The Use of Honey for Cicatrization and Pain Control of Obstetric Wounds: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol
2.2. Eligibility Criteria
2.3. Search Strategy and Data Extraction
2.4. Endpoints and Subgroup Analyses
2.5. Quality Assessment
2.6. Statistical Analysis
3. Results
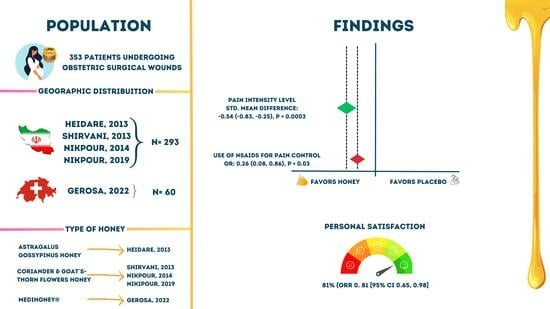
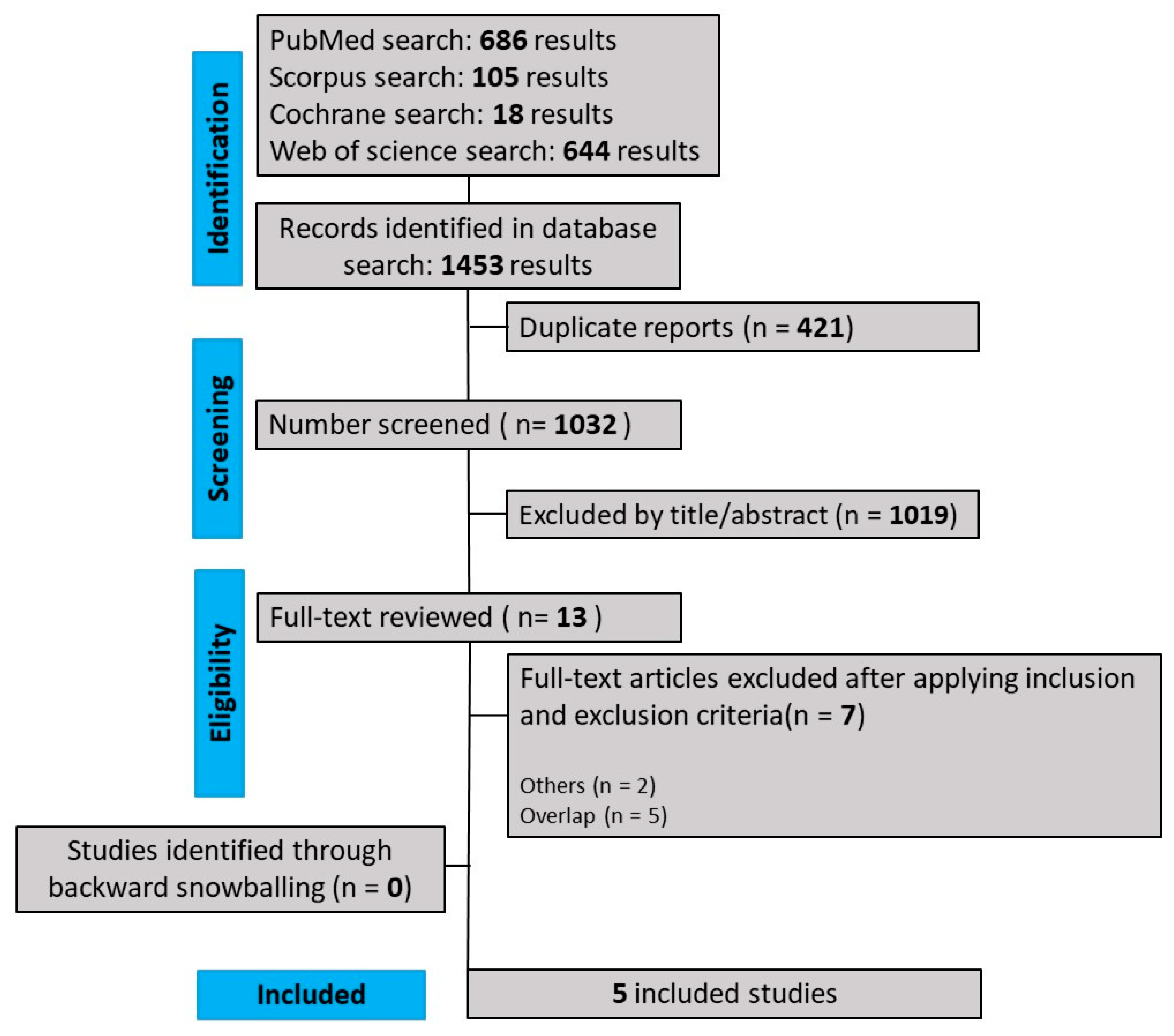
3.1. Selection and Characteristics
3.2. Demographic and Clinical Data
3.3. Combined Analysis of Results and Subgroup Analysis
3.3.1. Wound Healing
3.3.2. Pain Intensity Level
3.4. Secondary Outcomes
3.5. Quality Assessment
3.6. Sensitivity Analysis
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Gerosa, D.; Santagata, M.; Martinez de Tejada, B.; Guittier, M.-J. Application of Honey to Reduce Perineal Laceration Pain during the Postpartum Period: A Randomized Controlled Trial. Healthcare 2022, 10, 1515. [Google Scholar] [CrossRef] [PubMed]
- Mardani, F.; Hadizadeh- Talasaz, F.; Bahri, N. Effect of Medicinal Plants on Episiotomy Wound Healing In Iran: A Systematic Review Study. Iran. J. Obstet. Gynecol. Infertil. 2020, 23, 79–94. [Google Scholar]
- Niazi, A.; Moradi, M.; Askari, V.R.; Sharifi, N. Effect of Complementary Medicine on Pain Relief and Wound Healing after Cesarean Section: A Systematic Review. J. Pharmacopunct. 2021, 24, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Tashkandi, H. Honey in Wound Healing: An Updated Review. Open Life Sci. 2021, 16, 1091–1100. [Google Scholar] [CrossRef]
- Al-Waili, N.; Salom, K.; Al-Ghamdi, A.A. Honey for Wound Healing, Ulcers, and Burns; Data Supporting Its Use in Clinical Practice. Sci. World J. 2011, 11, 766–787. [Google Scholar] [CrossRef]
- da Silva, P.M.; Gauche, C.; Gonzaga, L.V.; Costa, A.C.O.; Fett, R. Honey: Chemical Composition, Stability and Authenticity. Food Chem. 2016, 196, 309–323. [Google Scholar] [CrossRef]
- Saikaly, S.K.; Khachemoune, A. Honey and Wound Healing: An Update. Am. J. Clin. Dermatol. 2017, 18, 237–251. [Google Scholar] [CrossRef]
- Hadagali, M.D.; Chua, L.S. The Anti-Inflammatory and Wound Healing Properties of Honey. Eur. Food Res. Technol. 2014, 239, 1003–1014. [Google Scholar] [CrossRef]
- El-Kased, R.F.; Amer, R.I.; Attia, D.; Elmazar, M.M. Honey-Based Hydrogel: In Vitro and Comparative In Vivo Evaluation for Burn Wound Healing. Sci. Rep. 2017, 7, 9692. [Google Scholar] [CrossRef]
- Jull, A.B.; Cullum, N.; Dumville, J.C.; Westby, M.J.; Deshpande, S.; Walker, N. Honey as a Topical Treatment for Wounds. Cochrane Database Syst. Rev. 2015, 2015, CD005083. [Google Scholar] [CrossRef]
- Al-Waili, N.S.; Saloom, K.Y. Effects of Topical Honey on Post-Operative Wound Infections Due to Gram Positive and Gram Negative Bacteria Following Caesarean Sections and Hysterectomies. Eur. J. Med. Res. 1999, 4, 126–130. [Google Scholar] [PubMed]
- Wang, C.; Guo, M.; Zhang, N.; Wang, G. Effectiveness of Honey Dressing in the Treatment of Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis. Complement. Ther. Clin. Pract. 2019, 34, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Shirvani, M.A.; Nikpour, M.; Azadbakht, M.; Banihosseini, S.Z.; Zanjani, R. The Effect of Honey Gel on Cesarean Incision Pain: A Triple Blind Clinical Trial. AJPP 2013, 7, 19–24. [Google Scholar] [CrossRef]
- RoB 2: A Revised Cochrane Risk-of-Bias Tool for Randomized Trials|Cochrane Bias. Available online: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials (accessed on 27 January 2023).
- OpenMeta[Analyst]—CEBM @ Brown. Available online: http://www.cebm.brown.edu/openmeta/ (accessed on 10 August 2023).
- Heidari, T.; Roozbahani, N.; Amiri Farahani, L.; Attarha, M.; Akbari Torkestani, N.; Jamilian, M.; Bekhradi, R. Does Iranian Astragalus Gossypinus Honey Assist in Healing Caesarean Wounds and Scars? Eur. J. Integr. Med. 2013, 5, 226–233. [Google Scholar] [CrossRef]
- Nikpour, M.; Shirvani, M.A.; Azadbakht, M.; Zanjani, R.; Mousavi, E. The Effect of Honey Gel on Abdominal Wound Healing in Cesarean Section: A Triple Blind Randomized Clinical Trial. Oman Med. J. 2014, 29, 255–259. [Google Scholar] [CrossRef]
- Nikpour, M.; Delavar, M.; Khafri, S.; Ghanbarpour, A.; Moghadamnia, A.; Esmaeilzadeh, S.; Behmanesh, F. The Use of Honey and Curcumin for Episiotomy Pain Relief and Wound Healing: A Three-Group Double-Blind Randomized Clinical Trial. Nurs. Midwifery Stud. 2019, 8, 64–69. [Google Scholar]
- Oryan, A.; Alemzadeh, E.; Moshiri, A. Biological Properties and Therapeutic Activities of Honey in Wound Healing: A Narrative Review and Meta-Analysis. J. Tissue Viability 2016, 25, 98–118. [Google Scholar] [CrossRef]
- Putri, N.M.; Kreshanti, P.; Tunjung, N.; Indania, A.; Basuki, A.; Sukasah, C.L. Efficacy of Honey Dressing versus Hydrogel Dressing for Wound Healing. AIP Conf. Proc. 2021, 2344, 020022. [Google Scholar] [CrossRef]
- Yilmaz, A.C.; Aygin, D. Honey dressing in wound treatment: A systematic review. Complement. Ther. Med. 2020, 51, 102388. [Google Scholar] [CrossRef]
- Lavaf, M.; Simbar, M.; Mojab, F.; Alavi Majd, H.; Samimi, M. Comparison of Honey and Phenytoin (PHT) Cream Effects on Intensity of Pain and Episiotomy Wound Healing in Nulliparous Women. J. Complement. Integr. Med. 2017, 15, 20160139. [Google Scholar] [CrossRef] [PubMed]
- Rohmatin, E.; Patmawati, N.M.; Yuliastuti, S.; Sahlan, M. Topical effect of tetragonula sapiens honey on the healing process of post-caesarean section wounds. Int. J. Appl. Pharm. 2022, 14, 18–21. [Google Scholar] [CrossRef]
- Sirkeci, I.; Cagan, O.; Koc, S. The Effect of Ylang Oil and Lemon Oil Inhalation on Labor Pain and Anxiety Pregnant Women: A Randomized Controlled Trial. Complement. Ther. Clin. Pract. 2023, 52, 101748. [Google Scholar] [CrossRef] [PubMed]
- Eskandari, F.; Mousavi, P.; Valiani, M.; Ghanbari, S.; Iravani, M. Investigating the Effect of Swedish Massage with Chamomile Oil on Labor Pain and Anxiety of Primiparous Women: A Clinical Trial. J. Educ. Health Promot. 2023, 12, 157. [Google Scholar]
| Gerosa, 2022 [1] | Nikpour, 2014 [18] | Nikpour, 2019 [19] | Heidari, 2013 [17] | Shirvani, 2013 [14] | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Placebo | Honey | Placebo | Honey | Placebo | Honey | Placebo | Honey | Placebo | Honey | |
| Location; Period | Maternity hospital of the University Hospital of Geneva (2018–2019) | North of Iran | Shahid Yahyanejad hospital, Babol, Iran (2014–2016) | Ayatollah Taleghani Hospital in Arak (2008–2010) | Imam Ali Hospital (in the North of Iran) (2010–2011) | |||||
| Study design | RCT | RCT | RCT | RCT | RCT | |||||
| Honey used | Medihoney® a | Coriander and Goat’s-thorn flowers honey | Coriander and Goat´s-thorn flowers honey | Astragalus gossypinus honey | Coriander and Goat´s-thorn flowers honey | |||||
| Type of wound | Perineal laceration | Cesarean section | Episiotomy | Cesarean section | Cesarean section | |||||
| Sample size | 31 | 29 | 38 | 37 | 29 | 30 | 40 | 44 | 38 | 37 |
| Age (years): mean ± SD | 33.80 ± 5.04 | 33.31 ± 4.31 | 26.57 ± 4.88 | 27.70 ± 4.97 | 24.39 ± 4.21 | 25.12 ± 3.72 | 27.38 ± 5.19 | 27.48 ± 4.31 | 26.57 ± 4.88 | 27.77 ± 4.97 |
| Education n (%): Primary school | 2/31 (6.45) b | 3/29 (10.34) b | 3 (50) | 3 (50) | 9 (31.0) | 12 (40.0) | NA | NA | 18 (21.1) | 11 (29.7) |
| High school | 7/31 (22.58) | 4/29 (13.79) | 25 (52) | 23 (48) | 14 (46.7) | 14 (46.7) | NA | NA | 20 (52.6) | 15 (40.5) |
| University | 7/31 (22.58) | 4/29 (13.79) | 10 (48) | 11 (52) | 6 (20.7) | 4 (13.3) | NA | NA | 10 (26.3) | 11 (29.7) |
| Mother’s occupation Housewife | NA | NA | 31 (53) | 28 (48) | 24 (82.8) | 25 (83.3) | NA | NA | 30 (78.9) | 28 (75.5) |
| Employed | NA | NA | At home 7(44) | At home 9(56) | 5 (17.2) | 5 (16.7) | NA | NA | 8 (21.1) | 9 (24.3) |
| Mean neonate weight (SD) | 3285 ± 570 | 3357 ± 350 | NA | NA | 3243 ± 29.65 | 3239 ± 35.69 | 3247.86 ± 397.86 | 3220.68 ± 406.89 | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferraz Barbosa, B.; de Moraes, F.C.A.; Araujo Alves da Silva, B.; Bordignon Barbosa, C.; Pereira da Silva, I.; da Silva, E.R.; Barros, J.C.M.; Rebouças, L.W.C.; dos Santos, N.P.C.; Fernandes, M.R. The Use of Honey for Cicatrization and Pain Control of Obstetric Wounds: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2024, 16, 185. https://doi.org/10.3390/nu16020185
Ferraz Barbosa B, de Moraes FCA, Araujo Alves da Silva B, Bordignon Barbosa C, Pereira da Silva I, da Silva ER, Barros JCM, Rebouças LWC, dos Santos NPC, Fernandes MR. The Use of Honey for Cicatrization and Pain Control of Obstetric Wounds: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2024; 16(2):185. https://doi.org/10.3390/nu16020185
Chicago/Turabian StyleFerraz Barbosa, Bárbara, Francisco Cezar Aquino de Moraes, Bruno Araujo Alves da Silva, Camila Bordignon Barbosa, Izael Pereira da Silva, Emanuele Rocha da Silva, Jamile Cristine Marques Barros, Laissa Wane Cavalcante Rebouças, Ney Pereira Carneiro dos Santos, and Marianne Rodrigues Fernandes. 2024. "The Use of Honey for Cicatrization and Pain Control of Obstetric Wounds: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" Nutrients 16, no. 2: 185. https://doi.org/10.3390/nu16020185
APA StyleFerraz Barbosa, B., de Moraes, F. C. A., Araujo Alves da Silva, B., Bordignon Barbosa, C., Pereira da Silva, I., da Silva, E. R., Barros, J. C. M., Rebouças, L. W. C., dos Santos, N. P. C., & Fernandes, M. R. (2024). The Use of Honey for Cicatrization and Pain Control of Obstetric Wounds: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients, 16(2), 185. https://doi.org/10.3390/nu16020185