The Return on Investment for the Prevention and Treatment of Childhood and Adolescent Overweight and Obesity in Beijing: A Modeling Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Model Overview
2.1.1. BMI, Overweight, and Obesity Prevalence
2.1.2. Health Consequences
2.1.3. Economic Consequences
2.2. Intervention Selection for Beijing
- Restrictions on unhealthy food marketing to children and adolescents limit advertising of unhealthy foods and beverages across all media channels for children and adolescents aged 2–18 years to reduce exposure to unhealthy dietary promotion.
- Mandatory Front of Package labeling (FOPL): It will ensure that clear nutritional information is directly available to consumers, especially parents and caregivers, to support them in making healthier food choices for young people. A mandatory FOPL policy would replace China’s current voluntary FOPL system, which has seen limited adoption among food manufacturers.
- Nutrition counseling in primary healthcare would be administered by physicians to children and adolescents aged 0–19 who are affected by OAO. For younger children, the intervention includes parents or caregivers to equip them with guidance on implementing appropriate nutritional strategies at home.
- Family-based intervention focuses on primary-school-aged children and aims to link the school and family environments. The program uses educational workshops to promote healthy eating and physical activity in the home and family, with engagement and educational activities for families.
- School-based intervention includes a structured nutrition education program in schools, regular assessments, school cafeteria menu improvements to ensure healthier food options, and implementation of the “Happy 10 Minutes” exercise sessions during the school day.
2.3. Intervention Cost and Target Population
2.4. Economic Outcome Indicator
3. Results
3.1. Cost on CAOAO
3.2. Cost Analysis of CAOAO Interventions in Beijing
3.3. Health and Economic Benefits of Implementing New Interventions
3.4. ROI Analysis of Interventions in Beijing
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aris, I.M.; Block, J.P. Childhood Obesity Interventions—Going Beyond the Individual. JAMA Pediatr. 2022, 176, e214388. [Google Scholar] [CrossRef] [PubMed]
- Watkins, D.; Hale, J.; Hutchinson, B.; Kataria, I.; Kontis, V.; Nugent, R. Investing in Non-Communicable Disease Risk Factor Control among Adolescents Worldwide: A Modelling Study. BMJ Glob. Health 2019, 4, e001335. [Google Scholar] [CrossRef]
- Wu, S.; Ding, Y.; Wu, F.; Li, R.; Hu, Y.; Hou, J.; Mao, P. Socio-Economic Position as an Intervention against Overweight and Obesity in Children: A Systematic Review and Meta-Analysis. Sci. Rep. 2015, 5, 11354. [Google Scholar] [CrossRef]
- WHO Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 2 January 2024).
- Okunogbe, A.; Nugent, R.; Spencer, G.; Powis, J.; Ralston, J.; Wilding, J. Economic Impacts of Overweight and Obesity: Current and Future Estimates for 161 Countries. BMJ Glob. Health 2022, 7, e009773. [Google Scholar] [CrossRef] [PubMed]
- NCD-RisC Data Downloads: Download Files Containing Country Risk Factor Data 2017. Available online: http://ncdrisc.org/data-downloads.html (accessed on 1 April 2022).
- Liu, Z.; Gao, P.; Gao, A.-Y.; Lin, Y.; Feng, X.-X.; Zhang, F.; Xu, L.-Q.; Niu, W.-Y.; Fang, H.; Zhou, S.; et al. Effectiveness of a Multifaceted Intervention for Prevention of Obesity in Primary School Children in China: A Cluster Randomized Clinical Trial. JAMA Pediatr. 2022, 176, e214375. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, L.; Xue, B.; Wang, Y. Associations between General and Central Obesity and Hypertension among Children: The Childhood Obesity Study in China Mega-Cities. Sci. Rep. 2017, 7, 16895. [Google Scholar] [CrossRef]
- Li, Z.; Fang, Y.; Zhang, N.; Zhu, W.; Chang, S.; Zhou, S.; Zhang, M.; Ma, G. Evaluating Childhood Overweight- and Obesity-Related Food Marketing Policies in China Using the Food–Environment Policy Index (Food–EPI). Nutrients 2024, 16, 482. [Google Scholar] [CrossRef] [PubMed]
- Ma, G.; Meyer, C.L.; Jackson-Morris, A.; Chang, S.; Narayan, A.; Zhang, M.; Wu, D.; Wang, Y.; Yang, Z.; Wang, H.; et al. The Return on Investment for the Prevention and Treatment of Childhood and Adolescent Overweight and Obesity in China: A Modelling Study. Lancet Reg. Health West. Pac. 2023, 43, 100977. [Google Scholar] [CrossRef]
- Liu, M.; Cao, B.; Liu, M.; Liang, X.; Wu, D.; Li, W.; Su, C.; Chen, J.; Gong, C. High Prevalence of Obesity but Low Physical Activity in Children Aged 9–11 Years in Beijing. Diabetes Metab. Syndr. Obes. 2021, 14, 3323–3335. [Google Scholar] [CrossRef]
- Gao, C.; Xu, J.; Liu, Y.; Yang, Y. Nutrition Policy and Healthy China 2030 Building. Eur. J. Clin. Nutr. 2021, 75, 238–246. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. Healthy China action 2019–2030; National Health Commission of the People’s Republic of China: Beijning, China, 2019; p. 17. [Google Scholar]
- Cai, L.; Hu, X.; Liu, S.; Wang, L.; Wang, X.; Tu, H.; Tong, Y. China Is Implementing the National Nutrition Plan of Action. Front. Nutr. 2022, 9, 983484. [Google Scholar] [CrossRef]
- Beijing Municipal Health Commission Guidelines for the Prevention and Control of Overweight and Obesity Among School Aged in Beijing. Available online: https://wjw.beijing.gov.cn/zwgk_20040/zxgk/202012/t20201222_2170248.html (accessed on 1 January 2024).
- Lavriša, Ž.; Pravst, I. Marketing of Foods to Children through Food Packaging Is Almost Exclusively Linked to Unhealthy Foods. Nutrients 2019, 11, 1128. [Google Scholar] [CrossRef] [PubMed]
- Taillie, L.S.; Busey, E.; Stoltze, F.M.; Dillman Carpentier, F.R. Governmental Policies to Reduce Unhealthy Food Marketing to Children. Nutr. Rev. 2019, 77, 787–816. [Google Scholar] [CrossRef] [PubMed]
- Turnwald, B.P.; Crum, A.J. Smart Food Policy for Healthy Food Labeling: Leading with Taste, Not Healthiness, to Shift Consumption and Enjoyment of Healthy Foods. Prev. Med. 2019, 119, 7–13. [Google Scholar] [CrossRef]
- Kraef, C.; Wood, B.; von Philipsborn, P.; Singh, S.; Peterson, S.S.; Kallestrup, P. Primary Health Care and Nutrition. Bull. World Health Organ. 2020, 98, 886–893. [Google Scholar] [CrossRef]
- Aboueid, S.; Bourgeault, I.; Giroux, I. Nutrition Care Practices of Primary Care Providers for Weight Management in Multidisciplinary Primary Care Settings in Ontario, Canada—a Qualitative Study. BMC Fam. Pract. 2018, 19, 69. [Google Scholar] [CrossRef] [PubMed]
- Billah, S.M.; Saha, K.K.; Khan, A.N.S.; Chowdhury, A.H.; Garnett, S.P.; Arifeen, S.E.; Menon, P. Quality of Nutrition Services in Primary Health Care Facilities: Implications for Integrating Nutrition into the Health System in Bangladesh. PLoS ONE 2017, 12, e0178121. [Google Scholar] [CrossRef]
- WHO; NFS. Mobilizing Ambitious and Impactful Commitments for Mainstreaming Nutrition in Health Systems: Nutrition in Universal Health Coverage—Global Nutrition Summit; WHO: Geneva, Switzerland, 2020; p. 45. [Google Scholar]
- Li, B.; Pallan, M.; Liu, W.J.; Hemming, K.; Frew, E.; Lin, R.; Liu, W.; Martin, J.; Zanganeh, M.; Hurley, K.; et al. The CHIRPY DRAGON Intervention in Preventing Obesity in Chinese Primary-School–Aged Children: A Cluster-Randomised Controlled Trial. PLOS Med. 2019, 16, e1002971. [Google Scholar] [CrossRef] [PubMed]
- Zanganeh, M.; Adab, P.; Li, B.; Pallan, M.; Liu, W.J.; Hemming, K.; Lin, R.; Liu, W.; Martin, J.; Cheng, K.K.; et al. Cost-Effectiveness of a School-and Family-Based Childhood Obesity Prevention Programme in China: The “CHIRPY DRAGON” Cluster-Randomised Controlled Trial. Int. J. Public. Health 2021, 66, 1604025. [Google Scholar] [CrossRef]
- Xu, H.; Li, Y.; Du, S.; Zhang, Q.; Liu, A.; Sun, J.; Ma, G. Cost-Utility and Cost-Benefit Analyses of School-Based Obesity Prevention Program. BMC Public Health 2020, 20, 1608. [Google Scholar] [CrossRef]
- Meng, L.; Xu, H.; Liu, A.; Van Raaij, J.; Bemelmans, W.; Hu, X.; Zhang, Q.; Du, S.; Fang, H.; Ma, J.; et al. The Costs and Cost-Effectiveness of a School-Based Comprehensive Intervention Study on Childhood Obesity in China. PLoS ONE 2013, 8, e77971. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Ma, L.; Jia, P.; Xue, H.; Xu, F.; Zhao, L.; Xue, B.; Wang, Y.; Wang, Y. Longitudinal Effects of School Policies on Children’s Eating Behaviors and Weight Status: Findings from the Childhood Obesity Study in China Megacities. Int. J. Obes. 2023, 47, 17–23. [Google Scholar] [CrossRef]
- Haby, M.M.; Vos, T.; Carter, R.; Moodie, M.; Markwick, A.; Magnus, A.; Tay-Teo, K.-S.; Swinburn, B. A New Approach to Assessing the Health Benefit from Obesity Interventions in Children and Adolescents: The Assessing Cost-Effectiveness in Obesity Project. Int. J. Obes. 2006, 30, 1463–1475. [Google Scholar] [CrossRef]
- Hayes, A.; Tan, E.J.; Lung, T.; Brown, V.; Moodie, M.; Baur, L. A New Model for Evaluation of Interventions to Prevent Obesity in Early Childhood. Front. Endocrinol. 2019, 10, 132. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Bai, R.; Wang, L.; Feng, X.; Liu, Y.; Zhou, M. A Projection of Life Expectancy Based on the Global Burden of Disease Study 2019—China, 1990–2030. CCDCW 2023, 5, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Collaborative Network Global Burden of Disease Study 2019 (GBD 2019) Results. Available online: https://vizhub.healthdata.org/gbd-results (accessed on 2 January 2024).
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide Trends in Body-Mass Index, Underweight, Overweight, and Obesity from 1975 to 2016: A Pooled Analysis of 2416 Population-Based Measurement Studies in 128·9 Million Children, Adolescents, and Adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- United Nations. P.D. World Population Prospects. Available online: https://population.un.org/wpp/Download/Standard/Population/ (accessed on 2 January 2024).
- Disability-Adjusted Life Years (DALYs). Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/158 (accessed on 26 April 2024).
- Robinson, L.A.; Hammitt, J.K.; Cecchini, M.; Chalkidou, K.; Claxton, K.; Cropper, M.; Eozenou, P.H.-V.; de Ferranti, D.; Deolalikar, A.B.; Campos Guanais de Aguiar, F.; et al. Reference Case Guidelines for Benefit-Cost Analysis in Global Health and Development 2019. Available online: https://www.hsph.harvard.edu/wp-content/uploads/sites/2447/2019/05/BCA-Guidelines-May-2019.pdf (accessed on 1 April 2022).
- Nishtar, S.; Gluckman, P.; Armstrong, T. Ending Childhood Obesity: A Time for Action. Lancet 2016, 387, 825–827. [Google Scholar] [CrossRef] [PubMed]
- A Healthy Diet Sustainably Produced: Information Sheet. Available online: https://www.who.int/publications-detail-redirect/WHO-NMH-NHD-18.12 (accessed on 2 April 2024).
- Promoting Physical Activity through Schools: Policy Brief. Available online: https://www.who.int/publications-detail-redirect/9789240049567 (accessed on 2 April 2024).
- Nutrition Labelling: Policy Brief. Available online: https://www.who.int/publications-detail-redirect/9789240051324 (accessed on 2 April 2024).
- Fiscal Policies to Promote Healthy Diets: Policy Brief. Available online: https://www.who.int/publications-detail-redirect/9789240049543 (accessed on 2 April 2024).
- A Primary Health Care Approach to Obesity Prevention and Management in Children and Adolescents: Policy Brief. Available online: https://www.who.int/publications-detail-redirect/9789240072671 (accessed on 2 April 2024).
- WHO Acceleration Plan to Stop Obesity. Available online: https://www.who.int/publications-detail-redirect/9789240075634 (accessed on 2 April 2024).
- Cecchini, M.; Sassi, F.; Lauer, J.A.; Lee, Y.Y.; Guajardo-Barron, V.; Chisholm, D. Tackling of Unhealthy Diets, Physical Inactivity, and Obesity: Health Effects and Cost-Effectiveness. Lancet 2010, 376, 1775–1784. [Google Scholar] [CrossRef]
- Xu, H.; Li, Y.; Zhang, Q.; Hu, X.; Liu, A.; Du, S.; Li, T.; Guo, H.; Li, Y.; Xu, G.; et al. Comprehensive School-Based Intervention to Control Overweight and Obesity in China: A Cluster Randomized Controlled Trial. Asia Pac. J. Clin. Nutr. 2017, 26, 1139–1151. [Google Scholar]
- NBS Survey Office in Beijing Beijing Municipal Bureau of Statistics and NBS Survey Office in Beijing. Available online: https://tjj.beijing.gov.cn/EnglishSite/ (accessed on 28 February 2024).
- National Bureau of Statistics of China. Available online: https://www.stats.gov.cn/english/ (accessed on 29 February 2024).
- Wilkinson, T.; Sculpher, M.J.; Claxton, K.; Revill, P.; Briggs, A.; Cairns, J.A.; Teerawattananon, Y.; Asfaw, E.; Lopert, R.; Culyer, A.J.; et al. The International Decision Support Initiative Reference Case for Economic Evaluation: An Aid to Thought. Value Health 2016, 19, 921–928. [Google Scholar] [CrossRef]
- Sanders, G.D.; Neumann, P.J.; Basu, A.; Brock, D.W.; Feeny, D.; Krahn, M.; Kuntz, K.M.; Meltzer, D.O.; Owens, D.K.; Prosser, L.A.; et al. Recommendations for Conduct, Methodological Practices, and Reporting of Cost-Effectiveness Analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA 2016, 316, 1093–1103. [Google Scholar] [CrossRef] [PubMed]
| Intervention | Intervention Target Population | Beijing Baseline (%) | Modeled Target (%) |
|---|---|---|---|
| Policy | |||
| Restrictions on unhealthy food marketing to children [43] | Children and adolescents aged 2–18 years | 0 | 80 |
| Mandatory Front of Package labeling (FOPL) [43] | All age label users | 5 | 100 |
| Nutrition Counseling | |||
| Nutrition counseling in primary healthcare [43] | Children and adolescents affected by OAO aged 0–19 years | 0 | 40 |
| School and Family Interventions | |||
| Family-based intervention [24] | School children aged 6–7 years | 0 | 80 |
| School-based intervention [25,44] | School children and adolescentsaged 6–17 years | 5 | 80 |
| YLL (Million) | YLD (Million) | DALYS (Million) | |
|---|---|---|---|
| Male | 5.8 | 1.5 | 7.3 |
| Females | 3.8 | 2.3 | 6.2 |
| Total | 9.6 | 3.8 | 13.4 |
| Total Cost USD (Billions) | Total Cost CNY (Billions, 2022) | Average Lifetime Cost per Child with Obesity (USD) | Average Lifetime Cost per Child with Obesity (CNY, 2022) | |
|---|---|---|---|---|
| Direct healthcare costs | ||||
| During childhood | 0.3 | 2.0 | 296.2 | 2103.0 |
| During adulthood | 2.5 | 17.8 | 2661.7 | 18,897.8 |
| Total direct healthcare costs | 2.8 | 19.9 | 2957.9 | 21,000.8 |
| Indirect costs | ||||
| Loss in lifetime wages | 27.8 | 197.1 | 13,160.2 | 93,437.3 |
| Productivity loss | 32.1 | 228.2 | 2208.2 | 15,678.5 |
| Mortality costs | 1999.0 | 14,197.5 | 947,926.8 | 6,730,280.5 |
| Total indirect costs | 2058.9 | 14,622.8 | 963,295.2 | 6,839,396.3 |
| Intervention Cost | Beijing (Million, USD) | Beijing (Million, CNY, 2022) |
|---|---|---|
| Policy | ||
| 0.63 | 4.5 |
| 3.73 | 26.5 |
| Nutrition Counseling | ||
| 5.55 | 39.5 |
| School and Family Interventions | ||
| 12.87 | 91.4 |
| 526 | 3736 |
| Package | ||
| Package 1 (Restrictions on unhealthy food marketing to children + FOPL) | 4.36 | 31 |
| Package 2 (Restrictions on unhealthy food marketing to children + FOPL + School-based intervention + Nutrition counseling in primary healthcare) | 535.95 | 3806.4 |
| All five interventions | 548.81 | 3897.8 |
| Intervention | Lifetime Reduction in DALYs |
|---|---|
| Policy | |
| 146,629 |
| 8430 |
| Nutrition Counseling | |
| 34,917 |
| School and Family Interventions | |
| 8438 |
| 83,062 |
| Package | |
| Package 1 (Restrictions on unhealthy food marketing to children + FOPL) | 155,436 |
| Package 2 (Restrictions on unhealthy food marketing to children + FOPL + School-based intervention + Nutrition counseling in primary healthcare) | 281,045 |
| All five interventions | 290,304 |
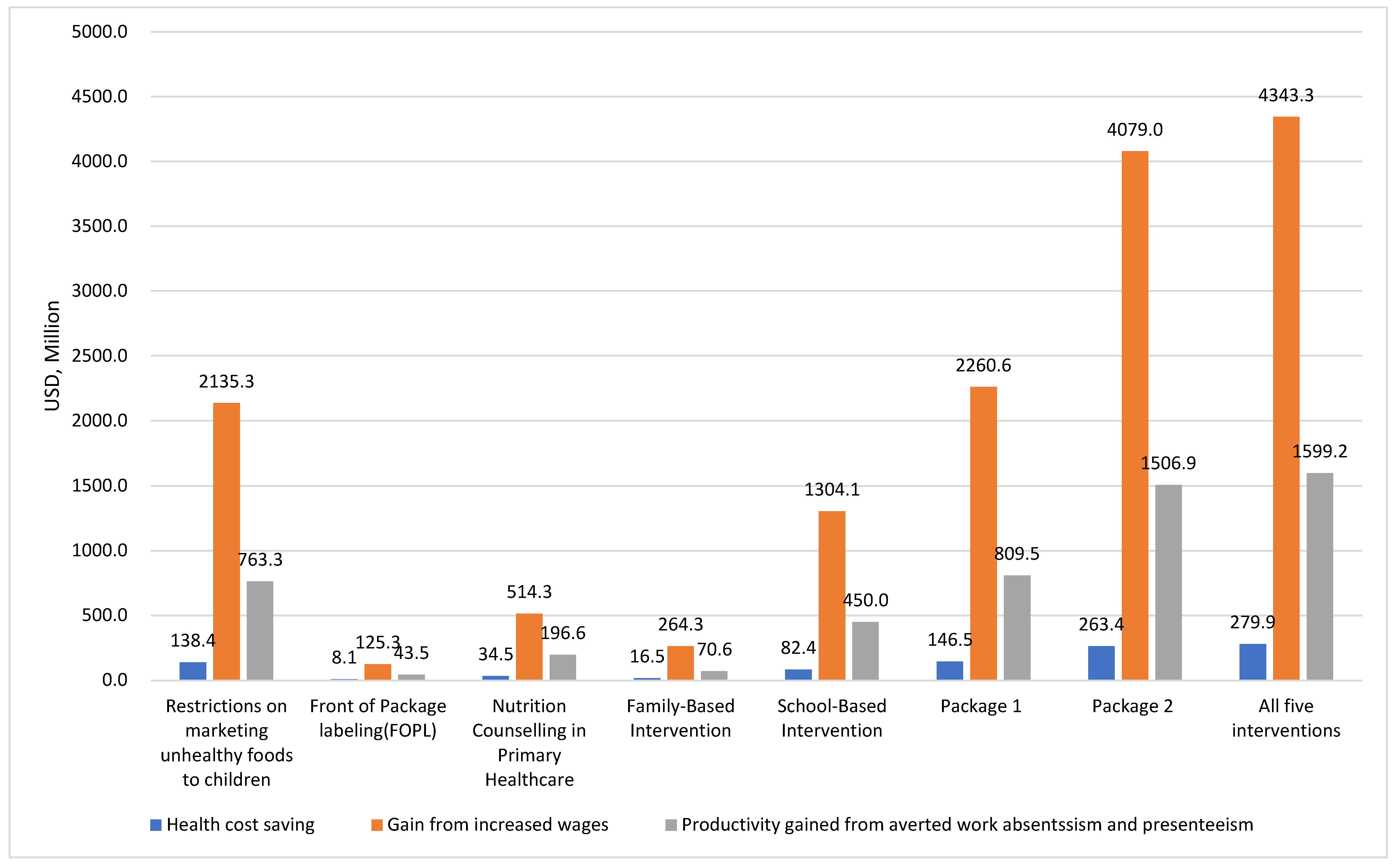
| Intervention | Healthcare Cost Savings (USD Millions) | Gains from Increased Wages (USD, Million) | Productivity Gained from Averted Work Absenteeism and Presenteeism (USD Millions) | Economic Value of Life Years Gained (YLLs only) (USD Millions) | Total Savings (USD Millions) |
|---|---|---|---|---|---|
| Policy | |||||
| 138.4 | 2135.3 | 763.3 | 18,171.4 | 21,208.4 |
| 8.1 | 125.3 | 43.5 | 1040.0 | 1216.9 |
| Nutrition Counseling | |||||
| 34.5 | 514.3 | 196.6 | 4566.4 | 5311.8 |
| School and Family Interventions | |||||
| 16.5 | 264.3 | 70.6 | 720.3 | 1071.7 |
| 82.4 | 1304.1 | 450.0 | 10,400.0 | 12,236.4 |
| Package | |||||
| Package 1 (Restrictions on unhealthy food marketing to children + FOPL) | 146.5 | 2260.6 | 809.5 | 19,268.9 | 22,485.5 |
| Package 2 (Restrictions on unhealthy food marketing to children + FOPL + School-based intervention + Nutrition counseling in primary healthcare) | 263.4 | 4079 | 1506.9 | 35,398.5 | 41,247.8 |
| All five interventions | 279.9 | 4343.3 | 1599.2 | 36,234.6 | 42,457.1 |
| Intervention | Return on Investment (ROI) | |||
|---|---|---|---|---|
| Over 10 Years | Over 30 Years | Over 50 Years | Over Lifetime | |
| Policy | ||||
| 287.37 | 2390.98 | 13,427.79 | 33,723.08 |
| 1.85 | 22.43 | 130.33 | 324.91 |
| Nutrition Counseling | ||||
| 8.55 | 80.08 | 438.08 | 955.23 |
| School and Family Interventions | ||||
| −0.76 | 8.51 | 13.63 | 82.30 |
| −0.90 | 0.73 | 8.78 | 22.26 |
| Package | ||||
| Package 1 (Restrictions on unhealthy food marketing to children + FOPL) | 43.01 | 364.21 | 2049.67 | 5152.86 |
| Package 2 (Restrictions on unhealthy food marketing to children + FOPL + School-based intervention + Nutrition counseling in primary healthcare) | −0.51 | 4.55 | 30.29 | 75.96 |
| All five interventions | −0.51 | 4.66 | 29.61 | 76.36 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Meyer, C.L.; Xu, H.; Jackson-Morris, A.; Zhang, M.; Wu, D.; He, H.; Chang, S.; Ma, G. The Return on Investment for the Prevention and Treatment of Childhood and Adolescent Overweight and Obesity in Beijing: A Modeling Study. Nutrients 2024, 16, 3006. https://doi.org/10.3390/nu16173006
Li Z, Meyer CL, Xu H, Jackson-Morris A, Zhang M, Wu D, He H, Chang S, Ma G. The Return on Investment for the Prevention and Treatment of Childhood and Adolescent Overweight and Obesity in Beijing: A Modeling Study. Nutrients. 2024; 16(17):3006. https://doi.org/10.3390/nu16173006
Chicago/Turabian StyleLi, Zhenhui, Christina L. Meyer, Haiquan Xu, Angie Jackson-Morris, Man Zhang, Daphne Wu, Hairong He, Suying Chang, and Guansheng Ma. 2024. "The Return on Investment for the Prevention and Treatment of Childhood and Adolescent Overweight and Obesity in Beijing: A Modeling Study" Nutrients 16, no. 17: 3006. https://doi.org/10.3390/nu16173006
APA StyleLi, Z., Meyer, C. L., Xu, H., Jackson-Morris, A., Zhang, M., Wu, D., He, H., Chang, S., & Ma, G. (2024). The Return on Investment for the Prevention and Treatment of Childhood and Adolescent Overweight and Obesity in Beijing: A Modeling Study. Nutrients, 16(17), 3006. https://doi.org/10.3390/nu16173006







