Assessing the Hypertension Risk: A Deep Dive into Cereal Consumption and Cooking Methods—Insights from China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Assessment of Hypertension
2.3. Assessment of Cereal Consumption
2.4. Assessment of Covariates
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Participants
3.2. Cereal Consumption and Risk of Hypertension
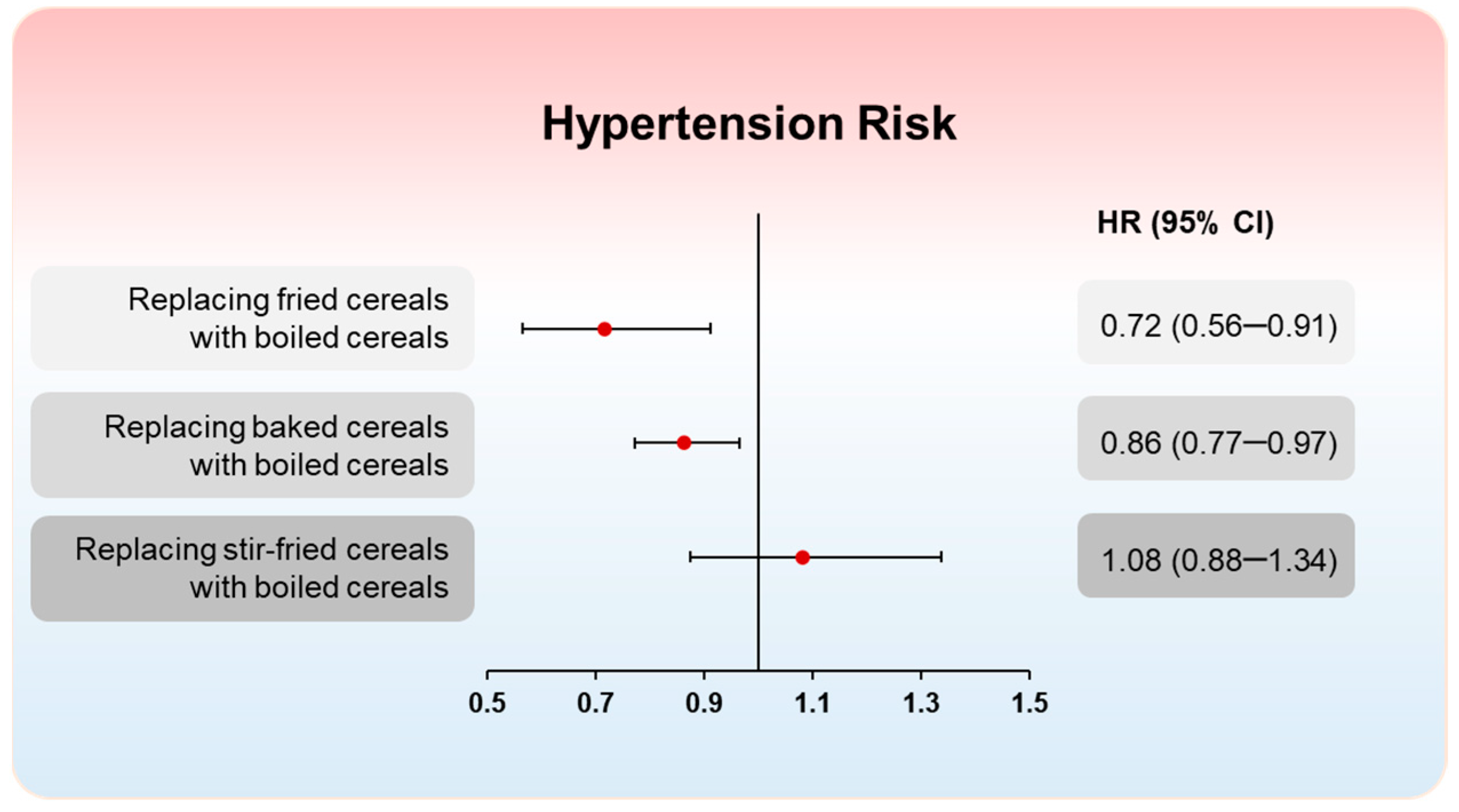
3.3. Substitution Analysis
3.4. Subgroup and Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Campos, H. Dietary Therapy in Hypertension. N. Engl. J. Med. 2010, 362, 2102–2112. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Qi, Y.; Zheng, Z.; Wang, Y.; Zhang, X.-Y.; Li, H.-J.; Liu, H.-H.; Zhang, X.-T.; Du, J.; Liu, J. Dietary factors associated with hypertension. Nat. Rev. Cardiol. 2011, 8, 456–465. [Google Scholar] [CrossRef] [PubMed]
- Nissensohn, M.; Roman-Vinas, B.; Sanchez-Villegas, A.; Piscopo, S.; Serra-Majem, L. The Effect of the Mediterranean Diet on Hypertension: A Systematic Review and Meta-Analysis. J. Nutr. Educ. Behav. 2016, 48, 42–53. [Google Scholar] [CrossRef]
- Jennings, A.; Berendsen, A.M.; de Groot, L.C.P.G.M.; Feskens, E.J.M.; Brzozowska, A.; Sicinska, E.; Pietruszka, B.; Meunier, N.; Caumon, E.; Malpuech-Brugere, C.; et al. Mediterranean-Style Diet Improves Systolic Blood Pressure and Arterial Stiffness in Older Adults Results of a 1-Year European Multi-Center Trial. Hypertension 2019, 73, 578–586. [Google Scholar] [CrossRef]
- Saneei, P.; Salehi-Abargouei, A.; Esmaillzadeh, A.; Azadbakht, L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: A systematic review and meta-analysis on randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 1253–1261. [Google Scholar] [CrossRef]
- Couch, S.C.; Saelens, B.E.; Khoury, P.R.; Dart, K.B.; Hinn, K.; Mitsnefes, M.M.; Daniels, S.R.; Urbina, E.M. Dietary Approaches to Stop Hypertension Dietary Intervention Improves Blood Pressure and Vascular Health in Youth With Elevated Blood Pressure. Hypertension 2021, 77, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Zafarmand, M.H.; Spanjer, M.; Nicolaou, M.; Wijnhoven, H.A.H.; van Schaik, B.D.C.; Uitterlinden, A.G.; Snieder, H.; Vrijkotte, T.G.M. Influence of Dietary Approaches to Stop Hypertension-Type Diet, Known Genetic Variants and Their Interplay on Blood Pressure in Early Childhood ABCD Study. Hypertension 2020, 75, 59–70. [Google Scholar] [CrossRef]
- Borg, J.; Kiær, L.P.; Lecarpentier, C.; Goldringer, I.; Gauffreteau, A.; Saint-Jean, S.; Barot, S.; Enjalbert, J. Unfolding the potential of wheat cultivar mixtures: A meta-analysis perspective and identification of knowledge gaps. Field Crop. Res. 2018, 221, 298–313. [Google Scholar] [CrossRef]
- Huang, L.; Wang, H.; Wang, Z.; Zhang, J.; Zhang, B.; Ding, G. Regional Disparities in the Association between Cereal Consumption and Metabolic Syndrome: Results from the China Health and Nutrition Survey. Nutrients 2019, 11, 764. [Google Scholar] [CrossRef]
- Chinese Nutrition Society. The Chinese Dietary Guidelines (2022); People’s Medical Publishing House: Beijing, China, 2022; pp. 93–304. [Google Scholar]
- Tighe, P.; Duthie, G.; Vaughan, N.; Brittenden, J.; Simpson, W.G.; Duthie, S.; Mutch, W.; Wahle, K.; Horgan, G.; Thies, F. Effect of increased consumption of whole-grain foods on blood pressure and other cardiovascular risk markers in healthy middle-aged persons: A randomized controlled trial. Am. J. Clin. Nutr. 2010, 92, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Kirwan, J.P.; Malin, S.K.; Scelsi, A.R.; Kullman, E.L.; Navaneethan, S.D.; Pagadala, M.R.; Haus, J.M.; Filion, J.; Godin, J.P.; Kochhar, S.; et al. A Whole-Grain Diet Reduces Cardiovascular Risk Factors in Overweight and Obese Adults: A Randomized Controlled Trial. J. Nutr. 2016, 146, 2244–2251. [Google Scholar] [CrossRef]
- Millen, B.E.; Abrams, S.; Adams-Campbell, L.; Anderson, C.A.M.; Brenna, J.T.; Campbell, W.W.; Clinton, S.; Hu, F.; Nelson, M.; Neuhouser, M.L.; et al. The 2015 Dietary Guidelines Advisory Committee Scientific Report: Development and Major Conclusions. Adv. Nutr. 2016, 7, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Knüppel, S.; Iqbal, K.; Andriolo, V.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food Groups and Risk of Hypertension: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2017, 8, 793–803. [Google Scholar] [CrossRef] [PubMed]
- Miglio, C.; Chiavaro, E.; Visconti, A.; Fogliano, V.; Pellegrini, N. Effects of different cooking methods on nutritional and physicochemical characteristics of selected vegetables. J. Agric. Food Chem. 2008, 56, 139–147. [Google Scholar] [CrossRef]
- Feng, X.; Yonghua, Z.; Zhenfeng, Y.; Shifeng, C.; Xingfeng, S.; Hongfei, W. Domestic cooking methods affect the nutritional quality of red cabbage. Food Chem. 2014, 161, 162–167. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Hao, T.; Rimm, E.B.; Willett, W.C.; Hu, F.B. Changes in diet and lifestyle and long-term weight gain in women and men. N. Engl. J. Med. 2011, 364, 2392–2404. [Google Scholar] [CrossRef]
- Zhang, B.; Zhai, F.Y.; Du, S.F.; Popkin, B.M. The China Health and Nutrition Survey, 1989-2011. Obes. Rev. 2014, 15, 2–7. [Google Scholar] [CrossRef]
- China Health and Nutrition Survey (CHNS). Available online: http://www.cpc.unc.edu/projects/china/ (accessed on 15 January 2024).
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T.; et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef]
- Du, S.; Neiman, A.; Batis, C.; Wang, H.; Zhang, B.; Zhang, J.; Popkin, B.M. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am. J. Clin. Nutr. 2014, 99, 334–343. [Google Scholar] [CrossRef]
- Batis, C.; Sotres-Alvarez, D.; Gordon-Larsen, P.; Mendez, M.A.; Adair, L.; Popkin, B. Longitudinal analysis of dietary patterns in Chinese adults from 1991 to 2009. Br. J. Nutr. 2014, 111, 1441–1451. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Zhang, Z.; Liu, M.; Zhang, Y.; Li, H.; He, P.; Li, Q.; Liu, C.; Qin, X. Dietary carbohydrate intake and new-onset diabetes: A nationwide cohort study in China. Metab. Clin. Exp. 2021, 123, 154865. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, D.C.; Hardie, L.J.; Frost, G.S.; Alwan, N.A.; Bradbury, K.E.; Carter, M.; Elliott, P.; Evans, C.E.L.; Ford, H.E.; Hancock, N.; et al. Validation of the Oxford WebQ Online 24-Hour Dietary Questionnaire Using Biomarkers. Am. J. Epidemiol. 2019, 188, 1858–1867. [Google Scholar] [CrossRef]
- McCullough, M.L.; Feskanich, D.; Stampfer, M.J.; Giovannucci, E.L.; Rimm, E.B.; Hu, F.B.; Spiegelman, D.; Hunter, D.J.; Colditz, G.A.; Willett, W.C. Diet quality and major chronic disease risk in men and women: Moving toward improved dietary guidance. Am. J. Clin. Nutr. 2002, 76, 1261–1271. [Google Scholar] [CrossRef]
- Chiuve, S.E.; Fung, T.T.; Rimm, E.B.; Hu, F.B.; McCullough, M.L.; Wang, M.; Stampfer, M.J.; Willett, W.C. Alternative dietary indices both strongly predict risk of chronic disease. J. Nutr. 2012, 142, 1009–1018. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C. Food frequency methods; Reproducibility and validity of food-frequency questionnaires; Implications of total energy intake for epidemiologic analyses. In Nutritional Epidemiology, 3rd ed.; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Huang, M.; Zhuang, P.; Jiao, J.; Wang, J.; Chen, X.; Zhang, Y. Potato consumption is prospectively associated with risk of hypertension: An 11.3-year longitudinal cohort study. Clin. Nutr. 2019, 38, 1936–1944. [Google Scholar] [CrossRef] [PubMed]
- Borgi, L.; Rimm, E.B.; Willett, W.C.; Forman, J.P. Potato intake and incidence of hypertension: Results from three prospective US cohort studies. BMJ-Br. Med. J. 2016, 353, i2351. [Google Scholar] [CrossRef]
- Hu, F.B. Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2013, 14, 606–619. [Google Scholar] [CrossRef]
- Qin, P.; Li, Q.; Zhao, Y.; Chen, Q.; Sun, X.; Liu, Y.; Li, H.; Wang, T.; Chen, X.; Zhou, Q.; et al. Sugar and artificially sweetened beverages and risk of obesity, type 2 diabetes mellitus, hypertension, and all-cause mortality: A dose-response meta-analysis of prospective cohort studies. Eur. J. Epidemiol. 2020, 35, 655–671. [Google Scholar] [CrossRef]
- Alonso, A.; Beunza, J.J.; Bes-Rastrollo, M.; Pajares, R.M.; Martínez-González, M.Á. Vegetable Protein and Fiber from Cereal Are Inversely Associated with the Risk of Hypertension in a Spanish Cohort. Arch. Med. Res. 2006, 37, 778–786. [Google Scholar] [CrossRef]
- Garcia-Castro, A.; Delia Roman-Gutierrez, A.; Castaneda-Ovando, A.; Carino-Cortes, R.; Arturo Acevedo-Sandoval, O.; Lopez-Perea, P.; Araceli Guzman-Ortiz, F. Cereals as a Source of Bioactive Compounds with Anti-Hypertensive Activity and Their Intake in Times of COVID-19. Foods 2022, 11, 3231. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.A. Anti-hypertensive Effect of Cereal Antioxidant Ferulic Acid and Its Mechanism of Action. Front. Nutr. 2019, 7, 121. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Shu, X.O.; Li, H.; Xiang, Y.B.; Yang, G.; Gao, Y.T.; Zheng, W.; Zhang, X. Dietary carbohydrates, refined grains, glycemic load, and risk of coronary heart disease in Chinese adults. Am. J. Epidemiol. 2013, 178, 1542–1549. [Google Scholar] [CrossRef] [PubMed]
- Musa-Veloso, K.; Poon, T.; Harkness, L.S.; O’Shea, M.; Chu, Y. The effects of whole-grain compared with refined wheat, rice, and rye on the postprandial blood glucose response: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2018, 108, 759–774. [Google Scholar] [CrossRef]
- Evans, C.E.L.; Greenwood, D.C.; Threapleton, D.E.; Gale, C.P.; Cleghorn, C.L.; Burley, V.J. Glycemic index, glycemic load, and blood pressure: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2017, 105, 1176–1190. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, B.; Flood, V.M.; Rochtchina, E.; Baur, L.A.; Smith, W.; Mitchell, P. Influence of High Glycemic Index and Glycemic Load Diets on Blood Pressure During Adolescence. Hypertension 2012, 59, 1272–1277. [Google Scholar] [CrossRef]
- Ludwig, D.S. The glycemic index: Physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA 2002, 287, 2414–2423. [Google Scholar] [CrossRef]
- Atkinson, F.S.; Brand-Miller, J.C.; Foster-Powell, K.; Buyken, A.E.; Goletzke, J. International tables of glycemic index and glycemic load values 2021: A systematic review. Am. J. Clin. Nutr. 2021, 114, 1625–1632. [Google Scholar] [CrossRef]
- Sarafidis, P.A.; Bakris, G.L. The antinatriuretic effect of insulin: An unappreciated mechanism for hypertension associated with insulin resistance? Am. J. Nephrol. 2007, 27, 44–54. [Google Scholar] [CrossRef]
- Wolever, T.M.; Gibbs, A.L.; Mehling, C.; Chiasson, J.L.; Connelly, P.W.; Josse, R.G.; Leiter, L.A.; Maheux, P.; Rabasa-Lhoret, R.; Rodger, N.W.; et al. The Canadian Trial of Carbohydrates in Diabetes (CCD), a 1-y controlled trial of low-glycemic-index dietary carbohydrate in type 2 diabetes: No effect on glycated hemoglobin but reduction in C-reactive protein. Am. J. Clin. Nutr. 2008, 87, 114–125. [Google Scholar] [CrossRef]
- Hu, E.A.; Pan, A.; Malik, V.; Sun, Q. White rice consumption and risk of type 2 diabetes: Meta-analysis and systematic review. BMJ 2012, 344, e1454. [Google Scholar] [CrossRef]
- Thathola, A.; Srivastava, S.; Singh, G. Effect of foxtail millet (setaria italica) supplementation on serum glucose, serum lipids and glycosylated hemoglobin in type 2 diabetics. Diabetol. Croat. 2011, 40, 23–29. [Google Scholar]
- Hou, D.; Chen, J.; Ren, X.; Wang, C.; Diao, X.; Hu, X.; Zhang, Y.; Shen, Q. A whole foxtail millet diet reduces blood pressure in subjects with mild hypertension. J. Cereal Sci. 2018, 84, 13–19. [Google Scholar] [CrossRef]
- Bouchard, J.; Valookaran, A.F.; Aloud, B.M.; Raj, P.; Malunga, L.N.; Thandapilly, S.J.; Netticadan, T. Impact of oats in the prevention/management of hypertension. Food Chem. 2022, 381, 132198. [Google Scholar] [CrossRef]
- Xue, Y.; Cui, L.; Qi, J.; Ojo, O.; Du, X.; Liu, Y.; Wang, X. The effect of dietary fiber (oat bran) supplement on blood pressure in patients with essential hypertension: A randomized controlled trial. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2458–2470. [Google Scholar] [CrossRef] [PubMed]
- Ascherio, A.; Hennekens, C.; Willett, W.C.; Sacks, F.; Rosner, B.; Manson, J.; Witteman, J.; Stampfer, M.J. Prospective study of nutritional factors, blood pressure, and hypertension among US women. Hypertension 1996, 27, 1065–1072. [Google Scholar] [CrossRef]
- Esmaillzadeh, A.; Mirmiran, P.; Azizi, F. Whole-grain consumption and the metabolic syndrome: A favorable association in Tehranian adults. Eur. J. Clin. Nutr. 2005, 59, 353–362. [Google Scholar] [CrossRef]
- Gaesser, G.A. Perspective: Refined Grains and Health: Genuine Risk, or Guilt by Association? Adv. Nutr. 2019, 10, 361–371. [Google Scholar] [CrossRef]
- Seal, C.J. Whole grains and CVD risk. Proc. Nutr. Soc. 2006, 65, 24–34. [Google Scholar] [CrossRef]
- Liu, X.; Lai, H.; Mi, B.; Qi, X.; Gan, W.; Du, H. Associations of Coarse Grain Intake with Undiagnosed Hypertension among Chinese Adults: Results from the China Kadoorie Biobank. Nutrients 2020, 12, 3814. [Google Scholar] [CrossRef]
- Kashino, I.; Eguchi, M.; Miki, T.; Kochi, T.; Nanri, A.; Kabe, I.; Mizoue, T. Prospective Association between Whole Grain Consumption and Hypertension: The Furukawa Nutrition and Health Study. Nutrients 2020, 12, 902. [Google Scholar] [CrossRef]
- Lelong, H.; Blacher, J.; Baudry, J.; Adriouch, S.; Galan, P.; Fezeu, L.; Hercberg, S.; Kesse-Guyot, E. Individual and Combined Effects of Dietary Factors on Risk of Incident Hypertension Prospective Analysis From the NutriNet-Sante Cohort. Hypertension 2017, 70, 712–720. [Google Scholar] [CrossRef]
- Vernay, M.; Aidara, M.; Salanave, B.; Deschamps, V.; Malon, A.; Oleko, A.; Mallion, J.-M.; Hercberg, S.; Castetbon, K. Diet and blood pressure in 18-74-year-old adults: The French Nutrition and Health Survey (ENNS, 2006–2007). J. Hypertens. 2012, 30, 1920–1927. [Google Scholar] [CrossRef] [PubMed]
- Ampatzoglou, A.; Atwal, K.K.; Maidens, C.M.; Williams, C.L.; Ross, A.B.; Thielecke, F.; Jonnalagadda, S.S.; Kennedy, O.B.; Yaqoob, P. Increased Whole Grain Consumption Does Not Affect Blood Biochemistry, Body Composition, or Gut Microbiology in Healthy, Low-Habitual Whole Grain Consumers. J. Nutr. 2015, 145, 215–221. [Google Scholar] [CrossRef]
- Li, S.; Zhu, Y.; Chavarro, J.E.; Bao, W.; Tobias, D.K.; Ley, S.H.; Forman, J.P.; Liu, A.; Mills, J.; Bowers, K.; et al. Healthful Dietary Patterns and the Risk of Hypertension Among Women With a History of Gestational Diabetes Mellitus A Prospective Cohort Study. Hypertension 2016, 67, 1157–1165. [Google Scholar] [CrossRef]
- Onyango, E.M.; Onyango, B.M. The Rise of Noncommunicable Diseases in Kenya: An Examination of the Time Trends and Contribution of the Changes in Diet and Physical Inactivity. J. Epidemiol. Glob. health 2018, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Björck, I.; Östman, E.; Kristensen, M.; Mateo Anson, N.; Price, R.K.; Haenen, G.R.M.M.; Havenaar, R.; Bach Knudsen, K.E.; Frid, A.; Mykkänen, H.; et al. Cereal grains for nutrition and health benefits: Overview of results from in vitro, animal and human studies in the HEALTHGRAIN project. Trends Food Sci. Technol. 2012, 25, 87–100. [Google Scholar] [CrossRef]
- De Pilli, T.; Alessandrino, O. Effects of different cooking technologies on biopolymers modifications of cereal-based foods: Impact on nutritional and quality characteristics review. Crit. Rev. Food Sci. Nutr. 2020, 60, 556–565. [Google Scholar] [CrossRef] [PubMed]
- Persson, E.; Sjöholm, I.; Nyman, M.; Skog, K. Addition of various carbohydrates to beef burgers affects the formation of heterocyclic amines during frying. J. Agric. Food Chem. 2004, 52, 7561–7566. [Google Scholar] [CrossRef]
- Boekel, M.v.; Fogliano, V.; Pellegrini, N.; Stanton, C.; Scholz, G.; Lalljie, S.; Somoza, V.; Knorr, D.; Rao Jasti, P.; Eisenbrand, G. A review on the beneficial aspects of food processing. Mol. Nutr. Food Res. 2010, 54, 1215–1247. [Google Scholar] [CrossRef]
- Bhardwaj, S.; Passi, S.J.; Misra, A. Overview of trans fatty acids: Biochemistry and health effects. Diabetes Metab. Syndr. 2011, 5, 161–164. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Mozaffarian, D. Trans fatty acids: Effects on cardiometabolic health and implications for policy. Prostaglandins Leukot. Essent. Fat. Acids 2008, 79, 147–152. [Google Scholar] [CrossRef]
- Brownell, K.D.; Pomeranz, J.L. The Trans-Fat Ban-Food Regulation and Long-Term Health. N. Engl. J. Med. 2014, 370, 1773–1775. [Google Scholar] [CrossRef]
- Tamanna, N.; Mahmood, N. Food Processing and Maillard Reaction Products: Effect on Human Health and Nutrition. Int. J. Food Sci. 2015, 2015, 526762. [Google Scholar] [CrossRef]
- Soriguer, F.; Rojo-Martínez, G.; Dobarganes, M.C.; García Almeida, J.M.; Esteva, I.; Beltrán, M.; Ruiz De Adana, M.S.; Tinahones, F.; Gómez-Zumaquero, J.M.; García-Fuentes, E.; et al. Hypertension is related to the degradation of dietary frying oils. Am. J. Clin. Nutr. 2003, 78, 1092–1097. [Google Scholar] [CrossRef]
- Hill, D.; Conner, M.; Clancy, F.; Moss, R.; Wilding, S.; Bristow, M.; O’Connor, D.B. Stress and eating behaviours in healthy adults: A systematic review and meta-analysis. Health psychol. Rev. 2022, 16, 280–304. [Google Scholar] [CrossRef] [PubMed]
- Coppi, F.; Nasi, M.; Farinetti, A.; Manenti, A.; Gallina, S.; Mattioli, A.V. Physical activity, sedentary behaviour, and diet in menopausal women: Comparison between COVID19 “first wave” and “second wave” of pandemic in Italy. Prog. Nutr. 2021, 23, 1–9. [Google Scholar] [CrossRef]
- van der Linde, N.A.J.; Sijbrands, E.J.G.; Boomsma, F.; van den Meiracker, A.H. Effect of low-density lipoprotein cholesterol on angiotensin II sensitivity-A Randomized trial with fluvastatin. Hypertension 2006, 47, 1125–1130. [Google Scholar] [CrossRef] [PubMed]
- Alpert, M.A.; Govindarajan, G.; Del Rosario, M.L.E.; Reisin, E. The role of the renin-angiotensin system in the pathophysiology, prevention, and treatment of renal impairment in patients with the cardiometabolic syndrome or its components. J. Cardiometabolic Syndr. 2009, 4, 57–62. [Google Scholar] [CrossRef]
- Wang, L.; Manson, J.E.; Forman, J.P.; Gaziano, J.M.; Buring, J.E.; Sesso, H.D. Dietary Fatty Acids and the Risk of Hypertension in Middle-Aged and Older Women. Hypertension 2010, 56, 598–604. [Google Scholar] [CrossRef]
- Arici, M.; Turgan, C.; Altun, B.; Sindel, S.; Erbay, B.; Derici, U.; Karatan, O.; Erdem, Y.; Hasanoglu, E.; Caglar, S.; et al. Hypertension incidence in Turkey (HinT): A population-based study. J. Hypertens. 2010, 28, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Akpolat, T.; Kadi, R.; Utaş, C. Hypertension, salt, and bread. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2009, 53, 1103. [Google Scholar] [CrossRef] [PubMed]
- Yuan, G.-f.; Sun, B.; Yuan, J.; Wang, Q.-M. Effects of different cooking methods on health-promoting compounds of broccoli. J. Zhejiang Univ. Sci. B 2009, 10, 580–588. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Chen, J.; Ye, X.; Chen, S. Health benefits of the potato affected by domestic cooking: A review. Food Chem. 2016, 202, 165–175. [Google Scholar] [CrossRef]

| Characteristics | Dietary Cereal Intake (g/2000 kcal/day) | |||
|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |
| N | 2770 | 2770 | 2770 | 2770 |
| Age (years) | 41.7 ± 0.3 | 40.7 ± 0.3 | 39.8 ± 0.2 | 39.9 ± 0.2 |
| Body mass index (kg/m2) | 22.7 ± 0.1 | 22.5 ± 0.1 | 22.3 ± 0.1 | 22.4 ± 0.1 |
| Household income (CNY/yr) † | 42,041.1 ± 960.2 | 29,604.7 ± 712.1 | 24,881.6 ± 541.6 | 23,020.4 ± 510.2 |
| Urbanization index | 72.7 ± 0.3 | 62.6 ± 0.4 | 56.6 ± 0.4 | 51.5 ± 0.4 |
| Male (%) | 41.9 | 44.0 | 46.1 | 46.3 |
| Han (%) | 90.9 | 86.6 | 86.4 | 88.6 |
| Married (%) | 84.7 | 84.4 | 86.0 | 85.1 |
| Greater than high school (%) | 14.8 | 6.0 | 4.6 | 3.9 |
| Moderate-to-vigorous activity (%) | 29.1 | 47.2 | 59.4 | 66.4 |
| Current drinker (%) | 36.4 | 32.3 | 34.5 | 31.8 |
| Current smoker (%) | 27.1 | 28.0 | 29.2 | 29.8 |
| Dietary intake | ||||
| Energy intake (kcal/day) | 2160.4 ± 9.9 | 2151.8 ± 8.6 | 2119.1 ± 9.0 | 2005.3 ± 10.4 |
| Whole grains (g/2000 kcal/day) | 3.4 ± 0.2 | 3.9 ± 0.2 | 5.3 ± 0.3 | 9.9 ± 0.8 |
| Refined grains (g/2000 kcal/day) | 257.8 ± 1.6 | 338.0 ± 1.6 | 403.1 ± 2.1 | 587.1 ± 5.6 |
| Fried cereals (g/2000 kcal/day) | 5.4 ± 0.2 | 6.2 ± 0.3 | 6.8 ± 0.3 | 8.0 ± 0.5 |
| Stir-fried cereals (g/2000 kcal/day) | 7.4 ± 0.3 | 8.4 ± 0.3 | 10.8 ± 0.4 | 12.6 ± 0.6 |
| Boiled cereals (g/2000 kcal/day) | 237.3 ± 1.1 | 316.4 ± 0.8 | 366.8 ± 0.9 | 483.8 ± 2.4 |
| Baked cereals (g/2000 kcal/day) | 7.5 ± 0.4 | 8.3 ± 0.4 | 13.0 ± 0.6 | 19.0 ± 0.9 |
| Sodium (mg/2000 kcal/day) | 5374.3 ± 458.4 | 5043.1 ± 375.2 | 4644.0 ± 239.5 | 4954.2 ± 413.0 |
| Potassium (mg/2000 kcal/day) | 1972.9 ± 22.4 | 1799.6 ± 14.1 | 1770.1 ± 13.9 | 1736.5 ± 14.4 |
| AHEI score ‡ | 42.5 ± 0.1 | 42.9 ± 0.1 | 44.5 ± 0.1 | 44.9 ± 0.1 |
| Quartiles of Dietary Cereal Intake (g/2000 kcal/day) | |||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | p-Trend | |
| Total cereals | |||||
| Median (g/2000 kcal/day) | 276 | 344 | 402 | 498 | |
| Cases/person-years | 755/16,620 | 952/24,930 | 948/24,930 | 988/19,390 | |
| Model 1 * | 1 | 1.01 (0.92–1.11) | 1.01 (0.91–1.11) | 1.12 (1.02–1.23) | 0.026 |
| Model 2 † | 1 | 1.04 (0.94–1.15) | 1.07 (0.97–1.18) | 1.16 (1.05–1.29) | 0.004 |
| Model 3 ‡ | 1 | 1.05 (0.95–1.15) | 1.06 (0.96–1.18) | 1.15 (1.03–1.29) | 0.015 |
| Fried cereals | |||||
| Median (g/2000 kcal/day) | 0 | 6 | 16 | 38 | |
| Cases/person-years | 2436/55,608 | 473/12,540 | 406/9414 | 328/6270 | |
| Model 1 * | 1 | 1.12 (1.01–1.23) | 1.23 (1.10–1.36) | 1.42 (1.26–1.59) | <0.001 |
| Model 2 † | 1 | 1.06 (0.96–1.17) | 1.15 (1.04–1.28) | 1.25 (1.11–1.41) | <0.0001 |
| Model 3 ‡ | 1 | 1.04 (0.94–1.16) | 1.11 (0.99–1.24) | 1.20 (1.06–1.36) | 0.002 |
| Baked cereals | |||||
| Median (g/2000 kcal/day) | 0 | 9 | 23 | 70 | |
| Cases/person-years | 2391/55,349 | 447/11,627 | 430/9522 | 375/7406 | |
| Model 1 * | 1 | 1.11 (1.01–1.23) | 1.43 (1.29–1.59) | 1.30 (1.17–1.45) | <0.001 |
| Model 2 † | 1 | 1.07 (0.97–1.19) | 1.33 (1.20–1.47) | 1.21 (1.08–1.35) | <0.001 |
| Model 3 ‡ | 1 | 1.07 (0.96–1.19) | 1.33 (1.19–1.49) | 1.20 (1.06–1.36) | <0.001 |
| Boiled cereals | |||||
| Median (g/2000 kcal/day) | 235 | 314 | 369 | 467 | |
| Cases/person-years | 803/13,850 | 915/24,930 | 950/24,930 | 975/24,930 | |
| Model 1 * | 1 | 0.88 (0.80–0.96) | 0.88 (0.80–0.97) | 0.95 (0.87–1.05) | 0.519 |
| Model 2 † | 1 | 0.92 (0.83–1.01) | 0.96 (0.87–1.07) | 1.02 (0.92–1.13) | 0.452 |
| Model 3 ‡ | 1 | 0.98 (0.89–1.08) | 1.04 (0.94–1.16) | 1.11 (0.99–1.25) | 0.034 |
| Stir-fried cereals | |||||
| Median (g/2000 kcal/day) | 0 | 7 | 16 | 40 | |
| Cases/person-years | 1987/39,810 | 648/17,772 | 586/13,338 | 422/10,374 | |
| Model 1 * | 1 | 0.94 (0.86–1.03) | 1.01 (0.92–1.11) | 0.93 (0.84–1.04) | 0.353 |
| Model 2 † | 1 | 0.95 (0.87–1.04) | 1.04 (0.95–1.14) | 0.97 (0.87–1.08) | 0.863 |
| Model 3 ‡ | 1 | 0.95 (0.87–1.04) | 1.05 (0.96–1.16) | 0.99 (0.89–1.11) | 0.733 |
| Whole Grain Consumer | |||
|---|---|---|---|
| No | Yes | p Value | |
| Total whole grains | |||
| Cases/person-years | 2785/60,963 | 858/21,339 | |
| Model 1 * | 1 | 0.95 (0.88–1.02) | 0.149 |
| Model 2 † | 1 | 0.93 (0.86–1.00) | 0.050 |
| Model 3 ‡ | 1 | 0.92 (0.85–0.99) | 0.027 |
| Fried whole grains | |||
| Cases/person-years | 3622/77,154 | 21/522 | |
| Model 1 * | 1 | 0.87 (0.57–1.34) | 0.524 |
| Model 2 † | 1 | 0.84 (0.55–1.30) | 0.436 |
| Model 3 ‡ | 1 | 0.86 (0.56–1.32) | 0.476 |
| Baked whole grains | |||
| Cases/person-years | 3571/76,328 | 72/1232 | |
| Model 1 * | 1 | 1.13 (0.89–1.42) | 0.324 |
| Model 2 † | 1 | 1.04 (0.82–1.32) | 0.731 |
| Model 3 ‡ | 1 | 1.03 (0.81–1.31) | 0.817 |
| Boiled whole grains | |||
| Cases/person-years | 3023/65,933 | 620/14,949 | |
| Model 1 * | 1 | 0.98 (0.90–1.07) | 0.623 |
| Model 2 † | 1 | 0.96 (0.88–1.04) | 0.310 |
| Model 3 ‡ | 1 | 0.96 (0.87–1.04) | 0.314 |
| Stir-fried whole grains | |||
| Cases/person-years | 3423/73,017 | 220/5841 | |
| Model 1 * | 1 | 0.83 (0.72–0.95) | 0.007 |
| Model 2 † | 1 | 0.85 (0.74–0.98) | 0.022 |
| Model 3 ‡ | 1 | 0.85 (0.74–0.98) | 0.025 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.; Ao, Y.; Wan, X.; Liu, X.; Yao, J.; Ye, H.; Wang, A.; Zhuang, P.; Jiao, J.; Zhang, Y. Assessing the Hypertension Risk: A Deep Dive into Cereal Consumption and Cooking Methods—Insights from China. Nutrients 2024, 16, 3027. https://doi.org/10.3390/nu16173027
Huang Y, Ao Y, Wan X, Liu X, Yao J, Ye H, Wang A, Zhuang P, Jiao J, Zhang Y. Assessing the Hypertension Risk: A Deep Dive into Cereal Consumption and Cooking Methods—Insights from China. Nutrients. 2024; 16(17):3027. https://doi.org/10.3390/nu16173027
Chicago/Turabian StyleHuang, Yingyu, Yang Ao, Xuzhi Wan, Xiaohui Liu, Jianxin Yao, Hao Ye, Anli Wang, Pan Zhuang, Jingjing Jiao, and Yu Zhang. 2024. "Assessing the Hypertension Risk: A Deep Dive into Cereal Consumption and Cooking Methods—Insights from China" Nutrients 16, no. 17: 3027. https://doi.org/10.3390/nu16173027
APA StyleHuang, Y., Ao, Y., Wan, X., Liu, X., Yao, J., Ye, H., Wang, A., Zhuang, P., Jiao, J., & Zhang, Y. (2024). Assessing the Hypertension Risk: A Deep Dive into Cereal Consumption and Cooking Methods—Insights from China. Nutrients, 16(17), 3027. https://doi.org/10.3390/nu16173027






