Identifying and Analyzing Low Energy Availability in Athletes: The Role of Biomarkers and Red Blood Cell Turnover
Abstract
1. Introduction
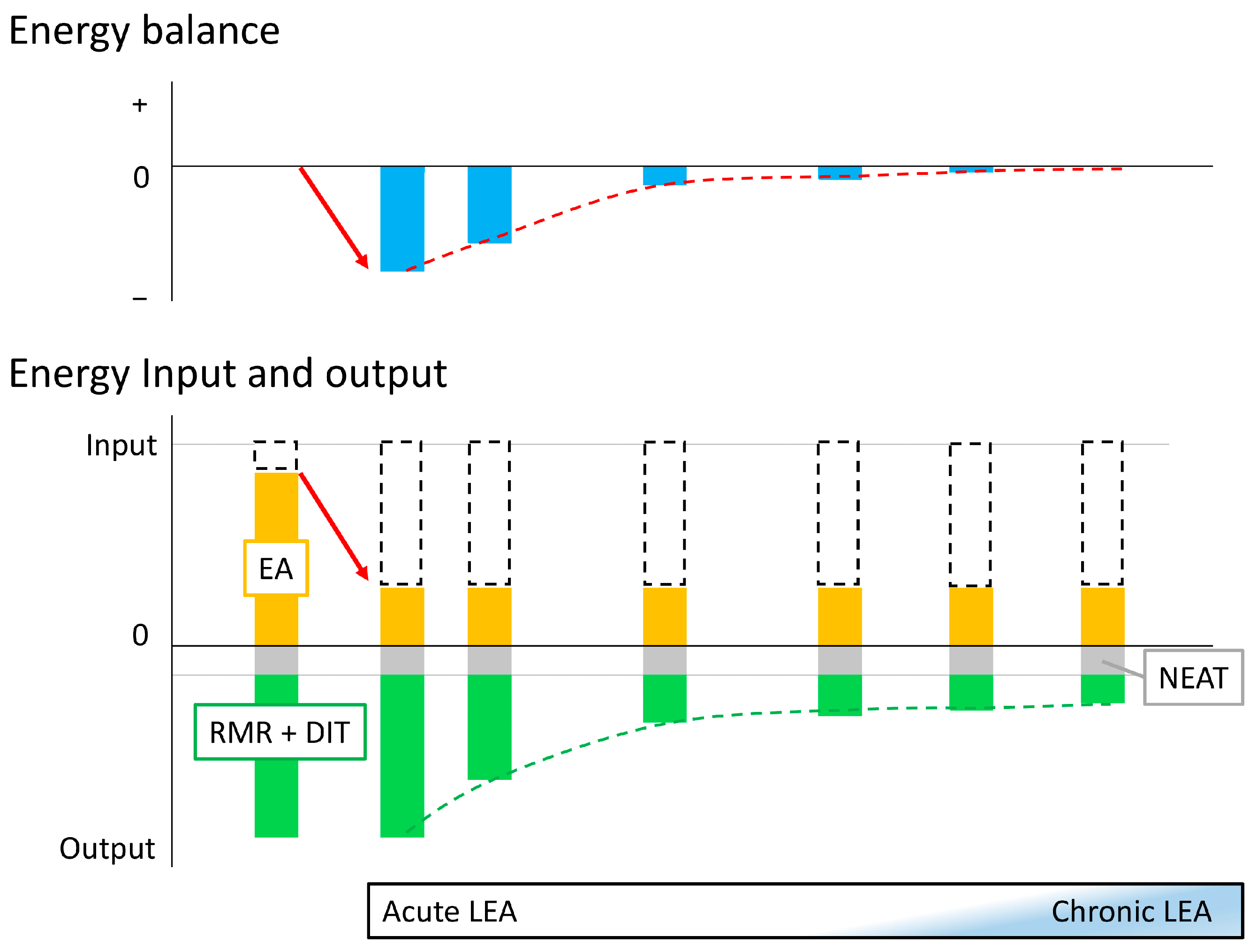
2. Metabolic Adaptation to Low Energy Availability
3. Influence of Low Energy Availability on Athletic Performance
4. Influence of Low Energy Availability on Health
5. Importance of Diagnosing Low Energy Availability
6. Diagnosing Acute Low Energy Availability
| Gender | Acute LEA | Ref. | Chronic LEA | Ref. |
|---|---|---|---|---|
| Both | Triiodothyronine (T3) ↓ | [61,62,63,64,65,75,76] | Triiodothyronine (T3) ↓ | [77,78,79,80] |
| IGF-1 ↓ | [63,64,75] | IGF-1 ↓ | [77,78,81] | |
| Leptin ↓ | [62,65,67,68,69] | Testosterone ↓ | [78,80,81] | |
| Luteinizing hormone (LH) ↓ | [62,71] | |||
| Insulin ↓ | [61,62,63,64,65,66,67,82] | |||
| Glucose ↓ | [61,62,65,66,67] | |||
| Protein synthesis ↓ | [37] | |||
| Growth hormone (GH) ↑ | [62,65,66,72,82] | |||
| Female | Follicle-stimulating hormone (FSH) ↑ | [66] | Leptin ↓ | [80,83,84,85] |
| Osteogenic markers ↓ | [68,69,73] | Ghrelin ↑ | [84,86] | |
| Bone resorption markers ↑ | [68,69,73] | Estradiol ↓ | [77,85] | |
| Beta-hydroxybutyrate ↑ | [61,62,65,76] | Progesterone ↓ | [77] | |
| Forearm resting blood flow | [76] | Luteinizing hormone (LH) ↓ | [83] | |
| Male | Muscle glycogen ↓ | [50,51] | Cholesterol ↓ | [78] |
| Hemoglobin ↓ | [75,87,88] | Insulin ↓ | [78] | |
| Cortisol ↑ | [63,82] | Thyroxine (T4) ↓ | [82] | |
| IGFBP-1 ↑ | [63] | |||
| Aldosterone ↑ | [63] | |||
| Free fatty acids ↓ | [63] | |||
| Iron ↓ & transferrin saturation ↓ | [48,77,78,79,80] | |||
| Testosterone ↓ | [82] | |||
| Sleep efficiency, N3 stage proportion ↓ | [89] | |||
| Wake after sleep onset ↑ | [89] |
7. Diagnosing Chronic Low Energy Availability
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Baker, E.R. Menstrual Dysfunction and Hormonal Status in Athletic Women: A Review. Fertil. Steril. 1981, 36, 691–696. [Google Scholar] [CrossRef] [PubMed]
- Hale, R.W. Exercise, Sports, and Menstrual Dysfunction. Clin. Obstet. Gynecol. 1983, 26, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Yeager, K.K.; Agostini, R.; Nattiv, A.; Drinkwater, B. The Female Athlete Triad: Disordered Eating, Amenorrhea, Osteoporosis. Med. Sci. Sports Exerc. 1993, 25, 775–777. [Google Scholar] [CrossRef] [PubMed]
- Williams, N.I.; Helmreich, D.L.; Parfitt, D.B.; Caston-Balderrama, A.; Cameron, J.L. Evidence for a Causal Role of Low Energy Availability in the Induction of Menstrual Cycle Disturbances during Strenuous Exercise Training. J. Clin. Endocrinol. Metab. 2001, 86, 5184–5193. [Google Scholar] [CrossRef] [PubMed]
- Nattiv, A.; Loucks, A.B.; Manore, M.M.; Sanborn, C.F.; Sundgot-Borgen, J.; Warren, M.P. The Female Athlete Triad. Med. Sci. Sports Exerc. 2007, 39, 1867–1882. [Google Scholar] [CrossRef] [PubMed]
- Mountjoy, M.; Sundgot-Borgen, J.; Burke, L.; Carter, S.; Constantini, N.; Lebrun, C.; Meyer, N.; Sherman, R.; Steffen, K.; Budgett, R.; et al. The IOC Consensus Statement: Beyond the Female Athlete Triad-Relative Energy Deficiency in Sport (RED-S). Br. J. Sports Med. 2014, 48, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Maughan, R.J.; Burke, L.M.; Dvorak, J.; Larson-Meyer, D.E.; Peeling, P.; Phillips, S.M.; Rawson, E.S.; Walsh, N.P.; Garthe, I.; Geyer, H.; et al. IOC Consensus Statement: Dietary Supplements and the High-Performance Athlete. Int. J. Sport. Nutr. Exerc. Metab. 2018, 28, 104–125. [Google Scholar] [CrossRef] [PubMed]
- Mountjoy, M.; Sundgot-Borgen, J.; Burke, L.; Carter, S.; Constantini, N.; Lebrun, C.; Meyer, N.; Sherman, R.; Steffen, K.; Budgett, R.; et al. Authors’ 2015 Additions to the IOC Consensus Statement: Relative Energy Deficiency in Sport (RED-S). Br. J. Sports Med. 2015, 49, 417–420. [Google Scholar] [CrossRef]
- De Souza, M.J.; Williams, N.I.; Nattiv, A.; Joy, E.; Misra, M.; Loucks, A.B.; Matheson, G.; Olmsted, M.P.; Barrack, M.; Mallinson, R.J.; et al. Misunderstanding the Female Athlete Triad: Refuting the IOC Consensus Statement on Relative Energy Deficiency in Sport (RED-S). Br. J. Sports Med. 2014, 48, 1461–1465. [Google Scholar] [CrossRef]
- Nattiv, A.; De Souza, M.J.; Koltun, K.J.; Misra, M.; Kussman, A.; Williams, N.I.; Barrack, M.T.; Kraus, E.; Joy, E.; Fredericson, M. The Male Athlete Triad-A Consensus Statement From the Female and Male Athlete Triad Coalition Part 1: Definition and Scientific Basis. Clin. J. Sport. Med. 2021, 31, 335–348. [Google Scholar] [CrossRef]
- Logue, D.; Madigan, S.M.; Delahunt, E.; Heinen, M.; Mc Donnell, S.-J.; Corish, C.A. Low Energy Availability in Athletes: A Review of Prevalence, Dietary Patterns, Physiological Health, and Sports Performance. Sports Med. 2018, 48, 73–96. [Google Scholar] [CrossRef] [PubMed]
- Logue, D.M.; Madigan, S.M.; Melin, A.; Delahunt, E.; Heinen, M.; Mc Donnell, S.J.; Corish, C.A. Low Energy Availability in Athletes 2020: An Updated Narrative Review of Prevalence, Risk, Within-Day Energy Balance, Knowledge, and Impact on Sports Performance. Nutrients 2020, 12, 835. [Google Scholar] [CrossRef] [PubMed]
- Loucks, A.B. Low Energy Availability in the Marathon and Other Endurance Sports. Sports Med. 2007, 37, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Mountjoy, M.; Sundgot-Borgen, J.K.; Burke, L.M.; Ackerman, K.E.; Blauwet, C.; Constantini, N.; Lebrun, C.; Lundy, B.; Melin, A.K.; Meyer, N.L.; et al. IOC Consensus Statement on Relative Energy Deficiency in Sport (RED-S): 2018 Update. Br. J. Sports Med. 2018, 52, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Mountjoy, M.; Ackerman, K.E.; Bailey, D.M.; Burke, L.M.; Constantini, N.; Hackney, A.C.; Heikura, I.A.; Melin, A.; Pensgaard, A.M.; Stellingwerff, T.; et al. 2023 International Olympic Committee’s (IOC) Consensus Statement on Relative Energy Deficiency in Sport (REDs). Br. J. Sports Med. 2023, 57, 1073–1097. [Google Scholar] [CrossRef] [PubMed]
- Salamunes, A.C.C.; Williams, N.I.; De Souza, M.J. Are Menstrual Disturbances Associated with an Energy Availability Threshold? A Critical Review of the Evidence. Appl. Physiol. Nutr. Metab. 2024, 49, 584–598. [Google Scholar] [CrossRef] [PubMed]
- Fredericson, M.; Kussman, A.; Misra, M.; Barrack, M.T.; De Souza, M.J.; Kraus, E.; Koltun, K.J.; Williams, N.I.; Joy, E.; Nattiv, A. The Male Athlete Triad-A Consensus Statement from the Female and Male Athlete Triad Coalition Part II: Diagnosis, Treatment, and Return-to-Play. Clin. J. Sport. Med. 2021, 31, 349–366. [Google Scholar] [CrossRef] [PubMed]
- Areta, J.L.; Taylor, H.L.; Koehler, K. Low Energy Availability: History, Definition and Evidence of Its Endocrine, Metabolic and Physiological Effects in Prospective Studies in Females and Males. Eur. J. Appl. Physiol. 2021, 121, 1–21. [Google Scholar] [CrossRef]
- Areta, J.L. Physical Performance during Energy Deficiency in Humans: An Evolutionary Perspective. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2023, 284, 111473. [Google Scholar] [CrossRef] [PubMed]
- Dipla, K.; Kraemer, R.R.; Constantini, N.W.; Hackney, A.C. Relative Energy Deficiency in Sports (RED-S): Elucidation of Endocrine Changes Affecting the Health of Males and Females. Hormones 2021, 20, 35–47. [Google Scholar] [CrossRef]
- Melin, A.K.; Heikura, I.A.; Tenforde, A.; Mountjoy, M. Energy Availability in Athletics: Health, Performance, and Physique. Int. J. Sport. Nutr. Exerc. Metab. 2019, 29, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Melin, A.K.; Areta, J.L.; Heikura, I.A.; Stellingwerff, T.; Torstveit, M.K.; Hackney, A.C. Direct and Indirect Impact of Low Energy Availability on Sports Performance. Scand. J. Med. Sci. Sports 2024, 34, e14327. [Google Scholar] [CrossRef] [PubMed]
- Popp, K.L.; Cooke, L.M.; Bouxsein, M.L.; Hughes, J.M. Impact of Low Energy Availability on Skeletal Health in Physically Active Adults. Calcif. Tissue Int. 2022, 110, 605–614. [Google Scholar] [CrossRef] [PubMed]
- Shirley, M.K.; Longman, D.P.; Elliott-Sale, K.J.; Hackney, A.C.; Sale, C.; Dolan, E. A Life History Perspective on Athletes with Low Energy Availability. Sports Med. 2022, 52, 1223–1234. [Google Scholar] [CrossRef] [PubMed]
- Scrimshaw, N.S.; Hussein, M.A.; Murray, E.; Rand, W.M.; Young, V.R. Protein Requirements of Man: Variations in Obligatory Urinary and Fecal Nitrogen Losses in Young Men. J. Nutr. 1972, 102, 1595–1604. [Google Scholar] [CrossRef]
- Quevedo, M.R.; Price, G.M.; Halliday, D.; Pacy, P.J.; Millward, D.J. Nitrogen Homoeostasis in Man: Diurnal Changes in Nitrogen Excretion, Leucine Oxidation and Whole Body Leucine Kinetics during a Reduction from a High to a Moderate Protein Intake. Clin. Sci. 1994, 86, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Waterlow, J.C. Protein Turnover with Special Reference to Man. Q. J. Exp. Physiol. 1984, 69, 409–438. [Google Scholar] [CrossRef] [PubMed]
- Welle, S.; Nair, K.S. Relationship of Resting Metabolic Rate to Body Composition and Protein Turnover. Am. J. Physiol. 1990, 258, E990–E998. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Bosy-Westphal, A. Adaptive Thermogenesis with Weight Loss in Humans. Obesity 2013, 21, 218–228. [Google Scholar] [CrossRef]
- Bosy-Westphal, A.; Kossel, E.; Goele, K.; Later, W.; Hitze, B.; Settler, U.; Heller, M.; Glüer, C.C.; Heymsfield, S.B.; Müller, M.J. Contribution of Individual Organ Mass Loss to Weight Loss–Associated Decline in Resting Energy Expenditure. Am. J. Clin. Nutr. 2009, 90, 993–1001. [Google Scholar] [CrossRef]
- Koehler, K.; Williams, N.I.; Mallinson, R.J.; Southmayd, E.A.; Allaway, H.C.M.; de Souza, M.J. Low Resting Metabolic Rate in Exercise-Associated Amenorrhea Is Not Due to a Reduced Proportion of Highly Active Metabolic Tissue Compartments. Am. J. Physiol. Endocrinol. Metab. 2016, 311, E480–E487. [Google Scholar] [CrossRef] [PubMed]
- Faintuch, J.; Soriano, F.G.; Ladeira, J.P.; Janiszewski, M.; Velasco, I.T.; Gama-Rodrigues, J.J. Changes in Body Fluid and Energy Compartments during Prolonged Hunger Strike. Rev. Hosp. Clin. Fac. Med. 2000, 55, 47–54. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Drew, M.; Vlahovich, N.; Hughes, D.; Appaneal, R.; Burke, L.M.; Lundy, B.; Rogers, M.; Toomey, M.; Watts, D.; Lovell, G.; et al. Prevalence of Illness, Poor Mental Health and Sleep Quality and Low Energy Availability Prior to the 2016 Summer Olympic Games. Br. J. Sports Med. 2018, 52, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, K.E.; Holtzman, B.; Cooper, K.M.; Flynn, E.F.; Bruinvels, G.; Tenforde, A.S.; Popp, K.L.; Simpkin, A.J.; Parziale, A.L. Low Energy Availability Surrogates Correlate with Health and Performance Consequences of Relative Energy Deficiency in Sport. Br. J. Sports Med. 2019, 53, 628–633. [Google Scholar] [CrossRef] [PubMed]
- Keay, N.; Francis, G.; Hind, K. Low Energy Availability Assessed by a Sport-Specific Questionnaire and Clinical Interview Indicative of Bone Health, Endocrine Profile and Cycling Performance in Competitive Male Cyclists. BMJ Open Sport. Exerc. Med. 2018, 4, e000424. [Google Scholar] [CrossRef] [PubMed]
- Woods, A.L.; Rice, A.J.; Garvican-Lewis, L.A.; Wallett, A.M.; Lundy, B.; Rogers, M.A.; Welvaert, M.; Halson, S.; McKune, A.; Thompson, K.G. The Effects of Intensified Training on Resting Metabolic Rate (RMR), Body Composition and Performance in Trained Cyclists. PLoS ONE 2018, 13, e0191644. [Google Scholar] [CrossRef] [PubMed]
- Areta, J.L.; Burke, L.M.; Camera, D.M.; West, D.W.D.; Crawshay, S.; Moore, D.R.; Stellingwerff, T.; Phillips, S.M.; Hawley, J.A.; Coffey, V.G. Reduced Resting Skeletal Muscle Protein Synthesis Is Rescued by Resistance Exercise and Protein Ingestion Following Short-Term Energy Deficit. Am. J. Physiol. Endocrinol. Metab. 2014, 306, E989–E997. [Google Scholar] [CrossRef] [PubMed]
- Pasiakos, S.M.; Vislocky, L.M.; Carbone, J.W.; Altieri, N.; Konopelski, K.; Freake, H.C.; Anderson, J.M.; Ferrando, A.A.; Wolfe, R.R.; Rodriguez, N.R. Acute Energy Deprivation Affects Skeletal Muscle Protein Synthesis and Associated Intracellular Signaling Proteins in Physically Active Adults. J. Nutr. 2010, 140, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Hector, A.J.; McGlory, C.; Damas, F.; Mazara, N.; Baker, S.K.; Phillips, S.M. Pronounced Energy Restriction with Elevated Protein Intake Results in No Change in Proteolysis and Reductions in Skeletal Muscle Protein Synthesis That Are Mitigated by Resistance Exercise. FASEB J. 2018, 32, 265–275. [Google Scholar] [CrossRef]
- Murphy, C.H.; Churchward-Venne, T.A.; Mitchell, C.J.; Kolar, N.M.; Kassis, A.; Karagounis, L.G.; Burke, L.M.; Hawley, J.A.; Phillips, S.M. Hypoenergetic Diet-Induced Reductions in Myofibrillar Protein Synthesis Are Restored with Resistance Training and Balanced Daily Protein Ingestion in Older Men. Am. J. Physiol. Endocrinol. Metab. 2015, 308, E734–E743. [Google Scholar] [CrossRef]
- Murphy, C.; Koehler, K. Energy Deficiency Impairs Resistance Training Gains in Lean Mass but Not Strength: A Meta-Analysis and Meta-Regression. Scand. J. Med. Sci. Sports 2022, 32, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Areta, J.L. Case Study: Resumption of Eumenorrhea in Parallel With High Training Load After 4 Years of Menstrual Dysfunction: A 5-Year Follow-Up of an Elite Female Cyclist. Int. J. Sport. Nutr. Exerc. Metab. 2020, 30, 229–234. [Google Scholar] [CrossRef]
- Burke, L.M.; Whitfield, J.; Ross, M.L.R.; Tee, N.; Sharma, A.P.; King, A.J.; Heikura, I.A.; Morabito, A.; McKay, A.K.A. Short Severe Energy Restriction with Refueling Reduces Body Mass without Altering Training-Associated Performance Improvement. Med. Sci. Sports Exerc. 2023, 55, 1487–1498. [Google Scholar] [CrossRef] [PubMed]
- Langan-Evans, C.; Germaine, M.; Artukovic, M.; Oxborough, D.L.; Areta, J.L.; Close, G.L.; Morton, J.P. The Psychological and Physiological Consequences of Low Energy Availability in a Male Combat Sport Athlete. Med. Sci. Sports Exerc. 2021, 53, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Stellingwerff, T. Case Study: Body Composition Periodization in an Olympic-Level Female Middle-Distance Runner Over a 9-Year Career. Int. J. Sport. Nutr. Exerc. Metab. 2018, 28, 428–433. [Google Scholar] [CrossRef]
- Tornberg, Å.B.; Melin, A.; Koivula, F.M.; Johansson, A.; Skouby, S.; Faber, J.; Sjödin, A. Reduced Neuromuscular Performance in Amenorrheic Elite Endurance Athletes. Med. Sci. Sports Exerc. 2017, 49, 2478–2485. [Google Scholar] [CrossRef] [PubMed]
- Fudge, B.W.; Westerterp, K.R.; Kiplamai, F.K.; Onywera, V.O.; Boit, M.K.; Kayser, B.; Pitsiladis, Y.P. Evidence of Negative Energy Balance Using Doubly Labelled Water in Elite Kenyan Endurance Runners Prior to Competition. Br. J. Nutr. 2006, 95, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Tokuyama, M.; Seino, J.; Sakuraba, K.; Suzuki, Y. Possible Association of Energy Availability with Transferrin Saturation and Serum Iron during Summer Camp in Male Collegiate Rugby Players. Nutrients 2021, 13, 2963. [Google Scholar] [CrossRef] [PubMed]
- Areta, J.L.; Hopkins, W.G. Skeletal Muscle Glycogen Content at Rest and During Endurance Exercise in Humans: A Meta-Analysis. Sports Med. 2018, 48, 2091–2102. [Google Scholar] [CrossRef]
- Ishibashi, A.; Kojima, C.; Tanabe, Y.; Iwayama, K.; Hiroyama, T.; Tsuji, T.; Kamei, A.; Goto, K.; Takahashi, H. Effect of Low Energy Availability during Three Consecutive Days of Endurance Training on Iron Metabolism in Male Long Distance Runners. Physiol. Rep. 2020, 8, e14494. [Google Scholar] [CrossRef]
- Kojima, C.; Ishibashi, A.Y.A.; Tanabe, Y.; Iwayama, K.; Kamei, A.; Takahashi, H.; Goto, K. Muscle Glycogen Content during Endurance Training under Low Energy Availability. Med. Sci. Sports Exerc. 2020, 52, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Olsson, K.-E.; Saltin, B. Variation in Total Body Water with Muscle Glycogen Changes in Man. Acta Physiol. Scand. 1970, 80, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Sherman, W.M.; Plyley, M.J.; Sharp, R.L.; Van Handel, P.J.; McAllister, R.M.; Fink, W.J.; Costill, D.L. Muscle Glycogen Storage and Its Relationship with Water. Int. J. Sports Med. 1982, 3, 22–24. [Google Scholar] [CrossRef] [PubMed]
- Leiter, L.A.; Marliss, E.B. Survival during Fasting May Depend on Fat as Well as Protein Stores. JAMA 1982, 248, 2306–2307. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.M.; Slater, G.J.; Matthews, J.J.; Langan-Evans, C.; Horswill, C.A. ACSM Expert Consensus Statement on Weight Loss in Weight-Category Sports. Curr. Sports Med. Rep. 2021, 20, 199–217. [Google Scholar] [CrossRef] [PubMed]
- Lakicevic, N.; Roklicer, R.; Bianco, A.; Mani, D.; Paoli, A.; Trivic, T.; Ostojic, S.M.; Milovancev, A.; Maksimovic, N.; Drid, P. Effects of Rapid Weight Loss on Judo Athletes: A Systematic Review. Nutrients 2020, 12, 1220. [Google Scholar] [CrossRef] [PubMed]
- Nohara, T.; Kamei, T.; Ohta, A. Accelerated Decrease in Bone Mineral Density in Women Aged 52–57 Years. Tohoku J. Exp. Med. 2006, 210, 341–347. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hoonpongsimanon, S.; Santipapmonthon, M.; Chuntana, M. Spinal Bone Mineral Density by Quantitative Computed Tomography in Thais Compared with Westerners. J. Med. Assoc. Thai 2005, 88, 1666–1673. [Google Scholar] [PubMed]
- Pumarino, H.; González, P.; Oviedo, S.; Lillo, R. Density and Bone Mineral Content and Their Relation to Anthropometric Parameters in a Normal Chilean Population. A Study with Women. Rev. Med. Chil. 1991, 119, 279–286. [Google Scholar]
- Dolan, E.; Varley, I.; Ackerman, K.E.; Pereira, R.M.R.; Elliott-Sale, K.J.; Sale, C. The Bone Metabolic Response to Exercise and Nutrition. Exerc. Sport. Sci. Rev. 2020, 48, 49–58. [Google Scholar] [CrossRef]
- Loucks, A.B.; Verdun, M. Slow Restoration of LH Pulsatility by Refeeding in Energetically Disrupted Women. Am. J. Physiol. 1998, 275, R1218–R1226. [Google Scholar] [CrossRef] [PubMed]
- Loucks, A.B. The Response of Luteinizing Hormone Pulsatility to 5 Days of Low Energy Availability Disappears by 14 Years of Gynecological Age. J. Clin. Endocrinol. Metab. 2006, 91, 3158–3164. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.L.; Heist, K.; DePaoli, A.M.; Veldhuis, J.D.; Mantzoros, C.S. The Role of Falling Leptin Levels in the Neuroendocrine and Metabolic Adaptation to Short-Term Starvation in Healthy Men. J. Clin. Investig. 2003, 111, 1409–1421. [Google Scholar] [CrossRef] [PubMed]
- Loucks, A.B.; Heath, E.M. Dietary Restriction Reduces Luteinizing Hormone (LH) Pulse Frequency during Waking Hours and Increases LH Pulse Amplitude during Sleep in Young Menstruating Women. J. Clin. Endocrinol. Metab. 1994, 78, 910–915. [Google Scholar] [CrossRef] [PubMed]
- Loucks, A.B.; Thuma, J.R. Luteinizing Hormone Pulsatility Is Disrupted at a Threshold of Energy Availability in Regularly Menstruating Women. J. Clin. Endocrinol. Metab. 2003, 88, 297–311. [Google Scholar] [CrossRef] [PubMed]
- Loucks, A.B.; Verdun, M.; Heath, E.M. Low Energy Availability, Not Stress of Exercise, Alters LH Pulsatility in Exercising Women. J. Appl. Physiol. 1998, 84, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Koehler, K.; Hoerner, N.R.; Gibbs, J.C.; Zinner, C.; Braun, H.; De Souza, M.J.; Schaenzer, W. Low Energy Availability in Exercising Men Is Associated with Reduced Leptin and Insulin but Not with Changes in Other Metabolic Hormones. J. Sports Sci. 2016, 34, 1921–1929. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, M.; Elliott-Sale, K.J.; Parsons, A.; Tang, J.C.Y.; Greeves, J.P.; Fraser, W.D.; Sale, C. Effects of Reduced Energy Availability on Bone Metabolism in Women and Men. Bone 2017, 105, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, M.; Martin, D.; Colgan, H.; Cooper, S.; Greeves, J.P.; Tang, J.C.Y.; Fraser, W.D.; Elliott-Sale, K.J.; Sale, C. Bone Metabolic Responses to Low Energy Availability Achieved by Diet or Exercise in Active Eumenorrheic Women. Bone 2018, 114, 181–188. [Google Scholar] [CrossRef]
- Hilton, L.K.; Loucks, A.B. Low Energy Availability, Not Exercise Stress, Suppresses the Diurnal Rhythm of Leptin in Healthy Young Women. Am. J. Physiol. Endocrinol. Metab. 2000, 278, E43–E49. [Google Scholar] [CrossRef]
- Bergendahl, M.; Aloi, J.A.; Iranmanesh, A.; Mulligan, T.M.; Veldhuis, J.D. Fasting Suppresses Pulsatile Luteinizing Hormone (LH) Secretion and Enhances Orderliness of LH Release in Young but Not Older Men. J. Clin. Endocrinol. Metab. 1998, 83, 1967–1975. [Google Scholar] [CrossRef]
- Murphy, C.; Koehler, K. Caloric Restriction Induces Anabolic Resistance to Resistance Exercise. Eur. J. Appl. Physiol. 2020, 120, 1155–1164. [Google Scholar] [CrossRef]
- Ihle, R.; Loucks, A.B. Dose-Response Relationships between Energy Availability and Bone Turnover in Young Exercising Women. J. Bone Miner. Res. 2004, 19, 1231–1240. [Google Scholar] [CrossRef] [PubMed]
- Tenforde, A.S.; Barrack, M.T.; Nattiv, A.; Fredericson, M. Parallels with the Female Athlete Triad in Male Athletes. Sports Med. 2016, 46, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Jurov, I.; Keay, N.; Rauter, S. Severe Reduction of Energy Availability in Controlled Conditions Causes Poor Endurance Performance, Impairs Explosive Power and Affects Hormonal Status in Trained Male Endurance Athletes. Appl. Sci. 2021, 11, 8618. [Google Scholar] [CrossRef]
- Hutson, M.J.; O’Donnell, E.; McConnell, K.; Chauntry, A.J.; Blagrove, R.C. Energy Availability Modulates Regional Blood Flow via Estrogen-Independent Pathways in Regularly Menstruating Young Women. Eur. J. Appl. Physiol. 2024. [Google Scholar] [CrossRef] [PubMed]
- Vanheest, J.L.; Rodgers, C.D.; Mahoney, C.E.; De Souza, M.J. Ovarian Suppression Impairs Sport Performance in Junior Elite Female Swimmers. Med. Sci. Sports Exerc. 2014, 46, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Friedl, K.E.; Moore, R.J.; Hoyt, R.W.; Marchitelli, L.J.; Martinez-Lopez, L.E.; Askew, E.W. Endocrine Markers of Semistarvation in Healthy Lean Men in a Multistressor Environment. J. Appl. Physiol. 2000, 88, 1820–1830. [Google Scholar] [CrossRef]
- Santtila, M.; Kyröläinen, H.; Häkkinen, K. Serum Hormones in Soldiers after Basic Training: Effect of Added Strength or Endurance Regimens. Aviat. Space Environ. Med. 2009, 80, 615–620. [Google Scholar] [CrossRef]
- Hulmi, J.J.; Isola, V.; Suonpää, M.; Järvinen, N.J.; Kokkonen, M.; Wennerström, A.; Nyman, K.; Perola, M.; Ahtiainen, J.P.; Häkkinen, K. The Effects of Intensive Weight Reduction on Body Composition and Serum Hormones in Female Fitness Competitors. Front. Physiol. 2017, 7, 689. [Google Scholar] [CrossRef]
- Hooper, D.R.; Kraemer, W.J.; Saenz, C.; Schill, K.E.; Focht, B.C.; Volek, J.S.; Maresh, C.M. The Presence of Symptoms of Testosterone Deficiency in the Exercise-Hypogonadal Male Condition and the Role of Nutrition. Eur. J. Appl. Physiol. 2017, 117, 1349–1357. [Google Scholar] [CrossRef] [PubMed]
- Kyröläinen, H.; Karinkanta, J.; Santtila, M.; Koski, H.; Mäntysaari, M.; Pullinen, T. Hormonal Responses during a Prolonged Military Field Exercise with Variable Exercise Intensity. Eur. J. Appl. Physiol. 2008, 102, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Perakakis, N.; Upadhyay, J.; Ghaly, W.; Chen, J.; Chrysafi, P.; Anastasilakis, A.D.; Mantzoros, C.S. Regulation of the Activins-Follistatins-Inhibins Axis by Energy Status: Impact on Reproductive Function. Metabolism 2018, 85, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Schaal, K.; Tiollier, E.; Le Meur, Y.; Casazza, G.; Hausswirth, C. Elite Synchronized Swimmers Display Decreased Energy Availability during Intensified Training. Scand. J. Med. Sci. Sports 2017, 27, 925–934. [Google Scholar] [CrossRef] [PubMed]
- Schaal, K.; VanLoan, M.D.; Hausswirth, C.; Casazza, G.A. Decreased Energy Availability during Training Overload Is Associated with Non-Functional Overreaching and Suppressed Ovarian Function in Female Runners. Appl. Physiol. Nutr. Metab. 2021, 46, 1179–1188. [Google Scholar] [CrossRef]
- Leidy, H.J.; Dougherty, K.A.; Frye, B.R.; Duke, K.M.; Williams, N.I. Twenty-Four-Hour Ghrelin Is Elevated after Calorie Restriction and Exercise Training in Non-Obese Women. Obesity 2007, 15, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Jurov, I.; Keay, N.; Spudić, D.; Rauter, S. Inducing Low Energy Availability in Trained Endurance Male Athletes Results in Poorer Explosive Power. Eur. J. Appl. Physiol. 2022, 122, 503–513. [Google Scholar] [CrossRef]
- Jurov, I.; Keay, N.; Rauter, S. Reducing Energy Availability in Male Endurance Athletes: A Randomized Trial with a Three-Step Energy Reduction. J. Int. Soc. Sports Nutr. 2022, 19, 179–195. [Google Scholar] [CrossRef]
- Saidi, O.; Souabni, M.; Del Sordo, G.C.; Maviel, C.; Peyrel, P.; Maso, F.; Vercruyssen, F.; Duché, P. Association between Low Energy Availability (LEA) and Impaired Sleep Quality in Young Rugby Players. Nutrients 2024, 16, 609. [Google Scholar] [CrossRef]
- Torres-McGehee, T.M.; Emerson, D.M.; Flanscha-Jacobson, A.; Uriegas, N.A.; Moore, E.M.; Smith, A.B. Energy Availability, Mental Health, and Sleep Patterns of Athletic Trainers. J. Athl. Train. 2023, 58, 788–795. [Google Scholar] [CrossRef]
- Risso, A.; Ciana, A.; Achilli, C.; Antonutto, G.; Minetti, G. Neocytolysis: None, One or Many? A Reappraisal and Future Perspectives. Front. Physiol. 2014, 5, 54. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Arias, C.F.; Arias, C.F. How Do Red Blood Cells Know When to Die? R. Soc. Open Sci. 2017, 4, 160850. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.; Lew, V.L. PIEZO1 and the Mechanism of the Long Circulatory Longevity of Human Red Blood Cells. PLoS Comput. Biol. 2021, 17, e1008496. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Sakuraba, K.; Sunohara, M.; Takaragawa, M. Variations in Iron Status Linked to Menstrual Cycles among Japanese Female Athletes. Int. J. Anal. Bio-Sci. 2018, 6, 45–50. [Google Scholar]
- Torstveit, M.K.; Fahrenholtz, I.; Stenqvist, T.B.; Sylta, O.; Melin, A. Within-Day Energy Deficiency and Metabolic Perturbation in Male Endurance Athletes. Int. J. Sport. Nutr. Exerc. Metab. 2018, 28, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Hackney, A.C.; Sharp, R.L.; Runyan, W.S.; Ness, R.J. Relationship of Resting Prolactin and Testosterone in Males during Intensive Training. Br. J. Sports Med. 1989, 23, 194. [Google Scholar] [CrossRef] [PubMed]
- Hackney, A.C.; Fahrner, C.L.; Gulledge, T.P. Basal Reproductive Hormonal Profiles Are Altered in Endurance Trained Men. J. Sports Med. Phys. Fit. 1998, 38, 138–141. [Google Scholar]
- Hennigar, S.R.; Berryman, C.E.; Harris, M.N.; Karl, J.P.; Lieberman, H.R.; McClung, J.P.; Rood, J.C.; Pasiakos, S.M. Testosterone Administration During Energy Deficit Suppresses Hepcidin and Increases Iron Availability for Erythropoiesis. J. Clin. Endocrinol. Metab. 2020, 105, E1316–E1321. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suzuki, D.; Suzuki, Y. Identifying and Analyzing Low Energy Availability in Athletes: The Role of Biomarkers and Red Blood Cell Turnover. Nutrients 2024, 16, 2273. https://doi.org/10.3390/nu16142273
Suzuki D, Suzuki Y. Identifying and Analyzing Low Energy Availability in Athletes: The Role of Biomarkers and Red Blood Cell Turnover. Nutrients. 2024; 16(14):2273. https://doi.org/10.3390/nu16142273
Chicago/Turabian StyleSuzuki, Daisuke, and Yoshio Suzuki. 2024. "Identifying and Analyzing Low Energy Availability in Athletes: The Role of Biomarkers and Red Blood Cell Turnover" Nutrients 16, no. 14: 2273. https://doi.org/10.3390/nu16142273
APA StyleSuzuki, D., & Suzuki, Y. (2024). Identifying and Analyzing Low Energy Availability in Athletes: The Role of Biomarkers and Red Blood Cell Turnover. Nutrients, 16(14), 2273. https://doi.org/10.3390/nu16142273







