The Relationship between Plant-Based Diet Indices and Sleep Health in Older Adults: The Mediating Role of Depressive Symptoms and Anxiety
Abstract
1. Background
2. Materials and Methods
2.1. Research Subjects
2.2. Outcome Measures
2.3. Measurements of PDI
2.4. Assessment of Depression and Anxiety
2.5. Covariates
2.6. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Association between the PDI and Sleep Health
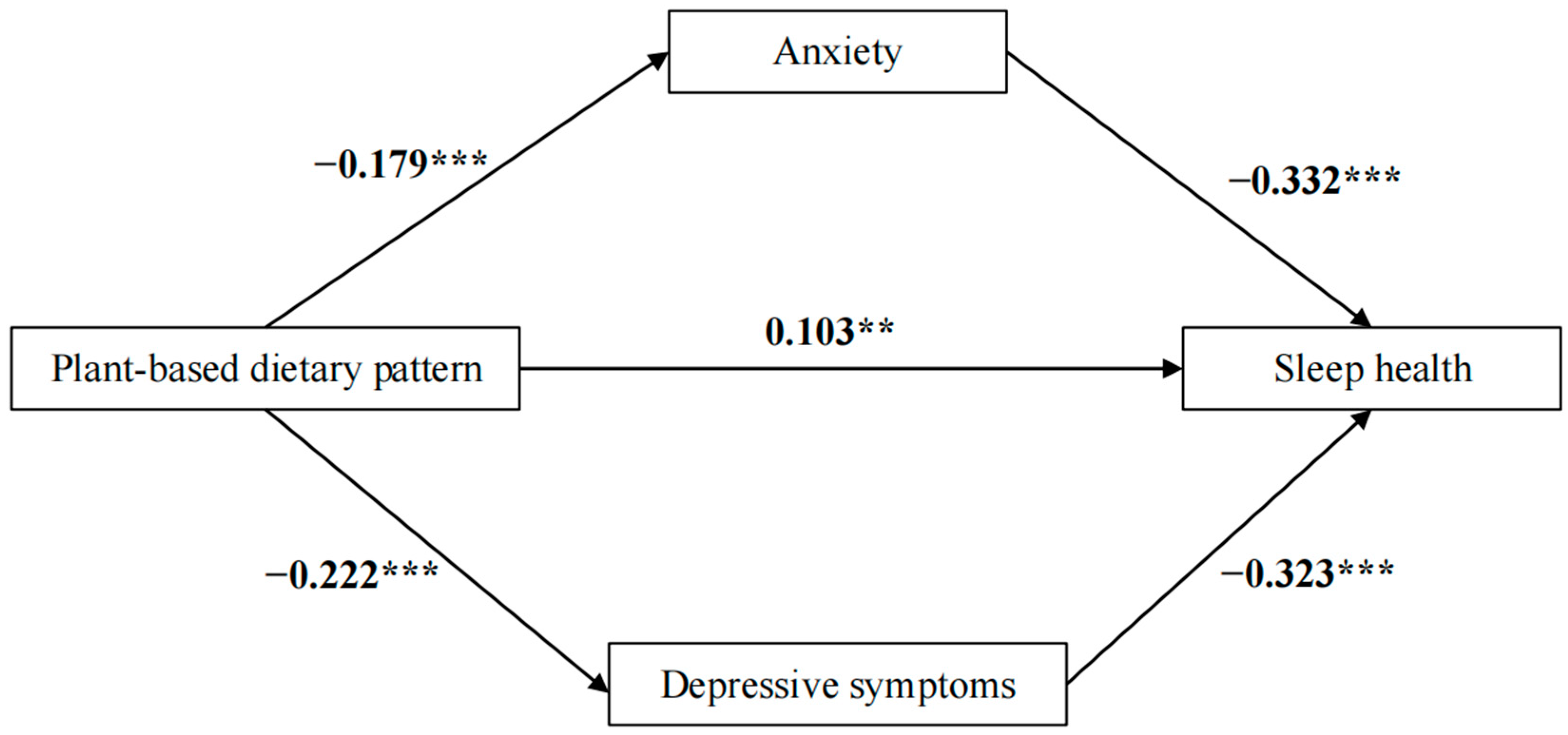
3.3. The Mediated Effect of Anxiety and Depression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stranges, S.; Tigbe, W.; Gómez-Olivé, F.X.; Thorogood, M.; Kandala, N.B. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 2012, 35, 1173–1181. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Wang, S.B.; Zheng, H.; Tan, W.Y.; Li, X.; Huang, Z.H.; Hou, C.L.; Jia, F.J. The role of anxiety and depression in the relationship between physical activity and sleep quality: A serial multiple mediation model. J. Affect. Disord. 2021, 290, 219–226. [Google Scholar] [CrossRef]
- Mollayeva, T.; Thurairajah, P.; Burton, K.; Mollayeva, S.; Shapiro, C.M.; Colantonio, A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 25, 52–73. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.P.; Jarrett, M.A.; Luebbe, A.M.; Garner, A.A.; Burns, G.L.; Kofler, M.J. Sleep in a large, multi-university sample of college students: Sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 2018, 4, 174–181. [Google Scholar] [CrossRef]
- Jean-Louis, G.; Kripke, D.F.; Ancoli-Israel, S. Sleep and quality of well-being. Sleep 2000, 23, 1115–1121. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Lin, H.; Zhang, J.; Sheng, M.; Kathleen, Y.; Zheng, P.; Jiang, S. Real-world association of self-reported sleep duration and quality with falls among older adults: A representative nationwide study of China. Sleep Med. 2022, 100, 212–218. [Google Scholar] [CrossRef]
- Jensen, J.D. Health economic benefits from optimized meal services to older adults-a literature-based synthesis. Eur. J. Clin. Nutr. 2021, 75, 26–37. [Google Scholar] [CrossRef]
- Fuentecilla, J.L.; Huo, M.; Birditt, K.S.; Charles, S.T.; Fingerman, K.L. Interpersonal Tensions and Pain Among Older Adults: The Mediating Role of Negative Mood. Res. Aging 2020, 42, 105–114. [Google Scholar] [CrossRef]
- Salo, P.; Vahtera, J.; Ferrie, J.E.; Akbaraly, T.; Goldberg, M.; Zins, M.; Pentti, J.; Virtanen, M.; Shipley, M.J.; Singh-Manoux, A.; et al. Trajectories of sleep complaints from early midlife to old age: Longitudinal modeling study. Sleep 2012, 35, 1559–1568. [Google Scholar] [CrossRef][Green Version]
- Kent, R.G.; Uchino, B.N.; Cribbet, M.R.; Bowen, K.; Smith, T.W. Social Relationships and Sleep Quality. Ann. Behav. Med. 2015, 49, 912–917. [Google Scholar] [CrossRef]
- Godos, J.; Grosso, G.; Castellano, S.; Galvano, F.; Caraci, F.; Ferri, R. Association between diet and sleep quality: A systematic review. Sleep Med. Rev. 2021, 57, 101430. [Google Scholar] [CrossRef] [PubMed]
- Zhu, A.; Chen, H.; Shen, J.; Wang, X.; Li, Z.; Zhao, A.; Shi, X.; Yan, L.; Zeng, Y.; Yuan, C.; et al. Interaction between plant-based dietary pattern and air pollution on cognitive function: A prospective cohort analysis of Chinese older adults. Lancet Reg. Health West. Pac. 2022, 20, 100372. [Google Scholar] [CrossRef]
- Khayyatzadeh, S.S.; Mehramiz, M.; Mirmousavi, S.J.; Mazidi, M.; Ziaee, A.; Kazemi-Bajestani, S.M.R.; Ferns, G.A.; Moharreri, F.; Ghayour-Mobarhan, M. Adherence to a Dash-style diet in relation to depression and aggression in adolescent girls. Psychiatry Res. 2018, 259, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Quek, J.; Lim, G.; Lim, W.H.; Ng, C.H.; So, W.Z.; Toh, J.; Pan, X.H.; Chin, Y.H.; Muthiah, M.D.; Chan, S.P.; et al. The Association of Plant-Based Diet with Cardiovascular Disease and Mortality: A Meta-Analysis and Systematic Review of Prospect Cohort Studies. Front. Cardiovasc. Med. 2021, 8, 756810. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; Liu, K.; Liang, C.; Wang, Y.; Guo, Z. The relationship between living alone or not and depressive symptoms in older adults: A parallel mediation effect of sleep quality and anxiety. BMC Geriatr. 2023, 23, 506. [Google Scholar] [CrossRef]
- Zhang, P.; Wang, L.; Zhou, Q.; Dong, X.; Guo, Y.; Wang, P.; He, W.; Wang, R.; Wu, T.; Yao, Z.; et al. A network analysis of anxiety and depression symptoms in Chinese disabled elderly. J. Affect. Disord. 2023, 333, 535–542. [Google Scholar] [CrossRef]
- Yuan, L.; Xu, Q.; Gui, J.; Liu, Y.; Lin, F.; Zhao, Z.; Sun, J. Decomposition and comparative analysis of differences in depressive symptoms between urban and rural older adults: Evidence from a national survey. Int. Psychogeriatr. 2023, 1–12. [Google Scholar] [CrossRef]
- Bai, W.; Zhang, J.; Smith, R.D.; Cheung, T.; Su, Z.; Ng, C.H.; Zhang, Q.; Xiang, Y.T. Inter-relationship between cognitive performance and depressive symptoms and their association with quality of life in older adults: A network analysis based on the 2017–2018 wave of Chinese Longitudinal Healthy Longevity Survey (CLHLS). J. Affect. Disord. 2023, 320, 621–627. [Google Scholar] [CrossRef]
- Zamani, B.; Daneshzad, E.; Siassi, F.; Guilani, B.; Bellissimo, N.; Azadbakht, L. Association of plant-based dietary patterns with psychological profile and obesity in Iranian women. Clin. Nutr. 2020, 39, 1799–1808. [Google Scholar] [CrossRef]
- Poulsen, N.B.; Lambert, M.N.T.; Jeppesen, P.B. The Effect of Plant Derived Bioactive Compounds on Inflammation: A Systematic Review and Meta-Analysis. Mol. Nutr. Food Res. 2020, 64, e2000473. [Google Scholar] [CrossRef]
- Zou, L.; Tian, Y.; Wang, Y.; Chen, D.; Lu, X.; Zeng, Z.; Chen, Z.; Lin, C.; Liang, Y. High-cholesterol diet promotes depression- and anxiety-like behaviors in mice by impact gut microbe and neuroinflammation. J. Affect. Disord. 2023, 327, 425–438. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Zhang, Q.; Han, Y.; Liu, J. Sleep Quality and Subjective Cognitive Decline among Older Adults: The Mediating Role of Anxiety/Depression and Worries. J. Aging Res. 2024, 2024, 4946303. [Google Scholar] [CrossRef] [PubMed]
- Naismith, S.L.; Rogers, N.L.; Lewis, S.J.; Terpening, Z.; Ip, T.; Diamond, K.; Norrie, L.; Hickie, I.B. Sleep disturbance relates to neuropsychological functioning in late-life depression. J. Affect. Disord. 2011, 132, 139–145. [Google Scholar] [CrossRef]
- Tang, S.; Zhou, J.; Liu, C.; Wang, S.; Cong, Y.; Chen, L.; Zhang, L.; Tan, X.; Li, T.; Li, Y.; et al. Association of plant-based diet index with sleep quality in middle-aged and older adults: The Healthy Dance Study. Sleep Health 2023, 9, 698–703. [Google Scholar] [CrossRef]
- Qi, R.; Sheng, B.; Zhou, L.; Chen, Y.; Sun, L.; Zhang, X. Association of Plant-Based Diet Indices and Abdominal Obesity with Mental Disorders among Older Chinese Adults. Nutrients 2023, 15, 2721. [Google Scholar] [CrossRef] [PubMed]
- Liang, F.; Fu, J.; Turner-McGrievy, G.; Wang, Y.; Qiu, N.; Ding, K.; Zeng, J.; Moore, J.B.; Li, R. Association of Body Mass Index and Plant-Based Diet with Cognitive Impairment among Older Chinese Adults: A Prospective, Nationwide Cohort Study. Nutrients 2022, 14, 3132. [Google Scholar] [CrossRef]
- Qi, R.; Yang, Y.; Sheng, B.; Li, H.; Zhang, X. Plant-Based Diet Indices and Their Association with Frailty in Older Adults: A CLHLS-Based Cohort Study. Nutrients 2023, 15, 5120. [Google Scholar] [CrossRef]
- Hu, C.; Jiang, K.; Sun, X.; He, Y.; Li, R.; Chen, Y.; Zhang, Y.; Tao, Y.; Jin, L. Change in healthy lifestyle and subsequent risk of cognitive impairment among Chinese older adults: A National Community-Based Cohort Study. J. Gerontol. A Biol. Sci. Med. Sci. 2024, 79, glae148. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation's sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef]
- Kim, J.; Kim, H.; Giovannucci, E.L. Plant-based diet quality and the risk of total and disease-specific mortality: A population-based prospective study. Clin. Nutr. 2021, 40, 5718–5725. [Google Scholar] [CrossRef]
- Huang, S.; Lou, Y.; Wang, S.; You, Q.; Jiang, Q.; Cao, S. Association of changes in plant-based diet consumption with all-cause mortality among older adults in China: A prospective study from 2008 to 2019. J. Nutr. Health Aging 2024, 28, 100027. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Shen, J.; Xuan, J.; Zhu, A.; Ji, J.S.; Liu, X.; Cao, Y.; Zong, G.; Zeng, Y.; Wang, X.; et al. Plant-based dietary patterns in relation to mortality among older adults in China. Nat. Aging 2022, 2, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Ding, K.; Zeng, J.; Zhang, X.; Wang, Y.; Liang, F.; Wang, L.; Guo, T.; Moore, J.B.; Li, R. Changes in Plant-Based Dietary Quality and Subsequent Risk of Cognitive Impairment Among Older Chinese Adults: A National Community-Based Cohort Study. Am. J. Clin. Nutr. 2023, 118, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Weston, L.J.; Kim, H.; Talegawkar, S.A.; Tucker, K.L.; Correa, A.; Rebholz, C.M. Plant-based diets and incident cardiovascular disease and all-cause mortality in African Americans: A cohort study. PLoS Med. 2022, 19, e1003863. [Google Scholar] [CrossRef]
- Xiao, S.; Shi, L.; Zhang, J.; Li, X.; Lin, H.; Xue, Y.; Xue, B.; Chen, Y.; Zhou, G.; Zhang, C. The role of anxiety and depressive symptoms in mediating the relationship between subjective sleep quality and cognitive function among older adults in China. J. Affect. Disord. 2023, 325, 640–646. [Google Scholar] [CrossRef]
- Huang, J.; Mao, Y.; Zhao, X.; Liu, Q.; Zheng, T. Association of anxiety, depression symptoms and sleep quality with chronic kidney disease among older Chinese. Medicine 2023, 102, e35812. [Google Scholar] [CrossRef]
- Li, S.H.; Lloyd, A.R.; Graham, B.M. Subjective sleep quality and characteristics across the menstrual cycle in women with and without Generalized Anxiety Disorder. J. Psychosom. Res. 2021, 148, 110570. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Zhu, H.; Zhang, Y.; Wang, D.; Guo, H.; Liu, X.; Lai, J.; Zhang, H.; Xu, H.; Bai, B. The relationship between dysphagia and frailty among Chinese hospitalized older patients: A serial mediation model through self-perceived oral health and self-reported nutritional status. BMC Geriatr. 2024, 24, 110. [Google Scholar] [CrossRef]
- Huang, S.; Zhong, D.; Lv, Z.; Cheng, J.; Zou, X.; Wang, T.; Wen, Y.; Wang, C.; Yu, S.; Huang, H.; et al. Associations of multiple plasma metals with the risk of metabolic syndrome: A cross-sectional study in the mid-aged and older population of China. Ecotoxicol. Environ. Saf. 2022, 231, 113183. [Google Scholar] [CrossRef]
- Pengpid, S.; Peltzer, K. Fruit and Vegetable Consumption is Protective from Short Sleep and Poor Sleep Quality Among University Students from 28 Countries. Nat. Sci. Sleep. 2020, 12, 627–633. [Google Scholar] [CrossRef]
- Godos, J.; Ferri, R.; Castellano, S.; Angelino, D.; Mena, P.; Del Rio, D.; Caraci, F.; Galvano, F.; Grosso, G. Specific Dietary (Poly)phenols Are Associated with Sleep Quality in a Cohort of Italian Adults. Nutrients 2020, 12, 1226. [Google Scholar] [CrossRef] [PubMed]
- Zuraikat, F.M.; Wood, R.A.; Barragán, R.; St-Onge, M.P. Sleep and Diet: Mounting Evidence of a Cyclical Relationship. Annu. Rev. Nutr. 2021, 41, 309–332. [Google Scholar] [CrossRef] [PubMed]
- Muthuraman, K.; Sankaran, A.; Subramanian, K. Association Between Sleep-related Cognitions, Sleep-related Behaviors, and Insomnia in Patients with Anxiety and Depression: A Cross-sectional Study. Indian. J. Psychol. Med. 2024, 46, 228–237. [Google Scholar] [CrossRef]
- Scott, A.J.; Webb, T.L.; Martyn-St James, M.; Rowse, G.; Weich, S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med. Rev. 2021, 60, 101556. [Google Scholar] [CrossRef]
- Assari, S.; Sonnega, A.; Pepin, R.; Leggett, A. Residual Effects of Restless Sleep over Depressive Symptoms on Chronic Medical Conditions: Race by Gender Differences. J. Racial Ethn. Health Disparities 2017, 4, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Irwin, M.R.; Olmstead, R.; Carroll, J.E. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol. Psychiatry 2016, 80, 40–52. [Google Scholar] [CrossRef]
- Mousavi, S.M.; Ebrahimi-Mousavi, S.; Hassanzadeh Keshteli, A.; Afshar, H.; Esmaillzadeh, A.; Adibi, P. The association of plant-based dietary patterns and psychological disorders among Iranian adults. J. Affect. Disord. 2022, 300, 314–321. [Google Scholar] [CrossRef]
- Daneshzad, E.; Keshavarz, S.A.; Qorbani, M.; Larijani, B.; Bellissimo, N.; Azadbakht, L. Association of dietary acid load and plant-based diet index with sleep, stress, anxiety and depression in diabetic women. Br. J. Nutr. 2020, 123, 901–912. [Google Scholar] [CrossRef]
- Wang, X.; Yin, Z.; Yang, Y.; Fu, X.; Guo, C.; Pu, K.; Zang, S. Association of plant-based dietary patterns with depression and anxiety symptoms in Chinese older adults: A nationwide study. J. Affect. Disord. 2024, 350, 838–846. [Google Scholar] [CrossRef]
- Li, Y.; Lv, M.R.; Wei, Y.J.; Sun, L.; Zhang, J.X.; Zhang, H.G.; Li, B. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 2017, 253, 373–382. [Google Scholar] [CrossRef]
- Godos, J.; Castellano, S.; Ray, S.; Grosso, G.; Galvano, F. Dietary Polyphenol Intake and Depression: Results from the Mediterranean Healthy Eating, Lifestyle and Aging (MEAL) Study. Molecules 2018, 23, 999. [Google Scholar] [CrossRef] [PubMed]
- Furihata, R.; Endo, D.; Nagaoka, K.; Hori, A.; Ito, T.; Iwami, T.; Akahoshi, T. Association between a composite measure of sleep health and depressive symptoms in patients with obstructive sleep apnea treated with CPAP therapy: Real-world data. Sleep Med. 2024, 120, 22–28. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Total (n = 6853) | Q1 (n = 1938) | Q2 (n = 1460) | Q3 (n = 1887) | Q4 (n = 1568) | p Value |
|---|---|---|---|---|---|---|
| Anxiety | 743 (10.84) | 260 (34.99) | 156 (21.00) | 193 (25.98) | 134 (18.03) | 0.000 |
| Depression | 3243 (47.32) | 1053 (32.47) | 720 (22.20) | 881 (27.17) | 589 (18.16) | 0.000 |
| Gender | ||||||
| Female | 3585 (52.31) | 1102 (30.74) | 776 (21.65) | 984 (27.45) | 723 (20.17) | 0.000 |
| Male | 3268 (47.69) | 836 (25.58) | 684 (20.93) | 903 (27.63) | 845 (25.86) | |
| Age * | 82.46 (11.31) | 85.15 (11.31) | 82.99 (11.30) | 81.35 (11.03) | 80.00 (10.89) | 0.000 |
| Residence | ||||||
| Rural | 5648 (82.42) | 1656 (29.32) | 1190 (21.07) | 1542 (27.30) | 1260 (22.31) | 0.000 |
| Urban | 1205 (17.58) | 282 (23.40) | 270 (22.41) | 345 (28.63) | 308 (25.56) | |
| Living condition | ||||||
| Live with family | 5719 (83.45) | 1559 (27.26) | 1227 (21.45) | 1593 (27.85) | 1340 (23.43) | 0.001 |
| Solitude | 1123 (16.39) | 375 (33.39) | 229 (20.39) | 294 (26.18) | 225 (20.04) | |
| Other | 11 (0.16) | 4 (36.36) | 4 (36.36) | 0 (0.00) | 3 (27.27) | |
| Marital status | ||||||
| Married/cohabitating | 3326 (48.53) | 776 (23.33) | 697 (20.96) | 975 (29.31) | 878 (26.40) | 0.000 |
| Widowed | 3365 (49.10) | 1115 (33.14) | 734 (21.81) | 863 (25.65) | 653 (19.41) | |
| Other | 162 (2.36) | 47 (29.01) | 29 (17.90) | 49 (30.25) | 37 (22.84) | |
| With formal education | 4048 (59.07) | 959 (23.48) | 887 (21.91) | 1150 (28.41) | 1052 (25.99) | 0.000 |
| Occupation | ||||||
| Professional and technical personnel | 542 (7.90) | 93 (17.16) | 124 (22.88) | 157 (28.97) | 168 (31.00) | 0.000 |
| Governmental, institutional, or managerial personnel | 317 (4.63) | 63 (19.87) | 68 (21.45) | 88 (27.76) | 98 (30.91) | |
| General staff, service personnel or workers | 1081 (15.77) | 253 (23.40) | 247 (22.85) | 311 (28.77) | 270 (24.98) | |
| Farmers | 4129 (60.25) | 1310 (31.73) | 854 (20.68) | 1127 (27.29) | 838 (20.30) | |
| Other | 784 (11.44) | 219 (27.93) | 167 (21.30) | 204 (26.02) | 194 (24.74) | |
| Sufficiency of living resources | 6036 (88.08) | 1626 (26.94) | 1305 (21.63) | 1693 (28.05) | 1412 (23.39) | 0.000 |
| Wealthy economic situation | 1457 (21.26) | 324 (22.24) | 318 (21.83) | 418 (26.69) | 397 (27.25) | 0.000 |
| Annual household income * | 43,507.55 (36,920.75) | 39,313.31 (35,421.25) | 44,861.19 (37,496.54) | 44,753.63 (37,183.04) | 45,931.50 (37,487.84) | 0.000 |
| Housing nature | ||||||
| Purchased or self-built | 5985 (87.33) | 1701 (28.42) | 1269 (21.21) | 1652 (27.60) | 1363 (22.77) | 0.831 |
| Other | 868 (12.67) | 237 (27.30) | 191 (22.00) | 235 (27.07) | 205 (23.62) | |
| Housing type | ||||||
| Bungalow | 637 (9.30) | 241 (37.83) | 114 (17.90) | 183 (28.73) | 99 (15.54) | 0.000 |
| Apartment | 2009 (29.32) | 516 (25.68) | 423 (21.06) | 545 (27.13) | 525 (26.13) | |
| Other | 4207 (61.39) | 1181 (28.07) | 923 (21.94) | 1159 (27.55) | 944 (22.44) | |
| Separated bedrooms | 6503 (94.89) | 1830 (28.14) | 1376 (21.16) | 1808 (27.80) | 1489 (22.90) | 0.142 |
| Self-reported health | ||||||
| Poor | 873 (12.74) | 310 (35.51) | 195 (22.34) | 206 (23.60) | 162 (18.56) | 0.000 |
| Fair | 2567 (37.46) | 794 (30.93) | 595 (23.18) | 679 (26.45) | 499 (19.44) | |
| Good | 3413 (49.80) | 834 (24.44) | 670 (19.63) | 1002 (29.36) | 907 (26.57) | |
| Smoking | ||||||
| Never | 4631 (67.58) | 1396 (30.14) | 1006 (21.72) | 1301 (28.09) | 928 (20.04) | 0.000 |
| Former | 1078 (15.73) | 247 (22.91) | 228 (21.15) | 280 (25.97) | 323 (29.96) | |
| Current | 1144 (16.69) | 295 (25.79) | 226 (19.76) | 306 (26.75) | 317 (27.71) | |
| Drinking | ||||||
| Never | 4895 (71.43) | 1424 (29.09) | 1081 (22.08) | 1367 (27.93) | 1023 (20.90) | 0.000 |
| Former | 820 (12.01) | 242 (29.51) | 156 (19.02) | 218 (26.59) | 204 (24.88) | |
| Current | 1138 (16.61) | 272 (23.90) | 223 (20.47) | 302 (26.54) | 341 (29.96) | |
| Exercise | ||||||
| Never | 3870 (56.47) | 1232 (31.83) | 868 (22.43) | 1043 (26.95) | 727 (18.76) | 0.000 |
| Former | 487 (7.11) | 152 (31.21) | 101 (20.74) | 120 (24.64) | 114 (23.41) | |
| Current | 2496 (36.42) | 554 (22.20) | 491 (19.67) | 724 (29.01) | 727 (29.13) | |
| BMI (kg/m2) * | 23.68 (36.72) | 23.15 (20.52) | 23.14 (14.87) | 24.93 (65.30) | 23.34 (5.85) | 0.000 |
| Hypertension | 2986 (43.57) | 745 (24.95) | 648 (21.70) | 874 (29.27) | 719 (24.08) | 0.000 |
| Diabetes | 560 (8.17) | 131 (23.39) | 147 (26.25) | 163 (25.08) | 119 (21.25) | 0.004 |
| Heart disease | 1231 (17.96) | 315 (25.59) | 271 (22.01) | 361 (29.33) | 284 (23.07) | 0.113 |
| Stroke, cerebrovascular disease | 748 (10.91) | 180 (24.06) | 172 (22.99) | 230 (30.75) | 166 (22.19) | 0.021 |
| Dyslipidemia | 468 (6.83) | 93 (19.87) | 114 (24.36) | 129 (27.56) | 132 (28.21) | 0.000 |
| Geographic region | ||||||
| East China | 3317 (48.40) | 747 (22.52) | 713 (21.50) | 989 (29.82) | 868 (26.17) | 0.000 |
| Central China | 1568 (22.88) | 466 (29.72) | 366 (23.34) | 432 (27.55) | 304 (19.39) | |
| West China | 1608 (23.46) | 649 (40.36) | 314 (19.53) | 348 (21.64) | 297 (18.47) | |
| Northeast China | 360 (5.25) | 76 (21.11) | 67 (18.61) | 118 (32.78) | 99 (27.50) |
| Continuous | Q1 | Q2 | Q3 | Q4 | p for Trend | |
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |||
| Sleep quality | ||||||
| PDI | ||||||
| Model 1 | 1.037 (1.028, 1.046) | 1.0 (ref.) | 1.104 (0.964, 1.264) | 1.269 (1.118, 1.442) | 1.676 (1.464, 1.919) | <0.001 |
| Model 2 | 1.014 (1.003, 1.024) | 1.0 (ref.) | 0.972 (0.837, 1.128) | 1.029 (0.894, 1.184) | 1.209 (1.039, 1.407) | 0.017 |
| hPDI | ||||||
| Model 1 | 1.025 (1.016, 1.035) | 1.0 (ref.) | 1.171 (1.030, 1.331) | 1.262 (1.101, 1.448) | 1.420 (1.238, 1.630) | <0.001 |
| Model 2 | 1.004 (0.993, 1.014) | 1.0 (ref.) | 1.013 (0.880, 1.166) | 1.002 (0.860, 1.167) | 1.076 (0.921, 1.256) | 0.413 |
| uPDI | ||||||
| Model 1 | 0.962 (0.956, 0.969) | 1.0 (ref.) | 0.911 (0.797, 1.041) | 0.744 (0.656, 0.844) | 0.474 (0.413, 0.543) | <0.001 |
| Model 2 | 0.982 (0.973, 0.990) | 1.0 (ref.) | 1.023 (0.880, 1.188) | 0.926 (0.797, 1.075) | 0.678 (0.574, 0.800) | <0.001 |
| Sleep duration | ||||||
| PDI | ||||||
| Model 1 | 1.033 (1.024, 1.043) | 1.0 (ref.) | 1.199 (1.040, 1.382) | 1.405 (1.231, 1.603) | 1.548 (1.349, 1.776) | <0.001 |
| Model 2 | 1.017 (1.007, 1.027) | 1.0 (ref.) | 1.086 (0.937, 1.258) | 1.204 (1.049, 1.382) | 1.241 (1.072, 1.437) | 0.001 |
| hPDI | ||||||
| Model 1 | 1.026 (1.017, 1.036) | 1.0 (ref.) | 1.073 (0.938, 1.227) | 1.351 (1.173, 1.556) | 1.412 (1.227, 1.625) | <0.001 |
| Model 2 | 1.007 (0.997, 1.017) | 1.0 (ref.) | 0.942 (0.820, 1.083) | 1.107 (0.955, 1.283) | 1.100 (0.947, 1.278) | 0.057 |
| uPDI | ||||||
| Model 1 | 0.969 (0.962, 0.976) | 1.0 (ref.) | 0.765 (0.669, 0.875) | 0.680 (0.598, 0.773) | 0.564 (0.490, 0.650) | <0.001 |
| Model 2 | 0.985 (0.977, 0.994) | 1.0 (ref.) | 0.869 (0.754, 1.002) | 0.819 (0.709, 0.946) | 0.762 (0.647, 0.896) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Liu, Z.; Zhou, Y.; Wu, L.; Wang, N.; Liu, X.; Liu, Y.; Yin, X.; Yang, A.; Liang, L. The Relationship between Plant-Based Diet Indices and Sleep Health in Older Adults: The Mediating Role of Depressive Symptoms and Anxiety. Nutrients 2024, 16, 3386. https://doi.org/10.3390/nu16193386
Liu J, Liu Z, Zhou Y, Wu L, Wang N, Liu X, Liu Y, Yin X, Yang A, Liang L. The Relationship between Plant-Based Diet Indices and Sleep Health in Older Adults: The Mediating Role of Depressive Symptoms and Anxiety. Nutrients. 2024; 16(19):3386. https://doi.org/10.3390/nu16193386
Chicago/Turabian StyleLiu, Junping, Zhaoyue Liu, Yue Zhou, Lin Wu, Nan Wang, Xinru Liu, Yaping Liu, Xinle Yin, Aiying Yang, and Libo Liang. 2024. "The Relationship between Plant-Based Diet Indices and Sleep Health in Older Adults: The Mediating Role of Depressive Symptoms and Anxiety" Nutrients 16, no. 19: 3386. https://doi.org/10.3390/nu16193386
APA StyleLiu, J., Liu, Z., Zhou, Y., Wu, L., Wang, N., Liu, X., Liu, Y., Yin, X., Yang, A., & Liang, L. (2024). The Relationship between Plant-Based Diet Indices and Sleep Health in Older Adults: The Mediating Role of Depressive Symptoms and Anxiety. Nutrients, 16(19), 3386. https://doi.org/10.3390/nu16193386






