Impact of Medical School on the Relationship between Nutritional Knowledge and Sleep Quality—A Longitudinal Study of Students at Wroclaw Medical University in Poland
Abstract
1. Introduction
2. Materials and Methods
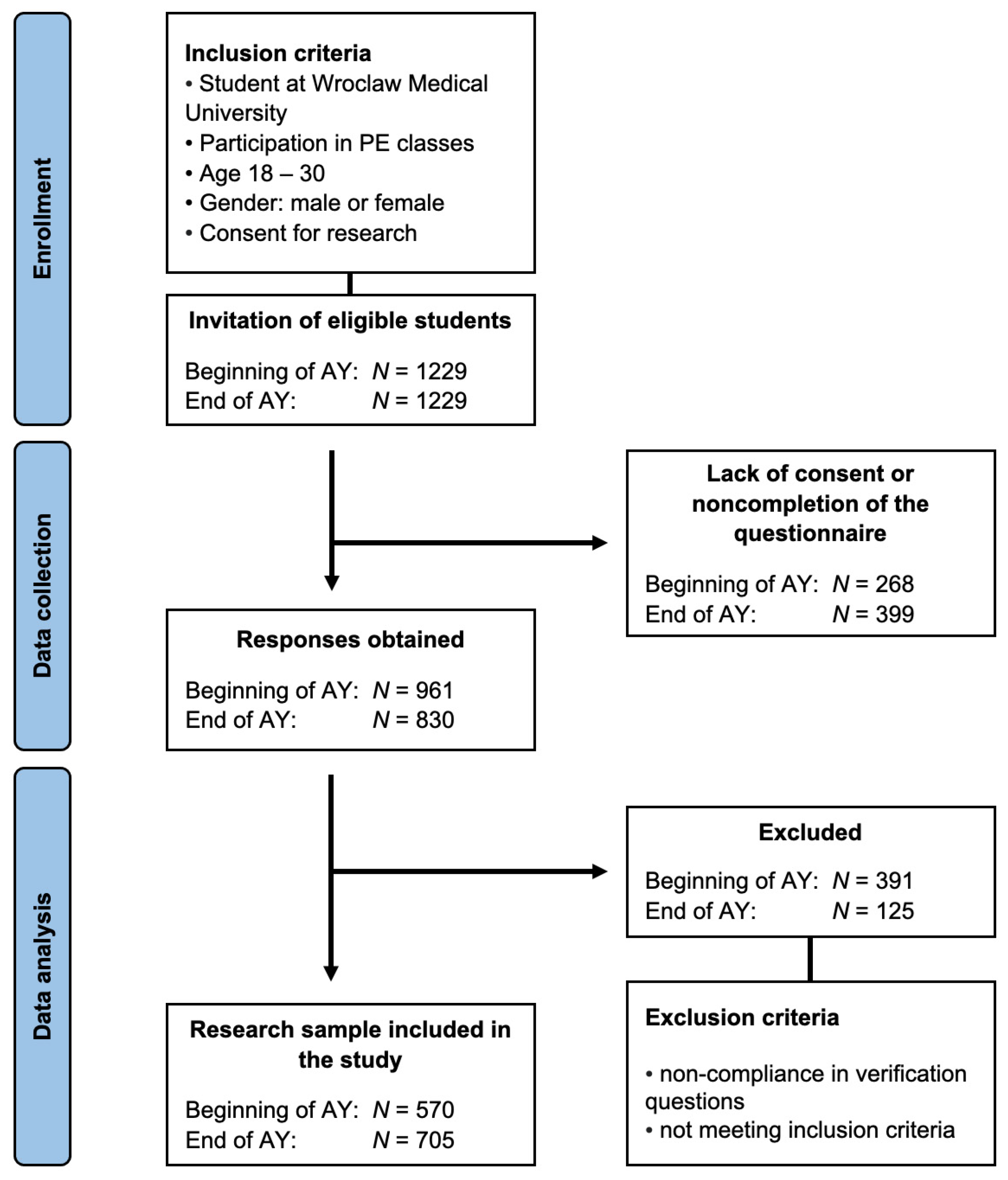
2.1. Study Design and Participants
2.2. Selection of Study Variables
2.3. KomPAN
2.4. The Pittsburgh Sleep Quality Index (PSQI)
- Sleep duration (DURAT): Awarding zero points for achieving 7 or more hours of sleep.
- Sleep disturbances (DISTB): A scoring system dependent on the presence of disturbances affecting the continuity of night sleep, such as feeling too hot or too cold, experiencing unsettling dreams, or discomfort in breathing.
- Sleep latency (LATEN): Allocating zero points for a latency period of less than 15 min and three points for a latency exceeding 60 min.
- Daytime dysfunctions (DAYDYS): Scoring based on the frequency with which a lack of nocturnal rest impacts daytime behavioral disruptions, such as eating habits or participation in meetings.
- Habitual sleep efficiency (HSE): Scoring contingent on the ratio of actual hours of sleep to the time spent in bed.
- Subjective sleep quality (SLPQUAL): Assigning a score based on the subjective evaluation of sleep quality by the respondent.
- Use of sleep medication (MEDS): Scoring in relation to the frequency of sleep medication usage by the respondent.
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Anthropometric Data
4.2. Sleep Quality
4.3. Nutritional Knowledge
4.4. Differences between Sleep Quality and Nutritional Knowledge Levels
4.5. Other Possibly Influential Factors
4.6. Future Implications
4.7. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Puthran, R.; Zhang, M.W.B.; Tam, W.W.; Ho, R.C. Prevalence of Depression amongst Medical Students: A Meta-Analysis. Med. Educ. 2016, 50, 456–468. [Google Scholar] [CrossRef]
- Sanagavarapu, P.; Abraham, J.; Taylor, E. Development and Validation of a Scale to Measure First Year Students’ Transitional Challenges, Wellbeing, Help-Seeking, and Adjustments in an Australian University. High Educ. 2019, 77, 695–715. [Google Scholar] [CrossRef]
- Bernier, A.; Larose, S.; Whipple, N. Leaving Home for College: A Potentially Stressful Event for Adolescents with Preoccupied Attachment Patterns. Attach. Hum. Dev. 2005, 7, 171–185. [Google Scholar] [CrossRef] [PubMed]
- Briggs, A.R.J.; Clark, J.; Hall, I. Building Bridges: Understanding Student Transition to University. Qual. High. Educ. 2012, 18, 3–21. [Google Scholar] [CrossRef]
- Vila-Martí, A.; Elío, I.; Sumalla-Cano, S. Eating Behavior during First-Year College Students, Including Eating Disorders—RUVIC-RUNEAT-TCA Project. Protocol of an Observational Multicentric Study. Int. J. Environ. Res. Public Health 2021, 18, 9457. [Google Scholar] [CrossRef]
- Examination of Grocery Shopping Skills among College Students—ProQuest. Available online: https://www.proquest.com/openview/0cd74078e17d4cd4374786f8242bbb32/1?pq-origsite=gscholar&cbl=18750&diss=y (accessed on 16 December 2023).
- Shim, S.; Barber, B.L.; Card, N.A.; Xiao, J.J.; Serido, J. Financial Socialization of First-Year College Students: The Roles of Parents, Work, and Education. J. Youth Adolesc. 2010, 39, 1457–1470. [Google Scholar] [CrossRef]
- Azad, M.C.; Fraser, K.; Rumana, N.; Abdullah, A.F.; Shahana, N.; Hanly, P.J.; Turin, T.C. Sleep Disturbances among Medical Students: A Global Perspective. J. Clin. Sleep Med. 2015, 11, 69–74. [Google Scholar] [CrossRef]
- Shah, M.; Hasan, S.; Malik, S.; Sreeramareddy, C.T. Perceived Stress, Sources and Severity of Stress among Medical Undergraduates in a Pakistani Medical School. BMC Med. Educ. 2010, 10, 2. [Google Scholar] [CrossRef]
- Harrison, P.L.; Shaddox, L.M.; Garvan, C.W.; Behar-Horenstein, L.S. Wellness Among Dental Students: An Institutional Study. J. Dent. Educ. 2016, 80, 1119–1125. [Google Scholar] [CrossRef]
- Ludy, M.-J.; Tan, S.-Y.; Leone, R.J.; Morgan, A.L.; Tucker, R.M. Weight Gain in First-Semester University Students: Positive Sleep and Diet Practices Associated with Protective Effects. Physiol. Behav. 2018, 194, 132–136. [Google Scholar] [CrossRef]
- Mudhovozi, P. Social and Academic Adjustment of First-Year University Students. J. Soc. Sci. 2012, 33, 251–259. [Google Scholar] [CrossRef]
- López-Hernández, L.; Martínez-Arnau, F.M.; Pérez-Ros, P.; Drehmer, E.; Pablos, A. Improved Nutritional Knowledge in the Obese Adult Population Modifies Eating Habits and Serum and Anthropometric Markers. Nutrients 2020, 12, 3355. [Google Scholar] [CrossRef]
- López-Olivares, M.; Mohatar-Barba, M.; Fernández-Gómez, E.; Enrique-Mirón, C. Mediterranean Diet and the Emotional Well-Being of Students of the Campus of Melilla (University of Granada). Nutrients 2020, 12, 1826. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.; Goldman, S.; Pursey, K.; Lim, R. Is There an Association between Dietary Intake and Academic Achievement: A Systematic Review. J. Hum. Nutr. Diet. 2017, 30, 117–140. [Google Scholar] [CrossRef]
- Reichelt, A.C.; Westbrook, R.F.; Morris, M.J. Editorial: Impact of Diet on Learning, Memory and Cognition. Front. Behav. Neurosci. 2017, 11, 96. [Google Scholar] [CrossRef] [PubMed]
- Schnettler, B.; Miranda, H.; Lobos, G.; Orellana, L.; Sepúlveda, J.; Denegri, M.; Etchebarne, S.; Mora, M.; Grunert, K.G. Eating Habits and Subjective Well-Being. A Typology of Students in Chilean State Universities. Appetite 2015, 89, 203–214. [Google Scholar] [CrossRef]
- Bremner, J.D.; Moazzami, K.; Wittbrodt, M.T.; Nye, J.A.; Lima, B.B.; Gillespie, C.F.; Rapaport, M.H.; Pearce, B.D.; Shah, A.J.; Vaccarino, V. Diet, Stress and Mental Health. Nutrients 2020, 12, 2428. [Google Scholar] [CrossRef]
- Silva, E.d.S.M.e.; Ono, B.H.V.S.; Souza, J.C. Sleep and Immunity in Times of COVID-19. Rev. Assoc. Med. Bras. 2020, 66, 143–147. [Google Scholar] [CrossRef]
- Irwin, M.R. Why Sleep Is Important for Health: A Psychoneuroimmunology Perspective. Annu. Rev. Psychol. 2015, 66, 143–172. [Google Scholar] [CrossRef]
- Medic, G.; Wille, M.; Hemels, M.E. Short- and Long-Term Health Consequences of Sleep Disruption. NSS 2017, 9, 151–161. [Google Scholar] [CrossRef]
- Brick, C.A.; Seely, D.L.; Palermo, T.M. Association Between Sleep Hygiene and Sleep Quality in Medical Students. Behav. Sleep Med. 2010, 8, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Pagnin, D.; de Queiroz, V.; Carvalho, Y.T.M.S.; Dutra, A.S.S.; Amaral, M.B.; Queiroz, T.T. The Relation Between Burnout and Sleep Disorders in Medical Students. Acad. Psychiatry 2014, 38, 438–444. [Google Scholar] [CrossRef]
- Rebello, C.R.; Kallingappa, P.B.; Hegde, P.G. Assessment of Perceived Stress and Association with Sleep Quality and Attributed Stressors among 1st-Year Medical Students: A Cross-Sectional Study from Karwar, Karnataka, India. Tzu Chi Med. J. 2018, 30, 221–226. [Google Scholar] [CrossRef]
- Alotaibi, A.D.; Alosaimi, F.M.; Alajlan, A.A.; Bin Abdulrahman, K.A. The Relationship between Sleep Quality, Stress, and Academic Performance among Medical Students. J. Fam. Community Med. 2020, 27, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Safhi, M.A.; Alafif, R.A.; Alamoudi, N.M.; Alamoudi, M.M.; Alghamdi, W.A.; Albishri, S.F.; Rizk, H. The Association of Stress with Sleep Quality among Medical Students at King Abdulaziz University. J. Fam. Med. Prim. Care 2020, 9, 1662–1667. [Google Scholar] [CrossRef] [PubMed]
- Doğan, İ.; Doğan, N. The Prevalence of Depression, Anxiety, Stress and Its Association with Sleep Quality among Medical Students. Ank. Med. J. 2019, 19, 550–558. [Google Scholar] [CrossRef]
- Alsaggaf, M.A.; Wali, S.O.; Merdad, R.A.; Merdad, L.A. Sleep Quantity, Quality, and Insomnia Symptoms of Medical Students during Clinical Years. Saudi Med. J. 2016, 37, 173–182. [Google Scholar] [CrossRef]
- Sullivan Bisson, A.N.; Robinson, S.A.; Lachman, M.E. Walk to a Better Night of Sleep: Testing the Relationship between Physical Activity and Sleep. Sleep Health 2019, 5, 487–494. [Google Scholar] [CrossRef]
- Bandura, A. Health Promotion from the Perspective of Social Cognitive Theory. In Understanding and Changing Health Behaviour; Psychology Press: London, UK, 2000; ISBN 978-1-315-08005-5. [Google Scholar]
- Tang, N.K.Y.; Sanborn, A.N. Better Quality Sleep Promotes Daytime Physical Activity in Patients with Chronic Pain? A Multilevel Analysis of the Within-Person Relationship. PLoS ONE 2014, 9, e92158. [Google Scholar] [CrossRef]
- Zschucke, E.; Heinz, A.; Ströhle, A. Exercise and Physical Activity in the Therapy of Substance Use Disorders. Sci. World J. 2012, 2012, e901741. [Google Scholar] [CrossRef]
- Peuhkuri, K.; Sihvola, N.; Korpela, R. Diet Promotes Sleep Duration and Quality. Nutr. Res. 2012, 32, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Grace, M.K.; VanHeuvelen, J.S. Occupational Variation in Burnout among Medical Staff: Evidence for the Stress of Higher Status. Soc. Sci. Med. 2019, 232, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Lewis, E.; Zauskova, A. Prolonged Stress, Anxiety, and Depression in Medical Staff during the COVID-19 Crisis. Psychosoc. Issues Hum. Resour. Manag. 2021, 9, 21. [Google Scholar] [CrossRef]
- Dharamsi, S.; Ho, A.; Spadafora, S.M.; Woollard, R. The Physician as Health Advocate: Translating the Quest for Social Responsibility Into Medical Education and Practice. Acad. Med. 2011, 86, 1108. [Google Scholar] [CrossRef] [PubMed]
- Thomasson, C. Physicians’ Social Responsibility. AMA J. Ethics 2014, 16, 753–757. [Google Scholar] [CrossRef]
- Rolstad, S.; Adler, J.; Rydén, A. Response Burden and Questionnaire Length: Is Shorter Better? A Review and Meta-Analysis. Value Health 2011, 14, 1101–1108. [Google Scholar] [CrossRef]
- Cernat, A.; Sakshaug, J.; Christmann, P.; Gummer, T. The Impact of Survey Mode Design and Questionnaire Length on Measurement Quality. Sociol. Methods Res. 2022, 2022, 00491241221140139. [Google Scholar] [CrossRef]
- Barros, M.B.d.A.; Lima, M.G.; Ceolim, M.F.; Zancanella, E.; Cardoso, T.A.M.D.O. Quality of Sleep, Health and Well-Being in a Population-Based Study. Rev. Saúde Pública 2019, 53, 82. [Google Scholar] [CrossRef]
- Coppoolse, H.L.; Seidell, J.C.; Dijkstra, S.C. Impact of Nutrition Education on Nutritional Knowledge and Intentions towards Nutritional Counselling in Dutch Medical Students: An Intervention Study. BMJ Open 2020, 10, e034377. [Google Scholar] [CrossRef]
- Tavakoli, H.R.; Dini-Talatappeh, H.; Rahmati-Najarkolaei, F.; Gholami Fesharaki, M. Efficacy of HBM-Based Dietary Education Intervention on Knowledge, Attitude, and Behavior in Medical Students. Iran Red Crescent Med. J. 2016, 18, e23584. [Google Scholar] [CrossRef][Green Version]
- Jezewska-Zychowicz, M.; Gawecki, J.; Wadolowska, L.; Czarnocinska, J.; Galinski, G.; Kollajtis-Dolowy, A.; Roszkowski, W.; Wawrzyniak, A.; Przybylowicz, K.; Stasiewicz, B.; et al. KomPAN® Dietary Habits and Nutrition Beliefs Questionnaire for People 15–65 Years Old, Version 1.1.—Interviewer Administered Questionnaire. Chapter 1. In KomPAN® Dietary Habits and Nutrition Beliefs Questionnaire and the Manual for Developing of Nutritional Data; The Committee of Human Nutrition, Polish Academy of Sciences: Olsztyn, Poland, 2020; pp. 4–21. ISBN 978-83-950330-2-5. [Google Scholar]
- Kowalkowska, J.; Wadolowska, L.; Czarnocinska, J.; Czlapka-Matyasik, M.; Galinski, G.; Jezewska-Zychowicz, M.; Bronkowska, M.; Dlugosz, A.; Loboda, D.; Wyka, J. Reproducibility of a Questionnaire for Dietary Habits, Lifestyle and Nutrition Knowledge Assessment (KomPAN) in Polish Adolescents and Adults. Nutrients 2018, 10, 1845. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Smyka, M.; Kosińska-Kaczyńska, K.; Sochacki-Wójcicka, N.; Zgliczyńska, M.; Wielgoś, M. Sleep Quality According to the Pittsburgh Sleep Quality Index in over 7000 Pregnant Women in Poland. Sleep Biol. Rhythm. 2021, 19, 353–360. [Google Scholar] [CrossRef]
- Moberly, T. Number of Women Entering Medical School Rises after Decade of Decline. BMJ 2018, 167, k254. [Google Scholar] [CrossRef]
- Kosendiak, A.A.; Wysocki, M.; Krysiński, P.; Kuźnik, Z.; Adamczak, B. Impact of the COVID-19 Pandemic on Physical Activity, Smoking, Alcohol Use, and Mental Well-Being—A Longitudinal Study of Nursing Students at Wroclaw Medical University in Poland. Front. Public Health 2023, 11, 1249509. [Google Scholar] [CrossRef] [PubMed]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef] [PubMed]
- Sumalla-Cano, S.; Forbes-Hernández, T.; Aparicio-Obregón, S.; Crespo, J.; Eléxpuru-Zabaleta, M.; Gracia-Villar, M.; Giampieri, F.; Elío, I. Changes in the Lifestyle of the Spanish University Population during Confinement for COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 2210. [Google Scholar] [CrossRef]
- Adamczak, B.; Kuźnik, Z.; Makles, S.; Kosendiak, A.A. Physical Activity of Ukrainian and Polish Medical Students in the Beginning of the War in Ukraine. Health Probl. Civiliz. 2023, 17, 388–398. [Google Scholar] [CrossRef]
- Gutin, I. In BMI We Trust: Reframing the Body Mass Index as a Measure of Health. Soc. Theory Health 2018, 16, 256–271. [Google Scholar] [CrossRef]
- Abdussalam, A.; Salman, M.T.; Gupta, S.; Trivedi, M.; Faruqi, M. Poor Quality of Sleep and Its Relationship with Depression in First Year Medical Students. Adv. Life Sci. Technol. 2013, 12, 17–21. [Google Scholar]
- Rao, W.-W.; Li, W.; Qi, H.; Hong, L.; Chen, C.; Li, C.-Y.; Ng, C.H.; Ungvari, G.S.; Xiang, Y.-T. Sleep Quality in Medical Students: A Comprehensive Meta-Analysis of Observational Studies. Sleep Breath 2020, 24, 1151–1165. [Google Scholar] [CrossRef] [PubMed]
- Corrêa, C.d.C.; Oliveira, F.K.d.; Pizzamiglio, D.S.; Ortolan, E.V.P.; Weber, S.A.T. Sleep Quality in Medical Students: A Comparison across the Various Phases of the Medical Course. J. Bras. Pneumol. 2017, 43, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Eleftheriou, A.; Rokou, A.; Arvaniti, A.; Nena, E.; Steiropoulos, P. Sleep Quality and Mental Health of Medical Students in Greece During the COVID-19 Pandemic. Front. Public Health 2021, 9, 775374. [Google Scholar] [CrossRef] [PubMed]
- Kosendiak, A.A.; Adamczak, B.; Kontek, S.; Kuźnik, Z.; Roman, M.; Gostkowski, M.; Niedziółka, A. Level of Physical Activity, Sleep Quality and Use of Personal Protective Equipment of Students at Wroclaw Medical University during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 2406. [Google Scholar] [CrossRef] [PubMed]
- Tahir, M.J.; Malik, N.I.; Ullah, I.; Khan, H.R.; Perveen, S.; Ramalho, R.; Siddiqi, A.R.; Waheed, S.; Shalaby, M.M.M.; Berardis, D.D.; et al. Internet Addiction and Sleep Quality among Medical Students during the COVID-19 Pandemic: A Multinational Cross-Sectional Survey. PLoS ONE 2021, 16, e0259594. [Google Scholar] [CrossRef] [PubMed]
- Özçelik, N.; Kesin, H.V.; Telatar, G.; Özyurt, S.; Yılmaz Kara, B.; Gümüş, A.; Hocaoğlu, Ç.; Şahin, Ü. ‘COVID-Somnia’ in Healthcare Workers during the Pandemic. Hosp. Pract. 2022, 50, 273–281. [Google Scholar] [CrossRef]
- Trabelsi, K.; Ammar, A.; Masmoudi, L.; Boukhris, O.; Chtourou, H.; Bouaziz, B.; Brach, M.; Bentlage, E.; How, D.; Ahmed, M.; et al. Sleep Quality and Physical Activity as Predictors of Mental Wellbeing Variance in Older Adults during COVID-19 Lockdown: ECLB COVID-19 International Online Survey. Int. J. Environ. Res. Public Health 2021, 18, 4329. [Google Scholar] [CrossRef]
- Tafoya, S.A.; Jurado, M.M.; Yépez, N.J.; Fouilloux, M.; Lara, M.C. Sleep Difficulties and Psychological Symptoms in Medicine Students in Mexico. Medicina 2013, 73, 247–251. [Google Scholar]
- Divani, A.; Heidari, M.E.; Ghavampour, N.; Parouhan, A.; Ahmadi, S.; Narimani Charan, O.; Shahsavari, H. Effect of Cancer Treatment on Sleep Quality in Cancer Patients: A Systematic Review and Meta-Analysis of Pittsburgh Sleep Quality Index. Support Care Cancer 2022, 30, 4687–4697. [Google Scholar] [CrossRef]
- Zeng, L.-N.; Yang, Y.; Wang, C.; Li, X.-H.; Xiang, Y.-F.; Hall, B.J.; Ungvari, G.S.; Li, C.-Y.; Chen, C.; Chen, L.-G.; et al. Prevalence of Poor Sleep Quality in Nursing Staff: A Meta-Analysis of Observational Studies. Behav. Sleep Med. 2020, 18, 746–759. [Google Scholar] [CrossRef]
- Hinz, A.; Glaesmer, H.; Brähler, E.; Löffler, M.; Engel, C.; Enzenbach, C.; Hegerl, U.; Sander, C. Sleep Quality in the General Population: Psychometric Properties of the Pittsburgh Sleep Quality Index, Derived from a German Community Sample of 9284 People. Sleep Med. 2017, 30, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Liao, Y.; Kelly, B.C.; Xie, L.; Xiang, Y.-T.; Qi, C.; Pan, C.; Hao, W.; Liu, T.; Zhang, F.; et al. Gender and Regional Differences in Sleep Quality and Insomnia: A General Population-Based Study in Hunan Province of China. Sci. Rep. 2017, 7, 43690. [Google Scholar] [CrossRef] [PubMed]
- Maqbool, S.; Sundus, O.; Khan, M.S.; Ihtesham, A.; Mohamed, W.; Khurshid, R.; Maqbool, M. Psychological Factors Related to Professional Exams and Their Association with Sleep Quality among Medical Students. J. Rawalpindi Med. Coll. 2021, 25, 40–47. [Google Scholar] [CrossRef]
- Chellappa, S.L.; Aeschbach, D. Sleep and Anxiety: From Mechanisms to Interventions. Sleep Med. Rev. 2022, 61, 101583. [Google Scholar] [CrossRef] [PubMed]
- O’Callaghan, F.; Muurlink, O.; Reid, N. Effects of Caffeine on Sleep Quality and Daytime Functioning. Risk Manag. Healthc. Policy 2018, 11, 263–271. [Google Scholar] [CrossRef]
- Christensen, M.A.; Bettencourt, L.; Kaye, L.; Moturu, S.T.; Nguyen, K.T.; Olgin, J.E.; Pletcher, M.J.; Marcus, G.M. Direct Measurements of Smartphone Screen-Time: Relationships with Demographics and Sleep. PLoS ONE 2016, 11, e0165331. [Google Scholar] [CrossRef]
- Thirunavukkarasu, A.; Wani, F.A.; Alkuaikibi, B.S. Prevalence and Side Effects of Energy Drink Consumption among Medical College Students of Jouf University. Natl. J. Res. Community Med. 2020, 9, 118–122. [Google Scholar]
- Al-Khani, A.M.; Sarhandi, M.I.; Zaghloul, M.S.; Ewid, M.; Saquib, N. A Cross-Sectional Survey on Sleep Quality, Mental Health, and Academic Performance among Medical Students in Saudi Arabia. BMC Res. Notes 2019, 12, 665. [Google Scholar] [CrossRef]
- Yahia, N.; Wang, D.; Rapley, M.; Dey, R. Assessment of Weight Status, Dietary Habits and Beliefs, Physical Activity, and Nutritional Knowledge among University Students. Perspect Public Health 2016, 136, 231–244. [Google Scholar] [CrossRef]
- Lua, P.L.; Wan Putri Elena, W.D. The Impact of Nutrition Education Interventions on the Dietary Habits of College Students in Developed Nations: A Brief Review. Malays J. Med. Sci. 2012, 19, 4–14. [Google Scholar]
- Chourdakis, M.; Tzellos, T.; Papazisis, G.; Toulis, K.; Kouvelas, D. Eating Habits, Health Attitudes and Obesity Indices among Medical Students in Northern Greece. Appetite 2010, 55, 722–725. [Google Scholar] [CrossRef] [PubMed]
- Lourida, I.; Soni, M.; Thompson-Coon, J.; Purandare, N.; Lang, I.A.; Ukoumunne, O.C.; Llewellyn, D.J. Mediterranean Diet, Cognitive Function, and Dementia: A Systematic Review. Epidemiology 2013, 24, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Shiraseb, F.; Siassi, F.; Qorbani, M.; Sotoudeh, G.; Rostami, R.; Narmaki, E.; Yavari, P.; Aghasi, M.; Shaibu, O.M. Higher Dietary Diversity Is Related to Better Visual and Auditory Sustained Attention. Br. J. Nutr. 2016, 115, 1470–1480. [Google Scholar] [CrossRef] [PubMed]
- Fares, J.; Al Tabosh, H.; Saadeddin, Z.; El Mouhayyar, C.; Aridi, H. Stress, Burnout and Coping Strategies in Preclinical Medical Students. N. Am. J. Med. Sci. 2016, 8, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Tian-Ci Quek, T.; Wai-San Tam, W.; Tran, B.X.; Zhang, M.; Zhang, Z.; Su-Hui Ho, C.; Chun-Man Ho, R. The Global Prevalence of Anxiety Among Medical Students: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 2735. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, M.J.; Miranda-Massari, J.R. Diet and Stress. Psychiatr. Clin. 2014, 37, 579–589. [Google Scholar] [CrossRef]
- Wardle, J.; Gibson, E.L. Chapter 55—Diet and Stress: Interactions with Emotions and Behavior. In Stress: Concepts, Cognition, Emotion, and Behavior; Fink, G., Ed.; Academic Press: San Diego, CA, USA, 2016; pp. 435–443. ISBN 978-0-12-800951-2. [Google Scholar]
- Toyoda, A. Nutritional Interventions for Promoting Stress Resilience: Recent Progress Using Psychosocial Stress Models of Rodents. Anim. Sci. J. 2020, 91, e13478. [Google Scholar] [CrossRef]
- de Ridder, D.; Kroese, F.; Evers, C.; Adriaanse, M.; Gillebaart, M. Healthy Diet: Health Impact, Prevalence, Correlates, and Interventions. Psychol. Health 2017, 32, 907–941. [Google Scholar] [CrossRef]
- Antonopoulou, M.; Mantzorou, M.; Serdari, A.; Bonotis, K.; Vasios, G.; Pavlidou, E.; Trifonos, C.; Vadikolias, K.; Petridis, D.; Giaginis, C. Evaluating Mediterranean Diet Adherence in University Student Populations: Does This Dietary Pattern Affect Students’ Academic Performance and Mental Health? Int. J. Health Plan. Manag. 2020, 35, 5–21. [Google Scholar] [CrossRef]
- Kim, S.Y.; Sim, S.; Park, B.; Kong, I.G.; Kim, J.-H.; Choi, H.G. Dietary Habits Are Associated With School Performance in Adolescents. Medicine 2016, 95, e3096. [Google Scholar] [CrossRef]
- Popławska, H.; Dmitruk, A.; Holub, W. Body Composition, physical fitness, nutritional habits and knowledge about food and nutrition in female students of physical education and medicine-related courses. Facta Univ. Ser. Phys. Educ. Sport 2019, 17, 427–436. [Google Scholar] [CrossRef]
- Kosendiak, A.A.; Wysocki, M.P.; Krysiński, P.P. Lifestyle, Physical Activity and Dietary Habits of Medical Students of Wroclaw Medical University during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 7507. [Google Scholar] [CrossRef]
- Popławska, H.; Dębowska, A.; Dmitruk, A.; Hołub, W. Nutritional behaviour and knowledge about food and nutrition among personal trainer students of Józef Piłsudski University of Physical Education in Warsaw, Branch in Biała Podlaska. Rozpr. Społeczne/Soc. Diss. 2022, 16, 104–116. [Google Scholar] [CrossRef]
- Adams, K.M.; Kohlmeier, M.; Zeisel, S.H. Nutrition Education in U.S. Medical Schools: Latest Update of a National Survey. Acad. Med. 2010, 85, 1537–1542. [Google Scholar] [CrossRef] [PubMed]
- Valmórbida, J.L.; Goulart, M.R.; Busnello, F.M.; Pellanda, L.C. Nutritional Knowledge and Body Mass Index: A Cross-Sectional Study. Rev. Assoc. Med. Bras. 2017, 63, 736–740. [Google Scholar] [CrossRef]
- Michels, N.; Man, T.; Vinck, B.; Verbeyst, L. Dietary Changes and Its Psychosocial Moderators during the University Examination Period. Eur. J. Nutr. 2020, 59, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Aschbacher, K.; Kornfeld, S.; Picard, M.; Puterman, E.; Havel, P.J.; Stanhope, K.; Lustig, R.H.; Epel, E. Chronic Stress Increases Vulnerability to Diet-Related Abdominal Fat, Oxidative Stress, and Metabolic Risk. Psychoneuroendocrinology 2014, 46, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Nicoli, M.G.; Junior, R.D.R.L. Binge Eating Disorder and Body Image Perception among University Students. Eat. Behav. 2011, 12, 284–288. [Google Scholar] [CrossRef]
- Palupi, R.; Findyartini, A. The Relationship between Gender and Coping Mechanisms with Burnout Events in First-Year Medical Students. Korean J. Med. Educ. 2019, 31, 331–342. [Google Scholar] [CrossRef]
- Chamunyonga, C.; Singh, A.; Gunn, T.; Edwards, C. Strategies to Develop Student Support Mechanisms in Medical Radiation Sciences Clinical Education. J. Med. Imaging Radiat. Sci. 2020, 51, 512–517. [Google Scholar] [CrossRef]
- Schiller, J.H.; Stansfield, R.B.; Belmonte, D.C.; Purkiss, J.A.; Reddy, R.M.; House, J.B.; Santen, S.A. Medical Students’ Use of Different Coping Strategies and Relationship With Academic Performance in Preclinical and Clinical Years. Teach. Learn. Med. 2018, 30, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Grosso, G.; Castellano, S.; Galvano, F.; Caraci, F.; Ferri, R. Association between Diet and Sleep Quality: A Systematic Review. Sleep Med. Rev. 2021, 57, 101430. [Google Scholar] [CrossRef]
- Ramón-Arbués, E.; Granada-López, J.-M.; Martínez-Abadía, B.; Echániz-Serrano, E.; Antón-Solanas, I.; Jerue, B.A. The Association between Diet and Sleep Quality among Spanish University Students. Nutrients 2022, 14, 3291. [Google Scholar] [CrossRef] [PubMed]
- Frank, S.; Gonzalez, K.; Lee-Ang, L.; Young, M.C.; Tamez, M.; Mattei, J. Diet and Sleep Physiology: Public Health and Clinical Implications. Front. Neurol. 2017, 8, 393. [Google Scholar] [CrossRef] [PubMed]
- Pereira, N.; Naufel, M.F.; Ribeiro, E.B.; Tufik, S.; Hachul, H. Influence of Dietary Sources of Melatonin on Sleep Quality: A Review. J. Food Sci. 2020, 85, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Clark, I.; Landolt, H.P. Coffee, Caffeine, and Sleep: A Systematic Review of Epidemiological Studies and Randomized Controlled Trials. Sleep Med. Rev. 2017, 31, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Pot, G.K. Sleep and Dietary Habits in the Urban Environment: The Role of Chrono-Nutrition. Proc. Nutr. Soc. 2018, 77, 189–198. [Google Scholar] [CrossRef]
- Campanini, M.Z.; Guallar-Castillón, P.; Rodríguez-Artalejo, F.; Lopez-Garcia, E. Mediterranean Diet and Changes in Sleep Duration and Indicators of Sleep Quality in Older Adults. Sleep 2017, 40, zsw083. [Google Scholar] [CrossRef]
- Godos, J.; Ferri, R.; Caraci, F.; Cosentino, F.I.I.; Castellano, S.; Galvano, F.; Grosso, G. Adherence to the Mediterranean Diet Is Associated with Better Sleep Quality in Italian Adults. Nutrients 2019, 11, 976. [Google Scholar] [CrossRef]
- Son, S.; Ro, Y.; Hyun, H.; Lee, H.; Song, K. A Comparative Study on Dietary Behavior, Nutritional Knowledge and Life Stress between Korean and Chinese Female High School Students. Nutr. Res. Pract. 2014, 8, 205–212. [Google Scholar] [CrossRef]
- Otsuka, Y.; Kaneita, Y.; Itani, O.; Osaki, Y.; Higuchi, S.; Kanda, H.; Nakagome, S.; Jike, M.; Ohida, T. Association between Unhealthy Dietary Behaviors and Sleep Disturbances among Japanese Adolescents: A Nationwide Representative Survey. Sleep Biol. Rhythm. 2019, 17, 93–102. [Google Scholar] [CrossRef]
- Scullin, M.K. The Eight Hour Sleep Challenge During Final Exams Week. Teach. Psychol. 2019, 46, 55–63. [Google Scholar] [CrossRef]
- Silber, B.Y.; Schmitt, J.A.J. Effects of Tryptophan Loading on Human Cognition, Mood, and Sleep. Neurosci. Biobehav. Rev. 2010, 34, 387–407. [Google Scholar] [CrossRef] [PubMed]
- Arab, A.; Rafie, N.; Amani, R.; Shirani, F. The Role of Magnesium in Sleep Health: A Systematic Review of Available Literature. Biol. Trace Elem. Res. 2023, 201, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.; St-Onge, M.-P.; Tasali, E. Diet Composition and Objectively Assessed Sleep Quality: A Narrative Review. J. Acad. Nutr. Diet. 2022, 122, 1182–1195. [Google Scholar] [CrossRef] [PubMed]
- Pattanaik, S.; Fastring, D.; Bateman, R.C. A Longitudinal Pilot Study of Stress and Sleep in First-Year Osteopathic Medical Students. J. Med. Educ. Curric. Dev. 2023, 10, 23821205231179532. [Google Scholar] [CrossRef] [PubMed]
- Koles, P.G.; Stolfi, A.; Borges, N.J.; Nelson, S.; Parmelee, D.X. The Impact of Team-Based Learning on Medical Students’ Academic Performance. Acad. Med. 2010, 85, 1739–1745. [Google Scholar] [CrossRef]
- Grzywacz, E.; Jaron, A. Well-Being and Mental Health—Diet, Supplements, Exercise or Sleep? A Review of Reports from the Last Five Years. BJHPA 2020, 12, 73–82. [Google Scholar] [CrossRef]
- Jha, V.; Mclean, M.; Gibbs, T.J.; Sandars, J. Medical Professionalism across Cultures: A Challenge for Medicine and Medical Education. Med. Teach. 2015, 37, 74–80. [Google Scholar] [CrossRef]
- Byrne, E.; Brugha, R.; McGarvey, A. ‘A Melting Pot of Cultures’ –Challenges in Social Adaptation and Interactions amongst International Medical Students. BMC Med. Educ. 2019, 19, 86. [Google Scholar] [CrossRef]
- Malau-Aduli, B.S. Exploring the Experiences and Coping Strategies of International Medical Students. BMC Med. Educ. 2011, 11, 40. [Google Scholar] [CrossRef] [PubMed]
- Abouammoh, N.; Irfan, F.; AlFaris, E. Stress Coping Strategies among Medical Students and Trainees in Saudi Arabia: A Qualitative Study. BMC Med. Educ. 2020, 20, 124. [Google Scholar] [CrossRef] [PubMed]
- Thompson, G.; McBride, R.B.; Hosford, C.C.; Halaas, G. Resilience Among Medical Students: The Role of Coping Style and Social Support. Teach. Learn. Med. 2016, 28, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Narayanasamy, M.; Ruban, A.; Sankaran, P.S. Factors Influencing to Study Medicine: A Survey of First-Year Medical Students from India. Korean J. Med. Educ. 2019, 31, 61–71. [Google Scholar] [CrossRef]
| Variables | Beginning of the AY, N = 570 [IQR], (%) | End of the AY, N = 705 [IQR], (%) |
|---|---|---|
| Age | 19.7 [19.0–20.0] | 20.0 [19.0–20.0] |
| Gender | ||
| Male | 130 (22.8) | 190 (27.0) |
| Female | 440 (77.2) | 515 (73.1) |
| Place of residence | ||
| Rural area | 154 (27.0) | 145 (20.6) |
| City <50,000 * | 137 (24.0) | 146 (20.7) |
| City 50,000–100,000 * | 73 (12.8) | 79 (11.2) |
| City 100,000+ * | 206 (36.2) | 335 (47.5) |
| Body Mass Index | ||
| Mean | 21.7 [19.5–23.4] | 21.6 [19.4–23.1] |
| Underweight | 75 (13.2) | 79 (11.2) |
| Normal weight | 414 (72.6) | 542 (76.9) |
| Overweight | 81 (14.2) | 84 (11.9) |
| Nutritional knowledge mark | ||
| Insufficient | 49 (8.6) | 138 (19.6) |
| Sufficient | 361 (63.3) | 385 (54.6) |
| Good | 160 (28.1) | 182 (25.8) |
| Sleep quality | ||
| Good | 214 (37.5) | 244 (34.6) |
| Poor | 356 (62.5) | 461 (65.4) |
| Beginning of the AY | End of the AY | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | Mdn | IQR | Mean | Mdn | IQR | p-Value | Z | |
| TOTAL | 6.86 | 6.0 | 4.0–9.0 | 7.38 | 7.0 | 5.0–10.0 | 0.0157 | 2.424 |
| DURAT | 0.45 | 0.0 | 0.0–1.0 | 0.79 | 1.0 | 0.0–1.0 | <0.0001 | 7.169 |
| DISTB | 1.19 | 1.0 | 1.0–2.0 | 1.22 | 1.0 | 1.0–2.0 | 0.4041 | 0.956 |
| LATEN | 2.08 | 2.0 | 1.0–3.0 | 1.86 | 2.0 | 1.0–3.0 | 0.0063 | 2.786 |
| DAYDYS | 1.45 | 2.0 | 0.0–2.0 | 1.43 | 2.0 | 0.0–2.0 | 0.6801 | 0.433 |
| HSE | 0.45 | 0.0 | 0.0–1.0 | 0.53 | 0.0 | 0.0–1.0 | 0.5998 | 0.647 |
| SLPQUAL | 0.94 | 1.0 | 1.0–1.0 | 1.01 | 1.0 | 1.0–1.0 | 0.1089 | 1.831 |
| MEDS | 0.30 | 0.0 | 0.0–0.0 | 0.54 | 0.0 | 0.0–1.0 | <0.0001 | 5.842 |
| Beginning of the AY | End of the AY | Beginning vs. End | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Mdn | IQR | p-Value | H | Post hoc | Mean | Mdn | IQR | p-Value | H | Post hoc | p-Value | Z | |
| TOTAL | ||||||||||||||
| Insufficient | 7.82 | 8.0 | 5.0–10.0 | 8.41 | 8.0 | 5.0–11.0 | 0.3026 | −1.029 | ||||||
| Sufficient | 6.72 | 6.0 | 4.0–9.0 | 0.1105 | 4.405 | N/S | 7.43 | 7.0 | 5.0–10.0 | 0.0001 | 19.732 | A > B > C | 0.0127 | −2.491 |
| Good | 6.89 | 6.0 | 4.0–9.0 | 6.49 | 6.0 | 4.0–9.0 | 0.3885 | 0.862 | ||||||
| DURAT | ||||||||||||||
| Insufficient | 0.65 | 0.0 | 0.0–1.0 | 0.80 | 1.0 | 0.0–1.0 | 0.3112 | −1.011 | ||||||
| Sufficient | 0.46 | 0.0 | 0.0–1.0 | 0.1482 | 3.818 | N/S | 0.81 | 1.0 | 0.0–1.0 | 0.7988 | 0.449 | N/S | <0.0001 | −5.834 |
| Good | 0.39 | 0.0 | 0.0–1.0 | 0.75 | 0.0 | 0.0–1.0 | 0.0001 | −3.878 | ||||||
| DISTB | ||||||||||||||
| Insufficient | 1.33 | 1.0 | 1.0–2.0 | 1.51 | 2.0 | 1.0–2.0 | 0.0997 | −1.645 | ||||||
| Sufficient | 1.20 | 1.0 | 1.0–2.0 | 0.0261 | 7.295 | N/S | 1.19 | 1.0 | 1.0–2.0 | <0.0001 | 40.276 | A > B, C | 0.9566 | 0.054 |
| Good | 1.12 | 1.0 | 1.0–1.0 | 1.05 | 1.0 | 1.0–1.0 | 0.2314 | 1.196 | ||||||
| LATEN | ||||||||||||||
| Insufficient | 2.06 | 2.0 | 1.0–3.0 | 2.00 | 2.00 | 1.0–3.0 | 0.7128 | 0.367 | ||||||
| Sufficient | 2.06 | 2.0 | 1.0–3.0 | 0.8013 | 0.443 | N/S | 1.92 | 2.0 | 1.0–3.0 | 0.0876 | 4.870 | N/S | 0.1596 | 1.406 |
| Good | 2.13 | 2.0 | 1.0–3.0 | 1.64 | 1.0 | 0.0–3.0 | 0.0015 | 3.167 | ||||||
| DAYDYS | ||||||||||||||
| Insufficient | 1.49 | 2.0 | 1.0–2.0 | 1.30 | 1.0 | 0.0–2.0 | 0.2683 | 1.105 | ||||||
| Sufficient | 1.42 | 2.0 | 0.0–2.0 | 0.5655 | 1.140 | N/S | 1.49 | 2.0 | 0.0–2.0 | 0.1724 | 3.516 | N/S | 0.3973 | −0.901 |
| Good | 1.53 | 2.0 | 1.0–2.0 | 1.39 | 2.0 | 0.0–2.0 | 0.2371 | 1.182 | ||||||
| HSE | ||||||||||||||
| Insufficient | 0.61 | 0.0 | 0.0–1.0 | 0.78 | 0.0 | 0.0–1.0 | 0.3564 | −0.921 | ||||||
| Sufficient | 0.44 | 0.0 | 0.0–1.0 | 0.6181 | 0.962 | N/S | 0.53 | 0.0 | 0.0–1.0 | 0.0001 | 19.691 | A > C | 0.2785 | −1.084 |
| Good | 0.44 | 0.0 | 0.0–1.0 | 0.32 | 0.0 | 0.0–0.0 | 0.0289 | 2.184 | ||||||
| SLPQUAL | ||||||||||||||
| Insufficient | 1.06 | 1.0 | 1.0–1.0 | 1.04 | 1.0 | 1.0–2.0 | 0.8932 | 0.133 | ||||||
| Sufficient | 0.92 | 1.0 | 1.0–1.0 | 0.4918 | 1.420 | N/S | 1.01 | 1.0 | 1.0–1.0 | 0.9139 | 0.180 | N/S | 0.1289 | −1.518 |
| Good | 0.94 | 1.0 | 1.0–1.0 | 1.00 | 1.0 | 1.0–1.0 | 0.2952 | −1.046 | ||||||
| MEDS | ||||||||||||||
| Insufficient | 0.61 | 0.0 | 0.0–1.0 | 0.97 | 1.0 | 0.0–2.0 | 0.0229 | −2.274 | ||||||
| Sufficient | 0.23 | 0.0 | 0.0–0.0 | 0.0006 | 14.830 | A > B | 0.49 | 0.0 | 0.0–1.0 | <0.0001 | 50.293 | A > B, C | <0.0001 | −4.930 |
| Good | 0.35 | 0.0 | 0.0–0.0 | 0.33 | 0.0 | 0.0–0.0 | 0.9586 | −0.051 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kosendiak, A.A.; Adamczak, B.B.; Kuźnik, Z.; Makles, S. Impact of Medical School on the Relationship between Nutritional Knowledge and Sleep Quality—A Longitudinal Study of Students at Wroclaw Medical University in Poland. Nutrients 2024, 16, 278. https://doi.org/10.3390/nu16020278
Kosendiak AA, Adamczak BB, Kuźnik Z, Makles S. Impact of Medical School on the Relationship between Nutritional Knowledge and Sleep Quality—A Longitudinal Study of Students at Wroclaw Medical University in Poland. Nutrients. 2024; 16(2):278. https://doi.org/10.3390/nu16020278
Chicago/Turabian StyleKosendiak, Aureliusz Andrzej, Bartosz Bogusz Adamczak, Zofia Kuźnik, and Szymon Makles. 2024. "Impact of Medical School on the Relationship between Nutritional Knowledge and Sleep Quality—A Longitudinal Study of Students at Wroclaw Medical University in Poland" Nutrients 16, no. 2: 278. https://doi.org/10.3390/nu16020278
APA StyleKosendiak, A. A., Adamczak, B. B., Kuźnik, Z., & Makles, S. (2024). Impact of Medical School on the Relationship between Nutritional Knowledge and Sleep Quality—A Longitudinal Study of Students at Wroclaw Medical University in Poland. Nutrients, 16(2), 278. https://doi.org/10.3390/nu16020278







