Estimating the Potential Health Care Cost-Savings from a Flax-Based Treatment for Hypertension
Abstract
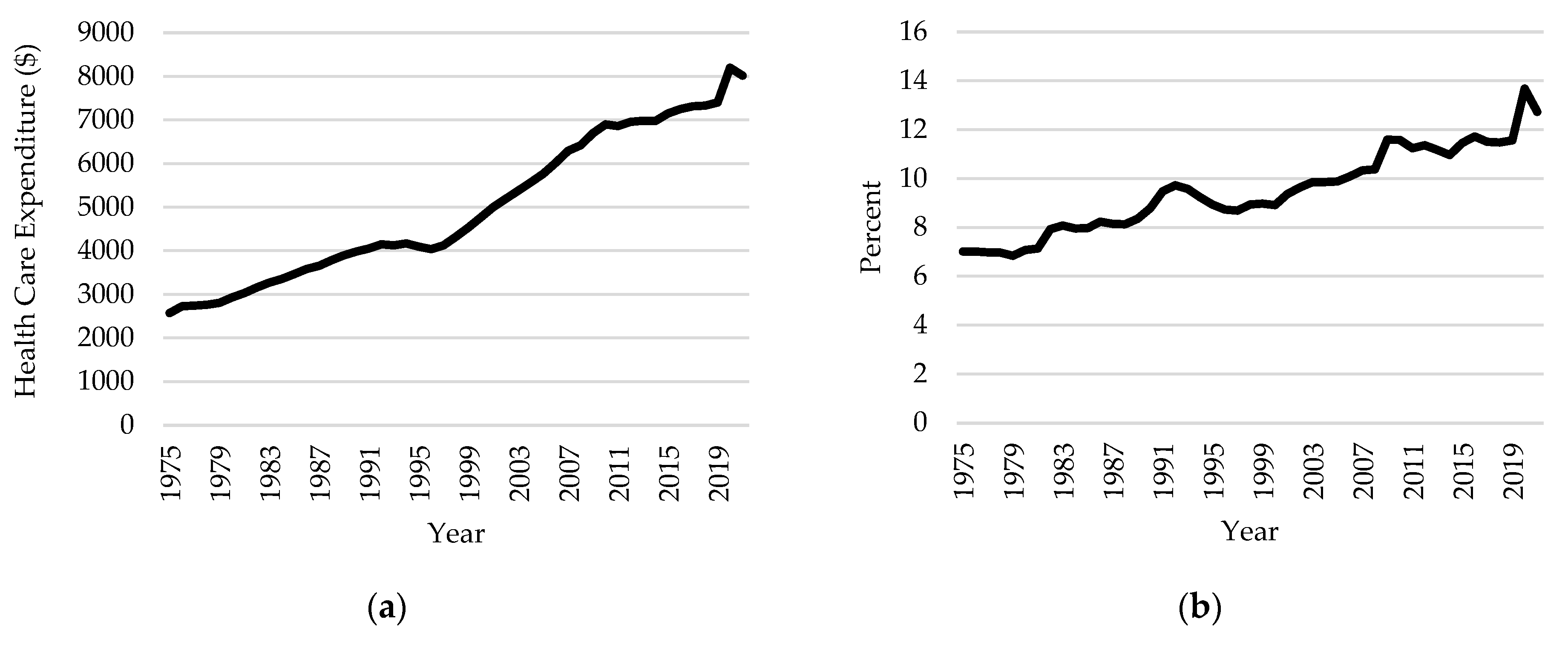
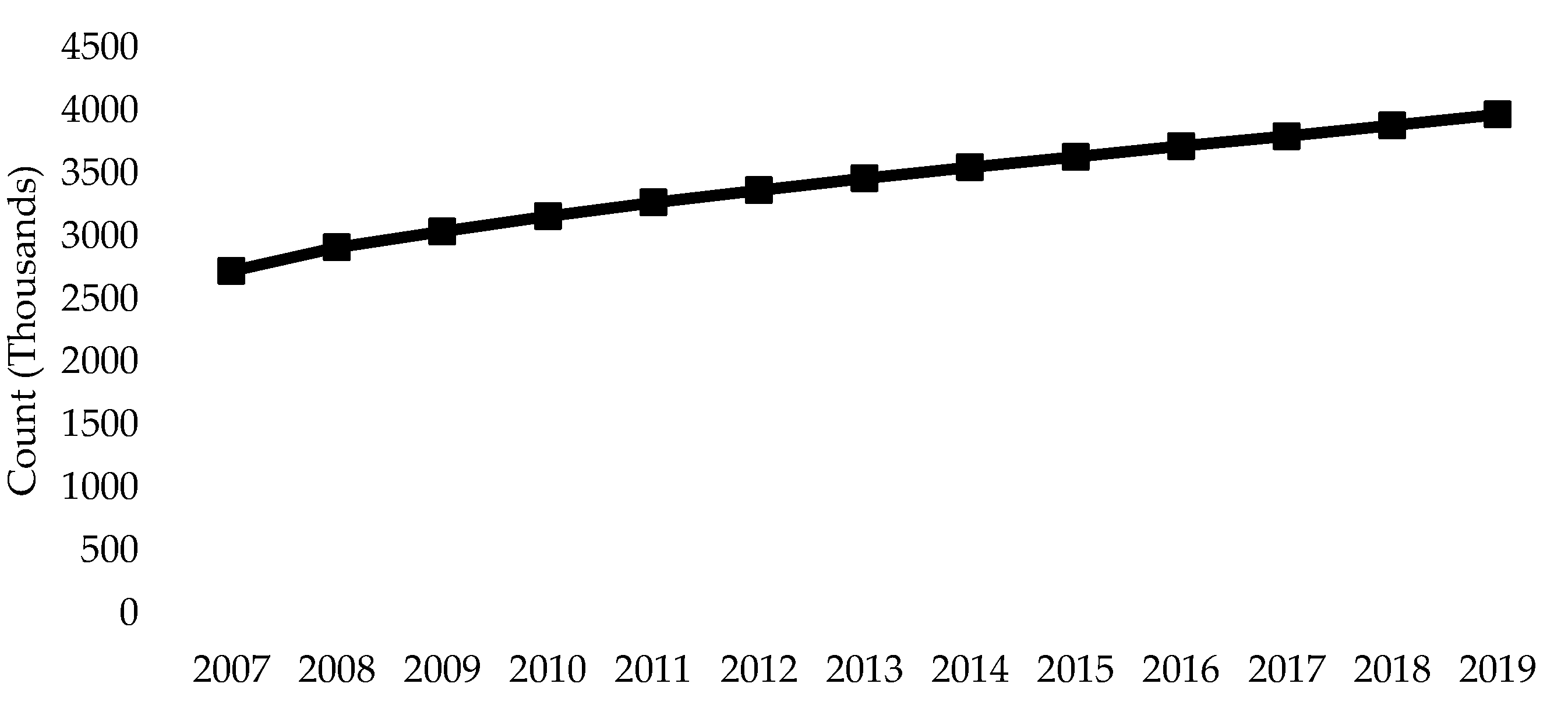
1. Introduction
2. Materials and Methods
2.1. Cost-of-Illness Analysis
2.1.1. Step 1: Intake Success Rate
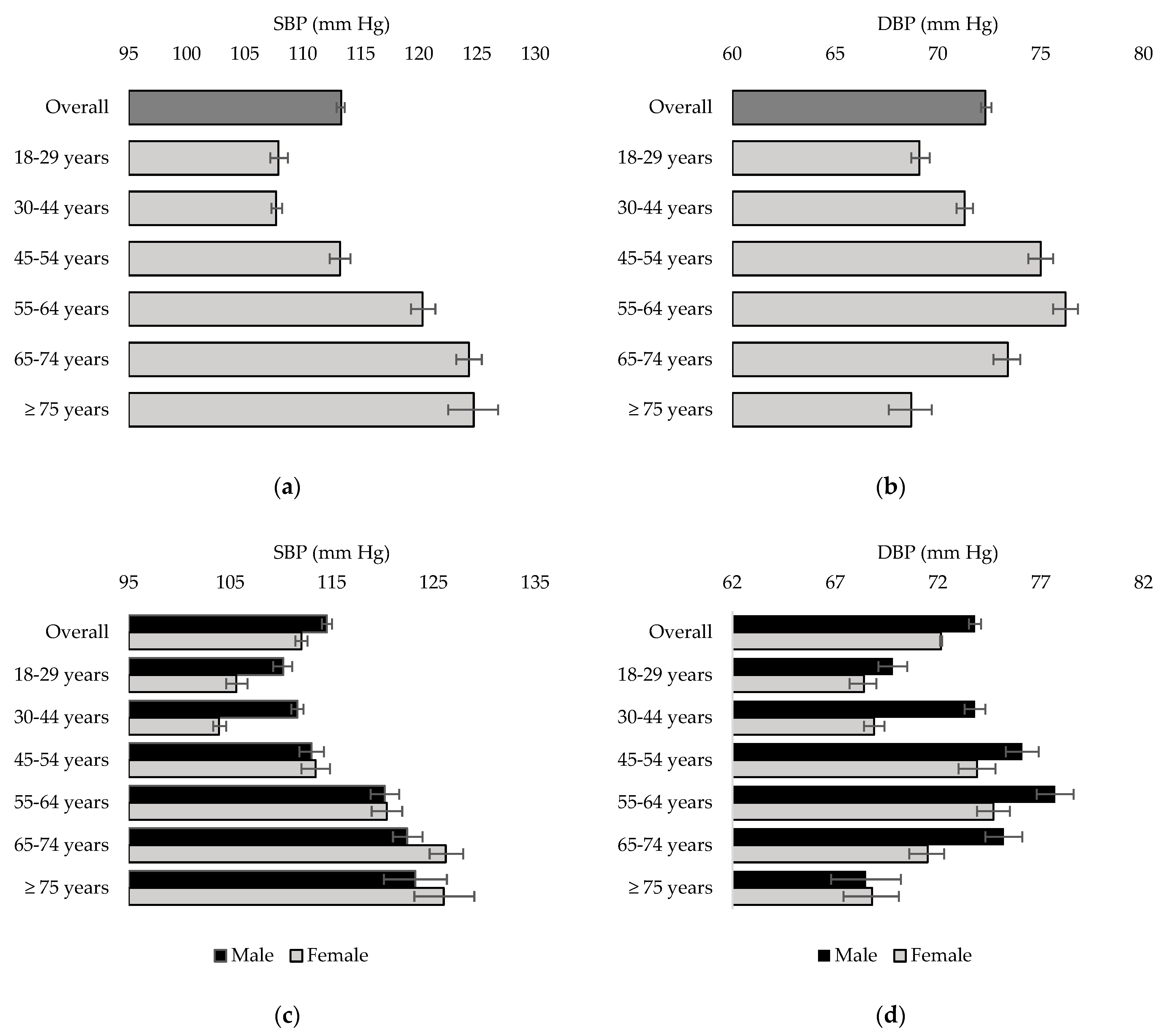
2.1.2. Step 2: Effect of Flaxseed on Blood Pressure
2.1.3. Step 3: Hypertension Prevalence Reduction
2.1.4. Step 4: Potential Health Care Cost-Savings
2.2. Simulations
2.2.1. Notation
2.2.2. Sensitivity Analysis
- For each , we adjust and to remove the effects of a standard dose of medications for hypertension. Let and denote the adjusted SBP and adjusted DBP, respectively, for individual . Then:andwhere denotes a random draw from the uniform distribution. For individual and , we set and .
- Let denote the subset individuals with and/or . From , we take a random sample of size , where is the intake success rate and is the number of individuals in . These are the individuals with hypertension who theoretically take the flax-based treatment.
- Let denote the sample in 2. For each , we estimate the effectiveness of the flax-based treatment. To estimate the impact of the flax-based treatment on SBP, we subtract a random variable from for each , where is a random draw from . To estimate the impact of the flax-based treatment on DBP, we subtract a random variable from the for each , where is a random draw from . Let and denote the new SBP and DBP, respectively, after the flax-based treatment for individual . Then:and
- We generate a new hypertension variable, which takes a value of 1 if the individual has an SBP 140 mm Hg and/or a DBP to 90 mm Hg. We call this variable . For individual :For individual , but , we set
- We calculate the reduced total health care costs associated with hypertension as
- We estimate the potential health care cost-savings as:
3. Results
3.1. Prevalence of Hypertension
3.2. COI Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Canadian Institute for Health Information. Graphic Illustration from the “Series A: Summary Data, Canada (XLSX)” per Capita Total Healthcare Expenditure Column. Available online: https://www.cihi.ca/en/national-health-expenditure-trends#data-tables (accessed on 20 January 2024).
- Statistics Canada: Older Adults and Population Aging Statistics. Available online: https://www.statcan.gc.ca/en/subjects-start/older_adults_and_population_aging (accessed on 10 January 2024).
- Chronic Disease Risk Factors. Available online: https://www.canada.ca/en/public-health/services/chronic-diseases/chronic-disease-risk-factors.html (accessed on 11 June 2023).
- Infographic: Canada’s Senior Population Outlook: Uncharted Territory. Available online: https://www.cihi.ca/en/infographic-canadas-seniors-population-outlook-uncharted-territory (accessed on 15 June 2023).
- Naylor, D. Innovation and reform in Canada. In Proceedings of the A Review Health Facilities & Services, St. John’s, NL, Canada, 19 October 2016. [Google Scholar]
- Clair, L.; Anderson, H.A.; Anderson, C.; Ekuma, O.; Prior, J. Cardiovascular disease and the risk of dementia: A survival analysis using administrative data from Manitoba. Can. J. Public Health 2022, 113, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.J.; Lee, J.-Y.; Han, K.; Kim, D.H.; Cho, H.; Kim, K.J.; Kang, E.S.; Cha, B.-S.; Lee, Y.-H.; Park, S. Blood pressure levels and risks of dementia: A nationwide study of 4.5 million people. Hypertension 2022, 79, 218–229. [Google Scholar] [CrossRef] [PubMed]
- Seretis, A.; Cividini, S.; Markozannes, G.; Tseretopoulou, X.; Lopez, D.S.; Ntzani, E.E.; Tsilidis, K.K. Association between blood pressure and risk of cancer development: A systematic review and meta-analysis of observational studies. Sci. Rep. 2019, 9, 8565. [Google Scholar] [CrossRef] [PubMed]
- Ettehad, D.; Emdin, C.A.; Kiran, A.; Anderson, S.G.; Callender, T.; Emberson, J.; Chalmers, J.; Rodgers, A.; Rahimi, K. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet 2015, 387, 957–967. [Google Scholar] [CrossRef] [PubMed]
- Tozawa, M.; Iseki, K.; Iseki, C.; Kinjo, K.; Ikemiya, Y.; Takishita, S. Blood pressure predicts risk of developing end-stage renal disease in men and women. Hypertension 2003, 41, 1341–1345. [Google Scholar] [CrossRef] [PubMed]
- Weaver, C.G.; Clement, F.M.; Campbell, N.R.; James, M.T.; Klarenbach, S.W.; Hemmelgarn, B.R.; Tonelli, M.; McBrien, K.A. Healthcare costs attributable to hypertension: Canadian population-based cohort study. Hypertension 2015, 66, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Li, H.; Gao, Y.; Vafaei, S.; Zhang, X.; Yang, M. Effect of flaxseed supplementation on blood pressure: A systematic review, and dose–response meta-analysis of randomized clinical trials. Food Funct. 2023, 14, 675–690. [Google Scholar] [CrossRef]
- Caligiuri, S.P.; Rodriguez-Leyva, D.; Aukema, H.M.; Ravandi, A.; Weighell, W.; Guzman, R.; Pierce, G.N. Dietary flaxseed reduces central aortic blood pressure without cardiac involvement but through changes in plasma oxylipins. Hypertension 2016, 68, 1031–1038. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Leyva, D.; Weighell, W.; Edel, A.L.; LaVallee, R.; Dibrov, E.; Pinneker, R.; Maddaford, T.G.; Ramjiawan, B.; Aliani, M.; Guzman, R.; et al. Potent antihypertensive action of dietary flaxseed in hypertensive patients. Hypertension 2013, 62, 1081–1089. [Google Scholar] [CrossRef]
- Rodriguez-Leyva, D.; Bassett, C.M.C.; McCullough, R.; Pierce, G.N. The cardiovascular effects of flaxseed and its omega-3 fatty acid, alpha-linolenic acid. Can. J. Cardiol. 2010, 26, 489–496. [Google Scholar] [CrossRef]
- Caligiuri, S.P.B.; Aukema, H.M.; Ravandi, A.; Pierce, G.N. Elevated levels of pro-inflammatory oxylipins in older subjects are normalized by flaxseed consumption. Exp. Gerontol. 2014, 59, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Dupasquier, C.M.C.; Dibrov, E.; Kneesh, A.L.; Cheung, P.K.M.; Lee, K.G.Y.; Alexander, H.K.; Yeganeh, B.K.; Moghadasian, M.H.; Pierce, G.N. Dietary flaxseed inhibits atherosclerosis in the LDL receptor-deficient mouse in part through antiproliferative and anti-inflammatory actions. Am. J. Physiol.-Heart Circ. Physiol. 2007, 293, H2394–H2402. [Google Scholar] [CrossRef] [PubMed]
- Caligiuri, S.P.B.; Aukema, H.M.; Ravandi, A.; Guzman, R.; Dibrov, E.; Pierce, G.N. Flaxseed consumption reduces blood pressure in patients with hypertension by altering circulating oxylipins via an α-linolenic acid–induced inhibition of soluble epoxide hydrolase. Hypertension 2014, 64, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Parikh, M.; Netticadan, T.; Pierce, G.N. Flaxseed: Its bioactive components and their cardiovascular benefits. Am. J. Physiol.-Heart Circ. Physiol. 2018, 314, H146–H159. [Google Scholar] [CrossRef] [PubMed]
- Chiamvimonvat, N.; Chin-Min, H.; Hsing-Ju, T.; Hammock, B.D. The soluble epoxide hydrolase as a pharmaceutical target for hypertension. J. Cardiovasc. Parmacol. 2007, 50, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Edel, A.L.; Rodriguez-Leyva, D.; Maddaford, T.G.; Caligiuri, S.P.; Austria, J.A.; Weighell, W.; Guzman, R.; Aliani, M.; Pierce, G.N. Dietary flaxseed independently lowers circulating cholesterol and lowers it beyond the effects of cholesterol-lowering medications alone in patients with peripheral artery disease. J. Nutr. 2015, 145, 749–757. [Google Scholar] [CrossRef]
- Health Canada. Summary of Health Canada’s Assessment of a Health Claim about Ground Whole Flaxseed and Blood Cholesterol Lowering. Available online: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/pdf/label-etiquet/claims-reclam/assess-evalu/flaxseed-graines-de-lin-eng.pdf (accessed on 2 May 2022).
- Outzen, M.; Thomsen, S.T.; Andersen, R.; Jakobsen, L.S.; Jakobsen, M.U.; Nauta, M.; Ravn-Haren, G.; Sloth, J.J.; Pilegaard, K.; Poulsen, M. Evaluating the health impact of increased linseed consumption in the Danish population. Food Chem. Toxicol. 2023, 183, 114308. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, M.M.H.; Hughes, J.; Grafenauer, S. Legume intake is associated with potential savings in coronary heart disease-related health care costs in Australia. Nutrients 2022, 14, 2912. [Google Scholar] [CrossRef] [PubMed]
- Canadian Grain Commission Quality of Western Canadian Flaxseed 2021. Available online: https://www.grainscanada.gc.ca/en/grain-research/export-quality/oilseeds/flaxseed/2021/01-summary.html (accessed on 20 June 2023).
- Abdullah, M.M.H.; Marinangeli, C.P.; Jones, P.J.H.; Carlberg, J.G. Canadian potential healthcare and societal cost savings from consumption of pulses: A cost-of-illness analysis. Nutrients 2017, 9, 793. [Google Scholar] [CrossRef]
- Abdullah, M.M.H.; Jew, S.; Jones, P.J.H. Health benefits and evaluation of healthcare cost savings if oils rich in monounsaturated fatty acids were substituted for conventional dietary oils in the United States. Nutr. Rev. 2017, 75, 163–174. [Google Scholar] [CrossRef]
- Abdullah, M.M.; Gyles, C.L.; Marinangeli, C.P.; Carlberg, J.G.; Jones, P.J. Dietary fibre intakes and reduction in functional constipation rates among Canadian adults: A cost-of-illness analysis. Food Nutr. Res. 2015, 59, 28646. [Google Scholar] [CrossRef] [PubMed]
- Kajla, P.; Sharma, A.; Sood, D.R. Flaxseed—A potential functional food source. J. Food Sci. Technol. 2015, 5, 1857–1871. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, K.; Verma, N.; Trivedi, R.; Bhardwaj, S. Effect of essential fatty acid blend on circadian variations of ambulatory blood pressure in patients with essential hypertension and coronary artery disease risk markers. J. Hum. Hypertens. 2022, 36, 289–298. [Google Scholar] [CrossRef] [PubMed]
- Mahmudiono, T.; Jasim, S.A.; Karim, Y.S.; Bokov, D.O.; Abdelbasset, W.K.; Akhmedov, K.S.; Yasin, G.; Thangavelu, L.; Mustafa, Y.F.; Shoukat, S.; et al. The effect of flaxseed oil consumtion on blood pressure among patients with metabolic syndrome and related disorders: A systematic review and meta-analysis of randomized clinical trials. Phytother. Res. 2022, 3, 3766–3773. [Google Scholar] [CrossRef] [PubMed]
- Akrami, A.; Nikaein, F.; Babajafari, S.; Faghih, S.; Yarmohammadi, H. Comparison of the effects of flaxseed oil and sunflower seed oil consumption on serum glucose, lipid profile, blood pressure, and lipid peroxidation in patients with metabolic syndrome. J. Clin. Lipidol. 2018, 12, 70–77. [Google Scholar] [CrossRef]
- Javidi, A.; Mozaffari-Khosravi, H.; Nadjarzadeh, A.; Dehghani, A.; Eftekhari, M.H. The effect of flaxseed powder on insulin resistance indices and blood pressure in prediabetic individuals: A randomized controlled clinical trial. J. Res. Med. Sci. 2016, 21, 70. [Google Scholar] [PubMed]
- Prasad, K. Importance of flaxseed and its components in the management of hypertension. Int. J. Angiol. 2019, 28, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Ursoniu, S.; Sahebkar, A.; Andrica, F.; Serban, C.; Banach, M. Effects of flaxseed supplements on blood pressure: A systematic review and meta-analysis of controlled clinical trial. Clin. Nutr. 2016, 35, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Khalesi, S.; Irwin, C.; Schubert, M. Flaxseed consumption may reduce blood pressure: A systematic review and meta-analysis of controlled trials. J. Nutr. 2015, 145, 758–765. [Google Scholar] [CrossRef]
- Law, M.; Wald, N.; Morris, J.; Jordan, R. Value of low dose combination treatment with blood pressure lowering drugs: Analysis of 354 randomised trials. Brit. Med. J. 2003, 326, 1427. [Google Scholar] [CrossRef]
- Canadian Institute for Health Information. Public and Private Sector Health Expenditures by Use of Funds. Available online: https://www.cihi.ca/en/public-and-private-sector-health-expenditures-by-use-of-funds (accessed on 5 July 2023).
- Government of Canada. Canadian Chronic Disease Surveillance System. Available online: https://health-infobase.canada.ca/ccdss/data-tool/Index?G=00&V=2&M=4&Y=2017 (accessed on 9 February 2024).
- DeGuire, J.; Clarke, J.; Rouleau, K.; Roy, J.; Bushnik, T. Blood pressure and hypertension. Health Rep. 2019, 30, 14–21. [Google Scholar] [PubMed]
- Cardoso Carraro, J.C.; Dantas, M.I.D.S.; Espeschit, A.C.R.; Martino, H.S.D.; Ribeiro, S.M.R. Flaxseed and human health: Reviewing benefits and adverse effects. Food Rev. Int. 2012, 28, 203–230. [Google Scholar] [CrossRef]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Savica, V.; Bellinghieri, G.; Kopple, J. The effect of nutrition on blood pressure. Annu. Rev. Nutr. 2010, 30, 365–401. [Google Scholar] [CrossRef] [PubMed]
- Chay, J.; Jafar, T.H.; Su, R.J.; Shirore, R.M.; Tan, N.C.; Finkelstein, E.A. Cost-effectiveness of a multicomponent primary care intervention for hypertension. J. Am. Heart Assoc. 2024, 13, e033631. [Google Scholar] [CrossRef]
- Bryant, K.B.; Rao, A.S.; Cohen, L.P.; Dandan, N.; Kronish, I.M.; Barai, N.; Fontil, V.; Zhang, Y.; Moran, A.E.; Bellows, B.K. Effectiveness and cost-effectiveness of team-based care for hypertension: A meta-analysis and simulation study. Hypertension 2023, 80, 1199–1208. [Google Scholar] [CrossRef]
- Rodriguez-Leyva, D.; Rodriguez-Portelles, A.; Weighell, W.; Guzman, R.; Maddaford, T.G.; Pierce, G.N. The effects of dietary flaxseed on cardiac arrhythmias and claudication in patients with peripheral arterial disease. Can. J. Physiol. Pharmacol. 2019, 97, 557–561. [Google Scholar] [CrossRef]



| Age Group | Per Capita Costs 1 (CAD) |
|---|---|
| 18–44 years | 2095.73 |
| 45–54 years | 2305.30 |
| 55–64 years | 2514.87 |
| 65–74 years | 2934.02 |
| Intake Success Rate (%) | Estimated Cost-Savings (CAD) |
|---|---|
| 5 | 96.28 (79.44, 113.12) |
| 10 | 195.12 (178.17, 212.07) |
| 25 | 490.39 (474.78,506) |
| 50 | 985.15 (970.31, 999.98) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clair, L.; Kashton, J.; Pierce, G.N. Estimating the Potential Health Care Cost-Savings from a Flax-Based Treatment for Hypertension. Nutrients 2024, 16, 2638. https://doi.org/10.3390/nu16162638
Clair L, Kashton J, Pierce GN. Estimating the Potential Health Care Cost-Savings from a Flax-Based Treatment for Hypertension. Nutrients. 2024; 16(16):2638. https://doi.org/10.3390/nu16162638
Chicago/Turabian StyleClair, Luc, Jared Kashton, and Grant N. Pierce. 2024. "Estimating the Potential Health Care Cost-Savings from a Flax-Based Treatment for Hypertension" Nutrients 16, no. 16: 2638. https://doi.org/10.3390/nu16162638
APA StyleClair, L., Kashton, J., & Pierce, G. N. (2024). Estimating the Potential Health Care Cost-Savings from a Flax-Based Treatment for Hypertension. Nutrients, 16(16), 2638. https://doi.org/10.3390/nu16162638





