Abstract
Multiple Myeloma (MM) is the second most prevalent hematologic malignancy, and its incidence has been increasing enormously in recent years. The prognosis of MM has changed radically with the introduction of new drugs that have improved life expectancy; recurrences are a common occurrence during the course of the disease and are characterized by an increase in refractory to treatment. Moreover, MM patients are challenged by quality of life-related concerns while limited conventional therapy may be offered. This includes bone pain and dialysis due to the complications of acute renal failure. We, therefore, believe that it is very important to add new treatment modalities, including supplements, nutritional modifications, acupuncture, and mind–body therapies, with the goal of improving treatment tolerance, effectiveness, and patients’ quality of life. Moreover, many patients use some of these supplements on their own, in the hope of reducing the side effects, so it is even more important to know their action and potential. The purpose of this review is to illustrate all these strategies potentially available to enrich our approach to this, to date, incurable disease.
Keywords:
Multiple Myeloma; nutrition; acupuncture; vitamin D; supplementation; integrative medicine 1. Introduction
Multiple Myeloma (MM) represents 10–15% of all hematological malignancies [1,2,3].
The last few years were characterized by a significant improvement in available therapies for this disease, including new-generation immune modulators and proteasome inhibitors (PIs), monoclonal antibodies, or immunotherapy (bispecific T-cell engagers or Chimeric Antigen Receptor T cell therapies, so-called CAR-T) [2].
Following this progress, the median overall survival has more than tripled [2]. However, MM is still an incurable disease and has become a chronic condition with patients experiencing many symptoms related to the disease itself or its treatment, which impacts health-related quality of life (QoL) [4,5,6,7]. These include pain, fatigue, sexual dysfunction, sleep disorders, immune deficiency, anxiety, depression, and/or loss of control [5,6,7,8], making patients with MM the most symptomatic in the haemato-oncologic field [9]. In the last few years, Integrative Oncology (IO) has been developed, and subsequently, Integrative Hematology (IH) was defined as a separate entity [10]. IO is a “patient-centered, evidence-informed field of cancer care that utilizes mind and body practices, natural products, and/or lifestyle modifications from different traditions alongside conventional cancer treatments, and aims to optimize health, QoL, and clinical outcomes across the cancer care continuum” [11].
Specifically, in the case of MM, patients have been shown to use complementary and alternative medicine widely but, generally, without informing their hematologist [12], potentially leading to safety issues [13]. The integrative approach to the treatment of myeloma therefore has many objectives: firstly, a reduction in disease-related symptoms such as bone pain, which is very detrimental to the patient’s life [9,14,15]; and a reduction in treatment side effects, allowing greater compliance to them as well as greater effectiveness. Another goal is to reduce the toxicity of drugs and improve the performance of the immune system. A patient with MM has many unmet needs, and a patient-centered approach, which includes mind–body techniques, can help to better manage the disease and therapies.
Finally, some techniques have also shown efficacy in improving the course of the disease [16]. In the present work, we aimed to review the different kinds of complementary and integrative techniques that may be effective and safe for the management of MM patients. The goal is also to propose preliminary consensus guidelines based on the existing literature for the safe and effective use of IH in MM.
2. Nutrition, Lifestyle Changes and Microbiota
2.1. Nutrition, Lifestyle Changes, and the Link with Pathogenesis and Progression of MM
Recently, a link between nutrition, lifestyle, and MM has emerged [17]. In addition, with the lengthening of the life of MM patients due to an improvement in the available treatments, it may be useful to design a nutritional-based consultation on how to improve the QoL of patients coping with MM. In particular, Monoclonal Gammopathy of Unknown Significance (MGUS) and Smoldering MM are situations in which preventive interventions may be considered.
In a study conducted with patients with MM, following diagnosis, 82% reported nutrition-related questions addressed to non-medical sources rather than the hematologist. Furthermore, 94% of those who received advice from a hematologist followed their instructions, which indicates that the hematologist’s expertise can address this need [18].
Firstly, nutrition could play a role in MM prevention strategy. This could be important to take into account: the protective role in the pathogenesis of the MM of some foods may also be associated in some cases with an antitumor role in the stage of overt disease.
Several studies suggest an association between diet and MM incidence. For example, the Epic study shows cancer risk reduction in vegetarians, vegans, and fish eaters, especially regarding MM [19].
Some case-control studies confirm the trend toward the protective action of fish use [20,21]. A meta-analysis [22] focusing precisely on the relationship between fish intake and myeloma showed an inverse but not a linear relationship, suggesting that an intermediate weekly consumption, not too frequent, may be the right compromise between an intake of omega 3, presumably responsible for the beneficial effect, and that of ocean pollutants, unfortunately, present especially in large fish.
Omega 3, in addition to the known anti-inflammatory effect, has demonstrated a specific action on mouse models of MM in vitro in which they can reduce cell growth. The reduction in interleukin 6 (IL6) production could also be involved in specific anti-MM action [23].
Although some case-control studies have not shown a significant association between fruit consumption and MM risk, there is evidence showing a linear beneficial trend for such an association [24,25].
A recent Icelandic prospective study of cohorts showed that fruit consumption (equal to or greater than 3 times a week in adolescence) is associated with a reduced risk of MGUS and, when consumed in adulthood, with reduced progression of MGUS to MM [25].
Also, adequate consumption of cruciferous, tomatoes, and whole grains may reduce the risk of MGUS and MM, and an excess of refined sugars and sugar-sweetened beverages can increase it [25,26].
The beneficial effect of plant-based foods could be attributed to the action of dietary fibers on the production of butyrate-producing bacteria such as Faecalibacterium Prausnitzii. Also, the presence of molecules with antitumor activity such as isothiocyanates, indoles, and flavonoids (for example, lycopene from tomatoes) can be protective. Fibers and micronutrients in whole grains may be associated with the metabolic effects of glycemic index modulation, reduced insulin stimulation, and reduced production of insulin-like growth factor (IGF1). IGF1 is a molecule well known for its stimulating action on proliferative molecular pathways; also, in MM, its activity has been documented to involve the processes of homing, cell proliferation, apoptosis, angiogenesis, and bone metabolism [27]. The Epic study and other cohort studies show a higher incidence of MM in meat eaters and dairy consumers [19,28]. The high levels of IGF1 resulting from the consumption of dairy products could partly explain this correlation. N-nitroso compounds, heterocyclic amines, and heme present in meat could exert an oxidizing and pro-carcinogenic action as well.
Among other lifestyle factors, alcohol has a controversial impact on the incidence of MM, with a significant reduction in the incidence in moderate drinkers (2–2.9 drinks/day) [29].
It is not clear why this beneficial action of alcohol is different from what happens in other cancers. Still, it could be linked to a direct modulation of the immune system in light and moderate drinkers [30].
2.2. Obesity, Sarcopenia, and MM
The relationship between obesity, MGUS, and myeloma is well known. Not only does obesity affect the incidence of MM but also the progression from MGUS to MM and MM mortality rate. Many mechanisms are involved: the production of IL6 and leptin by fat cells leads to increased inflammation and cell proliferation; the reduction in adiponectin is associated with increased IL6, activation of NFkB, and osteoclastic maturation. Finally, the presence of a more significant adipose tissue in the bone marrow stimulates the proliferation of MM cells and their migration outside the bone marrow [31].
Another important risk factor to consider at diagnosis is the nutritional status of the patient, especially the presence of sarcopenia, which is a negative prognostic factor.
Sarcopenia is frequent in patients with MM at diagnosis; the presence of reduced subcutaneous adipose tissue is associated with a worse prognosis [32].
The Controlling Nutritional Status (CONUT) score is a simpler tool to use but equally effective in predicting the outcome of MM patients, especially those undergoing autologous stem cell transplantation (ASCT) [33].
Finally, the risk of muscle mass deficiency must never be neglected, and an adequate protein intake must be guaranteed to the patient at diagnosis and throughout the treatment, which can itself contribute to sarcopenia: nausea, mucositis, and lack of physical activity due to bone pain can, in fact, reduce the patient’s food intake.
A daily protein intake of at least 1.4 g/kg appears to be necessary to obtain or maintain adequate muscle mass according to a recent systematic review [34].
2.3. The Role of Microbiota in the Pathogenesis and Treatment of MM
The microbiota of patients with MM shows less alpha diversity at diagnosis than controls [35]. Although there are conflicting data on the association of the disease with the presence of butyrate-producing bacteria, a dysbiotic feature seems to be present in patients with MM [35,36], and a correlation between levels of Interleukin 17 (IL17) in the bone marrow of patients with MM and the composition of the microbiota is currently being explored (NCT05712967) [37]. This increase could be induced by foods rich in salt and the subsequent increase in nitrogen-recycling bacteria (e.g., Klebsiella and Streptococcus) [38].
The microbiota is also inevitably involved in the link between nutrition and MM mentioned above, being the first mediator of the effect of food on the body.
This could affect not only the pathogenesis of the disease but also its course and response to therapy. A clinical study of 34 MM patients in maintenance therapy with lenalidomide showed interesting results in this regard. Patients following a plant-based diet had a higher fecal concentration of butyrate, the consequence of an increase in butyrate-producers E. Hallii and F. Prausnitzii [39]. The increased fecal butyrate concentration was associated with a more sustained minimal residual disease negativity, which is known to be predictive of longer Progression-Free Survival [40].
Although this is a small study, these results suggest and confirm an essential association between nutrition, microbiota, and the effect of conventional therapy in MM patients. Recently, the detection of a specific microbiota in the bone marrow of patients with MM, mainly localized intracellularly, widens this scenario. The researchers hypothesize that the presence of intratumor MB is a consequence of an impairment of the gut MB and intestinal permeability, confirming a direct relationship between gut MB and the pathogenesis of MM [41]. Further well-designed clinical studies are necessary to clarify the therapeutic potential of an integrated approach that includes a “pro-microbiota” diet. At present, the Nutrivention3 study (NCT05640843) is a randomized, multi-center pilot study comparing 150 patients to evaluate the effects of a plant-based diet versus an omega 3 or placebo supplementation in patients with MGUS or SMM and high Body Mass Index on the concentration of fecal butyrate [42].
3. Natural Compounds and Vitamins: Their Potential Role in the Treatment of MM
3.1. Curcumin
Curcumin (diferuloylmethane), the main bioactive component of Turmeric (curcuma longa), has demonstrated anti-inflammatory, antibacterial, and anticancer in vitro effects against many cancer cell lines [43].
In MM, its action is expressed both by affecting specific signaling pathways and with an epigenetic modulatory effect.
Among the various effects, Nuclear factor kappa B (NFκB) inhibition appears to be particularly important in this disease: one of the backbones of MM therapy is, in fact, constituted by PIs, which cause NFκB inhibition. This would suggest a possible hypothetical interaction between curcumin and PIs.
In vitro, curcumin has been shown to enhance the cytotoxic effect of bortezomib (the first PI) [44]; it also synergizes with carfilzomib through a major downregulation of NFkB [45].
Curcumin was also reported to downregulate the expression of cyclin D1, inhibit STAT3 phosphorylation, and reduce IL6, even in patients with unfavorable cytogenetics and regardless of Tumor Protein 53 (TP53) status: this sensitivity to curcumin is also present both in the cells of patients at diagnosis and at recurrence, demonstrating that resistance phenomena do not occur [46,47].
Finally, it inhibits osteoclastogenesis by inhibiting RANKL [48].
The main reason for the incurability of MM could be related to the presence of cancer stem cells (CSCs): they confer treatment resistance and are associated with recurrence and poor prognosis. Recently, curcumin has been demonstrated to be efficient against these cells, increasing apoptosis [49].
As an epigenetic modulator, curcumin also appears to act in MM by inducing DNA methyltransferase (DNMT)-mediated mTOR methylation: hypermethylation of the mTOR promoter region would inhibit the antiapoptotic action of this molecular pathway [50]; unlike the hypomethylating drugs used in hematology, such as azacitidine, curcumin would not cause an overall change in DNA methylation but only the specific one caused by DNMT3a and DNMT3b, and this could give it more peculiar anti-myeloma activity.
Finally, in some mouse models, it increases chemosensitivity to dexamethasone, doxorubicin, and melphalan and synergizes not only with the action of bortezomib and carfilzomib but also with immunomodulatory imide drugs (IMiDs) such as lenalidomide and thalidomide [51]; synergy with lenalidomide is expressed through the suppression of the cereblon gene, which is exactly the target of the IMiDs.
However, the literature on the association of these promising in vitro effects with effective clinical action is presently limited.
The first study, published in 2009, involved 26 patients with MGUS treated with 4 g daily of curcumin; in this study, the monoclonal component decreased in 50% of patients, in keeping with a reduction in markers of bone resorption [52]. Following, the authors published a randomized double-blind placebo-controlled trial in both MGUS and smoldering myeloma: they used curcumin in doses of 4 and 8 g daily, and this led to a reduction in the chain k/λ ratio by 35 and 36%, respectively, as well as the markers of bone resorption [53]. As not all cases of MGUS and smoldering myeloma evolve into frank disease, the use of conventional chemotherapy is not justified in these cases; precisely for this reason, supplements such as curcumin express all their chemopreventive potential in this phase of the pathogenesis of the disease.
In this regard, Zaidi et al. [54] published a case study in which curcumin (8 g daily) was associated with hyperbaric sessions that led to disease control in a case of refractory relapsed MM for 60 months, with an excellent safety profile.
A more recently published case study reported the efficacy of curcumin in replacing dexamethasone in patients who were intolerant to the latter. The authors treated 15 patients who were under treatment with regimens containing either IMiDs or PI combined with dexamethasone, substituting the latter with C3 complex curcumin at a dosage of 3–4 g daily. The researchers concluded that curcumin may act as a steroid-sparing agent in patients with MM who are intolerant of dexamethasone, with an excellent tolerability profile [55]. These data are exciting considering that in MM, we often use therapeutic regimens, if effective, up to progression; if these medications, as often happens, contain cortisone, the patient is frequently subjected to massive and prolonged doses of steroids and their heavy long-term side effects. Even with the aim of reducing steroid load and toxicity, curcumin is, therefore, an engaging weapon to take into consideration.
Finally, a pilot randomized trial was conducted [56] in which 33 newly diagnosed patients, ineligible for transplant, were randomized to receive melphalan 4 mg/m2 plus prednisone 40 mg/m2 for 7 days and curcumin 8 g/daily for 28 days or placebo for 4 cycles. Curcumin-treated patients showed a higher treatment response rate (75% vs. 33.3%) with a contextual reduction in NF-κB, IL-6, VEGF, and TNF-α levels. These few but promising results emphasize the need for more well-designed clinical studies to explore the potential additive healing effect of curcumin, as well as to identify the type of biochemical form most available (e.g., extract, liposomal, and water-soluble form).
3.2. Epigallocatechin Gallate (EGCG)
EGCG has shown an antiapoptotic effect on MM cells in vitro through the stimulation of ROS and a reduction in the levels of peroxiredoxin (an antioxidant molecule); moreover, a crucial role is played by the selective interaction with the laminin 1 receptor, which is much higher in patients with MM than in controls and whose absence prevents the apoptotic effect of EGCG [57]. Other mechanisms involve the inactivation of the enhancer of zeste homolog2 (EZH2) and the mitochondrial apoptosis pathway [58].
Although the in vitro antitumor efficacy of EGCG in MM is undisputed, its in vivo role and, in particular, its interaction with bortezomib, a backbone of the induction therapy, is controversial. In 2009, two contradictory studies were published in this regard. Golden et al., demonstrated that EGCG and other polyphenols derived from green tea prevented tumor cell apoptosis induced by bortezomib in vitro and in vivo at concentrations also easily achievable in humans: the antagonistic action of EGCG was evident only with boronic acid-based PIs, so the binding with the boronic acid of the molecule appears to be the mechanism underlying this inhibitory mechanism [59]. In the second work, however, a synergistic effect between the two substances was demonstrated, and this would be due, in the opinion of the authors, to the higher dosage of EGCG and bortezomib used [60]. The discrepancy of these data, the lack of clinical studies, and the possible difference between what happens in vitro and what occurs in vivo due to certain variables such as absorption and bioavailability impose a prudent attitude, especially until well-designed clinical trials are available.
Some more recent studies affirmed again the antagonism between the two substances [61,62]; in particular, Qiu et al. [62] have shown that EGCG may neutralize bortezomib-induced apoptosis, activate Wnt/β-catenin signaling, and result in the accumulation of beta catenin, which subsequently activated c-myc and cyclin D1. The authors conclude by discouraging green tea intake during bortezomib therapy.
Finally, EGCG is very interesting for its action on glutaminolysis: MM cells have a glutamine addiction, which is responsible for their dependence on glutamine uptake. In a recent study [63], Li et al., showed that the combination of EGCG and telaglenastat, a glutaminase inhibitor, synergistically inhibits proliferation and induces apoptosis in MM cells in vitro. Targeting glutamine metabolism, therefore, should be a winning strategy.
3.3. Vitamin D
Vitamin D deficiency is found in most patients with MM at diagnosis, as in many other types of cancer. This deficit is described as “alarming” in patients with bone involvement [64]. Even some peculiar polymorphisms of the vitamin D receptor (VDR) gene may be a molecular marker of the risk of development of the disease [65].
Low levels of vitamin D correlate with an increased C-reactive protein (CRP) and the ISS stage at the time of diagnosis: they may, therefore, be predictive of more advanced disease [66]. It is very interesting to observe how the action of some drugs used in MM also passes through the modulation of the molecular pathway of vitamin D: bortezomib, for example, upregulates the production of VDR, and this effect is amplified in the presence of vitamin D.
Thalidomide- or bortezomib-induced neuropathy is more severe in the case of concomitant vitamin D deficiency, which, however, does not appear to influence the incidence [67].
Vitamin D and its active metabolite, calcitriol, act as modulators of the immune system: absolute lymphocyte count recovery and relapse-free survival after ASCT are improved after daily administration of calcitriol of 0.25 μg, as shown in a randomized-controlled trial (RCT) vs. placebo [68].
Interestingly, vitamin D can increase CD38 expression in plasma cells, thereby amplifying the binding of CD38-targeting antibodies; however, the cytotoxicity of the latter could be compromised in case of vitamin D deficiency, which would cause a worse performance of the macrophages associated with myeloma (MAMs). Lenalidomide and pomalidomide can restore the vitamin D pathway in the MAMs, improving their cytotoxicity. In doing so, vitamin D becomes a crucial link to improve the synergy between immune modulators and monoclonal antibodies [69].
The above data may support the rationale to test vitamin D levels at diagnosis and supplement them before starting therapy and during treatment with anti-CD38 and immunomodulatory drugs.
Noteworthily, vitamin D levels do not appear to be significantly associated with the coexistence of bone disease [70].
In Figure 1, the main mechanisms of action of the supplements most studied in the MM are presented.
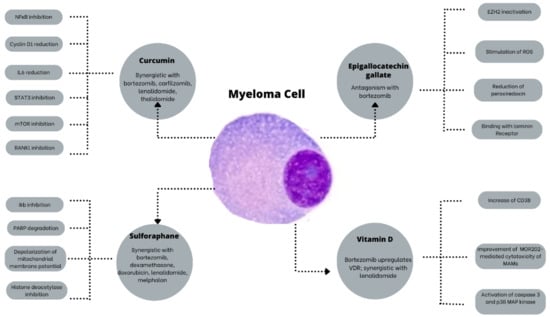
Figure 1.
The main mechanisms of action of the most studied supplements in MM. EZH2: Enhancer of zeste homolog2; IkB: NkB inhibitor; IL6: interleukin 6; MAMs: Macrophages associated with myeloma; mTOR: Mammalian target of rapamycin; NfkB: Nuclear factor kappa B; PARP: poly ADP ribose polymerase; RANKL: Receptor activator of nuclear factor kappa-Β ligand; ROS: Reactive oxygen species; STAT3: Signal transducer and activator of transcription 3; VDR: Vitamin D receptor.
3.4. Others
Ascorbic acid can reduce Bortezomib-induced neurotoxicity by leading to the recovery of damaged Schwann cells; unfortunately, it has been shown to inhibit Bortezomib cytotoxicity in vitro and in vivo, so its supplementation in patients who are on treatment with this PI is not recommended [71,72].
Despite its importance for the immune cells, it is ineffective in improving bone marrow recovery after ASCT both in MM and lymphoma patients, so its use is not advised in this setting [73].
Sulforaphane is an isothiocyanate derived from cruciferous vegetables, which has been shown to have similar action to bortezomib in inhibiting the degradation of inhibitory kappa B kinases (IkB), which, in turn, inhibits the proteasome complex.
Moreover, it shows synergy with dexamethasone, doxorubicin, bortezomib, and melphalan. In in vivo models, it leads to a reduction in the burden of disease and an increase in survival [74].
Resveratrol has shown strong antiangiogenic activity by regulating factors such as VEGF, matrix metalloproteinase-2 (MMP2), and matrix metalloproteinase-9 (MMP9).
By constitutively activating STAT3 and NFκB, it overcomes an essential mechanism of chemoresistance and it has a synergistic interaction with Bortezomib and Thalidomide [75]. There is insufficient clinical evidence to understand the clinical efficacy of resveratrol. In a single phase II study, it was administered in association with bortezomib: in this clinical experience, the toxicity profile was unacceptable, with 50% of patients developing severe renal failure. To date, resveratrol in combination with bortezomib is strongly discouraged. Further studies are needed to clarify the safety of this natural compound in this setting of patients [76].
Cannabinoids are compounds found in plants from the genus Cannabis, of which the most widely used is Cannabis Sativa. In recent years, their role in managing the patient’s symptoms has emerged and they are used primarily to reduce chronic pain and chemotherapy-induced nausea and vomiting and stimulate appetite [77]. Since many different cell lines express CB1/CB2 receptors for cannabinoids, their anti-cancer potential has been extensively investigated recently, in in vitro and in vivo models: among the various plant components most studied for their antiapoptotic activity are delta-trans-9-tetrahydrocannabinol (THC) and cannabidiol (CBD), with the latter being free of psychoactive effects. In contrast to the in vivo and in vitro settings, clinical research is limited, though suggests good patient tolerability even at high doses, particularly in glioblastoma and MM [78]. In MM, in vitro studies have demonstrated reduced viability of myeloma cells and proapoptotic activity in cannabinoid-treated MM cells, including dexamethasone-resistant cells. Cannabinoids can reduce the expression of the β5i subunit of the immunoproteasome, therefore increasing the efficacy of carfilzomib, a second-generation PI. In addition, they allow resistance mechanisms effectively linked to the expression levels of β5i to overcome [79]. These compounds are, therefore, promising not only for improving the symptoms and QoL of patients, but also for their anticancer and synergistic activities with currently used drugs. Further studies are needed to confirm this promising action.
Table 1 shows the potential use of the substances described above.

Table 1.
Potential use of supplements or natural compounds in Multiple Myeloma.
4. Acupuncture
Pain is a common QoL-related concern experienced by MM-diagnosed patients, with various etiologies, such as mechanical due to bone lesions, neuropathic due to the side effects of prescribed drugs (mainly PIs or immune modulators), infections (post-herpetic neuralgia), or direct infiltration of light chains or amyloid into peripheral nerves [80]. The management of these symptoms with conventional drugs is generally unsatisfactory and subject to side effects, while acupuncture has been shown to relieve cancer-related pain safely [81]. In a bibliometric analysis summarizing research conducted between 2012 and 2022, acupuncture was suggested as a leading modality in the treatment of MM-related pain [82,83]. This is particularly in regard to treatment of chemotherapy-induced peripheral neuropathy (CIPN), which is an unmet need in Western medicine [80]. Acupuncture has been widely studied for this condition with positive results [84,85]. Specifically, the widely used proteasome inhibitor (PI) bortezomib can cause CIPN in up to 40% of patients [86]. A number of studies have demonstrated the effectiveness of acupuncture for bortezomib-induced peripheral neuropathy (BIPN). Following case reports [87], a retrospective case series on 5 patients demonstrated the immediate and long-lasting pain reduction associated with acupuncture in BIPN [88]. Acupoints included bilateral ear points and body points (Large Intestine 4 (LI4), Triple Energizer 5 (TE5), Large Intestine 11 (LI11), Stomach 40 (ST40), and BaFeng) on a weekly basis. The effect of the same protocol has been confirmed in 27 patients with BIPN, in which a reduction in specific symptoms has been observed (numbness/tingling in hands and feet, cold sensitivity, and unpleasant feelings), although nerve conduction velocities (NCV) were unchanged [89,90]. Electroacupuncture has also been shown to reduce pain severity and improve QoL, as well as specific motor functions in 19 patients with grade 2 or higher thalidomide- or bortezomib-induced neuropathy [91]. In a 54-patient Chinese RCT, the combination of acupuncture + moxibustion was shown to improve QoL compared to conventional drugs, although no difference was shown in the improvement of NCV [92]. Finally, an additional RCT assigned 104 myeloma patients with CIPN to a methylcobalamin-alone group or one associated with three 28-day cycles of acupuncture in acupoints different than previously described (LR3, ST43, GB41, SP6, ST36, SP10, ST25, GV14, GV12, GV11, GV9, BL13, BL17, and BL58). Each treatment cycle included three daily acupuncture treatments followed by 10 days of treatment once every other day.
This study showed that adding acupuncture led to a significant pain reduction while improving both daily activity and nerve conduction velocities compared to methylcobalamin alone [93]. These studies suggest that acupuncture may be an effective treatment to improve QoL in patients suffering from Myeloma-related CIPN, although its effect on nerve conduction is controversial.
Another important challenge in patients with MM is ASCT, which is still a common practice guideline in fit patients following first-line induction and a reduction in disease burden. Deng et al., published an RCT with 60 patients who were assigned to true or sham acupuncture once daily for 5 days after receiving high-dose chemotherapy for ASCT [94]. Acupoints included GV20, Yintang (Ex-HN3), Heart 7 (HT7), Pericardium 6 (PC6), Stomach 36 (ST36), Spleen 6 (SP6), Kidney 3 (KI3), Liver 3 (LR3), and Ear Shen Men. Although the overall MD Anderson Symptom Inventory (MDASI) improved non-significantly during transplantation, at 15 days and at 30 days [94], true acupuncture was more effective than sham in alleviating nausea, poor appetite, and drowsiness [94,95]. This specifically improved sleep efficiency [96] and reduced the use of analgesics during ASCT and the number of opioid users post-ASCT among opioid-naïve patients [95,97].
Acupuncture’s mechanism of action for such symptom relief in MM patients has been studied as well. A Chinese RCT showed that the improvement of QoL in MM patients following heat-sensitive moxibustion was associated with decreased inflammatory markers, strengthened T-cell immunity, and a rise in the expression of some micro-RNAs (miR-125a, miR-140-5p, and miR-302′) [98]. These chemo-biological changes seem to be involved in the pathophysiology of acupuncture treating MM-associated symptoms. Finally, a murine model mice study demonstrated the synergism between acupuncture and bortezomib in improving survival in mice with MM. The pathophysiology seems to function by decreasing ornithine [99].
Last but not least, acupuncture-related safety concerns should be recognized in patients with MM and decreased immune system activity. This includes neutropenia and hypo-gammaglobulinemia exposing patients to severe infections, as well as thrombocytopenia during ASCT with its high risk of bleeding. The risk of infection following acupuncture therapy is very low. Still, we should note a recent case report on the exacerbation of pyoderma gangrenosum in a patient with MM treated with acupuncture [100]. Therefore, acupuncture should always be practiced with extreme precaution in MM and other immune-compromised patients with active infection, and for skin infection, one should avoid puncturing affected areas. As for severe thrombocytopenia, a recent retrospective chart review analyzing 815 acupuncture sessions on thrombocytopenic patients with hematological malignancies demonstrated the safety of acupuncture even with platelet counts below 20 × 109/L [101]. Table 2 shows the possible indications of acupuncture in MM.

Table 2.
Proposed guidelines on the indications of acupuncture in Multiple Myeloma.
5. Mind–Body Medicine
Mind–body medicine is one of the main IO modalities encompassing a wide spectrum of interventions from traditional medicine systems like Tibetan, Ayurvedic (e.g., Yoga), and Chinese (e.g., Qi Gong) medicine to more contemporary Western approaches of relaxation, guided imagery, hypnosis, and mindfulness-based interventions (MBI). The hallmarks of many mind–body interventions are mindfulness and intention to berating, gentle touch, movement, and spirituality. Recent IO-related clinical guidelines on pain, depression, and anxiety co-published by the Society for Integrative Oncology (SIO) and the American Society of Clinical Oncology (ASCO) recommend mind–body medicine for the following indications: hypnosis in patients who experience procedural pain; MBIs, yoga, relaxation, and music therapy for treating symptoms of anxiety during active treatment; MBIs, yoga, tai chi, and/or qigong for treating anxiety symptoms after cancer treatment; MBIs, yoga, music therapy, and relaxation for depression symptoms during oncology treatment; and MBIs, yoga, and tai chi and/or qigong post-treatment depression [102,103]. In the field of Multiple Myeloma, Lamers et al., reported that as many as 52% of patients desired psychosocial interventions near diagnosis, where relaxation techniques were the most common preferred modality reported by 21% of patients [104]. This inclination toward mind–body intervention is perceived in the context of a coping strategy, which may also correlate with the immunological response after ASCT [105]. In the U.S., LeBlanc et al., reported a pilot RCT with a group of patients diagnosed with MM or Chronic Lymphocytic Leukemia, intending to examine the impact of a Mobile App to support self-management, which also included mindfulness activities [106]. The authors reported that distress tracking and guided meditations were among the most used functions within the app. In another study recruiting patients with a variety of hematological oncology diagnoses (13.8% with MM), patients were randomized to a single session of 30 min mindful breathing versus standard care and reported significantly less fatigue in the intervention group [107]. Bates and colleagues explored the impact of music therapy considered by some scholars in the context of mind–body medicine, while others categorize it independently among the art therapies discipline. The RCT explored symptom management following ASCT in patients with lymphoma or MM and found that the patients receiving music therapy used significantly less narcotic pain medication [108]. In the United Kingdom, semi-structured qualitative interviews in a purposive sample of MM patients suggested that spirituality is one of the main themes that patients perceive as important to consider regarding their QoL [7]. In a stimulating article, Saha and Mallik challenged rehabilitation with patients undergoing MM treatment, emphasizing patients’ unmet spiritual needs in India [109]. In this regard, it is of utmost importance to consider the cross-cultural context of spirituality, which may be regarded in different cultures in close proximity to religion and/or mind–body medicine. In this regard, Sherman and colleagues in the United States studied prospectively religious coping and orientation among 94 myeloma patients undergoing ASCT [110]. The results suggested that religious struggle may contribute to adverse changes in health outcomes in this clinical setting.
6. Discussion
This narrative review aimed to identify the tools that can integrate conventional MM treatment to enhance its effectiveness and tolerability, as well as the quality of life and overall survival of patients with MM.
We have identified four fundamental pillars to build this approach: nutrition, acupuncture, mind–body techniques, and the use of supplements.
Nutrition, also through the remodeling of the microbiota, is, in our opinion and based on the available scientific literature, not only a useful tool in the preventive stage or in cases of MGUS but also an essential therapeutic tool to meet patients’ unmet needs.
Many mechanisms are involved in food’s effects, such as the modulation of IGF1, the reduction in inflammation, and butyrate’s influence on the bone marrow microenvironment. This justifies the need for nutritional counseling and further clinical studies to lay the foundations for the definition of shared nutritional guidelines.
Acupuncture and mind–body techniques, which have a good safety profile, can provide valuable help in improving tolerance and compliance with treatment.
Among supplements and vitamins, we have identified those that have been most studied in MM both for their in vitro action and for their efficacy demonstrated in clinical studies. Most of the data we have available unfortunately come from preclinical studies that, although promising, are not yet confirmed by clinical trials. For this reason, well-designed clinical trials are absolutely necessary: they will allow us to propose guidelines that include the recommended supplements but also provide warnings for those with bad safety profiles. It is also very important to take into account the potential interactions with conventional drugs used in MM. As we have seen, some substances such as vitamin C may limit the effectiveness of drugs such as bortezomib. These are substances often used by the patients without communicating to their hematologist, thinking that they are harmless. In-depth knowledge of the mechanisms of action and possible drug interactions is therefore mandatory. These interactions could also be synergistic, opening up new horizons for integrative therapy, which could be a way of making the best use of the drugs currently at our disposal.
7. Conclusions
Integrative oncology modalities may offer significant improvement of QoL-related concerns in patients coping with Multiple Myeloma diagnosis and treatment. This is particularly relevant in the present era where effective hematology treatment is associated with increased life expectancy.
In this narrative review, we examine the data regarding acupuncture, dietary interventions, and supplements, while also considering mind–body interventions as part of the entire hematologic approach (Figure 2).
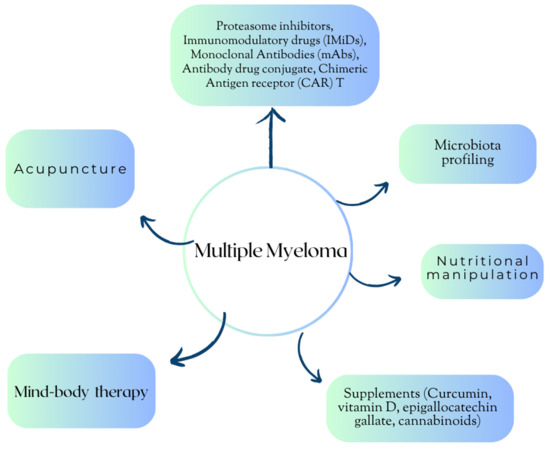
Figure 2.
Multiple Myeloma: an integrative approach.
More studies, primarily randomized controlled, are needed to explore if the effect of these IH modalities is limited to enhanced supportive and palliative care or may also contribute to better therapy efficacy. Not least important is exploring IH modalities’ effects regarding the safety and risk of drug interactions.
Further well-designed clinical trials will allow the construction of evidence-based guidelines.
Author Contributions
Conceptualization, F.A. and I.L.Y.; writing—original draft preparation, F.A., I.L.Y. and E.B.-A.; writing—review and editing, F.A., I.L.Y., E.B.-A. and M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors are grateful to Carla Fiorentini and Sara Andreazzoli for their valuable administrative and technical support.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| ASCO | American Society of Clinical Oncology |
| ASCT | Autologous stem cell transplantation |
| BIPN | Bortezomib-induced peripheral neuropathy |
| CAR-T | Chimeric Antigen Receptor T cell |
| CB1 | Cannabinoid type 1 receptors |
| CB2 | Cannabinoid type 2 receptors |
| CBD | Cannabidiol |
| CIPN | Chemotherapy-induced peripheral neuropathy |
| CRP | C-reactive Protein |
| CSCs | Cancer stem cells |
| DNMT | DNA methyltransferase |
| EGCG | Epigallocatechin 3 gallate |
| EZH2 | Enhancer of zeste homolog2 |
| IH | Integrative Hematology |
| IGF1 | Insulin-like growth factor 1 |
| IkB | NkB inhibitor |
| IL6 | Interleukin 6 |
| IL17 | Interleukin 17 |
| IMiDs | Immunomodulatory imide drugs |
| IO | Integrative Oncology |
| MAMs | Macrophages associated with myeloma |
| MBI | Mindfulness-based interventions |
| MDASI | MD Anderson Symptom Inventory |
| MGUS | Monoclonal gammopathy of unknown significance |
| MM | Multiple Myeloma |
| MMP2 | Matrix metalloproteinase-2 |
| MMP9 | Matrix metalloproteinase-9 |
| mTOR | Mammalian target of rapamycin |
| NCV | Nerve conduction velocity |
| NfkB | Nuclear factor kappa B |
| PI | Proteasome inhibitor |
| PIs | Proteasome inhibitors |
| QoL | Quality of life |
| RANKL | Receptor activator of nuclear factor kappa-Β ligand |
| RCT | Randomized-controlled trial |
| ROS | Reactive oxygen species |
| SIO | Society for Integrative Oncology |
| STAT3 | Signal transducer and activator of transcription 3 |
| THC | Delta-trans-9-tetrahydrocannabinol |
| TNFα | Tumor necrosis factor-α |
| TP53 | Tumor protein p53 |
| VEGF | Vascular endothelium growth factor |
| VDR | Vitamin D receptor |
References
- Palumbo, A.; Anderson, K. Multiple Myeloma. N. Engl. J. Med. 2011, 364, 1046–1060. [Google Scholar] [CrossRef]
- Cowan, A.J.; Green, D.J.; Kwok, M.; Lee, S.; Coffey, D.G.; Holmberg, L.A.; Tuazon, S.; Gopal, A.K.; Libby, E.N. Diagnosis and Management of Multiple Myeloma: A Review. JAMA 2022, 327, 464–477. [Google Scholar] [CrossRef] [PubMed]
- Bird, S.A.; Boyd, K. Multiple Myeloma: An Overview of Management. Palliat. Care Soc. Pract. 2019, 13, 1178224219868235. [Google Scholar] [CrossRef] [PubMed]
- Kvam, A.K.; Waage, A. Health-Related Quality of Life in Patients with Multiple Myeloma-Does It Matter? Haematologica 2015, 100, 704–705. [Google Scholar] [CrossRef] [PubMed]
- Zaleta, A.K.; Miller, M.F.; Olson, J.S.; Yuen, E.Y.N.; LeBlanc, T.W.; Cole, C.E.; McManus, S.; Buzaglo, J.S. Symptom Burden, Perceived Control, and Quality of Life among Patients Living with Multiple Myeloma. JNCCN J. Natl. Compr. Cancer Netw. 2020, 18, 1087–1095. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, E.K.; Shapiro, Y.N.; Yee, A.J.; Nadeem, O.; Hu, B.Y.; Laubach, J.P.; Branagan, A.R.; Anderson, K.C.; Mo, C.C.; Munshi, N.C.; et al. Quality of Life, Psychological Distress, and Prognostic Perceptions in Patients with Multiple Myeloma. Cancer 2022, 128, 1996–2004. [Google Scholar] [CrossRef] [PubMed]
- Osborne, T.R.; Ramsenthaler, C.; de Wolf-Linder, S.; Schey, S.A.; Siegert, R.J.; Edmonds, P.M.; Higginson, I.J. Understanding What Matters Most to People with Multiple Myeloma: A Qualitative Study of Views on Quality of Life. BMC Cancer 2014, 14, 496. [Google Scholar] [CrossRef]
- Cenzer, I.; Berger, K.; Rodriguez, A.M.; Ostermann, H.; Covinsky, K.E. Patient-Reported Measures of Well-Being in Older Multiple Myeloma Patients: Use of Secondary Data Source. Aging Clin. Exp. Res. 2020, 32, 1153–1160. [Google Scholar] [CrossRef]
- Shapiro, Y.N.; Peppercorn, J.M.; Yee, A.J.; Branagan, A.R.; Raje, N.S.; Donnell, E.K.O. Lifestyle Considerations in Multiple Myeloma. Blood Cancer J. 2021, 11, 172. [Google Scholar] [CrossRef]
- Bonucci, M.; Andreazzoli, F. New approach of Integration: Integrative Hematology. Br. J. Res. 2017, 4, 6. [Google Scholar]
- Witt, C.M.; Balneaves, L.G.; Cardoso, M.J.; Cohen, L.; Greenlee, H.; Johnstone, P.; Kucuk, O.; Mailman, J.; Mao, J.J. A Comprehensive Definition for Integrative Oncology. J. Natl. Cancer Inst. Monogr. 2017, 2017, lgx012. [Google Scholar] [CrossRef] [PubMed]
- Okolo, O.; Wertheim, B.C.; Larsen, A.; Sweeney, N.W.; Ahlstrom, J.M.; Gowin, K. Integrative Medicine in Multiple Myeloma and Plasma Cell Disorders. Complement. Ther. Med. 2023, 73, 102939. [Google Scholar] [CrossRef] [PubMed]
- Roydhouse, J.K.; Bhatnagar, V.; Berman, T.; Menapace, L.A.; Agarwal, R.; Fiero, M.H.; Kluetz, P. Botanical Product Use Among Multiple Myeloma Patients in Commercial Drug Trials. Blood 2019, 134 (Suppl. S1), 4769. [Google Scholar] [CrossRef]
- Jogdand, R.P.; Singh, A.; Khumbhare, U.; Parameshwar; Nagaratna, R. Impact of Integrative Therapy in Remission of Multiple Myloma: A Case Study. Integr. Med. Case Rep. 2022, 3, 25. [Google Scholar] [CrossRef]
- Korde, N.; Tavitian, E.; Mastey, D.; Lengfellner, J.; Hevroni, G.; Zarski, A.; Salcedo, M.; Mailankody, S.; Hassoun, H.; Smith, E.L.; et al. Association of Patient Activity Bio-Profiles with Health-Related Quality of Life in Patients with Newly Diagnosed Multiple Myeloma: A Prospective Observational Cohort Study. Lancet 2023, 57, 101854. [Google Scholar] [CrossRef]
- Yu, C.C.; Li, Y.; Cheng, Z.J.; Wang, X.; Mao, W.; Zhang, Y.W. Active Components of Traditional Chinese Medicinal Material for Multiple Myeloma: Current Evidence and Future Directions. Front. Pharmacol. 2022, 13, 818179. [Google Scholar] [CrossRef]
- Shah, U.A.; Parikh, R.; Castro, F.; Bellone, M.; Lesokhin, A.M. Dietary and microbiome evidence in multiple myeloma and other plasma cell disorders. Leukemia 2023, 37, 964–980. [Google Scholar] [CrossRef]
- Malik, M.A.; Sweeney, N.W.; Jafri, M.; Derkach, A.; Chmielewski, C.; Adintori, P.A.; Mailankody, S.; Korde, N.; Tan, C.R.; Hassoun, H.; et al. Nutrition perceptions, needs and practices among patients with plasma cell disorders. Blood Cancer J. 2022, 12, 70. [Google Scholar] [CrossRef]
- Key, T.J.; Appleby, P.N.; Crowe, F.L.; Bradbury, K.E.; Schmidt, J.A.; Travis, R.C. Cancer in British vegetarians: Updated analyses of 4998 incident cancers in a cohort of 32,491 meat eaters, 8612 fish eaters, 18,298 vegetarians, and 2246 vegans. Am. J. Clin. Nutr. 2014, 100, 378s–385s. [Google Scholar] [CrossRef]
- Brown, L.M.; Gridley, G.; Pottern, L.M.; Baris, D.; Swanson, C.A.; Silverman, D.T.; Hayes, R.B.; Greenberg, R.S.; Swanson, G.M.; Schoenberg, J.B.; et al. Diet and nutrition as risk factors for multiple myeloma among blacks and whites in the United States. Cancer Causes Control CCC 2001, 12, 117–125. [Google Scholar] [CrossRef]
- Fritschi, L.; Ambrosini, G.L.; Kliewer, E.V.; Johnson, K.C. Dietary fish intake and risk of leukaemia, multiple myeloma, and non-Hodgkin lymphoma. Cancer epidemiology, biomarkers & prevention: A publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive. Oncology 2004, 13, 532–537. [Google Scholar]
- Wang, Y.Z.; Wu, Q.J.; Zhu, J.; Wu, L. Fish consumption and risk of myeloma: A meta-analysis of epidemiological studies. Cancer Causes Control CCC 2015, 26, 1307–1314. [Google Scholar] [CrossRef]
- Parolini, C. Effects of Fish n-3 PUFAs on Intestinal Microbiota and Immune System. Mar. Drugs 2019, 17, 374. [Google Scholar] [CrossRef] [PubMed]
- Vlajinac, H.D.; Pekmezović, T.D.; Adanja, B.J.; Marinković, J.M.; Kanazir, M.S.; Suvajdzić, N.D.; Colović, M.D. Case-control study of multiple myeloma with special reference to diet as risk factor. Neoplasma 2003, 50, 79–83. [Google Scholar]
- Thordardottir, M.; Lindqvist, E.K.; Lund, S.H.; Costello, R.; Burton, D.; Steingrimsdottir, L.; Korde, N.; Mailankody, S.; Eiriksdottir, G.; Launer, L.J.; et al. Dietary intake is associated with risk of multiple myeloma and its precursor disease. PLoS ONE 2018, 13, e0206047. [Google Scholar] [CrossRef] [PubMed]
- Hosgood, H.D., 3rd; Baris, D.; Zahm, S.H.; Zheng, T.; Cross, A.J. Diet and risk of multiple myeloma in Connecticut women. Cancer Causes Control CCC 2007, 18, 1065–1076. [Google Scholar] [CrossRef]
- Bieghs, L.; Johnsen, H.E.; Maes, K.; Menu, E.; Van Valckenborgh, E.; Overgaard, M.T.; Nyegaard, M.; Conover, C.A.; Vanderkerken, K.; De Bruyne, E. The insulin-like growth factor system in multiple myeloma: Diagnostic and therapeutic potential. Oncotarget 2016, 7, 48732–48752. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Fung, T.T.; Tabung, F.K.; Marinac, C.R.; Devore, E.E.; Rosner, B.A.; Ghobrial, I.M.; Colditz, G.A.; Giovannucci, E.L.; Birmann, B.M. Prediagnosis dietary pattern and survival in patients with multiple myeloma. Int. J. Cancer 2020, 147, 1823–1830. [Google Scholar] [CrossRef]
- Santo, L.; Liao, L.M.; Andreotti, G.; Purdue, M.P.; Hofmann, J.N. Alcohol consumption and risk of multiple myeloma in the NIH-AARP Diet and Health Study. Int. J. Cancer 2019, 144, 43–48. [Google Scholar] [CrossRef]
- Díaz, L.E.; Montero, A.; González-Gross, M.; Vallejo, A.I.; Romeo, J.; Marcos, A. Influence of alcohol consumption on immunological status: A review. Eur. J. Clin. Nutr. 2002, 56, S50–S53. [Google Scholar] [CrossRef]
- Marques-Mourlet, C.; Di Iorio, R.; Fairfield, H.; Reagan, M.R. Obesity and myeloma: Clinical and mechanistic contributions to disease progression. Front. Endocrinol. 2023, 14, 1118691. [Google Scholar] [CrossRef]
- Takeoka, Y.; Sakatoku, K.; Miura, A.; Yamamura, R.; Araki, T.; Seura, H.; Okamura, T.; Koh, H.; Nakamae, H.; Hino, M.; et al. Prognostic Effect of Low Subcutaneous Adipose Tissue on Survival Outcome in Patients with Multiple Myeloma. Clin. Lymphoma Myeloma Leuk. 2016, 16, 434–441. [Google Scholar] [CrossRef]
- Kamiya, T.; Ito, C.; Fujita, Y.; Ogura, S.; Mizuno, K.; Sakurai, A.; Aisa, Y.; Nakazato, T. The prognostic value of the controlling nutritional status score in patients with multiple myeloma. Leuk. Lymphoma 2020, 61, 1894–1900. [Google Scholar] [CrossRef] [PubMed]
- Capitão, C.; Coutinho, D.; Neves, P.M.; Capelas, M.L.; Pimenta, N.M.; Santos, T.; Mäkitie, A.; Ravasco, P. Protein intake and muscle mass maintenance in patients with cancer types with high prevalence of sarcopenia: A systematic review. Support. Care Cancer 2022, 30, 3007–3015. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Gu, J.; Liu, J.; Huang, B.; Li, J. Fecal microbiota taxonomic shifts in Chinese multiple myeloma patients analyzed by quantitative polimerase chain reaction (QPCR) and 16S rRNA high-throughput sequencing. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 8269–8280. [Google Scholar] [CrossRef] [PubMed]
- Antoine Pepeljugoski, C.; Morgan, G.; Braunstein, M. Analysis of intestinal microbiome in multiple myeloma reveals progressive dysbiosis compared to MGUS and healthy individuals. Blood 2019, 134, 3076. [Google Scholar] [CrossRef]
- Available online: https://clinicaltrials.gov/study/NCT05712967 (accessed on 30 November 2023).
- Jian, X.; Zhu, Y.; Ouyang, J.; Wang, Y.; Lei, Q.; Xia, J.; Guan, Y.; Zhang, J.; Guo, J.; He, Y.; et al. Alterations of gut microbiome accelerate multiple myeloma progression by increasing the relative abundances of nitrogen-recycling bacteria. Microbiome 2020, 8, 74. [Google Scholar] [CrossRef]
- Pianko, M.J.; Devlin, S.M.; Littmann, E.R.; Chansakul, A.; Mastey, D.; Salcedo, M.; Fontana, E.; Ling, L.; Tavitian, E.; Slingerland, J.B.; et al. Minimal residual disease negativity in multiple myeloma is associated with intestinal microbiota composition. Blood Adv. 2019, 3, 2040–2044. [Google Scholar] [CrossRef]
- Shah, U.A.; Maclachlan, K.H.; Derkach, A.; Salcedo, M.; Barnett, K.; Caple, J.; Blaslov, J.; Tran, L.; Ciardiello, A.; Burge, M.; et al. Sustained minimal residual disease negativity in multiple myeloma is associated with stool butyrate and healthier plant-based diets. Clin. Cancer Res. 2022, 28, 5149–5155. [Google Scholar] [CrossRef]
- Zhu, G.; Jin, L.; Shen, W.; Zhao, M.; Liu, N. Intratumor microbiota: Occult participants in the microenvironment of multiple myeloma. Biochim. Biophys. Acta Rev. Cancer 2023, 1878, 188959. [Google Scholar] [CrossRef]
- Available online: https://clinicaltrials.gov/study/NCT05640843 (accessed on 30 November 2023).
- Zoi, V.; Galani, V.; Lianos, G.D.; Voulgaris, S.; Kyritsis, A.P.; Alexiou, G.A. The Role of Curcumin in Cancer Treatment. Biomedicines 2021, 9, 1086. [Google Scholar] [CrossRef] [PubMed]
- Bai, Q.X.; Zhang, X.Y. Curcumin enhances cytotoxic effects of bortezomib in human multiple myeloma H929 cells: Potential roles of NF-κB/JNK. Int. J. Mol. Sci. 2012, 13, 4831–4838. [Google Scholar] [CrossRef] [PubMed]
- Allegra, A.; Speciale, A.; Molonia, M.S.; Guglielmo, L.; Musolino, C.; Ferlazzo, G.; Costa, G.; Saija, A.; Cimino, F. Curcumin ameliorates the in vitro efficacy of carfilzomib in human multiple myeloma U266 cells targeting p53 and NF-kappaB pathways. Toxicol. Vitr. 2018, 47, 186–194. [Google Scholar] [CrossRef]
- Gomez-Bougie, P.; Halliez, M.; Maïga, S.; Godon, C.; Kervoëlen, C.; Pellat-Deceunynck, C.; Moreau, P.; Amiot, M. Curcumin induces cell death of the main molecular myeloma subtypes, particularly the poor prognosis subgroups. Cancer Biol. Ther. 2015, 16, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Bharti, A.C.; Donato, N.; Aggarwal, B.B. Curcumin (diferuloylmethane) inhibits constitutive and IL-6-inducible STAT3 phosphorylation in human myeloma cells. J. Immunol. 2003, 171, 3863–3871. [Google Scholar] [CrossRef] [PubMed]
- Bashang, H.; Tamma, S. The use of curcumin as an effective adjuvant to cancer therapy: A short review. Biotechnol. Appl. Biochem. 2020, 67, 171–179. [Google Scholar] [CrossRef]
- Mekkawy, S.A.; Abdalla, M.S.; Omran, M.M.; Hassan, N.M.; Abdelfattah, R.; Abdel-Salam, I.M. Cancer Stem Cells as a Prognostic Biomarker and Therapeutic Target Using Curcumin/Piperine Extract for Multiple Myeloma. Asian Pac. J. Cancer Prev. APJCP 2022, 23, 3507–3515. [Google Scholar] [CrossRef]
- Chen, J.; Ying, Y.; Zhu, H.; Zhu, T.; Qu, C.; Jiang, J.; Fang, B. Curcumin-induced promoter hypermethylation of the mammalian target of rapamycin gene in multiple myeloma cells. Oncol. Lett. 2019, 17, 1108–1114. [Google Scholar] [CrossRef]
- Sung, B.; Kunnumakkara, A.B.; Sethi, G.; Anand, P.; Guha, S.; Aggarwal, B.B. Curcumin circumvents chemoresistance in vitro and potentiates the effect of thalidomide and bortezomib against human multiple myeloma in nude mice model. Mol. Cancer Ther. 2009, 8, 959–970. [Google Scholar] [CrossRef]
- Golombick, T.; Diamond, T.H.; Badmaev, V.; Manoharan, A.; Ramakrishna, R. The potential role of curcumin in patients with monoclonal gammopathy of undefined significance—Its effect on paraproteinemia and the urinary N-telopeptide of type I collagen bone turnover marker. Clin. Cancer Res. 2009, 15, 5917–5922. [Google Scholar] [CrossRef]
- Golombick, T.; Diamond, T.H.; Manoharan, A.; Ramakrishna, R. Monoclonal gammopathy of undetermined significance, smoldering multiple myeloma, and curcumin: A randomized, double-blind placebo-controlled cross-over 4g study and an open-label 8g extension study. Am. J. Hematol. 2012, 87, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, A.; Lai, M.; Cavenagh, J. Long-term stabilisation of myeloma with curcumin Case Reports. BMJ Case Rep. 2017, 2017, bcr2016218148. [Google Scholar] [CrossRef]
- Ramakrishna, R.; Diamond, T.H.; Alexander, W.; Manoharan, A.; Golombick, T. Use of Curcumin in Multiple Myeloma patients intolerant of steroid therapy. Clin. Case Rep. 2020, 8, 739–744. [Google Scholar] [CrossRef]
- Santosa, D.; Suharti, C.; Riwanto, I.; Dharmana, E.; Pangarsa, E.A.; Setiawan, B.; Suyono, S.; Tobing, M.L.; Suhartono, S.; Hadisapurto, S. Curcumin as adjuvant therapy to improve remission in myeloma patients: A pilot randomized clinical trial. Casp. J. Intern. Med. 2022, 13, 375–384. [Google Scholar]
- Shammas, M.A.; Neri, P.; Koley, H.; Batchu, R.B.; Bertheau, R.C.; Munshi, V.; Prabhala, R.; Fulciniti, M.; Tai, Y.T.; Treon, S.P.; et al. Specific killing of multiple myeloma cells by (−)-epigallocatechin-3-gallate extracted from green tea: Biologic activity and therapeutic implications. Blood 2006, 108, 2804–2810. [Google Scholar] [CrossRef]
- Zhou, C.G.; Hui, L.M.; Luo, J.M. Epigallocatechin gallate inhibits the proliferation and induces apoptosis of multiple myeloma cells via inactivating EZH2. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 2093–2098. [Google Scholar] [PubMed]
- Golden, E.B.; Lam, P.Y.; Kardosh, A.; Gaffney, K.J.; Cadenas, E.; Louie, S.G.; Petasis, N.A.; Chen, T.C.; Schönthal, A.H. Green tea polyphenols block the anticancer effects of bortezomib and other boronic acid-based proteasome inhibitors. Blood 2009, 113, 5927–5937. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Li, J.; Gu, J.; Huang, B.; Zhao, Y.; Zheng, D.; Ding, Y.; Zeng, L. Potentiation of (−)-epigallocatechin-3-gallate-induced apoptosis by bortezomib in multiple myeloma cells. Acta Biochim. Biophys. Sin. 2009, 41, 1018–1026. [Google Scholar] [CrossRef]
- Modernelli, A.; Naponelli, V.; Troglio, M.G.; Bonacini, M.; Ramazzina, I.; Bettuzzi, S.; Rizzi, F. EGCG antagonizes Bortezomib cytotoxicity in prostate cancer cells by an autophagic mechanism. Sci. Rep. 2015, 5, 15270. [Google Scholar] [CrossRef]
- Qiu, X.; Wu, X.; He, W. (−)-Epigallocatechin-3-gallate plays an antagonistic role in the antitumor effect of bortezomib in myeloma cells via activating Wnt/β-catenin signaling pathway. Adv. Clin. Exp. Med. 2022, 31, 789–794. [Google Scholar] [CrossRef]
- Li, C.; Feng, Y.; Wang, W.; Xu, L.; Zhang, M.; Yao, Y.; Wu, X.; Zhang, Q.; Huang, W.; Wang, X.; et al. Targeting Glutaminolysis to Treat Multiple Myeloma: An In Vitro Evaluation of Glutaminase Inhibitors Telaglenastat and Epigallocatechin-3-gallate. Anti-cancer Agents Med. Chem. 2023, 23, 779–785. [Google Scholar]
- Maier, G.S.; Horas, K.; Kurth, A.A.; Lazovic, D.; Seeger, J.B.; Maus, U. Prevalence of Vitamin D Deficiency in Patients with Bone Metastases and Multiple Myeloma. Anticancer Res. 2015, 35, 6281–6285. [Google Scholar] [PubMed]
- Rui, H.; Liu, Y.; Lin, M.; Zheng, X. Vitamin D receptor gene polymorphism is associated with multiple myeloma. J. Cell. Biochem. 2020, 121, 224–230. [Google Scholar] [CrossRef]
- Ng, A.C.; Kumar, S.K.; Rajkumar, S.V.; Drake, M.T. Impact of vitamin D deficiency on the clinical presentation and prognosis of patients with newly diagnosed multiple myeloma. Am. J. Hematol. 2009, 84, 397–400. [Google Scholar] [CrossRef]
- Wang, J.; Udd, K.A.; Vidisheva, A.; Swift, R.A.; Spektor, T.M.; Bravin, E.; Ibrahim, E.; Treisman, J.; Masri, M.; Berenson, J.R. Low serum vitamin D occurs commonly among multiple myeloma patients treated with bortezomib and/or thalidomide and isassociated with severe neuropathy. Support. Care Cancer 2016, 24, 3105–3110. [Google Scholar] [PubMed]
- Raoufinejad, K.; Shamshiri, A.R.; Pezeshki, S.; Chahardouli, B.; Hadjibabaie, M.; Jahangard-Rafsanjani, Z.; Gholami, K.; Rajabi, M.; Vaezi, M. Oral calcitriol in hematopoietic recovery and survival after autologous stem cell transplantation: A randomized clinical trial. DARU 2009, 27, 709–720. [Google Scholar] [CrossRef]
- Flamann, C.; Busch, L.; Mackensen, A.; Bruns, H. Combination of lenalidomide and vitamin D enhances MOR202-mediated cytotoxicity of macrophages: It takes three to tango. Oncotarget 2019, 10, 10–12. [Google Scholar] [CrossRef]
- Mirhosseini, N.; Psihogios, A.; McLaren, M.D.; Seely, D. Vitamin D and Multiple Myeloma: A Scoping Review. Curr. Oncol. 2023, 30, 3263–3276. [Google Scholar] [CrossRef]
- Perrone, G.; Hideshima, T.; Ikeda, H.; Okawa, Y.; Calabrese, E.; Gorgun, G.; Santo, L.; Cirstea, D.; Raje, N.; Chauhan, D.; et al. Ascorbic acid inhibits antitumor activity of bortezomib in vivo. Leukemia 2009, 23, 1679–1686. [Google Scholar] [CrossRef]
- Nakano, A.; Abe, M.; Oda, A.; Amou, H.; Hiasa, M.; Nakamura, S.; Miki, H.; Harada, T.; Fujii, S.; Kagawa, K.; et al. Delayed treatment with vitamin C and N-acetyl-l-cysteine protects Schwann cells without compromising the anti-myeloma activity of bortezomib. Int. J. Hematol. 2011, 93, 727–735. [Google Scholar] [CrossRef]
- Van Gorkom, G.N.Y.; Boerenkamp, L.S.; Gijsbers, B.L.M.G.; van Ojik, H.H.; Wodzig, W.K.W.H.; Wieten, L.; Van Elssen, C.H.M.J.; Bos, G.M.J. No Effect of Vitamin C Administration on Neutrophil Recovery in Autologous Stem Cell Transplantation for Myeloma or Lymphoma: A Blinded, Randomized Placebo-Controlled Trial. Nutrients 2022, 14, 4784. [Google Scholar] [CrossRef] [PubMed]
- Jakubikova, J.; Cervi, D.; Ooi, M.; Kim, K.; Nahar, S.; Klippel, S.; Cholujova, D.; Leiba, M.; Daley, J.F.; Delmore, J.; et al. Anti-tumor activity and signaling events triggered by the isothiocyanates, sulforaphane and phenethyl isothiocyanate, in multiple myeloma. Haematologica 2011, 96, 1170–1179. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, A.; Sethi, G.; Vadhan-Raj, S.; Bueso-Ramos, C.; Takada, Y.; Gaur, U.; Nair, A.S.; Shishodia, S.; Aggarwal, B.B. Resveratrol inhibits proliferation, induces apoptosis, and overcomes chemoresistance through down-regulation of STAT3 and nuclear factor-kappaB-regulated antiapoptotic and cell survival gene products in human multiple myeloma cells. Blood 2007, 109, 2293–2302. [Google Scholar] [CrossRef]
- Popat, R.; Plesner, T.; Davies, F.; Cook, G.; Cook, M.; Elliott, P.; Jacobson, E.; Gumbleton, T.; Oakervee, H.; Cavenagh, J. A phase 2 study of SRT501 (resveratrol) with bortezomib for patients with relapsed and or refractory multiple myeloma. Br. J. Haematol. 2013, 160, 714–717. [Google Scholar] [CrossRef] [PubMed]
- Bilbao, A.; Spanagel, R. Medical cannabinoids: A pharmacology-based systematic review and meta-analysis for all relevant medical indications. BMC Med. 2022, 20, 259. [Google Scholar] [CrossRef]
- Dariš, B.; Tancer Verboten, M.; Knez, Ž.; Ferk, P. Cannabinoids in cancer treatment: Therapeutic potential and legislation. Bosn. J. Basic Med. Sci. 2019, 19, 14–23. [Google Scholar] [CrossRef]
- Nabissi, M.; Morelli, M.B.; Offidani, M.; Amantini, C.; Gentili, S.; Soriani, A.; Cardinali, C.; Leoni, P.; Santoni, G. Cannabinoids synergize with carfilzomib, reducing multiple myeloma cells viability and migration. Oncotarget 2016, 7, 77543–77557. [Google Scholar] [CrossRef]
- Coluzzi, F.; Rolke, R.; Mercadante, S. Pain Management in Patients with Multiple Myeloma: An Update. Cancers 2019, 11, 2037. [Google Scholar] [CrossRef]
- Lu, W.; Rosenthal, D.S. Oncology Acupuncture for Chronic Pain in Cancer Survivors: A Reflection on the American Society of Clinical Oncology Chronic Pain Guideline. Hematol. Oncol. Clin. N. Am. 2018, 32, 519–533. [Google Scholar] [CrossRef]
- Ling, F.; Qi, W.; Li, X.; Zhou, J.; Xiong, J.; Zhao, Y.; Zheng, Q.; Liang, F. Bibliometric Analysis of Acupuncture Therapy for Cancer Pain Over the Past 10 Years. J. Pain Res. 2023, 16, 985–1003. [Google Scholar] [CrossRef]
- Huang, L.; Zhao, Y.; Xiang, M. Knowledge Mapping of Acupuncture for Cancer Pain: A Scientometric Analysis (2000–2019). J. Pain Res. 2021, 14, 343–358. [Google Scholar] [CrossRef] [PubMed]
- Kutcher, A.M.; LeBaron, V.T. Evaluating Acupuncture for the Treatment of Chemotherapy-Induced Peripheral Neuropathy: An Integrative Review. West. J. Nurs. Res. 2022, 44, 169–179. [Google Scholar] [CrossRef]
- Ben-Arye, E.; Hausner, D.; Samuels, N.; Gamus, D.; Lavie, O.; Tadmor, T.; Gressel, O.; Agbarya, A.; Attias, S.; David, A.; et al. Impact of Acupuncture and Integrative Therapies on Chemotherapy-Induced Peripheral Neuropathy: A Multicentered, Randomized Controlled Trial. Cancer 2022, 128, 3641–3652. [Google Scholar] [CrossRef] [PubMed]
- Richardson, P.G.; Briemberg, H.; Jagannath, S.; Wen, P.Y.; Barlogie, B.; Berenson, J.; Singhal, S.; Siegel, D.S.; Irwin, D.; Schuster, M.; et al. Frequency, Characteristics, and Reversibility of Peripheral Neuropathy during Treatment of Advanced Multiple Myeloma with Bortezomib. J. Clin. Oncol. 2006, 24, 3113–3120. [Google Scholar] [CrossRef] [PubMed]
- Mandiroǧlu, S.; Cevik, C.; Ayli, M. Acupuncture for Neuropathic Pain Due to Bortezomib in a Patient with Multiple Myeloma. Acupunct. Med. 2014, 32, 194–196. [Google Scholar] [CrossRef]
- Bao, T.; Lao, L.; Medeiros, M.; Zhang, R.; Dorsey, S.G.; Badros, A. Improvement of Painful Bortezomib-Induced Peripheral Neuropathy Following Acupuncture Treatment in a Case Series of Multiple Myeloma Patients. Med. Acupunct. 2012, 24, 181–187. [Google Scholar] [CrossRef]
- Bao, T.; Goloubeva, O.; Pelser, C.; Porter, N.; Primrose, J.; Hester, L.; Sadowska, M.; Lapidus, R.; Medeiros, M.; Lao, L.; et al. A Pilot Study of Acupuncture in Treating Bortezomib-Induced Peripheral Neuropathy in Patients with Multiple Myeloma. Integr. Cancer Ther. 2014, 13, 396–404. [Google Scholar] [CrossRef]
- Zhi, W.I.; Ingram, E.; Li, S.Q.; Chen, P.; Piulson, L.; Bao, T. Acupuncture for Bortezomib-Induced Peripheral Neuropathy: Not Just for Pain. Integr. Cancer Ther. 2018, 17, 1079–1086. [Google Scholar] [CrossRef]
- Garcia, M.K.; Cohen, L.; Guo, Y.; Zhou, Y.; You, B.; Chiang, J.; Orlowski, R.Z.; Weber, D.; Shah, J.; Alexanian, R.; et al. Electroacupuncture for Thalidomide/Bortezomib-Induced Peripheral Neuropathy in Multiple Myeloma: A Feasibility Study. J. Hematol. Oncol. 2014, 7, 41. [Google Scholar] [CrossRef]
- Wang, L.; Xu, X.; Yao, L.; Huang, Y.; Zou, Q.; Wu, B.; Yin, D. Intervention Effect of Acupuncture and Moxibustion in Treatment of Chemotherapy-Induced Peripheral Neuropathy in Patients with Multiple Myeloma. J. Clin. Med. Pract. 2022, 26, 28–30. [Google Scholar]
- Han, X.; Wang, L.; Shi, H.; Zheng, G.; He, J.; Wu, W.; Shi, J.; Wei, G.; Zheng, W.; Sun, J.; et al. Acupuncture Combined with Methylcobalamin for the Treatment of Chemotherapy-Induced Peripheral Neuropathy in Patients with Multiple Myeloma. BMC Cancer 2017, 17, 40. [Google Scholar] [CrossRef] [PubMed]
- Deng, G.; Giralt, S.; Chung, D.J.; Landau, H.; Siman, J.; Search, B.; Coleton, M.; Vertosick, E.; Shapiro, N.; Chien, C.; et al. Acupuncture for Reduction of Symptom Burden in Multiple Myeloma Patients Undergoing Autologous Hematopoietic Stem Cell Transplantation: A Randomized Sham-Controlled Trial. Support. Care Cancer 2018, 26, 657–665. [Google Scholar] [CrossRef]
- Deng, G. Acupuncture as a Potential Opioid-Sparing Pain Management Intervention for Patients Undergoing Cancer Treatment. Med. Acupunct. 2020, 32, 394–395. [Google Scholar] [CrossRef]
- El Iskandarani, S.; Sun, L.; Li, S.Q.; Pereira, G.; Giralt, S.; Deng, G. Acupuncture Improves Certain Aspects of Sleep in Hematopoietic Stem Cell Transplantation Patients: A Secondary Analysis of a Randomized Controlled Trial. Acupunct. Med. 2023, 41, 319–326. [Google Scholar] [CrossRef]
- Deng, G.; Giralt, S.; Chung, D.J.; Landau, H.; Siman, J.; Li, Q.S.; Lapen, K.; Mao, J.J. Reduction of Opioid Use by Acupuncture in Patients Undergoing Hematopoietic Stem Cell Transplantation: Secondary Analysis of a Randomized, Sham-Controlled Trial. Pain Med. 2020, 21, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Jiang, C. Effects of Heat-Sensitive Moxibustion plus Chinese Medication on the Expression of Serum Inflammatory Indicators and MicroRNAs in Patients with Multiple Myeloma after Chemotherapy. J. Acupunct. Tuina Sci. 2023, 21, 51–58. [Google Scholar] [CrossRef]
- Ke, M.; Qian, J.; Hao, F.; Li, X.; Wu, H.; Luo, X.; Xu, B.; Gu, C.; Yang, Y. Acupuncture Synergized with Bortezomib Improves Survival of Multiple Myeloma Mice via Decreasing Metabolic Ornithine. Front. Oncol. 2021, 11, 779562. [Google Scholar] [CrossRef]
- Lyu, J.; Wang, S.; Zhang, H.; Liu, S. Acupuncture-Exacerbated Pyoderma Gangrenosum Associated with IgG Multiple Myeloma. Wounds 2022, 34, e108–e111. [Google Scholar] [CrossRef]
- Kayo, T.; Suzuki, M.; Mitsuma, T.; Suzuki, M.; Ikeda, S.; Sukegawa, M.; Tsunoda, S.; Ohta, M. Bleeding Risk of Acupuncture for Patients with Hematological Malignancies Accompanying Thrombocytopenia: A Retrospective Chart Review. J. Integr. Complement. Med. 2023. ahead of print. [Google Scholar] [CrossRef]
- Mao, J.J.; Ismaila, N.; Bao, T.; Barton, D.; Ben-Arye, E.; Garland, E.L.; Greenlee, H.; Leblanc, T.; Lee, R.T.; Lopez, A.M.; et al. Integrative Medicine for Pain Management in Oncology: Society for Integrative Oncology-ASCO Guideline. J. Clin. Oncol. 2022, 40, 3998–4024. [Google Scholar] [CrossRef]
- Carlson, L.E.; Ismaila, N.; Addington, E.L.; Asher, G.N.; Atreya, C.; Balneaves, L.G.; Bradt, J.; Fuller-Shavel, N.; Goodman, J.; Hoffman, C.J.; et al. Integrative Oncology Care of Symptoms of Anxiety and Depression in Adults with Cancer: Society for Integrative Oncology-ASCO Guideline. J. Clin. Oncol. 2023, 41, 4562–4591. [Google Scholar] [CrossRef]
- Lamers, J.; Hartmann, M.; Goldschmidt, H.; Brechtel, A.; Hillengass, J.; Herzog, W. Psychosocial support in patients with multiple myeloma at time of diagnosis: Who wants what? Psychooncology 2013, 22, 2313–2320. [Google Scholar] [CrossRef] [PubMed]
- Pulgar, Á.; Garrido, S.; Alcalá, A.; Reyes del Paso, G.A. Psychosocial predictors of immune response following bone marrow transplantation. Behav. Med. 2012, 38, 12–18. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, M.R.; LeBlanc, T.W.; Yang, Q.; McLaughlin, J.; Irish, K.; Smith, S.K. A Mobile App to Support Self-Management in Patients with Multiple Myeloma or Chronic Lymphocytic Leukemia: Pilot Randomized Controlled Trial. JMIR Cancer 2023, 9, e44533. [Google Scholar] [CrossRef] [PubMed]
- Ng, D.L.; Gan, G.G.; Anuar, N.A.; Tung, Y.Z.; Lai, N.Z.; Tan, Y.W.; Said, S.N.M.; Madihie, A.; Chai, C.S.; Tan, S.B. The effect of a single session of 30-min mindful breathing in reducing fatigue among patients with haematological cancer—A randomised controlled trial. BMC Palliat. Care 2021, 20, 160. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.; Bolwell, B.; Majhail, N.S.; Rybicki, L.; Yurch, M.; Abounader, D.; Kohuth, J.; Jarancik, S.; Koniarczyk, H.; McLellan, L.; et al. Music Therapy for Symptom Management After Autologous Stem Cell Transplantation: Results from a Randomized Study. Biol. Blood Marrow Transplant. 2017, 23, 1567–1572. [Google Scholar] [CrossRef]
- Saha, V.; Mallik, K.C. Psycho-socio-spiritual care in multiple myeloma: Are we lagging behind? Indian J. Cancer 2022, 59, 128–131. [Google Scholar]
- Sherman, A.C.; Plante, T.G.; Simonton, S.; Latif, U.; Anaissie, E.J. Prospective study of religious coping among patients undergoing autologous stem cell transplantation. J. Behav. Med. 2009, 32, 118–128. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).