What Is the Relationship between Chronotype and Disordered Eating in Adolescents? The EHDLA Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Study Variables
2.2.1. Chronotype (Independent Variable)
2.2.2. Disordered Eating (Dependent Variable)
2.3. Covariates
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Treasure, J.; Duarte, T.A.; Schmidt, U. Eating Disorders. Lancet 2020, 395, 899–911. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association (Ed.) Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR, 5th ed.; Text Revision; American Psychiatric Association Publishing: Washington, DC, USA, 2022; ISBN 978-0-89042-575-6. [Google Scholar]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems (ICD); World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- GBD 2019 Mental Disorders Collaborators. Global, Regional, and National Burden of 12 Mental Disorders in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Chesney, E.; Goodwin, G.M.; Fazel, S. Risks of All-Cause and Suicide Mortality in Mental Disorders: A Meta-Review. World Psychiatry 2014, 13, 153–160. [Google Scholar] [CrossRef]
- Smink, F.R.E.; van Hoeken, D.; Hoek, H.W. Epidemiology of Eating Disorders: Incidence, Prevalence and Mortality Rates. Curr. Psychiatry Rep. 2012, 14, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Galmiche, M.; Déchelotte, P.; Lambert, G.; Tavolacci, M.P. Prevalence of Eating Disorders over the 2000–2018 Period: A Systematic Literature Review. Am. J. Clin. Nutr. 2019, 109, 1402–1413. [Google Scholar] [CrossRef] [PubMed]
- Lindvall Dahlgren, C.; Wisting, L. Transitioning from DSM-IV to DSM-5: A systematic review of eating disorder prevalence assessment. Int. J. Eat. Disord. 2016, 49, 975–997. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Marti, C.N.; Rohde, P. Prevalence, Incidence, Impairment, and Course of the Proposed DSM-5 Eating Disorder Diagnoses in an 8-Year Prospective Community Study of Young Women. J. Abnorm. Psychol. 2013, 122, 445–457. [Google Scholar] [CrossRef] [PubMed]
- Forrest, L.N.; Smith, A.R.; Swanson, S.A. Characteristics of Seeking Treatment among U.S. Adolescents with Eating Disorders. Int. J. Eat. Disord. 2017, 50, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Attia, E.; Guarda, A.S. Prevention and Early Identification of Eating Disorders. JAMA 2022, 327, 1029. [Google Scholar] [CrossRef]
- Toni, G.; Berioli, M.; Cerquiglini, L.; Ceccarini, G.; Grohmann, U.; Principi, N.; Esposito, S. Eating Disorders and Disordered Eating Symptoms in Adolescents with Type 1 Diabetes. Nutrients 2017, 9, 906. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Wall, M.; Guo, J.; Story, M.; Haines, J.; Eisenberg, M. Obesity, Disordered Eating, and Eating Disorders in a Longitudinal Study of Adolescents: How Do Dieters Fare 5 Years Later? J. Am. Diet. Assoc. 2006, 106, 559–568. [Google Scholar] [CrossRef]
- Quick, V.M.; Byrd-Bredbenner, C.; Neumark-Sztainer, D. Chronic Illness and Disordered Eating: A Discussion of the Literature. Adv. Nutr. 2013, 4, 277–286. [Google Scholar] [CrossRef]
- López-Gil, J.F.; García-Hermoso, A.; Smith, L.; Firth, J.; Trott, M.; Mesas, A.E.; Jiménez-López, E.; Gutiérrez-Espinoza, H.; Tárraga-López, P.J.; Victoria-Montesinos, D. Global Proportion of Disordered Eating in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2023, 177, 363–372. [Google Scholar] [CrossRef]
- Adelantado-Renau, M.; Beltran-Valls, M.R.; Toledo-Bonifás, M.; Bou-Sospedra, C.; Pastor, M.C.; Moliner-Urdiales, D. The Risk of Eating Disorders and Academic Performance in Adolescents: DADOS Study. Nutr. Hosp. 2018, 35, 1201–1207. [Google Scholar] [CrossRef]
- López-Gil, J.F.; Jiménez-López, E.; Fernández-Rodríguez, R.; Garrido-Miguel, M.; Victoria-Montesinos, D.; Gutiérrez-Espinoza, H.; Tárraga-López, P.J.; Mesas, A.E. Prevalence of Disordered Eating and Its Associated Factors from a Socioecological Approach among a Sample of Spanish Adolescents: The EHDLA Study. Int. J. Public Health 2023, 68, 1605820. [Google Scholar] [CrossRef]
- Veses, A.M.; Martínez-Gómez, D.; Gómez-Martínez, S.; Vicente-Rodriguez, G.; Castillo, R.; Ortega, F.B.; González-Gross, M.; Calle, M.E.; Veiga, O.L.; Marcos, A.; et al. Physical Fitness, Overweight and the Risk of Eating Disorders in Adolescents. The AVENA and AFINOS Studies. Pediatr. Obes. 2014, 9, 1–9. [Google Scholar] [CrossRef]
- Phoi, Y.Y.; Rogers, M.; Bonham, M.P.; Dorrian, J.; Coates, A.M. A Scoping Review of Chronotype and Temporal Patterns of Eating of Adults: Tools Used, Findings, and Future Directions. Nutr. Res. Rev. 2022, 35, 112–135. [Google Scholar] [CrossRef]
- Adan, A.; Archer, S.N.; Hidalgo, M.P.; Di Milia, L.; Natale, V.; Randler, C. Circadian Typology: A Comprehensive Review. Chronobiol. Int. 2012, 29, 1153–1175. [Google Scholar] [CrossRef]
- Natale, V.; Cicogna, P. Morningness-Eveningness Dimension: Is It Really a Continuum? Personal. Individ. Differ. 2002, 32, 809–816. [Google Scholar] [CrossRef]
- Roenneberg, T.; Kuehnle, T.; Juda, M.; Kantermann, T.; Allebrandt, K.; Gordijn, M.; Merrow, M. Epidemiology of the Human Circadian Clock. Sleep Med. Rev. 2007, 11, 429–438. [Google Scholar] [CrossRef]
- Randler, C.; Faßl, C.; Kalb, N. From Lark to Owl: Developmental Changes in Morningness-Eveningness from New-Borns to Early Adulthood. Sci. Rep. 2017, 7, 45874. [Google Scholar] [CrossRef]
- Fischer, D.; Lombardi, D.A.; Marucci-Wellman, H.; Roenneberg, T. Chronotypes in the US–Influence of Age and Sex. PLoS ONE 2017, 12, e0178782. [Google Scholar] [CrossRef]
- Karan, M.; Bai, S.; Almeida, D.M.; Irwin, M.R.; McCreath, H.; Fuligni, A.J. Sleep–Wake Timings in Adolescence: Chronotype Development and Associations with Adjustment. J. Youth Adolesc. 2021, 50, 628–640. [Google Scholar] [CrossRef]
- Rodríguez-Cortés, F.J.; Morales-Cané, I.; Rodríguez-Muñoz, P.M.; Cappadona, R.; De Giorgi, A.; Manfredini, R.; Rodríguez-Borrego, M.A.; Fabbian, F.; López-Soto, P.J. Individual Circadian Preference, Eating Disorders and Obesity in Children and Adolescents: A Dangerous Liaison? A Systematic Review and a Meta-Analysis. Children 2022, 9, 167. [Google Scholar] [CrossRef]
- Fabbian, F.; Zucchi, B.; De Giorgi, A.; Tiseo, R.; Boari, B.; Salmi, R.; Cappadona, R.; Gianesini, G.; Bassi, E.; Signani, F.; et al. Chronotype, Gender and General Health. Chronobiol. Int. 2016, 33, 863–882. [Google Scholar] [CrossRef]
- López-Soto, P.J.; Fabbian, F.; Cappadona, R.; Zucchi, B.; Manfredini, F.; García-Arcos, A.; Carmona-Torres, J.M.; Manfredini, R.; Rodríguez-Borrego, M.A. Chronotype, Nursing Activity, and Gender: A Systematic Review. J. Adv. Nurs. 2019, 75, 734–748. [Google Scholar] [CrossRef]
- Bhar, D.; Bagepally, B.S.; Rakesh, B. Association between Chronotype and Cardio-Vascular Disease Risk Factors: A Systematic Review and Meta-Analysis. Clin. Epidemiol. Glob. Health 2022, 16, 101108. [Google Scholar] [CrossRef]
- Lotti, S.; Pagliai, G.; Asensi, M.T.; Giangrandi, I.; Colombini, B.; Sofi, F.; Dinu, M. Morning Chronotype Is Associated with Higher Adherence to the Mediterranean Diet in a Sample of Italian Adults. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 2086–2092. [Google Scholar] [CrossRef]
- Vetrani, C.; Barrea, L.; Verde, L.; Sarno, G.; Docimo, A.; De Alteriis, G.; Savastano, S.; Colao, A.; Muscogiuri, G. Evening Chronotype Is Associated with Severe NAFLD in Obesity. Int. J. Obes. 2022, 46, 1638–1643. [Google Scholar] [CrossRef]
- Ekiz Erim, S.; Sert, H. The Relationship between Chronotype and Obesity: A Systematic Review. Chronobiol. Int. 2023, 40, 529–541. [Google Scholar] [CrossRef]
- Mazri, F.H.; Manaf, Z.A.; Shahar, S.; Mat Ludin, A.F. The Association between Chronotype and Dietary Pattern among Adults: A Scoping Review. Int. J. Environ. Res. Public Health 2019, 17, 68. [Google Scholar] [CrossRef]
- Sirtoli, R.; Mata, G.D.G.; Rodrigues, R.; Martinez-Vizcaíno, V.; López-Gil, J.F.; Guidoni, C.M.; Mesas, A.E. Is Evening Chronotype Associated with Higher Alcohol Consumption? A Systematic Review and Meta-Analysis. Chronobiol. Int. 2023, 40, 1467–1479. [Google Scholar] [CrossRef]
- López-Gil, J.F.; Moreno-Galarraga, L.; Mesas, A.E.; Gutiérrez-Espinoza, H.; López-Bueno, R.; Gaffin, J.M. Is Chronotype Linked with Adherence to the Mediterranean Diet among Adolescents? The EHDLA Study. Pediatr. Res. 2023, 94, 2070–2076. [Google Scholar] [CrossRef]
- Kivelä, L.; Papadopoulos, M.R.; Antypa, N. Chronotype and Psychiatric Disorders. Curr. Sleep Med. Rep. 2018, 4, 94–103. [Google Scholar] [CrossRef]
- Zou, H.; Zhou, H.; Yan, R.; Yao, Z.; Lu, Q. Chronotype, Circadian Rhythm, and Psychiatric Disorders: Recent Evidence and Potential Mechanisms. Front. Neurosci. 2022, 16, 811771. [Google Scholar] [CrossRef]
- Esin, K.; Ayyıldız, F. Relationship Between Chronotype With Emotional Eating, Eating Disorder Risk and Depression: A Cross-Sectional Study. Sage Open 2024, 14, 21582440231224221. [Google Scholar] [CrossRef]
- Amicis, R.D.; Galasso, L.; Cavallaro, R.; Mambrini, S.P.; Castelli, L.; Montaruli, A.; Roveda, E.; Esposito, F.; Leone, A.; Foppiani, A.; et al. Sex Differences in the Relationship between Chronotype and Eating Behaviour: A Focus on Binge Eating and Food Addiction. Nutrients 2023, 15, 4580. [Google Scholar] [CrossRef]
- Romo-Nava, F.; Blom, T.J.; Guerdjikova, A.; Winham, S.J.; Cuellar-Barboza, A.B.; Nunez, N.A.; Singh, B.; Biernacka, J.M.; Frye, M.A.; McElroy, S.L. Evening Chronotype, Disordered Eating Behavior, and Poor Dietary Habits in Bipolar Disorder. Acta Psychiatr. Scand. 2020, 142, 58–65. [Google Scholar] [CrossRef]
- López-Gil, J.F. The Eating Healthy and Daily Life Activities (EHDLA) Study. Children 2022, 9, 370. [Google Scholar] [CrossRef]
- Carskadon, M.A.; Vieira, C.; Acebo, C. Association between Puberty and Delayed Phase Preference. Sleep 1993, 16, 258–262. [Google Scholar] [CrossRef]
- Díaz-Morales, J.F.; de León, M.C.D.; Sorroche, M.G. Validity of the Morningness-Eveningness Scale for Children among Spanish Adolescents. Chronobiol. Int. 2007, 24, 435–447. [Google Scholar] [CrossRef]
- Díaz-Morales, J.F.; Sorroche, M.G. Morningness-Eveningness in Adolescents. Span. J. Psychol. 2008, 11, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Campayo, J.; Sanz-Carrillo, C.; Ibañez, J.A.; Lou, S.; Solano, V.; Alda, M. Validation of the Spanish Version of the SCOFF Questionnaire for the Screening of Eating Disorders in Primary Care. J. Psychosom. Res. 2005, 59, 51–55. [Google Scholar] [CrossRef]
- Muro-Sans, P.; Amador-Campos, J.A.; Morgan, J.F. The SCOFF-c: Psychometric Properties of the Catalan Version in a Spanish Adolescent Sample. J. Psychosom. Res. 2008, 64, 81–86. [Google Scholar] [CrossRef]
- Currie, C.; Molcho, M.; Boyce, W.; Holstein, B.; Torsheim, T.; Richter, M. Researching Health Inequalities in Adolescents: The Development of the Health Behaviour in School-Aged Children (HBSC) Family Affluence Scale. Soc. Sci. Med. 2008, 66, 1429–1436. [Google Scholar] [CrossRef]
- Segura-Díaz, J.M.; Barranco-Ruiz, Y.; Saucedo-Araujo, R.G.; Aranda-Balboa, M.J.; Cadenas-Sanchez, C.; Migueles, J.H.; Saint-Maurice, P.F.; Ortega, F.B.; Welk, G.J.; Herrador-Colmenero, M.; et al. Feasibility and Reliability of the Spanish Version of the Youth Activity Profile Questionnaire (YAP-Spain) in Children and Adolescents. J. Sports Sci. 2021, 39, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in Children and Adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, I.T.; Ballart, J.F.; Pastor, G.C.; Jordà, E.B.; Val, V.A. [Validation of a short questionnaire on frequency of dietary intake: Reproducibility and validity]. Nutr. Hosp. 2008, 23, 242–252. [Google Scholar]
- Maechler, M.; Rousseeuw, P.; Croux, C.; Todorov, V.; Ruckstuhl, A.; Salibian-Barrera, M.; Verbeke, T.; Koller, M.; Conceicao, E.L.; di Palma, M.A. Robustbase: Basic Robust Statistics. Available online: https://cran.r-project.org/web/packages/robustbase/index.html (accessed on 26 March 2024).
- Riccobono, G.; Pompili, A.; Iannitelli, A.; Pacitti, F. The Relationship between Night Eating Syndrome, Depression and Chronotype in a Non-Clinical Adolescent Population. Riv. Psichiatr. 2019, 54, 115–119. [Google Scholar] [CrossRef]
- Kandeger, A.; Egilmez, U.; Sayin, A.A.; Selvi, Y. The Relationship between Night Eating Symptoms and Disordered Eating Attitudes via Insomnia and Chronotype Differences. Psychiatry Res. 2018, 268, 354–357. [Google Scholar] [CrossRef]
- Harb, A.; Levandovski, R.; Oliveira, C.; Caumo, W.; Allison, K.C.; Stunkard, A.; Hidalgo, M.P. Night Eating Patterns and Chronotypes: A Correlation with Binge Eating Behaviors. Psychiatry Res. 2012, 200, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social Jetlag: Misalignment of Biological and Social Time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef]
- Touitou, Y. Adolescent Sleep Misalignment: A Chronic Jet Lag and a Matter of Public Health. J. Physiol.-Paris 2013, 107, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T. How Can Social Jetlag Affect Health? Nat. Rev. Endocrinol. 2023, 19, 383–384. [Google Scholar] [CrossRef] [PubMed]
- Lukoševičiūtė-Barauskienė, J.; Žemaitaitytė, M.; Šūmakarienė, V.; Šmigelskas, K. Adolescent Perception of Mental Health: It’s Not Only about Oneself, It’s about Others Too. Children 2023, 10, 1109. [Google Scholar] [CrossRef] [PubMed]
- Carpio-Arias, T.V.; Solís Manzano, A.M.; Sandoval, V.; Vinueza-Veloz, A.F.; Rodríguez Betancourt, A.; Betancourt Ortíz, S.L.; Vinueza-Veloz, M.F. Relationship between Perceived Stress and Emotional Eating. A Cross Sectional Study. Clin. Nutr. ESPEN 2022, 49, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.; Greene, G.; Schwartz-Barcott, D. Perceptions of Emotional Eating Behavior. A Qualitative Study of College Students. Appetite 2013, 60, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Polańska, S.; Karykowska, A.; Pawelec, Ł. Associations between Chronotype and Physical Activity and Well-Being in Adults. Chronobiol. Int. 2024, 41, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Sempere-Rubio, N.; Aguas, M.; Faubel, R. Association between Chronotype, Physical Activity and Sedentary Behaviour: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 9646. [Google Scholar] [CrossRef] [PubMed]
- Uccella, S.; Cordani, R.; Salfi, F.; Gorgoni, M.; Scarpelli, S.; Gemignani, A.; Geoffroy, P.A.; De Gennaro, L.; Palagini, L.; Ferrara, M.; et al. Sleep Deprivation and Insomnia in Adolescence: Implications for Mental Health. Brain Sci. 2023, 13, 569. [Google Scholar] [CrossRef]
- Haupt, S.; Eckstein, M.L.; Wolf, A.; Zimmer, R.T.; Wachsmuth, N.B.; Moser, O. Eat, Train, Sleep—Retreat? Hormonal Interactions of Intermittent Fasting, Exercise and Circadian Rhythm. Biomolecules 2021, 11, 516. [Google Scholar] [CrossRef]
- Klok, M.D.; Jakobsdottir, S.; Drent, M.L. The Role of Leptin and Ghrelin in the Regulation of Food Intake and Body Weight in Humans: A Review. Obes. Rev. 2007, 8, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-L.; Schnepp, J.; Tucker, R.M. Increased Hunger, Food Cravings, Food Reward, and Portion Size Selection after Sleep Curtailment in Women Without Obesity. Nutrients 2019, 11, 663. [Google Scholar] [CrossRef] [PubMed]
- Monteleone, P.; Maj, M. Dysfunctions of Leptin, Ghrelin, BDNF and Endocannabinoids in Eating Disorders: Beyond the Homeostatic Control of Food Intake. Psychoneuroendocrinology 2013, 38, 312–330. [Google Scholar] [CrossRef] [PubMed]
- Chao, A.M.; Jastreboff, A.M.; White, M.A.; Grilo, C.M.; Sinha, R. Stress, Cortisol, and Other Appetite-related Hormones: Prospective Prediction of 6-month Changes in Food Cravings and Weight. Obesity 2017, 25, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Huang, J.; Yang, M. Association between Chronotype and Sleep Quality among Chinese College Students: The Role of Bedtime Procrastination and Sleep Hygiene Awareness. Int. J. Environ. Res. Public Health 2022, 20, 197. [Google Scholar] [CrossRef] [PubMed]
- Alhola, P.; Polo-Kantola, P. Sleep Deprivation: Impact on Cognitive Performance. Neuropsychiatr. Dis. Treat. 2007, 3, 553–567. [Google Scholar] [PubMed]
- Higgs, S.; Spetter, M.S. Cognitive Control of Eating: The Role of Memory in Appetite and Weight Gain. Curr. Obes. Rep. 2018, 7, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Zerón-Rugerio, M.F.; Cambras, T.; Izquierdo-Pulido, M. Social Jet Lag Associates Negatively with the Adherence to the Mediterranean Diet and Body Mass Index among Young Adults. Nutrients 2019, 11, 1756. [Google Scholar] [CrossRef]
- Greer, S.M.; Goldstein, A.N.; Walker, M.P. The Impact of Sleep Deprivation on Food Desire in the Human Brain. Nat. Commun. 2013, 4, 2259. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Dutil, C. Lack of Sleep as a Contributor to Obesity in Adolescents: Impacts on Eating and Activity Behaviors. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 103. [Google Scholar] [CrossRef]
- Fleig, D.; Randler, C. Association between Chronotype and Diet in Adolescents Based on Food Logs. Eat. Behav. 2009, 10, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.Y.-M.; Yeung, W.-F.; Ho, Y.-S.; Ho, F.Y.Y.; Chung, K.F.; Lee, R.L.T.; Lam, M.Y.; Chen, S. Associations between the Chronotypes and Eating Habits of Hong Kong School-Aged Children. Int. J. Environ. Res. Public Health 2020, 17, 2583. [Google Scholar] [CrossRef] [PubMed]
- Arora, T.; Taheri, S. Associations among Late Chronotype, Body Mass Index and Dietary Behaviors in Young Adolescents. Int. J. Obes. 2015, 39, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Golley, R.K.; Maher, C.A.; Matricciani, L.; Olds, T.S. Sleep Duration or Bedtime? Exploring the Association between Sleep Timing Behaviour, Diet and BMI in Children and Adolescents. Int. J. Obes. 2013, 37, 546–551. [Google Scholar] [CrossRef]
- Tardy, A.-L.; Pouteau, E.; Marquez, D.; Yilmaz, C.; Scholey, A. Vitamins and Minerals for Energy, Fatigue and Cognition: A Narrative Review of the Biochemical and Clinical Evidence. Nutrients 2020, 12, 228. [Google Scholar] [CrossRef]
- Polivy, J. Psychological Consequences of Food Restriction. J. Am. Diet. Assoc. 1996, 96, 589–592. [Google Scholar] [CrossRef]
- Elran-Barak, R.; Bromberg, M.; Shimony, T.; Dichtiar, R.; Mery, N.; Nitsan, L.; Keinan-Boker, L. Disordered Eating among Arab and Jewish Youth in Israel: The Role of Eating Dinner with the Family. Isr. J. Health Policy Res. 2020, 9, 27. [Google Scholar] [CrossRef]
- al Balushi, R.; Carciofo, R. Chronotype, Binge-Eating, and Depression: The Mediating Effect of Skipping Breakfast. Biol. Rhythm Res. 2023, 54, 707–721. [Google Scholar] [CrossRef]
- López-Gil, J.F.; Smith, L.; López-Bueno, R.; Tárraga-López, P.J. Breakfast and Psychosocial Behavioural Problems in Young Population: The Role of Status, Place, and Habits. Front. Nutr. 2022, 9, 871238. [Google Scholar] [CrossRef]
- Lee, G.; Han, K.; Kim, H. Risk of Mental Health Problems in Adolescents Skipping Meals: The Korean National Health and Nutrition Examination Survey 2010 to 2012. Nurs. Outlook 2017, 65, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Suarez-Albor, C.L.; Galletta, M.; Gómez-Bustamante, E.M. Factors Associated with Eating Disorders in Adolescents: A Systematic Review. Acta Biomed. Atenei Parm. 2022, 93, e2022253. [Google Scholar] [CrossRef]
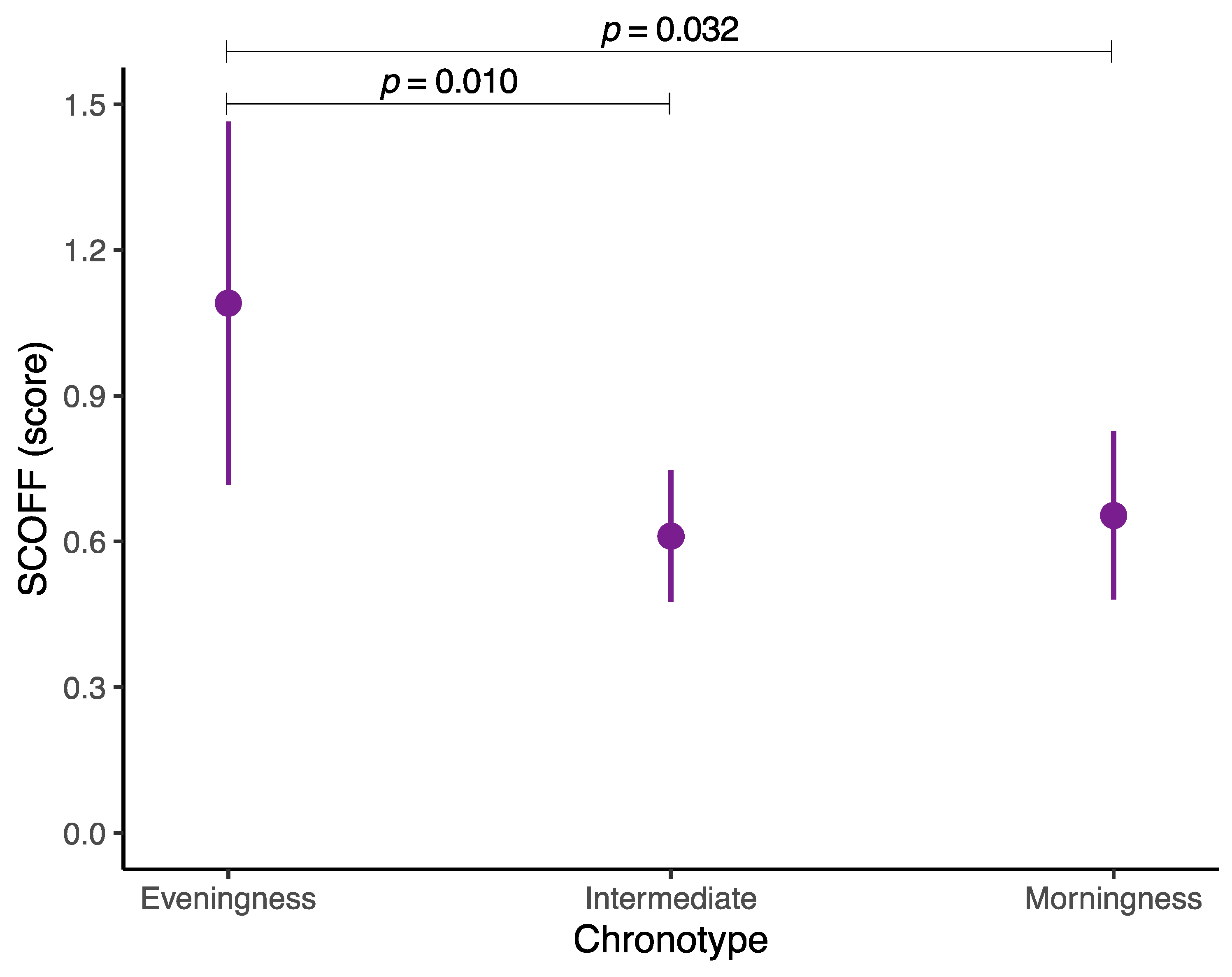
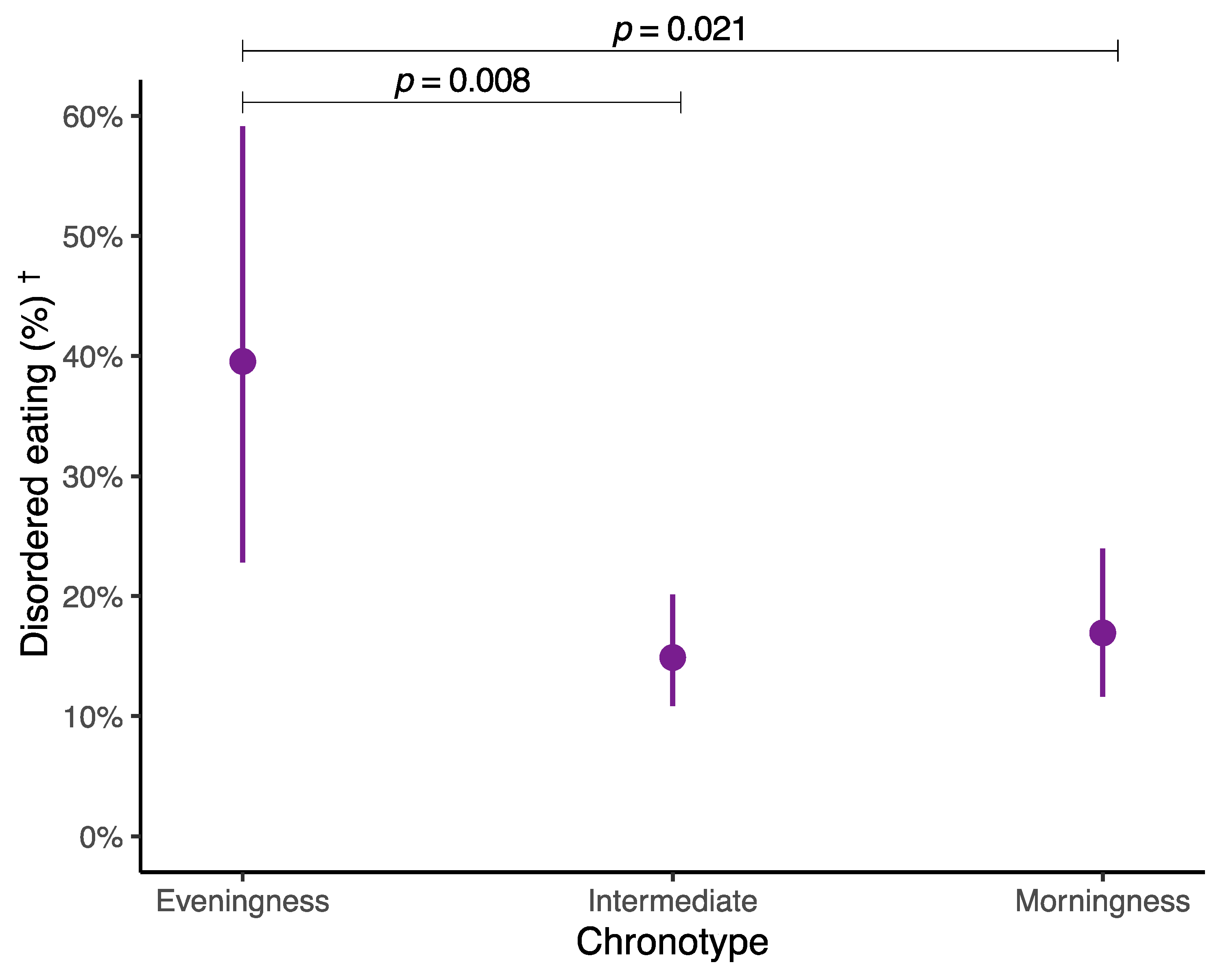
| Chronotype | ||||
|---|---|---|---|---|
| Variable | Eveningness | Intermediate | Morningness | |
| Participants | n (%) | 39 (5.5) | 483 (68.7) | 181 (25.7) |
| Sex | Boys (%) | 13 (33.3) | 194 (40.2) | 100 (55.2) |
| Girls (%) | 26 (66.7) | 289 (59.8) | 81 (44.8) | |
| Age (years) | Median (IQR) | 13.0 (1.5) | 14.0 (2.0) | 13.0 (3.0) |
| FAS-III (score) | Median (IQR) | 8.0 (3.0) | 8.0 (2.5) | 8.0 (3.0) |
| YAP-S physical activity (score) | Median (IQR) | 2.4 (0.8) | 2.6 (0.8) | 2.8 (0.9) |
| YAP-S sedentary behaviors (score) | Median (IQR) | 3.2 (0.8) | 2.6 (0.8) | 2.4 (0.8) |
| Body mass index (kg/m2) | Median (IQR) | 22.1 (6.6) | 21.6 (5.6) | 21.7 (6.8) |
| KIDMED (score) | Median (IQR) | 4.0 (3.0) | 6.0 (3.0) | 8.0 (3.0) |
| Energy intake (kcal) | Median (IQR) | 2929.0 (1540.2) | 2590.9 (1458.7) | 2448.2 (1290.7) |
| SCOFF (score) | Median (IQR) | 2.0 (3.0) | 1.0 (2.0) | 1.0 (2.0) |
| Disordered eating (%) † | No (%) | 17 (43.6) | 345 (71.4) | 128 (70.7) |
| Yes (%) | 22 (56.4) | 138 (28.6) | 53 (29.3) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Gil, J.F.; Olivares-Arancibia, J.; Yáñez-Sepúlveda, R.; Martínez-López, M.F. What Is the Relationship between Chronotype and Disordered Eating in Adolescents? The EHDLA Study. Nutrients 2024, 16, 2576. https://doi.org/10.3390/nu16162576
López-Gil JF, Olivares-Arancibia J, Yáñez-Sepúlveda R, Martínez-López MF. What Is the Relationship between Chronotype and Disordered Eating in Adolescents? The EHDLA Study. Nutrients. 2024; 16(16):2576. https://doi.org/10.3390/nu16162576
Chicago/Turabian StyleLópez-Gil, José Francisco, Jorge Olivares-Arancibia, Rodrigo Yáñez-Sepúlveda, and Mayra Fernanda Martínez-López. 2024. "What Is the Relationship between Chronotype and Disordered Eating in Adolescents? The EHDLA Study" Nutrients 16, no. 16: 2576. https://doi.org/10.3390/nu16162576
APA StyleLópez-Gil, J. F., Olivares-Arancibia, J., Yáñez-Sepúlveda, R., & Martínez-López, M. F. (2024). What Is the Relationship between Chronotype and Disordered Eating in Adolescents? The EHDLA Study. Nutrients, 16(16), 2576. https://doi.org/10.3390/nu16162576








