Prevalence of Overweight and Obesity among Primary School Students in Split, Croatia
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection and Description
2.3. Ethical Aspects
2.4. Statistical Analysis
3. Results
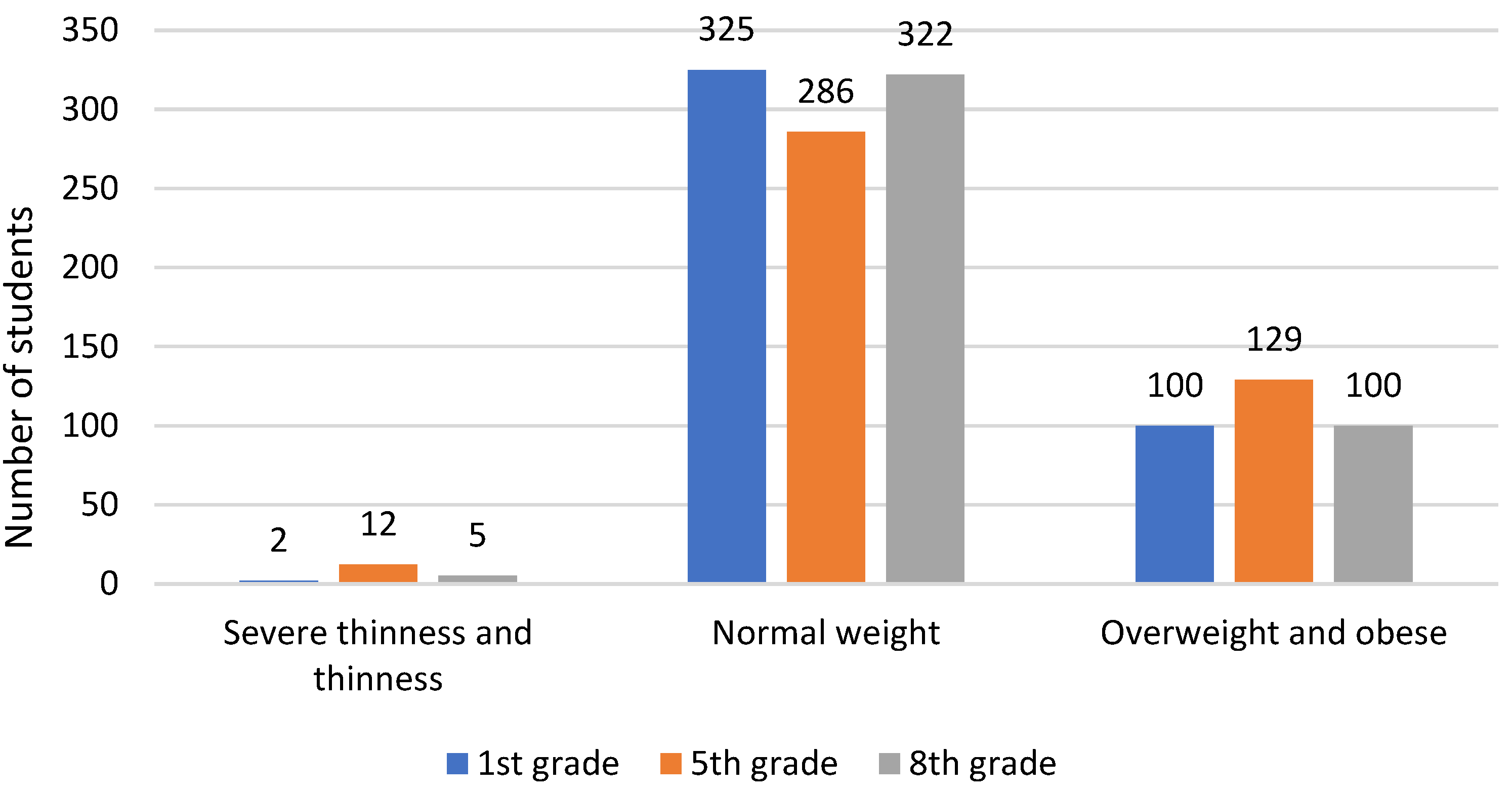
3.1. Weight Status and Prevalence of Overweight and Obesity
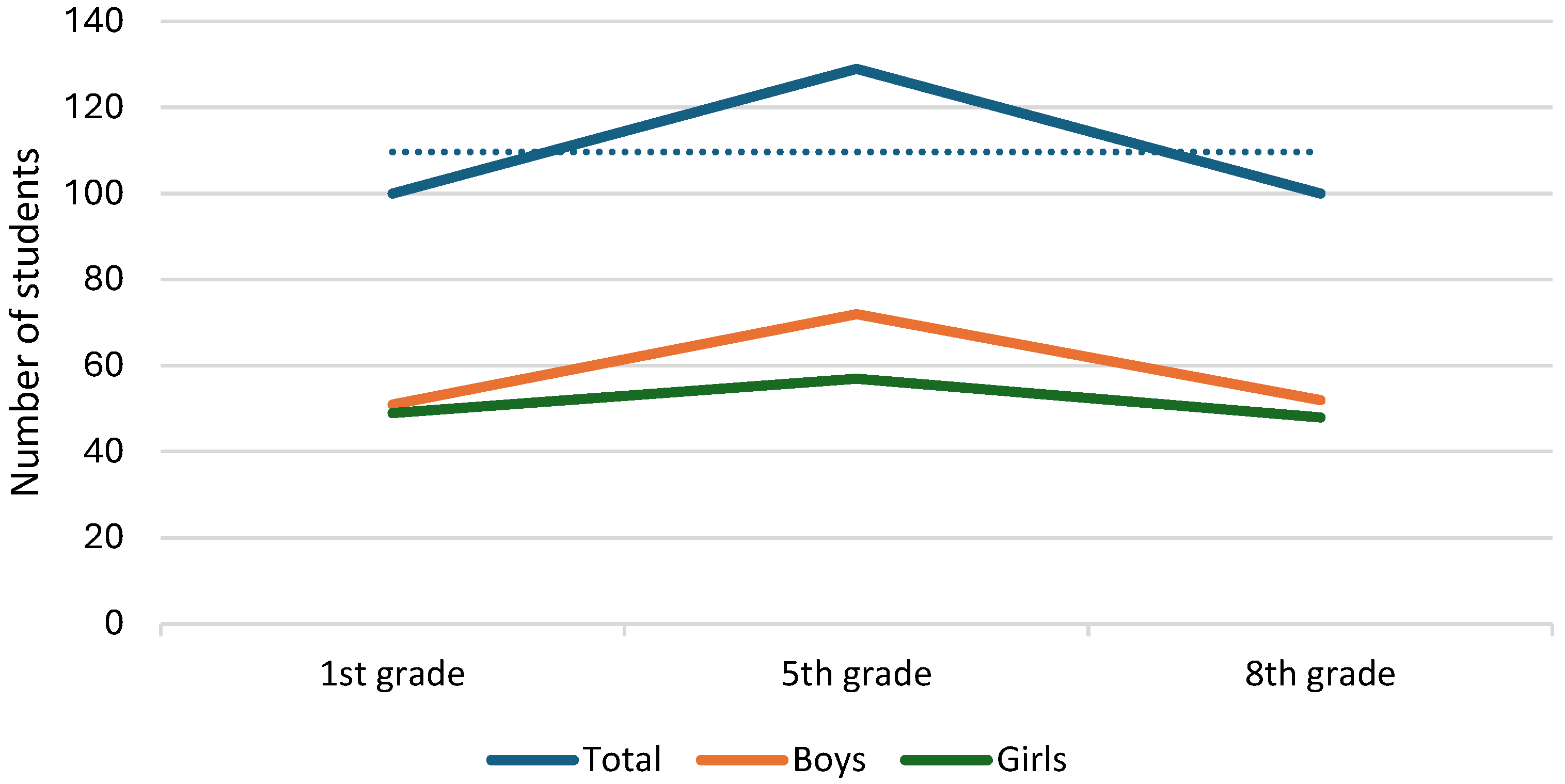
3.2. Sex Differences between Anthropometric Indices
3.3. Sports Participation and Differences in Anthropometric Indices
3.4. Parents’ Education Level and Differences in Anthropometric Indices and Student’s Sport Participation
3.5. Weight Status of Students Compared with Parents’ Education Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bousquet, J.; Anto, J.M.; Sterk, P.J.; Adcock, I.M.; Chung, K.F.; Roca, J.; Agusti, A.; Brightling, C.; Cambon-Thomsen, A.; Cesario, A.; et al. Systems Medicine and Integrated Care to Combat Chronic Noncommunicable Diseases. Genome Med. 2011, 3, 43. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.E.; Stevens, G.A.; Mathers, C.D.; Bonita, R.; Rehm, J.; Kruk, M.E.; Riley, L.M.; Dain, K.; Kengne, A.P.; Chalkidou, K.; et al. NCD Countdown 2030: Worldwide Trends in Non-Communicable Disease Mortality and Progress towards Sustainable Development Goal Target 3.4. Lancet 2018, 392, 1072–1088. [Google Scholar] [CrossRef] [PubMed]
- Hosseinpoor, A.R.; Bergen, N.; Mendis, S.; Harper, S.; Verdes, E.; Kunst, A.; Chatterji, S. Socioeconomic Inequality in the Prevalence of Noncommunicable Diseases in Low- and Middle-Income Countries: Results from the World Health Survey. BMC Public Health 2012, 12, 474. [Google Scholar] [CrossRef] [PubMed]
- Budreviciute, A.; Damiati, S.; Sabir, D.K.; Onder, K.; Schuller-Goetzburg, P.; Plakys, G.; Katileviciute, A.; Khoja, S.; Kodzius, R. Management and Prevention Strategies for Non-Communicable Diseases (NCDs) and Their Risk Factors. Front. Public Health 2020, 8, 574111. [Google Scholar] [CrossRef] [PubMed]
- Noncommunicable Diseases Country Profiles 2018. Available online: https://www.who.int/publications/i/item/9789241514620 (accessed on 6 August 2024).
- Wu, F.; Guo, Y.; Chatterji, S.; Zheng, Y.; Naidoo, N.; Jiang, Y.; Biritwum, R.; Yawson, A.; Minicuci, N.; Salinas-Rodriguez, A.; et al. Common Risk Factors for Chronic Non-Communicable Diseases among Older Adults in China, Ghana, Mexico, India, Russia and South Africa: The Study on Global AGEing and Adult Health (SAGE) Wave 1. BMC Public Health 2015, 15, 88. [Google Scholar] [CrossRef]
- Heidari-Beni, M. Early Life Nutrition and Non Communicable Disease. Adv. Exp. Med. Biol. 2019, 1121, 33–40. [Google Scholar] [CrossRef]
- Panuganti, K.K.; Nguyen, M.; Kshirsagar, R.K. Obesity. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023; Available online: http://www.ncbi.nlm.nih.gov/books/NBK459357/ (accessed on 6 August 2024).
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 11 May 2024).
- World Obesity Atlas 2023. Available online: https://www.worldobesity.org/resources/resource-library/world-obesity-atlas-2023 (accessed on 28 February 2024).
- Medanić, D.; Pucarin-Cvetković, J. Pretilost—Javnozdravstveni problem i izazov. Acta Med. Croatica. 2012, 66, 347–354. [Google Scholar] [PubMed]
- Kansra, A.R.; Lakkunarajah, S.; Jay, M.S. Childhood and Adolescent Obesity: A Review. Front. Pediatr. 2021, 8, 581461. [Google Scholar] [CrossRef]
- Pulgarón, E.R. Childhood Obesity: A Review of Increased Risk for Physical and Psychological Comorbidities. Clin. Ther. 2013, 35, A18–A32. [Google Scholar] [CrossRef]
- Obradovic Salcin, L.; Karin, Z.; Miljanovic Damjanovic, V.; Ostojic, M.; Vrdoljak, A.; Gilic, B.; Sajber, D. Physical Activity, Body Mass, and Adherence to the Mediterranean Diet in Preschool Children: A Cross-Sectional Analysis in the Split-Dalmatia County (Croatia). Int. J. Environ. Res. Public Health 2019, 16, 3237. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Aralica, M.; Jukić, M.; Žitko, V.; Despot, R.; Jurić, I. Gallbladder Disease in Children: A 20-year Single-center Experience. Indian Pediatr. 2019, 56, 384–386. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J.; Kelly, J. Long-Term Impact of Overweight and Obesity in Childhood and Adolescence on Morbidity and Premature Mortality in Adulthood: Systematic Review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Growth Reference 5–19 Years—BMI-for-Age (5–19 Years). Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age (accessed on 22 July 2024).
- Conolly, A.; Byron, D. Health Survey for England 2017: Adult and Child Overweight and Obesity; National Centre for Social Research, NHS Digital: London, UK, 2018. [Google Scholar]
- Overweight and Obesity among Australian Children and Adolescents, Summary. Available online: https://www.aihw.gov.au/reports/overweight-obesity/overweight-obesity-australian-children-adolescents/summary (accessed on 29 May 2024).
- Schienkiewitz, A.; Brettschneider, A.-K.; Damerow, S.; Rosario, A.S. Overweight and Obesity among Children and Adolescents in Germany. Results of the Cross-Sectional KiGGS Wave 2 Study and Trends. J. Health Monit. 2018, 3, 15–22. [Google Scholar] [CrossRef]
- Stavridou, A.; Kapsali, E.; Panagouli, E.; Thirios, A.; Polychronis, K.; Bacopoulou, F.; Psaltopoulou, T.; Tsolia, M.; Sergentanis, T.N.; Tsitsika, A. Obesity in Children and Adolescents during COVID-19 Pandemic. Children 2021, 8, 135. [Google Scholar] [CrossRef] [PubMed]
- Musić Milanović, S.; Križan, H.; Lang Morović, M.; Meštrić, S.; Šlaus, N.; Pezo, A. Europska Inicijativa Praćenja Debljine u Djece, Hrvatska 2021./2022. (CroCOSI); Hrvatski zavod za javno zdravstvo: Zagreb, Croatia, 2024. [Google Scholar]
- Ruiz, M.; Goldblatt, P.; Morrison, J.; Porta, D.; Forastiere, F.; Hryhorczuk, D.; Antipkin, Y.; Saurel-Cubizolles, M.-J.; Lioret, S.; Vrijheid, M.; et al. Impact of Low Maternal Education on Early Childhood Overweight and Obesity in Europe. Paediatr. Perinat. Epidemiol. 2016, 30, 274–284. [Google Scholar] [CrossRef]
- Lamerz, A.; Kuepper-Nybelen, J.; Wehle, C.; Bruning, N.; Trost-Brinkhues, G.; Brenner, H.; Hebebrand, J.; Her-pertz-Dahlmann, B. Social Class, Parental Education, and Obesity Prevalence in a Study of Six-Year-Old Children in Germany. Int. J. Obes. 2005, 29, 373–380. [Google Scholar] [CrossRef]
- Lamb, M.; Pleck, J.; Charnov, E.; Levine, J. A Biosocial Perspective on Paternal Behavior and Involvement: Biosocial Dimensions; Routledge: Abingdon, Oxfordshire, 2017; pp. 111–142. ISBN 978-1-315-12600-5. [Google Scholar]
- Laessle, R.G.; Uhl, H.; Lindel, B. Parental Influences on Eating Behavior in Obese and Nonobese Preadolescents. Int. J. Eat. Disord. 2001, 30, 447–453. [Google Scholar] [CrossRef]
- Klesges, R.C.; Stein, R.J.; Eck, L.H.; Isbell, T.R.; Klesges, L.M. Parental Influence on Food Selection in Young Children and Its Relationships to Childhood Obesity. Am. J. Clin. Nutr. 1991, 53, 859–864. [Google Scholar] [CrossRef]
- van Ansem, W.J.; Schrijvers, C.T.; Rodenburg, G.; van de Mheen, D. Maternal Educational Level and Children’s Healthy Eating Behaviour: Role of the Home Food Environment (Cross-Sectional Results from the INPACT Study). Int. J. Behav. Nutr. Phys. Act. 2014, 11, 113. [Google Scholar] [CrossRef]
- Lindsay, A.C.; Sussner, K.M.; Kim, J.; Gortmaker, S.L. The Role of Parents in Preventing Childhood Obesity. Future Child. 2006, 16, 169–186. [Google Scholar] [CrossRef] [PubMed]
- Wilk, P.; Clark, A.F.; Maltby, A.; Tucker, P.; Gilliland, J.A. Exploring the Effect of Parental Influence on Children’s Physical Activity: The Mediating Role of Children’s Perceptions of Parental Support. Prev. Med. 2018, 106, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Garriguet, D.; Colley, R.; Bushnik, T. Parent-Child Association in Physical Activity and Sedentary Behaviour. Health Rep. 2017, 28, 3–11. [Google Scholar] [PubMed]
- Vermeiren, A.P.; Willeboordse, M.; Oosterhoff, M.; Bartelink, N.; Muris, P.; Bosma, H. Socioeconomic Multi-Domain Health Inequalities in Dutch Primary School Children. Eur. J. Public Health 2018, 28, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Sweatt, K.; Garvey, W.T.; Martins, C. Strengths and Limitations of BMI in the Diagnosis of Obesity: What Is the Path Forward? Curr. Obes. Rep. 2024, 13, 584–595. [Google Scholar] [CrossRef] [PubMed]
- Franco, L.P.; Morais, C.C.; Cominetti, C. Normal-Weight Obesity Syndrome: Diagnosis, Prevalence, and Clinical Implications. Nutr. Rev. 2016, 74, 558–570. [Google Scholar] [CrossRef]
- Ara, I.; Vicente-Rodriguez, G.; Perez-Gomez, J.; Jimenez-Ramirez, J.; Serrano-Sanchez, J.A.; Dorado, C.; Calbet, J.a.L. Influ-ence of Extracurricular Sport Activities on Body Composition and Physical Fitness in Boys: A 3-Year Longitudinal Study. Int. J. Obes. 2006, 30, 1062–1071. [Google Scholar] [CrossRef] [PubMed]
- Kantanista, A.; Osiński, W.; Borowiec, J.; Tomczak, M.; Król-Zielińska, M. Body Image, BMI, and Physical Activity in Girls and Boys Aged 14–16 Years. Body Image 2015, 15, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.R.; Morgan, P.J.; Okely, A.D.; Dewar, D.; Collins, C.E.; Batterham, M.; Callister, R.; Plotnikoff, R.C. Preventing Obesity Among Adolescent Girls: One-Year Outcomes of the Nutrition and Enjoyable Activity for Teen Girls (NEAT Girls) Cluster Randomized Controlled Trial. Arch. Pediatr. Adolesc. Med. 2012, 166, 821–827. [Google Scholar] [CrossRef]
- Zhou, X.; Li, J.; Jiang, X. Effects of Different Types of Exercise Intensity on Improving Health-Related Physical Fitness in Children and Adolescents: A Systematic Review. Sci. Rep. 2024, 14, 14301. [Google Scholar] [CrossRef]
- Branco, B.H.M.; Mariano, I.R.; de Oliveira, L.P.; Bertolini, S.M.M.G.; de Oliveira, F.M.; Araújo, C.G.A.; Adamo, K. Sports and Functional Training Improve a Subset of Obesity-Related Health Parameters in Adolescents: A Randomized Controlled Trial. Front. Psychol. 2021, 11, 589554. [Google Scholar] [CrossRef] [PubMed]
- Bogataj, Š.; Trajković, N.; Cadenas-Sanchez, C.; Sember, V. Effects of School-Based Exercise and Nutrition Intervention on Body Composition and Physical Fitness in Overweight Adolescent Girls. Nutrients 2021, 13, 238. [Google Scholar] [CrossRef] [PubMed]
- US Preventive Services Task Force. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 2017, 317, 2417–2426. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhao, L.; Gao, L.; Pan, A.; Xue, H. Health Policy and Public Health Implications of Obesity in China. Lancet Diabetes Endocrinol. 2021, 9, 446–461. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Hu, F.B. The Role of Sugar-Sweetened Beverages in the Global Epidemics of Obesity and Chronic Diseases. Nat. Rev. Endocrinol. 2022, 18, 205–218. [Google Scholar] [CrossRef]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric Obesity—Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef]
- Akcijski Plan Za Prevenciju Debljine 2024–2027. Available online: https://zdravlje.gov.hr/programi-i-projekti/nacionalni-programi-projekti-i-strategije/ostali-programi/akcijski-plan-za-prevenciju-debljine-2024-2027/6275 (accessed on 6 August 2024).
| Total n = 427 | Boys n = 209 | Girls n = 218 | p | |
|---|---|---|---|---|
| 1st grade | ||||
| Weight (kg) | 25 (22, 28) | 25.5 (23, 28) | 24 (22, 27.5) | 0.085 * |
| Height (m) | 1.26 ± 0.06 | 1.26 ± 0.06 | 1.25 ± 0.06 | 0.039 ⸸ |
| BMI (kg/m2) | 15.80 (14.69, 19.91) | 15.80 (14.78, 16.83) | 15.80 (14.65, 17) | 0.765 * |
| BMI z-score | 0.30 ± 1.09 | 0.33 ± 1.12 | 0.28 ± 1.07 | 0.67 ⸸ |
| 5th grade | ||||
| Weight (kg) | 45 (39, 52.5) | 45 (38, 52) | 45 (40, 52.5) | 0.293 * |
| Height (m) | 1.56 ± 0.08 | 1.55 ± 0.08 | 1.56 ± 0.08 | 0.019 ⸸ |
| BMI (kg/m2) | 18.38 (16.73, 21.18) | 18.46 (16.78, 21.23) | 18.32 (16.73, 21.14) | 0.871 * |
| BMI z-score | 0.29 (−0.52, 1.26) | 0.43 (−0.43, 1.01) | 0.13 (−0.59, 1.01) | 0.052 * |
| 8th grade | ||||
| Weight (kg) | 58 (52, 65.75) | 59.5 (53, 69) | 56.5 (51.5, 63) | 0.002 * |
| Height (m) | 1.71 ± 0.08 | 1.74 ± 0.08 | 1.68 ± 0.06 | 0.001 ⸸ |
| BMI (kg/m2) | 19.77 (18.07, 22.14) | 19.49 (17.9, 21.72) | 19.95 (18.36, 22.24) | 0.165 * |
| BMI z-score | 0.15 (−0.51, 0.93) | 0.20 (−0.52, 0.98) | 0.14 (−0.48, 0.87) | 0.522 * |
| Sports Participation—Girls (n = 218) | Sports Participation—Boys (n = 209) | |||||
|---|---|---|---|---|---|---|
| Yes | No | p | Yes | No | p | |
| 1st grade | n = 131 | n = 87 | n = 137 | n = 72 | ||
| Weight (kg) | 24 (22, 27) | 24 (22, 28) | 0.641 * | 26 (23, 28) | 26 (21.5, 26.63) | 0.017 * |
| Height (m) | 1.25 ± 0.05 | 1.25 ± 0.06 | 0.704 ⸸ | 1.26 ± 0.05 | 1.26 ± 0.06 | 0.127 ⸸ |
| BMI (kg/m2) | 15.8 (14.69, 16.77) | 15.81 (14.54, 17.31) | 0.538 * | 16 (14.96, 16.92) | 15.42 (14.55, 16.55) | 0.022 * |
| BMI z-score | 0.285 ± 0.97 | 0.314 ± 1.21 | 0.641 * | 0.437 ± 1.09 | 0.113 ± 1.14 | 0.023 * |
| 5th grade | n = 144 | n = 74 | n = 153 | n = 56 | ||
| Weight (kg) | 44.75 (40, 51.63) | 45.75 (41.25, 54.5) | 0.871 * | 44 (38.5, 51) | 46 (38, 57.63) | 0.820 * |
| Height (m) | 1.56 ± 0.08 | 1.57 ± 0.07 | 0.869 ⸸ | 1.55 ± 0.08 | 1.55 ± 0.08 | 0.444 ⸸ |
| BMI (kg/m2) | 18.16 (16.66, 21.20) | 18.75 (16.98, 20.89) | 0.779 * | 18.38 (16.88, 20.72) | 18.67 (16.74, 22.93) | 0.842 * |
| BMI z-score | 0.18 ± 1.17 | 0.32 ± 1.20 | 0.789 ⸸ | 0.39 (−0.34, 1.25) | 0.51 (−0.42, 1.85) | 0.842 * |
| 8th grade | n = 142 | n = 76 | n = 149 | n = 60 | ||
| Weight (kg) | 55.5 (51.63, 62) | 57.25 (51, 67.13) | 0.883 * | 60 (54, 68) | 58.25 (49.75, 72) | 0.266 * |
| Height (m) | 1.68 ± 0.06 | 1.68 ± 0.0 | 0.635 ⸸ | 1.74 ± 0.08 | 1.74 ± 0.08 | 0.275 * |
| BMI (kg/m2) | 19.67 (18.40, 21.57) | 20.62 (18.15, 23.77) | 0.914 * | 19.66 (18, 21.53) | 19.05 (17.15, 23.77) | 0.247 * |
| BMI z-score | 0.39 (−0.46, 0.67) | 0.37 (−0.57, 1.26) | 0.914 * | 0.29 ± 1.01 | 0.18 ± 1.42 | 0.281 ⸸ |
| Mother’s Education | Father’s Education | |||||
|---|---|---|---|---|---|---|
| SE n = 211 | HE n = 216 | p | SE n = 229 | HE n = 198 | p | |
| 1st grade | ||||||
| Weight (kg) | 25 (22, 28) | 25 (22, 27.5) | 0.543 * | 25 (23, 28) | 24.75 (22, 27) | 0.207 * |
| Height (m) | 1.26 ± 0.06 | 1.26 ± 0.05 | 0.926 ⸸ | 1.26 ± 0.05 | 1.25 ± 0.06 | 0.236 ⸸ |
| BMI (kg/m2) | 15.84 (14.71, 17.2) | 15.79 (14.68, 16.70) | 0.211 * | 15.98 (14.71, 17.22) | 15.68 (14.68, 16.66) | 0.182 * |
| BMI z-score | 0.37 ± 1.153 | 0.237 ± 1.026 | 0.206 ⸸ | 0.4 (−0.43, 1.08) | 0.21 (−0.48, 0.83) | 0.172 * |
| Sports participation | 117 (54.5%) | 151 (69.9%) | 0.002 ⁑ | 127 (55.5%) | 141 (71.2%) | <0.001 ⁑ |
| 5th grade | ||||||
| Weight (kg) | 46 (40, 55.5) | 44 (38, 51) | 0.008 * | 46 (40, 55.5) | 43 (38, 51) | 0.002 * |
| Height (m) | 1.56 ± 0.08 | 1.55 ± 0.08 | 0.838 ⸸ | 1.56 ± 0.07 | 1.55 ± 0.08 | 0.321 ⸸ |
| BMI (kg/m2) | 18.92 (17.24, 21.97) | 18.03 (16.35, 20.45) | 0.001 * | 18.94 (17.19, 21.9) | 17.99 (16.37, 20.28) | <0.001 * |
| BMI z-score | 0.12 (−0.28, 1.49) | 0.12 (−0.75, 0.98) | 0.002 * | 0.55 (−0.32, 1.48) | 0.1 (−0.74, 0.95) | <0.001 * |
| Sports participation | 134 (63.5%) | 163 (75.5%) | 0.007 ⁑ | 149 (65.1%) | 148 (74.8%) | 0.03 ⁑ |
| 8th grade | ||||||
| Weight (kg) | 59 (53, 68) | 57 (52, 63.5) | 0.017 * | 59 (53, 67.5) | 57.5 (52, 63.5) | 0.467 * |
| Height (m) | 1.71 ± 0.07 | 1.71 ± 0.08 | 0.277 ⸸ | 1.71 ± 0.08 | 1.71 ± 0.08 | 0.579 ⸸ |
| BMI (kg/m2) | 20.15 (18.4, 23.23) | 19.26 (17.92, 21.32) | 0.003 * | 20.08 (18.31, 22.76) | 19.2 (17.9, 21.37) | 0.012 * |
| BMI z-score | 0.39 (−0.40, 1.23) | −0.002 (−0.60, 0.75) | 0.003 * | −0.006 (−0.43, 1.06) | −0.006 (−0.60, 0.77) | 0.012 * |
| Sports participation | 128 (60.7%) | 163 (75.5%) | 0.001 ⁑ | 146 (63.8%) | 145 (73.2%) | 0.036 ⁑ |
| Mother’s Education | Father’s Education | |||||
|---|---|---|---|---|---|---|
| SE n = 211 | HE n = 216 | p ⁑ | SE n = 229 | HE n = 198 | p ⁑ | |
| 1st grade | ||||||
| Underweight and Normal Weight | 153 (72.5%) | 174 (80.6%) | 0.049 | 165 (72.1%) | 162 (81.8%) | 0.017 |
| Overweight and Obese | 58 (27.5%) | 42 (19.4%) | 64 (27.9%) | 36 (18.2%) | ||
| 5th grade | ||||||
| Underweight and Normal Weight | 136 (64.5%) | 162 (75%) | 0.018 | 146 (63.8%) | 152 (76.8%) | 0.003 |
| Overweight and Obese | 75 (35.5%) | 54 (25%) | 83 (36.2%) | 46 (23.2%) | ||
| 8th grade | ||||||
| Underweight and Normal Weight | 152 (72%) | 175 (81%) | 0.028 | 168 (73.4%) | 159 (80.3%) | 0.091 |
| Overweight and Obese | 59 (28%) | 41 (19%) | 61 (26.6%) | 39 (19.7%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Šimunović, I.; Mrčela, D.; Karin, Ž.; Pogorelić, Z.; Markić, J. Prevalence of Overweight and Obesity among Primary School Students in Split, Croatia. Nutrients 2024, 16, 3488. https://doi.org/10.3390/nu16203488
Šimunović I, Mrčela D, Karin Ž, Pogorelić Z, Markić J. Prevalence of Overweight and Obesity among Primary School Students in Split, Croatia. Nutrients. 2024; 16(20):3488. https://doi.org/10.3390/nu16203488
Chicago/Turabian StyleŠimunović, Ivan, Dina Mrčela, Željka Karin, Zenon Pogorelić, and Joško Markić. 2024. "Prevalence of Overweight and Obesity among Primary School Students in Split, Croatia" Nutrients 16, no. 20: 3488. https://doi.org/10.3390/nu16203488
APA StyleŠimunović, I., Mrčela, D., Karin, Ž., Pogorelić, Z., & Markić, J. (2024). Prevalence of Overweight and Obesity among Primary School Students in Split, Croatia. Nutrients, 16(20), 3488. https://doi.org/10.3390/nu16203488








