Effectiveness of DASH Diet versus Other Diet Modalities in Patients with Metabolic Syndrome: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Literature Search
2.3. Study Selection
2.4. Data Extraction and Quality Assessment
2.5. Data Synthesis and Analysis
2.6. Rating the Quality of Evidence
3. Results
3.1. Study Selection
3.2. Study Characteristics
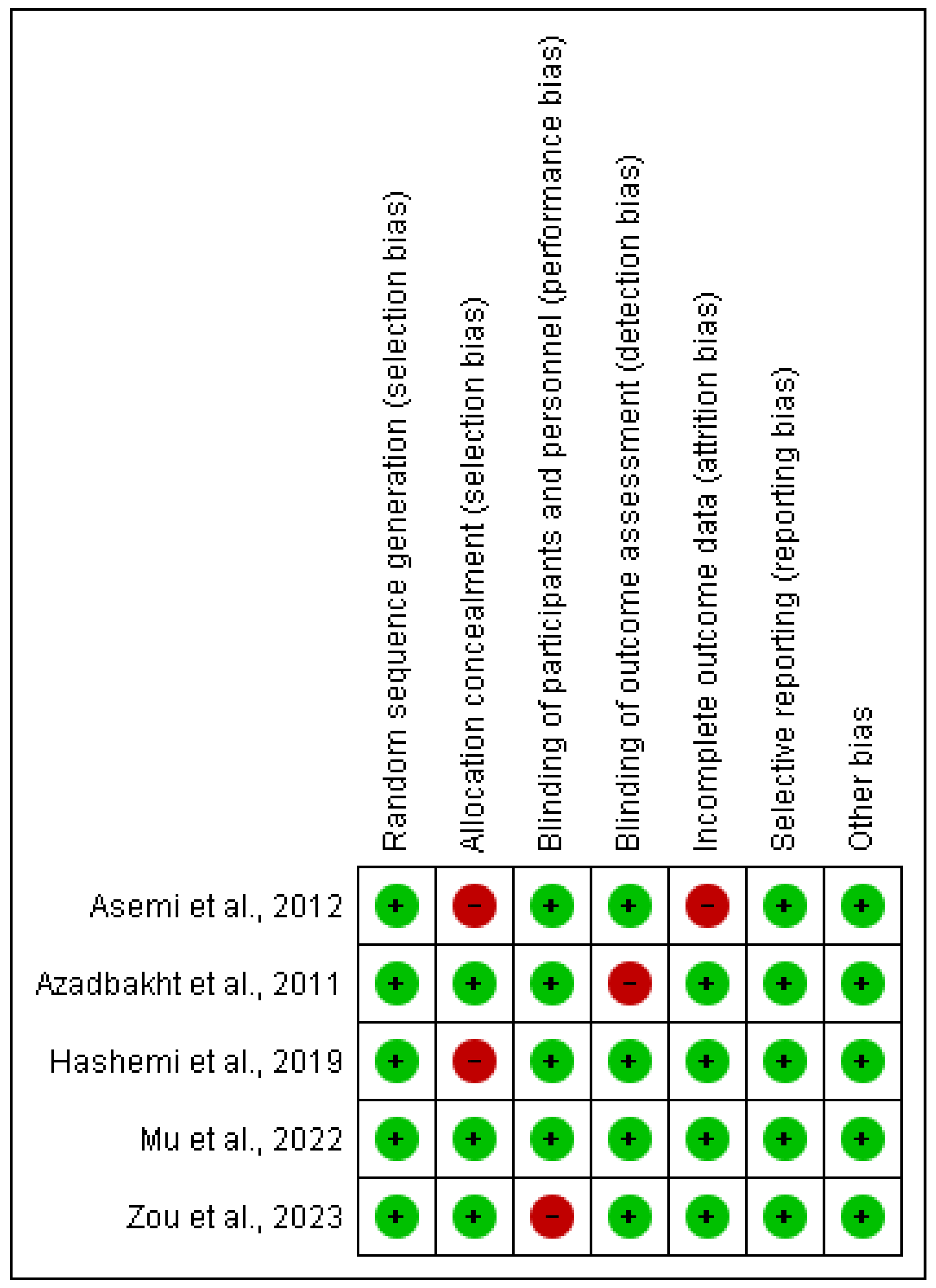
3.3. Risk of Bias Assessment in Individual Studies
3.4. Descriptive Analysis of the Included Studies
3.5. Synthesis of Results
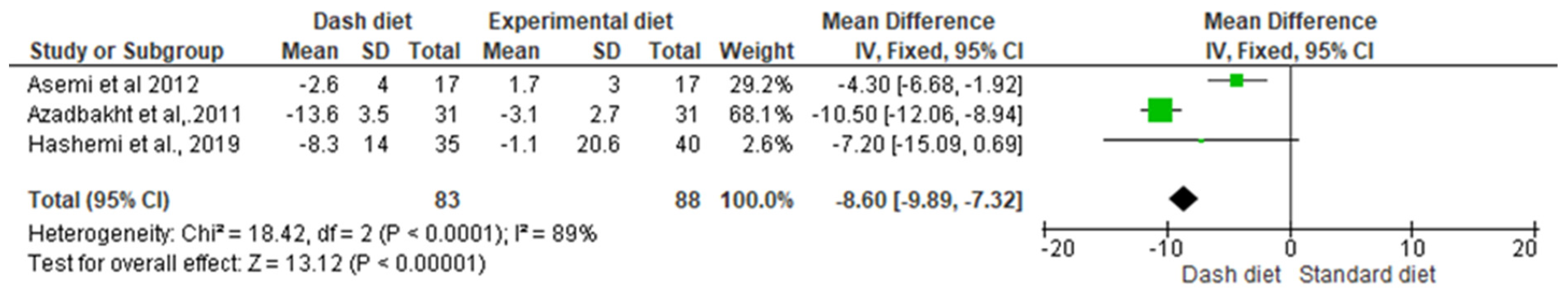
3.5.1. SBP—1 to 4 Months’ Follow-Up
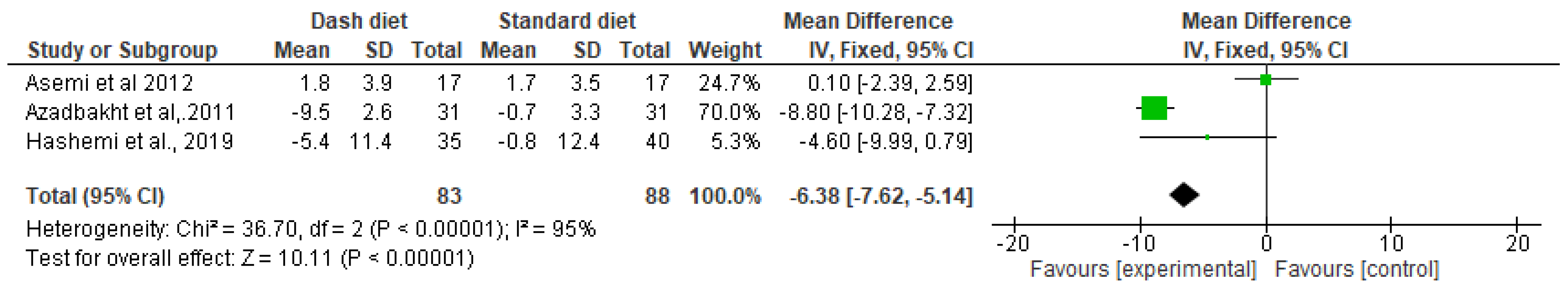
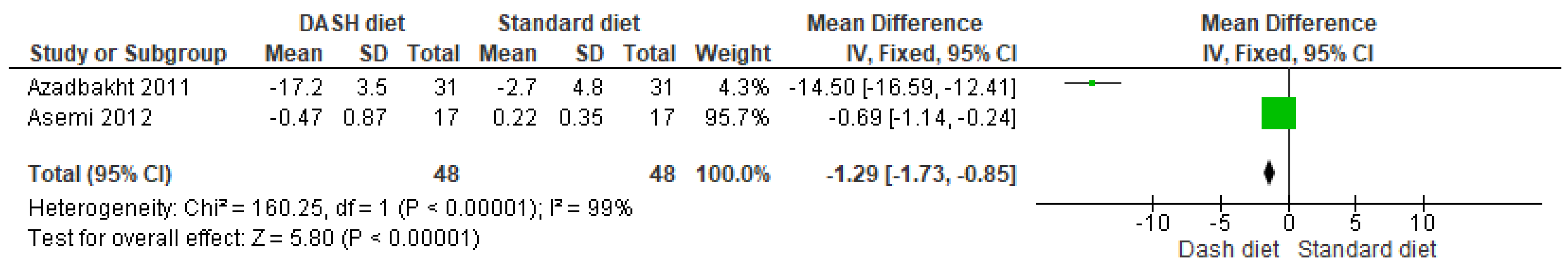
3.5.2. DBP—1 to 4 Months’ Follow-Up
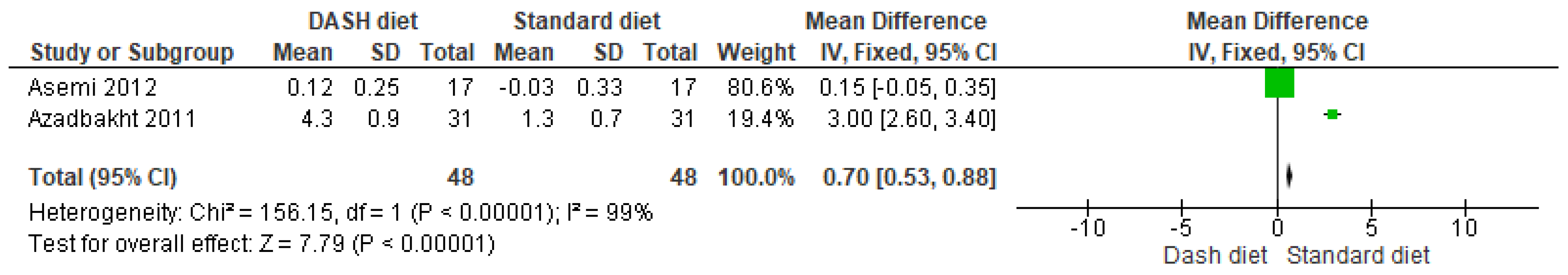
3.5.3. HDL—1 to 2 Months’ Follow-Up
3.5.4. LDL—1 to 2 Months’ Follow-Up
3.5.5. SBP SALT—8 Weeks’ Follow-Up
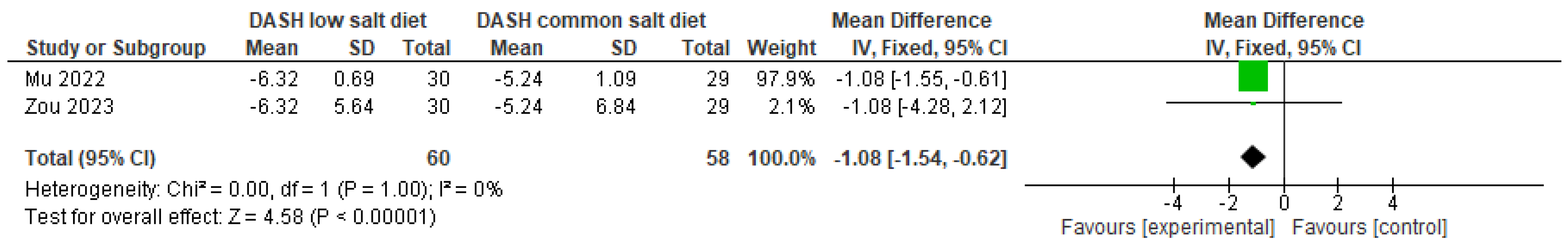
3.5.6. DBP SALT—8 Weeks’ Follow-Up
4. Discussion
Strengths and Limitations
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Hashemi, R.; Rahimlou, M.; Baghdadian, S.; Manafi, M. Investigating the effect of DASH diet on blood pressure of patients with type 2 diabetes and prehypertension: Randomized clinical trial. Diabetes Metab. Syndr. 2019, 13, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Lien, L.F.; Brown, A.J.; Ard, J.D.; Loria, C.; Erlinger, T.P.; Feldstein, A.C.; Lin, P.-H.; Champagne, C.M.; King, A.C.; McGuire, H.L.; et al. Effects of PREMIER lifestyle modifications on participants with and without the metabolic syndrome. Hypertension 2007, 50, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Paula, T.P.; Viana, L.V.; Neto, A.T.Z.; Leitão, C.B.; Gross, J.L.; Azevedo, M.J. Effects of the DASH diet and walking on blood pressure in patients with type 2 diabetes and uncontrolled hypertension: A randomized controlled trial. J. Clin. Hypertens. 2015, 17, 895–901. [Google Scholar] [CrossRef]
- Mu, L.; Zou, Y.; Tang, J.; Zhang, F.; Chen, D.; Mu, L.; Xu, H.; Yu, P.; Ren, Y.; Mei, Y. Effect of low-sodium salt applied to Chinese modified DASH diet on arterial stiffness in older patients with hypertension and type 2 diabetes. Nutr. Hosp. 2023, 40, 967–974. [Google Scholar] [CrossRef]
- Asemi, Z.; Tabassi, Z.; Samimi, M.; Fahiminejad, T.; Esmaillzadeh, A. Favourable effects of the Dietary Approaches to Stop Hypertension diet on glucose tolerance and lipid profiles in gestational diabetes: A randomised clinical trial. Br. J. Nutr. 2013, 109, 2024–2030. [Google Scholar] [CrossRef]
- Saslow, L.R.; Jones, L.M.; Sen, A.; Wolfson, J.A.; Diez, H.L.; O’brien, A.; Leung, C.W.; Bayandorian, H.; Daubenmier, J.; Missel, A.L.; et al. Comparing very low-carbohydrate vs DASH diets for overweight or obese adults with hypertension and prediabetes or type 2 diabetes: A randomized trial. Ann. Fam. Med. 2023, 21, 256–263. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Eldridge, S.; Campbell, M.K.; Campbell, M.J.; Revised Cochrane Risk of Bias Tool for Randomized Trials (RoB2). AdditionalConsiderations for Cluster-Randomized Trials (RoB 2 CRT). Available online: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials (accessed on 10 June 2024).
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef]
- Mu, L.; Mu, L.; Mu, L.; Mu, L.; Yu, P.; Yu, P.; Xu, H.; Xu, H.; Gong, T.; Gong, T.; et al. Efecto de la reducción de sodio basada en la dieta DASH sobre la presión arterial en pacientes hipertensos con diabetes tipo 2. Nutr. Hosp. 2022, 39, 537–546. [Google Scholar] [CrossRef]
- Azadbakht, L.; Fard, N.R.P.; Karimi, M.; Baghaei, M.H.; Surkan, P.J.; Rahimi, M.; Esmaillzadeh, A.; Willett, W.C. Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks Among type 2 diabetic patients. Diabetes Care 2011, 34, 55–57. [Google Scholar] [CrossRef]
- Belfort, G.P.; Padilha, P.d.C.; Farias, D.R.; da Silva, L.B.G.; dos Santos, K.; Gomes, E.d.S.; Lima, T.S.V.; Bornia, R.B.R.G.; Rezende, K.B.C.; Saunders, C. Effect of the Dietary Approaches to Stop Hypertension (DASH) diet on the development of preeclampsia and metabolic outcomes in pregnant women with pre-existing diabetes mellitus: A randomised, controlled, single-blind trial. J. Nutr. Sci. 2023, 12, e73. [Google Scholar] [CrossRef] [PubMed]
- Hikmat, F.; Appel, L.J. Effects of the DASH diet on blood pressure in patients with and without metabolic syndrome: Results from the DASH trial. J. Hum. Hypertens. 2014, 28, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Shenoy, S.F.; Poston, W.S.; Reeves, R.S.; Kazaks, A.G.; Holt, R.R.; Keen, C.L.; Chen, H.J.; Haddock, C.K.; Winters, B.L.; Khoo, C.S.H.; et al. Weight loss in individuals with metabolic syndrome given DASH diet counseling when provided a low sodium vegetable juice: A randomized controlled trial. Nutr. J. 2010, 9, 8. [Google Scholar] [CrossRef]
- Root, M.M.; Dawson, H.R. DASH-like diets high in protein or monounsaturated fats improve metabolic syndrome and calculated vascular risk. Int. J. Vitam. Nutr. Res. 2013, 83, 224–231. [Google Scholar] [CrossRef]
- Al-Solaiman, Y.; Jesri, A.; Mountford, W.K.; Lackland, D.T.; Zhao, Y.; Egan, B.M. DASH lowers blood pressure in obese hypertensives beyond potassium, magnesium and fibre. J. Hum. Hypertens. 2010, 24, 237–246. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Babyak, M.A.; Sherwood, A.; Craighead, L.; Lin, P.-H.; Johnson, J.; Watkins, L.L.; Wang, J.T.; Kuhn, C.; Feinglos, M.; et al. Effects of the Dietary Approaches to Stop Hypertension diet alone and in combination with exercise and caloric restriction on insulin sensitivity and lipids. Hypertension 2010, 55, 1199–1205. [Google Scholar] [CrossRef]
- Lari, A.; Sohouli, M.H.; Fatahi, S.; Cerqueira, H.S.; Santos, H.O.; Pourrajab, B.; Rezaei, M.; Saneie, S.; Rahideh, S.T. The effects of the Dietary Approaches to Stop Hypertension (DASH) diet on metabolic risk factors in patients with chronic disease: A systematic review and meta-analysis of randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2766–2778. [Google Scholar] [CrossRef]
- Juhász, A.E.; Stubnya, M.P.; Teutsch, B.; Gede, N.; Hegyi, P.; Nyirády, P.; Bánhidy, F.; Ács, N.; Juhász, R. Clasificación de las intervenciones dietéticas según su eficacia en el tratamiento del síndrome de ovario poliquístico: Una revisión sistemática y un metanálisis en red. Reprod. Health 2024, 21, 28. [Google Scholar] [CrossRef]
- Salehi-Abargouei, A.; Maghsoudi, Z.; Shirani, F.; Azadbakht, L. Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases—Incidence: A systematic review and meta-analysis on observational prospective studies. Nutrition 2013, 29, 611–618. [Google Scholar] [CrossRef]
- Zidek, W.; Naditch-Brûlé, L.; Perlini, S.; Farsang, C.; E Kjeldsen, S. Control de la presión arterial y componentes del síndrome metabólico: La encuesta GOOD. Cardiovasc. Diabetol. 2009, 8, 51. [Google Scholar] [CrossRef]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Said, M.S.; El Sayed, I.T.; Ibrahim, E.E.; Khafagy, G.M. Effect of DASH diet versus healthy dietary advice on the estimated atherosclerotic cardiovascular disease risk. J. Prim. Care Community Health 2021, 12, 215013272098095. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.R. Caso Clínico: Efeitos da Dieta Dietary Approaches to Stop Hypertension (Dash) No Controle Metabólico. Available online: https://expertisecia.com/wp-content/uploads/simple-file-list/TCC-ADRIANA-REIS-Final-1_1.pdf (accessed on 19 July 2024).
- Juraschek, S.P.; Miller, E.R.; Weaver, C.M.; Appel, L.J. Effects of sodium reduction and the DASH diet in relation to baseline blood pressure. J. Am. Coll. Cardiol. 2017, 70, 2841–2848. [Google Scholar] [CrossRef]
- Al-Solaiman, Y.; Jesri, A.; Zhao, Y.; Morrow, J.D.; Egan, B.M. Low-sodium DASH reduces oxidative stress and improves vascular function in salt-sensitive humans. J. Hum. 2009, 23, 826–835. [Google Scholar] [CrossRef]

| Author | Country | Population | Intervention | Outcomes | Follow-Up | Results | ||
|---|---|---|---|---|---|---|---|---|
| Sample Size (n) | Patient Mean Age (SD) | Intervention | Characteristics/Dose | |||||
| Paula et al., 2015 [3] | Brazil | CG: 20 EG: 20 | CG: 62.5 (8.8) EG: 61.8 (8.1) | CG: American diet EG: DASH Diet | CG: 4 weeks. Total daily energy, 25 to 30 kcal of body weight, 50% to 60% of energy in the form of carbohydrates, 10% to 20% in the form of protein, and 25% to 30% in the form of total fat EG: 4 weeks with advice to increase walking. Total energy, 25 to 30 kcal of body weight, 55% of energy in the form of carbohydrates, 18% in the form of protein, and 27% in the form of total fat. |
| Not follow up |
|
| Mu et al., 2022 [10] | China | CG: 29 EG: 30 | CG: 68.03 (3.82) EG: 70.00 (4.24) | CG: Modified DASH + Common salt EG: Modified DASH + Low-sodium salt | CG: 8 weeks. The amount of salt intake was controlled at 5 g/day per person. Common salt with sodium chloride content >99%. Special requirements for the modified DASH diet were the addition of brown rice, corn, soybeans, red beans, and other cereals to rice. EG: 8 weeks. The amount of salt intake was controlled at 5 g/day per person. Salt formula with 52% sodium. Special requirements for the modified DASH diet were the addition of brown rice, corn, soybeans, red beans, and other cereals to rice; eating lean meats, poultry, fish, and other meats < 120 g/day, with less red meat and more white meat. |
| Not follow up |
|
| Saslow et al., 2023 [6] | USA | CG: 23 CG + Support: 22 EG: 25 EG + Support: 24 | VLC: 60.09 (6.03) VLC + Support: 55.18 (10.48) DASH: 58.40 (8.11) DASH + Support: 60.21 (6.19) | CG: Very low carbohydrate diet. CG + Support: Very low carbohydrate diet + support with information. EG: DASH diet. EG + Support: DASH diet + support with information. | VLC: 4 months Decrease carbohydrate intake to 20 to 35 g of non-fiber carbohydrates per day. VLC + Support: 4 months Decrease carbohydrate intake to 20 to 35 g of non-fiber carbohydrates per day. DASH: 4 months Limit sodium to <2300 mg daily and fat intake to 20% to 30% of calories per day. DASH + Support: 4 months Limit sodium to < 2300 mg daily and fat intake to 20% to 30% of calories per day. Recommended consumption of a variety of fruits and vegetables, lean meats and fish, whole grains, and low-fat dairy products. | SBP HbA1c (%) Weight (lb) | No follow-up | *
|
| Belfort et al., 2023 [12] | Brazil | CG: 35 EG: 3 | No report | CG: Standard diet. EG: Adapted DASH diet. | CG: 18 weeks Oatmeal ration (250 gr), skimmed milk (1–2%, 300 gr), and extra virgin olive oil 500 mL were provided. EG: 18 weeks Provides a ration of seeds (200 gr), nuts (150 gr), skimmed milk (280 gr), and 500 mL of extra virgin olive oil. | SBP (mmHg) DBP (mmHg) LDL-cholesterol (mg/dL) HDL-cholesterol (mg/dL) Glycated hemoglobin (%) Triglycerides (mg/dL) Glutathione peroxidase (µmol/L) CRP (mg/dL) Total cholesterol (mg/dL) | No reported |
|
| Zou et al., 2023 [4] | China | CG: 29 EG: 30 | CG: 68.03 (3.82) EG: 70.00 (4.24) | CG: Common salt EG: Low- sodium salt | CG: 8 weeks standard diet EG: 8 weeks Rice: whole grain. Mainly white meat (poultry or fish). Low-fat milk. Sufficient vegetables (mainly green leafy vegetables). | SBP (mmHg) DBP (mmHg) FBG (mmol/L) PBG (mmol/L) BMI (kg/cm2) WHR (cm) | Not follow up |
|
| Hashemi et al., 2019 [1] | Iran | CG: 40 EG: 35 | CG: <50 EG: <50 | CG: Control group diet EG: DASH diet | CG: 12 weeks 18% protein, 52% carbohydrates, 30% fat. EG: 12 weeks 8 to 10 daily servings of fruits and vegetables; 4 to 5 weekly servings of nuts, seeds or beans. | SBP (mmHg) DBP (mmHg) | No follow-up |
|
| Hikmat et al., 2013 [13] | USA | CG: 133 EG: 138 AG: 140 | CG: 45.4 (11.4) EG: 44.5 (10.5) AG: 48.4 (11) | CG: Protein, Carbohydrates, Fat Diet EG: DASH Diet | CG: Protein, carbohydrate, and fat diet. EG: DASH diet: 12 weeks. 8 to 10 daily servings of fruits and vegetables; 4 to 5 weekly servings of nuts, seeds, or beans. At least six daily servings from a grain group (half of them should be whole grains). | BMI BP TG HDL SBP DBP | No follow-up |
|
| Azadbakht et al., 2011 [11] | Iran | CG: 31 EG:31 | CG:Not reported EG:Not reported | CG: Protein, carbohydrate and fat EG: Dieta DASH | CG: Control diet: 8 weeks 50 to 60% carbohydrates; 15 to 20% protein; 30% total fat; 5% of caloric intake comes from simple sugars. EG: DASH diet: 8 weeks Rich in fruits, vegetables, whole grains, and low-fat dairy products and low in saturated fat, total fat, cholesterol, refined grains, and sweets. Amount of sodium consumed was 2400 mg per day | SBP (mmHg) DBP (mmHg) FBG (mg/dL) A1C (%) TG (mg/dL) HDL-C (mg/dL) LDL-C (mg/dL) | No follow-up |
|
| Shenoy et al., 2010 [14] | USA | CG: 27 EG: 27 AG: 27 | CG: 50.1 (5.1) EG: 51.2 (7.4) AG: 48.0 (7.7) | CG: not reported EG: DASH Diet and Vegetable Juice 8 oz AG: DASH Diet and Vegetable Juice 16 oz | CG: not reported EG: DASH diet without vegetable juice: 12 weeks. Men 1800 Kcal diet, and women 1600 Kcal. EG: DASH diet of 8 fluid ounces of low-sodium vegetable juice per day: 12 weeks. Men 1800 Kcal diet, and women 1600 Kcal. EG: DASH diet of 16 fluid ounces of low-sodium vegetable juice per day: 12 weeks. Men 1800 kcal diet and women 1600 kcal diet. | HDL: (mg/dL; %) Blood Glucose: (mg/dL; %) BMI: (KG) SBP: (mmHg) DBP: (mmHg) TG: (mg/dL; %) | No follow-up |
|
| Lien et al., 2007 [2] | USA | CG: 397 EG: 399 | CG: 49.9 (9.0) EG:49.7 (8.6) | CG: DASH diet with metabolic syndrome EG: DASH diet | CG: Not reported Group receiving the intervention plus the DASH dietary pattern. EG: Group receiving an intensive behavioral intervention based on established lifestyle modifications to lower blood pressure and receiving the intervention plus the DASH dietary pattern. | TG (mg/dL) SBP (mmHg) DBP (mmHg) LDL-C (mg/dL) HDL-C (mg/dL) FG (mmol/L) FI (micro-IU/mL) HOMA | No follow-up |
|
| Asemi et al., 2012 [5] | Iran | CG:17 EG:17 | CG: 29.4 (6.2) EG: 30.7 (6.7) | CG: Standard Diet EG: DASH Diet | CG: No reported EG: No reported | BMI (kg/m2) HDL (mmol/L) LDL (mmol/L) SBP (mmHg) DBP (mmHg) GTT (mmol/L) | No follow-up |
|
| Root et al., 2013 [15] | USA | CG: Not reported EG:Not reported AG:Not reported AG:Not reported | CG:Not reported EG: 30≥ AG: 30≥ AG: 30≥ | CG: Not reported EG: High-carbohydrate DASH-like diet AG: High-protein DASH-like diet AG: High-unsaturated fat DASH-like diet | CG: Not reported EG: High-carbohydrate DASH-like diet 6 weeks. Diet based on 58% carbohydrates, 15% protein, and 27% fat. 5.5% plant-based protein, 13% monounsaturated fats, and 8% polyunsaturated fats. | Glucose (mmol/L) HDL-C (mmol/L) TG (mmol/L) SBP (mmHg) | 5 years | Glucose:
|
| Al-Solaiman et al., 2010 [16] | USA | CG: 30 EG: 30 | CG: Not reported. EG: Not reported. | CG: ULFV-S EG: DASH | CG: Diet with an average of one fruit and one vegetable (ULFV), ∼1700 mg potassium, 250 mg magnesium, and 11 g of fiber daily; supplemented with potassium, magnesium, and fiber (ULFV-S) to match DASH, or DASH itself. EG: ∼50% carbohydrate, 35% fat, and 15% protein with 3000 mg sodium and 700 mg calcium daily. | Not reported | No follow-up | Not reported |
| Blumental et al., 2010 [17] | USA | CG: 49 EG: 46 AG: 49 | CG: 52.0 (10) EG: 51.8 (10) AG: 52.3 (10) | CG: UC EG: DASH-A AG: DASH-WM | CG: Regular diet: 4 weeks with the cases, 2 weeks with controls; the following weeks, only an indication to follow the diet was given: isocaloric diet to maintain weight proteins 16.5%, saturated fat 36.8%, fiber 16 G EG: DASH diet alone 4 weeks with the cases, 2 weeks with controls; the following weeks, only an indication to follow the diet was given: isocaloric diet to maintain weight proteins 19.4%, saturated fat 27.8%, fiber 26% | FG (mg/dL) FI (μU/mL) Glucosa AUC (mg/dl·minutes) TG (mg/dL) Total Cholesterol (mg/dL) Low-Density Lipoprotein-Cholesterol (mg/dL) High-Density Lipoprotein-Cholesterol (mg/dL) | 4 months | FG:
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valenzuela-Fuenzalida, J.J.; Bravo, V.S.; Valarezo, L.M.; Delgado Retamal, M.F.; Leiva, J.M.; Bruna-Mejías, A.; Nova-Baeza, P.; Orellana-Donoso, M.; Suazo-Santibañez, A.; Oyanedel-Amaro, G.; et al. Effectiveness of DASH Diet versus Other Diet Modalities in Patients with Metabolic Syndrome: A Systematic Review and Meta-Analysis. Nutrients 2024, 16, 3054. https://doi.org/10.3390/nu16183054
Valenzuela-Fuenzalida JJ, Bravo VS, Valarezo LM, Delgado Retamal MF, Leiva JM, Bruna-Mejías A, Nova-Baeza P, Orellana-Donoso M, Suazo-Santibañez A, Oyanedel-Amaro G, et al. Effectiveness of DASH Diet versus Other Diet Modalities in Patients with Metabolic Syndrome: A Systematic Review and Meta-Analysis. Nutrients. 2024; 16(18):3054. https://doi.org/10.3390/nu16183054
Chicago/Turabian StyleValenzuela-Fuenzalida, Juan José, Vicente Silva Bravo, Laura Moyano Valarezo, María Fernanda Delgado Retamal, Josefa Matta Leiva, Alejandro Bruna-Mejías, Pablo Nova-Baeza, Mathias Orellana-Donoso, Alejandra Suazo-Santibañez, Gustavo Oyanedel-Amaro, and et al. 2024. "Effectiveness of DASH Diet versus Other Diet Modalities in Patients with Metabolic Syndrome: A Systematic Review and Meta-Analysis" Nutrients 16, no. 18: 3054. https://doi.org/10.3390/nu16183054
APA StyleValenzuela-Fuenzalida, J. J., Bravo, V. S., Valarezo, L. M., Delgado Retamal, M. F., Leiva, J. M., Bruna-Mejías, A., Nova-Baeza, P., Orellana-Donoso, M., Suazo-Santibañez, A., Oyanedel-Amaro, G., & Gutierrez-Espinoza, H. (2024). Effectiveness of DASH Diet versus Other Diet Modalities in Patients with Metabolic Syndrome: A Systematic Review and Meta-Analysis. Nutrients, 16(18), 3054. https://doi.org/10.3390/nu16183054