Food Insecurity and Dietary Quality in African American Patients with Gastrointestinal Cancers: An Exploratory Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants and Recruitment
2.3. Study Procedure
2.4. Assessments and Measures
- Overall scores of 90 to 100, or component scores that are 90% to 100% of maximum score: A;
- Overall scores of 80 to 89, or component scores that are 80% to 89% of maximum score: B;
- Overall scores of 70 to 79, or component scores that are 70% to 79% of maximum score: C;
- Overall scores of 60 to 69, or component scores that are 60% to 69% of maximum score: D; and
- Overall scores of 0 to 59, or component scores that are 0% to 59% of maximum score: F [25].
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- USDA ERS. Definitions of Food Security. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx (accessed on 22 April 2023).
- Pan, L.; Sherry, B.; Njai, R.; Blanck, H. Food Insecurity Is Associated with Obesity among US Adults in 12 States. J. Acad. Nutr. Diet. 2012, 112, 1403–1409. [Google Scholar] [CrossRef] [PubMed]
- Morales, M.E.; Berkowitz, S.A. The Relationship between Food Insecurity, Dietary Patterns, and Obesity. Curr. Nutr. Rep. 2016, 5, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Household Food Security in the United States in 2019; United States Department of Agriculture, Economic Research Service: Washington, DC, USA, 2020. Available online: https://www.ers.usda.gov/webdocs/publications/99282/err-275.pdf?v=6912.2 (accessed on 15 March 2022).
- Dennard, E.; Kristjansson, E.; Tchangalova, N.; Totton, S.; Winham, D.; O’Connor, A. Food insecurity among African Americans in the United States: A scoping review. PLoS ONE 2022, 17, e0274434. [Google Scholar] [CrossRef]
- Morales, D.X.; Morales, S.A.; Beltran, T.F. Racial/Ethnic Disparities in Household Food Insecurity During the COVID-19 Pandemic: A Nationally Representative Study. J. Racial Ethn. Health Disparities 2021, 8, 1300–1314. [Google Scholar] [CrossRef] [PubMed]
- Powell, L.M.; Slater, S.; Mirtcheva, D.; Bao, Y.; Chaloupka, F.J. Food store availability and neighborhood characteristics in the United States. Prev. Med. 2007, 44, 189–195. [Google Scholar] [CrossRef]
- Mayer, V.L.; Hillier, A.; Bachhuber, M.A.; Long, J.A. Food insecurity, neighborhood food access, and food assistance in Philadelphia. J. Urban Health 2014, 91, 1087–1097. [Google Scholar] [CrossRef]
- Bovell-Benjamin, A.; Dawkins, N.; Pace, R.; Shikany, J.M. Dietary Consumption Practices and Cancer Risk In African Americans in the Rural South. J. Health Care Poor Underserved 2010, 21 (Suppl. 3), 57–75. [Google Scholar] [CrossRef][Green Version]
- Lin, B.H.; Ver Ploeg, M.; Kasteridis, P.; Yen, S. The roles of food prices and food access in determining food purchases of low-income households. J. Policy Model. 2014, 36, 938–952. [Google Scholar] [CrossRef]
- Rahkovsky, I.; Snyder, S. Food Choices and Store Proximity; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2015; ERR-195. [Google Scholar]
- Trego, M.L.; Baba, Z.M.; DiSantis, K.I.; Longacre, M.L. Food insecurity among adult cancer survivors in the United States. J. Cancer Surviv. 2019, 13, 641–652. [Google Scholar] [CrossRef]
- Coughlin, S.S. Social Determinants of Health and Cancer Survivorship. J. Environ. Health Sci. 2021, 7, 11–15. [Google Scholar]
- Rinninella, E.; Mele, M.C.; Cintoni, M.; Raoul, P.; Ianiro, G.; Salerno, L.; Pozzo, C.; Bria, E.; Muscaritoli, M.; Molfino, A.; et al. The Facts about Food after Cancer Diagnosis: A Systematic Review of Prospective Cohort Studies. Nutrients 2020, 12, 2345. [Google Scholar] [CrossRef] [PubMed]
- Milajerdi, A.; Namazi, N.; Larijani, B.; Azadbakht, L. The Association of Dietary Quality Indices and Cancer Mortality: A Systematic Review and Meta- analysis of Cohort Studies. Nutr. Cancer 2018, 70, 1091–1105. [Google Scholar] [CrossRef] [PubMed]
- Jain, R.; Handorf, E.; Khare, V.; Blau, M.; Chertock, Y.; Hall, M.J. Impact of Baseline Nutrition and Exercise Status on Toxicity and Outcomes in Phase I and II Oncology Clinical Trial Participants. Oncologist 2019, 25, 161–169. [Google Scholar] [CrossRef]
- Isenring, E.S.; Capra, S.; Bauer, J.D. Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. Br. J. Cancer 2004, 91, 447–452. [Google Scholar] [CrossRef]
- Tabung, F.K.; Fung, T.T.; Chavarro, J.E.; Smith-Warner, S.A.; Willett, W.C.; Giovannucci, E.L. Associations between adherence to the World Cancer Research Fund/American Institute for Cancer Research cancer prevention recommendations and biomarkers of inflammation, hormonal and insulin response. Int. J. Cancer 2017, 140, 764–776. [Google Scholar] [CrossRef] [PubMed]
- Trujillo, E.B.; Claghorn, K.; Dixon, S.W.; Hill, E.B.; Braun, A.; Lipinski, E.; Platek, M.E.; Vergo, M.T.; Spees, C. Inadequate Nutrition Coverage in Outpatient Cancer Centers: Results of a National Survey. J. Oncol. 2019, 2019, 7462940. [Google Scholar] [CrossRef]
- Resnicow, K.; Odom, E.; Wang, T.; Dudley, W.N.; Mitchell, D.; Vaughan, R.; Jackson, A.; Baranowski, T. Validation of Three Food Frequency Questionnaires and 24-Hour Recalls with Serum Carotenoid Levels in a Sample of African-American Adults. Am. J. Epidemiol. 2000, 152, 1072–1080. [Google Scholar] [CrossRef]
- Kristal, A.R.; Kolar, A.S.; Fisher, J.L.; Plascak, J.J.; Stumbo, P.J.; Weiss, R.; Paskett, E.D. Evaluation of Web-Based, Self-Administered, Graphical Food Frequency Questionnaire. J. Acad. Nutr. Diet. 2014, 114, 613–621. [Google Scholar] [CrossRef]
- Bickel, G.; Nord, M.; Price, C.; Hamilton, W.; Cook, J. Guide to Measuring Household Food Security; U.S. Department of Agriculture, Food and Nutrition Service: Alexandria, VA, USA, 2000. [Google Scholar]
- Deierlein, A.L.; Bihuniak, J.D.; Nagi, E.; Litvak, J.; Victoria, C.; Braune, T.; Weiss, R.; Parekh, N. Development of a Technology-Assisted Food Frequency Questionnaire for Elementary and Middle School Children: Findings from a Pilot Study. Nutrients 2019, 11, 1103. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans; U.S. Department of Health and Human Services: Washington, DC, USA; U.S. Department of Agriculture: Washington, DC, USA, 2015. [Google Scholar]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- Robien, K.; Clausen, M.; Sullo, E.; Ford, Y.R.; Griffith, K.A.; Le, D.; Wickersham, K.E.; Wallington, S.F. Prevalence of Food Insecurity Among Cancer Survivors in the United States: A Scoping Review. J. Acad. Nutr. Diet. 2023, 123, 330–346. [Google Scholar] [CrossRef] [PubMed]
- Poghosyan, H.; Scarpino, S.V. Food insecure cancer survivors continue to smoke after their diagnosis despite not having enough to eat: Implications for policy and clinical interventions. Cancer Causes Control 2019, 30, 241–248. [Google Scholar] [CrossRef] [PubMed]
- SNAP Benefits—COVID-19 Pandemic and Beyond. Available online: https://www.fns.usda.gov/snap/benefit-changes-2021 (accessed on 5 April 2023).
- Lee, E.; Zhu, J.; Velazquez, J.; Bernardo, R.; Garcia, J.; Rovito, M.; Hines, R.B. Evaluation of Diet Quality Among American Adult Cancer Survivors: Results From 2005-2016 National Health and Nutrition Examination Survey. J. Acad. Nutr. Diet. 2021, 121, 217–232. [Google Scholar] [CrossRef] [PubMed]
- The Demographic Statistical Atlas of the United States. Available online: https://statisticalatlas.com/neighborhood/Pennsylvania/Philadelphia/North-Central/Overview (accessed on 6 February 2022).
- The Demographic Statistical Atlas of the United States. Available online: https://statisticalatlas.com/neighborhood/Pennsylvania/Philadelphia/Fox-Chase/Household-Income (accessed on 6 February 2022).
- Lauren, B.N.; Silver, E.R.; Faye, A.S.; Rogers, A.M.; Baidal, J.A.W.; Ozanne, E.M.; Hur, C. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutr. 2021, 24, 3929–3936. [Google Scholar] [CrossRef] [PubMed]
- Furness, B.W.; Simon, P.A.; Wold, C.M.; Asarian-Anderson, J. Prevalence and predictors of food insecurity among low-income households in Los Angeles County. Public Health Nutr. 2004, 7, 791–794. [Google Scholar] [CrossRef]
- Hollis-Hansen, K.; Haskins, C.; Turcios, J.; Bowen, M.E.; Leonard, T.; Lee, M.; Albin, J.; Wadkins-Chambers, B.; Thompson, C.; Hall, T.; et al. A pilot randomized controlled trial comparing nutritious meal kits and no-prep meals to improve food security and diet quality among food pantry clients. BMC Public Health 2023, 23, 2389. [Google Scholar] [CrossRef]
- DiMaria-Ghalili, R.A.; Laverty, N.; Baron, K.; Nasser, J.A. Benchmarking a Home-Delivered Meal Program’s Annual Satisfaction Survey: A Metropolitan Area Neighborhood Nutrition Alliance (MANNA) Initiative in Philadelphia. J. Nutr. Gerontol. Geriatr. 2015, 34, 189–206. [Google Scholar] [CrossRef]
- Gurvey, J.; Rand, K.; Daugherty, S.; Dinger, C.; Schmeling, J.; Laverty, N. Examining health care costs among MANNA clients and a comparison group. J. Prim. Care Community Health 2013, 4, 311–317. [Google Scholar] [CrossRef]
| Variable | Total (n = 40) | Temple University Hospital (n = 24) | Fox Chase Cancer Center (n = 16) | p Value |
|---|---|---|---|---|
| Age (years), mean (SD a) | 63 (13) | 66 (10) | 58 (15) | 0.05 |
| BMI (kg/m2), n (%) | 0.66 | |||
| Underweight (BMI < 18.5) | 2 (5%) | 4(16.7%) | 2 (12.5%) | |
| Normal (18.5–24.9) | 10 (25%) | 4 (16.7%) | 3 (18.7%) | |
| Overweight (25–29.9) | 13 (32.5%) | 6 (25%) | 7 (43.8%) | |
| Obese, Class I (30–34.9) | 7 (17.5%) | 5 (20.8%) | 3 (18.7%) | |
| Obese, Class II (35–39.9) | 4 (10%) | 2 (8.3%) | 1 (6.3%) | |
| Obese, Class III (≥40) | 4 (10%) | 3 (12.5%) | 0 (0%) | |
| Gender, n (%) | 0.74 | |||
| Male | 17 (42%) | 11(46%) | 6 (37.5%) | |
| Female | 23 (58%) | 13 (54%) | 10 (62.5%) | |
| Cancer Type, n (%) | 0.51 | |||
| Colorectal | 21 (53%) | 12 (50%) | 9 (56.3%) | |
| Pancreatic | 5 (12.5%) | 3 (12.5%) | 2 (12.5%) | |
| Liver | 4 (10%) | 4 (16.7%) | 0 (0%) | |
| Gastric | 3 (7.5%) | 2 (8.3%) | 1 (6.3%) | |
| Gallbladder/Biliary Tract | 3 (7.5%) | 1 (4.2%) | 2 (12.5 %) | |
| Esophageal | 2 (5%) | 1 (4.2%) | 1 (6.3%) | |
| Small Bowel | 1 (2.5%) | 0 (0%) | 1 (6.3%) | |
| Anal | 1(2.5%) | 1 (4.2%) | 0 (0%) | |
| Treatment Phase, n (%) | 0.02 | |||
| Active Treatment | 31 (77.5%) | 15 (62.5%) | 16 (100%) | |
| Post-operative | 2 (5%) | 2 (8.3%) | 0 (0%) | |
| Surveillance | 7 (17.5%) | 7 (29.2%) | 0 (0%) | |
| Stage, n (%) | 0.75 | |||
| Early | 14 (35%) | 9 (37.5%) | 5 (31%) | |
| Late | 26 (65%) | 15 (62.5%) | 11 (69%) | |
| Insurance Type, n (%) b | 0.03 | |||
| Private | 14 (35%) | 4 (16.7%) | 10 (62.5%) | |
| Medicare | 20 (50%) | 14 (58.3%) | 6 (37.5%) | |
| Medicaid | 12 (30%) | 9 (37.5%) | 3 (18.8%) | |
| Education, n (%) | 0.02 | |||
| Some High School | 14 (35%) | 12 (50%) | 2 (12.5%) | |
| High School Diploma/GED | 14 (35%) | 9 (37.5%) | 5 (31.3%) | |
| Some College or More | 12 (30%) | 3 (12.5%) | 9 (56.2%) | |
| Marital Status, n (%) | 0.22 | |||
| Single | 17 (42.5%) | 8 (33.3%) | 9 (56.2%) | |
| Married/Living with Partner | 14 (35%) | 8 (33.3%) | 6 (37.5%) | |
| Divorced | 4 (10%) | 4 (16.7%) | 0 (0%) | |
| Widowed | 5 (12.5%) | 4 (16.7%) | 1 (6.3%) | |
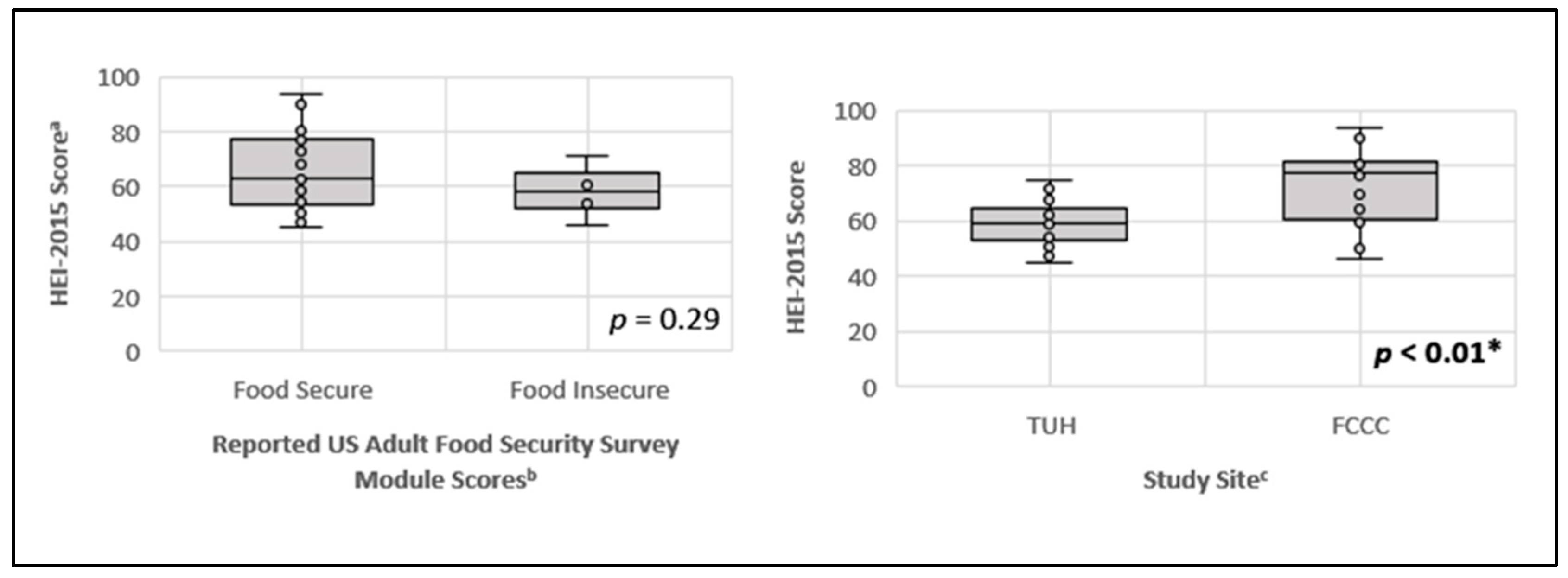
| Food Security Scores ≥ 3, total (%) c | 6 (15%) | 5 (20.8%) | 1 (6.3%) | 0.04 |
| HEI-2015 d Score, mean (SD) | 64.1 (12.6) | 57.8 (8.2) | 73.5 (14.3) | <0.01 |
| HEI-2015 a Components | Mean Component Scores-Both Sites (n = 40) | TUH c Mean Component Scores (n = 24) | FCCC d Mean Component Scores (n = 16) | p Value |
|---|---|---|---|---|
| Adequacy (increased consumption is reflected by higher scores) | ||||
| Total Fruits (5) b | 4.5 | 4.2 | 4.9 | 0.44 |
| Whole Fruits (5) | 4.6 | 4.3 | 5.0 | 0.25 |
| Total Vegetables (5) | 3.8 | 3.7 | 4.1 | 0.26 |
| Greens and Beans (5) | 3.9 | 3.6 | 4.4 | 0.07 |
| Whole Grains 10) | 3.5 | 2.5 | 5.2 | <0.01 |
| Dairy (10) | 5.6 | 5.3 | 6.1 | 0.99 |
| Total Protein Foods (5) | 4.1 | 3.9 | 4.4 | 0.75 |
| Seafood and Plant Proteins (5) | 3.7 | 3.3 | 4.4 | 0.21 |
| Fatty Acids (10) | 5.4 | 4.5 | 6.8 | 0.01 |
| Moderation (reduced consumption is reflected by higher scores) | ||||
| Refined Grains (10) | 7.8 | 7.1 | 8.8 | 0.16 |
| Sodium (10) | 4.2 | 4.1 | 4.4 | 0.76 |
| Saturated Fat (10) | 6.0 | 5.1 | 7.3 | 0.07 |
| Added Sugars (10) | 6.9 | 6.4 | 7.7 | 0.04 |
| Total Score (100) | 64.2 | 57.8 | 73.5 | 0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dratsky, D.; McGillivray, E.; Mittal, J.; Handorf, E.A.; Berardi, G.; Astsaturov, I.; Hall, M.J.; Yeh, M.-C.; Jain, R.; Fang, C.Y. Food Insecurity and Dietary Quality in African American Patients with Gastrointestinal Cancers: An Exploratory Study. Nutrients 2024, 16, 3057. https://doi.org/10.3390/nu16183057
Dratsky D, McGillivray E, Mittal J, Handorf EA, Berardi G, Astsaturov I, Hall MJ, Yeh M-C, Jain R, Fang CY. Food Insecurity and Dietary Quality in African American Patients with Gastrointestinal Cancers: An Exploratory Study. Nutrients. 2024; 16(18):3057. https://doi.org/10.3390/nu16183057
Chicago/Turabian StyleDratsky, Daaimah, Erin McGillivray, Juhi Mittal, Elizabeth A. Handorf, Giuliana Berardi, Igor Astsaturov, Michael J. Hall, Ming-Chin Yeh, Rishi Jain, and Carolyn Y. Fang. 2024. "Food Insecurity and Dietary Quality in African American Patients with Gastrointestinal Cancers: An Exploratory Study" Nutrients 16, no. 18: 3057. https://doi.org/10.3390/nu16183057
APA StyleDratsky, D., McGillivray, E., Mittal, J., Handorf, E. A., Berardi, G., Astsaturov, I., Hall, M. J., Yeh, M.-C., Jain, R., & Fang, C. Y. (2024). Food Insecurity and Dietary Quality in African American Patients with Gastrointestinal Cancers: An Exploratory Study. Nutrients, 16(18), 3057. https://doi.org/10.3390/nu16183057






