Telenutrition Education Is Effective for Glycemic Management in People with Type 2 Diabetes Mellitus: A Non-Inferiority Randomized Controlled Trial in Japan
Abstract
1. Introduction
2. Materials and Methods
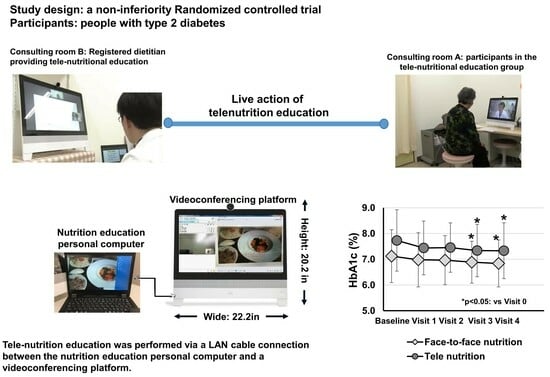
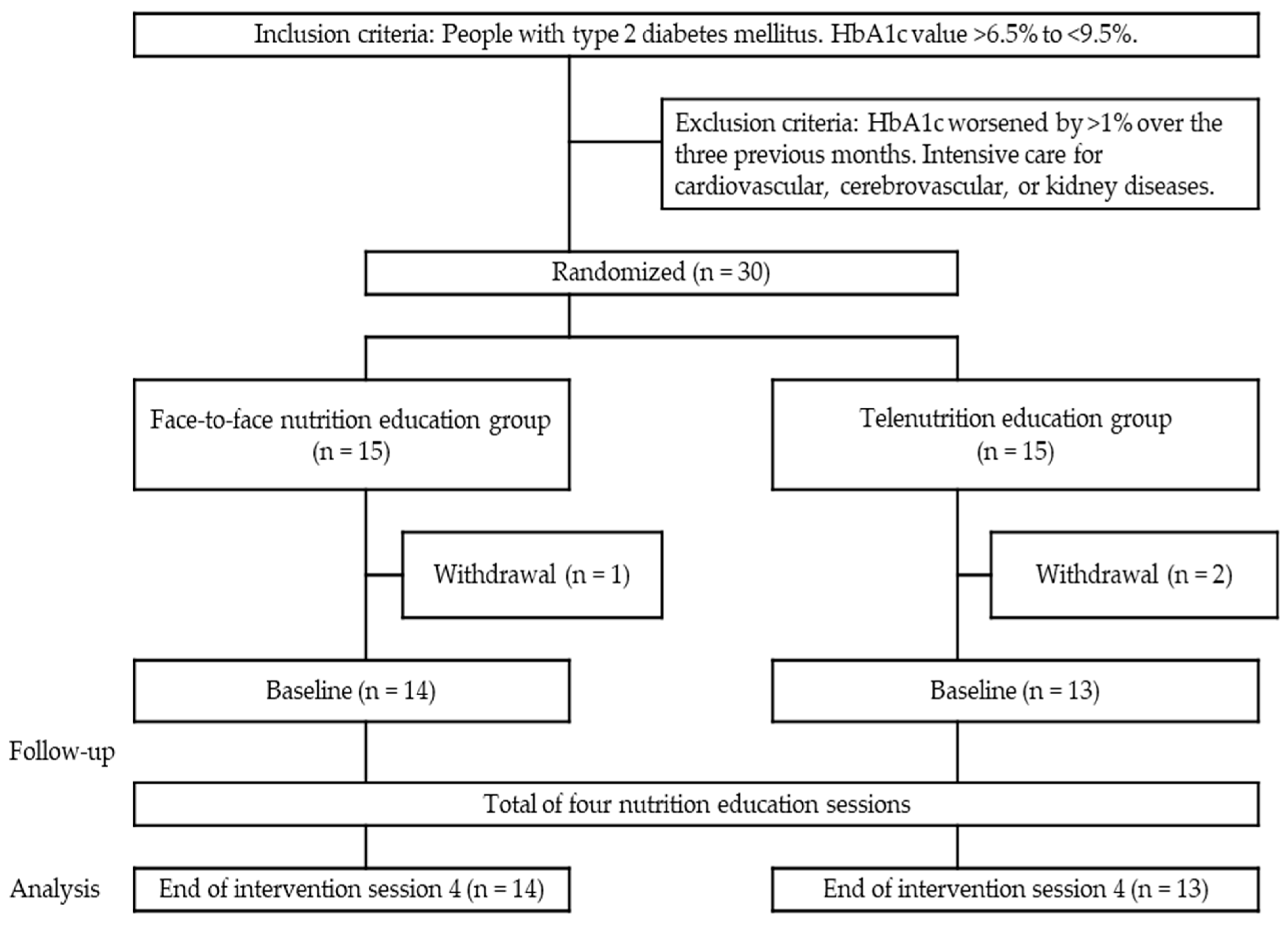
2.1. Study Design
2.2. Participants
2.3. Nutrition Education Program
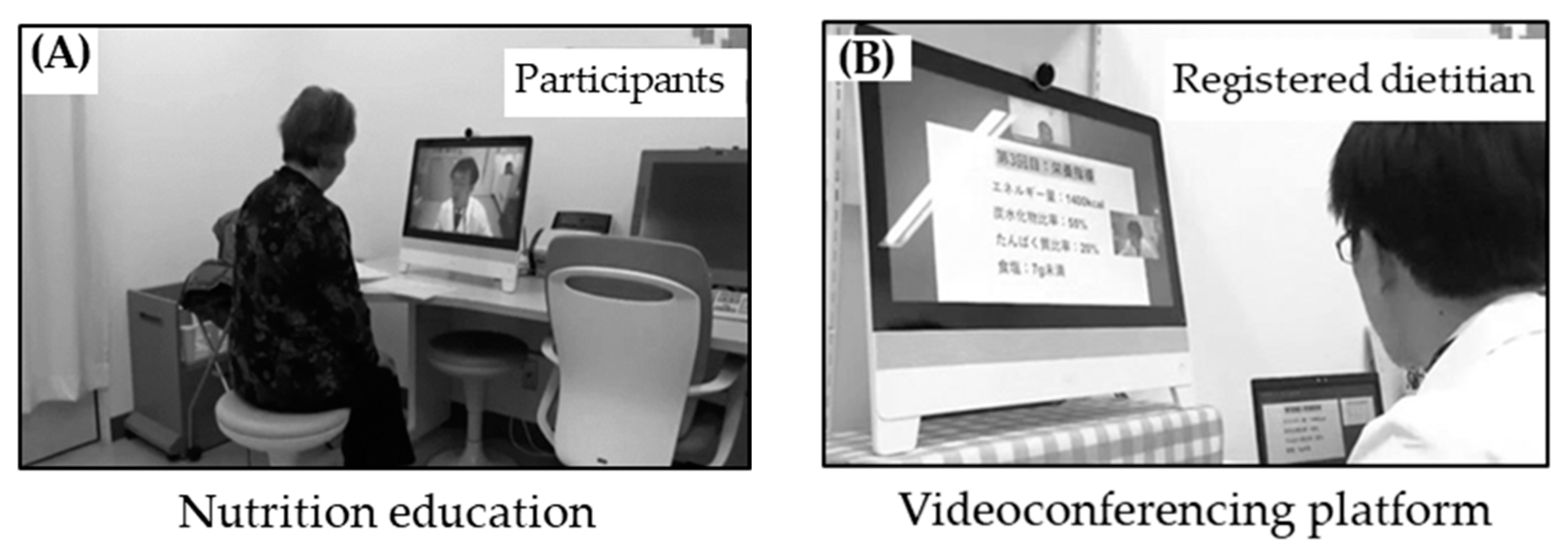
2.4. Telenutrition Education Materials
2.5. Face-to-Face Nutrition Education Materials
2.6. Outcome Measures
2.7. Clinical Date
2.8. Assessment of Physical Activity
Assessment of Body Composition
2.9. Assessments of Health Behavior Change
2.10. Assessment of Total Energy, Macronutrients, and Salt Intake
2.11. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Diabetes Association Professional Practice Committee; Draznin, B.; Aroda, V.R.; Bakris, G. 16. Diabetes care in the hospital: Standards of medical care in diabetes-2022. Diabetes Care 2022, 45 (Suppl. S1), S244–S253. [Google Scholar] [CrossRef]
- Correia, J.C.; Waqas, A.; Huat, T.S.; Gariani, K.; Jornayvaz, F.R.; Golay, A.; Pataky, Z. Effectiveness of therapeutic patient education interventions in obesity and diabetes: A systematic review and meta-analysis of randomized controlled trials. Nutrients 2022, 14, 3807. [Google Scholar] [CrossRef] [PubMed]
- Guilbert, E.; Perry, R.; Whitmarsh, A.; Sauchelli, S. Short-term effectiveness of nutrition therapy to treat type 2 diabetes in low-income and middle-income countries: Systematic review and meta-analysis of randomised controlled trials. BMJ Open 2022, 12, e056108. [Google Scholar] [CrossRef] [PubMed]
- Brunton, C.; Arensberg, M.B.; Drawert, S.; Badaracco, C.; Everett, W.; McCauley, S.M. Perspectives of registered dietitian nutritionists on adoption of telehealth for nutrition care during the COVID-19 pandemic. Healthcare 2021, 9, 235. [Google Scholar] [CrossRef]
- Gnagnarella, P.; Ferro, Y.; Monge, T.; Troiano, E.; Montalcini, T.; Pujia, A.; Mazza, E. Telenutrition: Changes in professional practice and in the nutritional assessments of Italian dietitian nutritionists in the COVID-19 era. Nutrients 2022, 14, 1359. [Google Scholar] [CrossRef]
- Dhediya, R.; Chadha, M.; Bhattacharya, A.D.; Godbole, S.; Godbole, S. Role of telemedicine in diabetes management. J. Diabetes Sci. Technol. 2023, 17, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Fitzner, K.K.; Heckinger, E.; Tulas, K.M.; Specker, J.; McKoy, J. Telehealth technologies: Changing the way we deliver efficacious and cost-effective diabetes self-management education. J. Health Care Poor Underserved 2014, 25, 1853–1897. [Google Scholar] [CrossRef]
- Hinchliffe, N.; Capehorn, M.S.; Bewick, M.; Feenie, J. The potential role of digital health in obesity care. Adv. Ther. 2022, 39, 4397–4412. [Google Scholar] [CrossRef]
- Morgan-Bathke, M.; Raynor, H.A.; Baxter, S.D.; Halliday, T.M.; Lynch, A.; Malik, N.; Garay, J.L.; Rozga, M. Medical nutrition therapy interventions provided by dietitians for adult overweight and obesity management: An Academy of Nutrition and Dietetics evidence-based practice guideline. J. Acad. Nutr. Diet. 2023, 123, 520–545.e10. [Google Scholar] [CrossRef]
- Haneda, M.; Noda, M.; Origasa, H.; Noto, H.; Yabe, D.; Fujita, Y.; Goto, A.; Kondo, T.; Araki, E. Japanese clinical practice guideline for diabetes 2016. Diabetol. Int. 2018, 9, 1–45. [Google Scholar] [CrossRef]
- Japan Diabetes Society. Food Exchange Lists—Dietary Guidance for Persons with Diabetes, 7th ed.; Bunkodo, Co., Ltd.: Tokyo, Japan, 2013; pp. 1–132. (In Japanese) [Google Scholar]
- Food and Nutrition Press Education. Japan Dietetic Association. Available online: https://www.dietitian.or.jp/english/health/# (accessed on 10 July 2023).
- Writing Group of the Nutrition Care Process; Standardized Language Committee. Nutrition care process and model part I: The 2008 update. J. Am. Diet. Assoc. 2008, 108, 1113–1117. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.F.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; DiClemente, C.C.; Norcross, J.C. In search of how people change. Applications to addictive behaviors. Am. Psychol. 1992, 47, 1102–1114. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Health and Nutrition. The summary report from the scientific committee of “dietary reference intakes for Japanese”. Ministry of Health, Labour and Welfare, Toyama building official Web site. Diet. Ref. Intakes Jpn. 2015. Available online: https://www.mhlw.go.jp/stf/shingi/0000041824.html (accessed on 21 July 2021). (In Japanese).
- Yamazaki, S.; Takano, T.; Tachibana, K.; Takeda, S.; Terauchi, Y. Comparison of the effectiveness of once-daily alogliptin/metformin and twice-daily anagliptin/metformin combination tablet in a randomized, parallel-group, open-label trial in Japanese patients with type 2 diabetes. Diabetes Ther. 2022, 13, 1559–1569. [Google Scholar] [CrossRef]
- Matsuhisa, M.; Koyama, M.; Cheng, X.; Takahashi, Y.; Riddle, M.C.; Bolli, G.B.; Hirose, T.; on behalf of the EDITION JP 1 Study Group. New insulin glargine 300 U/mL versus glargine 100 U/ml in Japanese adults with type 1 diabetes using basal and mealtime insulin: Glucose control and hypoglycaemia in a randomized controlled trial (EDITION JP 1). Diabetes Obes. Metab. 2016, 18, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Meneghini, L.; Atkin, S.L.; Gough, S.C.L.; Raz, I.; Blonde, L.; Shestakova, M.; Bain, S.; Johansen, T.; Begtrup, K.; Birkeland, K.I.; et al. The efficacy and safety of insulin degludec given in variable once-daily dosing intervals compared with insulin glargine and insulin degludec dosed at the same time daily: A 26-week, randomized, open-label, parallel-group, treat-to-target trial in individuals with type 2 diabetes. Diabetes Care 2013, 36, 858–864. [Google Scholar] [CrossRef]
- Siopis, G.; Colagiuri, S.; Allman-Farinelli, M. Effectiveness of dietetic intervention for people with type 2 diabetes: A meta-analysis. Clin. Nutr. 2021, 40, 3114–3122. [Google Scholar] [CrossRef]
- Robert, C.; Erdt, M.; Lee, J.; Cao, Y.; Naharudin, N.B.; Theng, Y.L. Effectiveness of ehealth nutritional interventions for middle-aged and older adults: Systematic review and meta-analysis. J. Med. Internet Res. 2021, 23, e15649. [Google Scholar] [CrossRef]
- Ventura Marra, M.V.; Lilly, C.L.; Nelson, K.R.; Woofter, D.R.; Malone, J. A pilot randomized controlled trial of a telenutrition weight loss intervention in middle-aged and older men with multiple risk factors for cardiovascular disease. Nutrients 2019, 11, 229. [Google Scholar] [CrossRef]
- Schrauben, S.J.; Inamdar, A.; Yule, C.; Kwiecien, S.; Krekel, C.; Collins, C.; Anderson, C.; Bailey-Davis, L.; Chang, A.R. Effects of dietary app-supported tele-counseling on sodium intake, diet quality, and blood pressure in patients with diabetes and kidney disease. J. Ren. Nutr. 2022, 32, 39–50. [Google Scholar] [CrossRef]
- Benson, G.A.; Sidebottom, A.; Hayes, J.; Miedema, M.D.; Boucher, J.; Vacquier, M.; Sillah, A.; Gamam, S.; VanWormer, J.J. Impact of ENHANCED (diEtitiaNs Helping pAtieNts CarE for Diabetes) telemedicine randomized controlled trial on diabetes optimal care outcomes in patients with type 2 diabetes. J. Acad. Nutr. Diet. 2019, 119, 585–598. [Google Scholar] [CrossRef]
- Dyson, P.A.; Beatty, S.; Matthews, D.R. An assessment of lifestyle video education for people newly diagnosed with type 2 diabetes. J. Hum. Nutr. Diet. 2010, 23, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Pickup, J.C.; Freeman, S.C.; Sutton, A.J. Glycaemic control in type 1 diabetes during real time continuous glucose monitoring compared with self monitoring of blood glucose: Meta-analysis of randomised controlled trials using individual patient data. BMJ 2011, 343, d3805. [Google Scholar] [CrossRef]
- Coniff, R.; Krol, A. Acarbose: A review of US clinical experience. Clin. Ther. 1997, 19, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Muramoto, A.; Matsushita, M.; Kato, A.; Yamamoto, N.; Koike, G.; Nakamura, M.; Numata, T.; Tamakoshi, A.; Tsushita, K. Three percent weight reduction is the minimum requirement to improve health hazards in obese and overweight people in Japan. Obes. Res. Clin. Pract. 2014, 8, e466–e475. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Wang, T.; Gao, M.; Wang, F.; Zhu, X.; Zhang, X.; Li, D.; Gan, Y.; Zhang, Y.; Gao, Y.; et al. Association of glucose control and stages of change for multiple self-management behaviors in patients with diabetes: A latent profile analysis. Patient Educ. Couns. 2020, 103, 214–219. [Google Scholar] [CrossRef]
- Tseng, H.M.; Liao, S.F.; Wen, Y.P.; Chuang, Y.J. Stages of change concept of the transtheoretical model for healthy eating links health literacy and diabetes knowledge to glycemic control in people with type 2 diabetes. Prim. Care Diabetes 2017, 11, 29–36. [Google Scholar] [CrossRef]
- Rigby, R.R.; Mitchell, L.J.; Hamilton, K.; Ball, L.; Williams, L.T. Analyzing dietary behaviors self-reported by people with diabetes using a behavior change technique taxonomy. J. Nutr. Educ. Behav. 2022, 54, 753–763. [Google Scholar] [CrossRef]
- Vartanian, L.R.; Reily, N.M.; Spanos, S.; Herman, C.P.; Polivy, J. Self-reported overeating and attributions for food intake. Psychol. Health 2017, 32, 483–492. [Google Scholar] [CrossRef]
- Keenan, G.S.; Childs, L.; Rogers, P.J.; Hetherington, M.M.; Brunstrom, J.M. The portion size effect: Women demonstrate an awareness of eating more than intended when served larger than normal portions. Appetite 2018, 126, 54–60. [Google Scholar] [CrossRef] [PubMed]

| Baseline of Intervention: Before Session 1 | Face-to-Face Nutrition Group (n = 14) | Telenutrition Group (n = 13) | p vs. between Groups 1 |
|---|---|---|---|
| Age, years | 64.0 ± 9.2 | 62.8 ± 10.7 | 0.766 |
| Sex, Female/male | 10/4 | 9/4 | 0.999 |
| Duration of type 2 diabetes, year | 14.3 ± 8.2 | 16.9 ± 11.1 | 0.488 |
| HbA1c, % | 7.1 ± 1.0 | 7.7 ± 1.2 | 0.166 |
| Body weight, kg | 66.6 ± 9.0 | 66.9 ± 10.2 | 0.950 |
| BMI, kg/m2 | 27.6 ± 3.2 | 27.5 ± 4.6 | 0.958 |
| SBP, mmHg | 133 ± 13 | 133 ± 7 | 0.930 |
| Behavior change stage, score | 4 [3, 5] | 4 [3, 4] | 0.430 |
| Total energy intake, kcal/day | 1964 ± 295 | 1944 ± 354 | 0.874 |
| End of Intervention: After Session 4 | Face-to-Face Nutrition Group (n = 14) | 1 p vs. Baseline | Telenutrition Group (n = 13) | 1 p vs. Baseline |
|---|---|---|---|---|
| Primary outcome | ||||
| HbA1c, % | 6.8 ± 0.8 | 0.002 | 7.3 ± 1.1 | 0.012 |
| Secondary outcome | ||||
| Body weight, kg | 65.7 ± 10.8 | 0.019 | 64.9 ± 8.6 | 0.008 |
| SBP, mmHg | 130 ± 13 | 0.016 | 130 ± 13 | 0.025 |
| Behavior change stage, score | 7 [5, 8] | 0.001 | 7 [5, 7] | 0.001 |
| Total energy intake, kcal/day | 1841 ± 298 | 0.001 | 1847 ± 321 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mori, H.; Taniguchi, S.; Tamaki, Y.; Tamaki, M.; Akehi, Y.; Kuroda, A.; Matsuhisa, M. Telenutrition Education Is Effective for Glycemic Management in People with Type 2 Diabetes Mellitus: A Non-Inferiority Randomized Controlled Trial in Japan. Nutrients 2024, 16, 268. https://doi.org/10.3390/nu16020268
Mori H, Taniguchi S, Tamaki Y, Tamaki M, Akehi Y, Kuroda A, Matsuhisa M. Telenutrition Education Is Effective for Glycemic Management in People with Type 2 Diabetes Mellitus: A Non-Inferiority Randomized Controlled Trial in Japan. Nutrients. 2024; 16(2):268. https://doi.org/10.3390/nu16020268
Chicago/Turabian StyleMori, Hiroyasu, Satoshi Taniguchi, Yu Tamaki, Motoyuki Tamaki, Yuko Akehi, Akio Kuroda, and Munehide Matsuhisa. 2024. "Telenutrition Education Is Effective for Glycemic Management in People with Type 2 Diabetes Mellitus: A Non-Inferiority Randomized Controlled Trial in Japan" Nutrients 16, no. 2: 268. https://doi.org/10.3390/nu16020268
APA StyleMori, H., Taniguchi, S., Tamaki, Y., Tamaki, M., Akehi, Y., Kuroda, A., & Matsuhisa, M. (2024). Telenutrition Education Is Effective for Glycemic Management in People with Type 2 Diabetes Mellitus: A Non-Inferiority Randomized Controlled Trial in Japan. Nutrients, 16(2), 268. https://doi.org/10.3390/nu16020268