae_unclassified |
| All Washouts, Post vs. Pre | Genera: Blautia, Dorea, Mediterraneibacter, Collinsella, Romboutsia, Turicibacter OTUs: OTU0008-Fusicatenibacter OTU0017-Dorea OTU0026-Mediterraneibacter OTU0032-Mediterraneibacter OTU0035-Romboutsia OTU0056-Roseburia OTU0057-Dorea OTU0110-Turicibacter OTU0006-Blautia | Genera: Parabacteroides, Coprococcus, Akkermansia, Lachnospira OTUs: OTU0034-Lachnospiraceae_unclassified OTU0039-Alistipes OTU0043-Ruminococcaceae_unclassified OTU0058-Parabacteroides OTU0066-Roseburia OTU0076-Lachnospira |
| At Post, Among HDPs (Post-1 vs. Post-2 vs. Post-3) | Genera: Anaerostipes (higher in Post-1 than Post-2) Parabacteroides, Clostridium_IV (higher in Post-1 than Post-3) Dorea (higher in Post-3 than Post-2) Parabacteroides, Bacteria_unclassified (higher in Post-2 than Post-3) OTUs: OTU0050-Blautia, OTU0057-Dorea (higher in Post-3 than Post-1) OTU0063-Parabacteroides (higher in Post-1 than Post-3) OTU0017-Dorea, OTU0057-Dorea (higher in Post-3 than Post-2) OTU0034-Lachnospiraceae_unclassified, OTU0063-Parabacteroides (higher in Post-2 than Post-3) | |
| At Pre, Among HDPs (Pre-1 vs. Pre-2 vs. Pre-3) | Genera: Roseburia (higher in Pre-2 than Pre-1) Clostridiales_unclassified, Bacteria_unclassified (higher in Pre-1 than Pre-3) Streptococcus (higher in Pre-3 than Pre-2) OTUs: OTU0023-Blautia, OTU0050-Blautia, OTU0073-Lachnospiraceae_unclassified (higher in Pre-3 than Pre-1) OTU0012-Bacteroides, OTU0078-Faecalibacterium (higher in Pre-2 than Pre-3) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Cross, T.-W.L.; Lindemann, S.R.; Tang, M.; Campbell, W.W. Healthy Dietary Pattern Cycling Affects Gut Microbiota and Cardiovascular Disease Risk Factors: Results from a Randomized Controlled Feeding Trial with Young, Healthy Adults. Nutrients 2024, 16, 3619. https://doi.org/10.3390/nu16213619
Wang Y, Cross T-WL, Lindemann SR, Tang M, Campbell WW. Healthy Dietary Pattern Cycling Affects Gut Microbiota and Cardiovascular Disease Risk Factors: Results from a Randomized Controlled Feeding Trial with Young, Healthy Adults. Nutrients. 2024; 16(21):3619. https://doi.org/10.3390/nu16213619
Chicago/Turabian StyleWang, Yu, Tzu-Wen L. Cross, Stephen R. Lindemann, Minghua Tang, and Wayne W. Campbell. 2024. "Healthy Dietary Pattern Cycling Affects Gut Microbiota and Cardiovascular Disease Risk Factors: Results from a Randomized Controlled Feeding Trial with Young, Healthy Adults" Nutrients 16, no. 21: 3619. https://doi.org/10.3390/nu16213619
APA StyleWang, Y., Cross, T.-W. L., Lindemann, S. R., Tang, M., & Campbell, W. W. (2024). Healthy Dietary Pattern Cycling Affects Gut Microbiota and Cardiovascular Disease Risk Factors: Results from a Randomized Controlled Feeding Trial with Young, Healthy Adults. Nutrients, 16(21), 3619. https://doi.org/10.3390/nu16213619






