Panax notoginseng: Pharmacological Aspects and Toxicological Issues
Abstract
1. Introduction
2. Pharmacognosy of P. notoginseng
3. Pharmacokinetics of P. notoginseng
4. Pharmacodynamics of P. notoginseng
4.1. Immune System
4.2. Inflammation
4.3. Cardiovascular System
4.4. Central Nervous System
4.5. Metabolism
4.6. Cancer
5. Clinical Studies
6. Interactions and Precautions
7. Toxicology
8. Conclusions and Future Directions
Funding
Conflicts of Interest
References
- Dennehy, C.E.; Tsourounis, C. Botanicals (“Herbal medications”) & nutritional supplements. In Basic & Clinical Pharmacology, 8th ed.; Katzung, B.G., Ed.; Lange Medical Books/McGraw-Hill: New York, NY, USA, 2001; pp. 1088–1103. [Google Scholar]
- Tayeb, B.A.; Kusuma, I.Y.; Osman, A.A.M.; Minorics, R. Herbal compounds as promising therapeutic agents in precision medicine strategies for cancer: A systematic review. J. Integr. Med. 2024, 22, 137–162. [Google Scholar] [CrossRef]
- de Waure, C.; Bertola, C.; Baccarini, G.; Chiavarini, M.; Mancuso, C. Exploring the contribution of curcumin to cancer therapy: A systematic review of randomized controlled trials. Pharmaceutics 2023, 15, 1275. [Google Scholar] [CrossRef]
- Grujić-Milanović, J.; Rajković, J.; Milanović, S.; Jaćević, V.; Miloradović, Z.; Nežić, L.; Novaković, R. Natural substances vs. approved drugs in the treatment of main cardiovascular disorders-Is there a breakthrough? Antioxidants 2023, 12, 2088. [Google Scholar] [CrossRef]
- Islam, A.; Mishra, A.; Ahsan, R.; Fareha, S. Phytopharmaceuticals and herbal approaches to target neurodegenerative disorders. Drug Res. 2023, 73, 388–407. [Google Scholar] [CrossRef]
- Rahman, M.M.; Islam, M.R.; Shohag, S.; Hossain, M.E.; Rahaman, M.S.; Islam, F.; Ahmed, M.; Mitra, S.; Khandaker, M.U.; Idris, A.M.; et al. The multifunctional role of herbal products in the management of diabetes and obesity: A comprehensive review. Molecules 2022, 27, 1713. [Google Scholar] [CrossRef]
- Mhillaj, E.; Cuomo, V.; Trabace, L.; Mancuso, C. The heme oxygenase/biliverdin reductase system as effector of the neuroprotective outcomes of herb-based nutritional supplements. Front. Pharmacol. 2019, 10, 1298. [Google Scholar] [CrossRef]
- Mancuso, C.; Santangelo, R. Panax ginseng and Panax quinquefolius: From pharmacology to toxicology. Food. Chem. Toxicol. 2017, 107, 362–372. [Google Scholar] [CrossRef]
- Mancuso, C.; Santangelo, R. Ferulic acid: Pharmacological and toxicological aspects. Food. Chem. Toxicol. 2014, 65, 185–195. [Google Scholar] [CrossRef]
- Mancuso, C.; Siciliano, R.; Barone, E.; Preziosi, P. Natural substances and Alzheimer’s disease: From preclinical studies to evidence based medicine. Biochim. Biophys. Acta. 2012, 1822, 616–624. [Google Scholar] [CrossRef]
- Botanicals. Available online: https://www.efsa.europa.eu/en/topics/topic/botanicals (accessed on 8 April 2024).
- Botanical Medicine. Available online: https://www.takingcharge.csh.umn.edu/10-top-best-selling-botanicals-what-they-do (accessed on 8 April 2024).
- Baeg, I.H.; So, S.H. The world ginseng market and the ginseng (Korea). J. Ginseng Res. 2013, 37, 1–7. [Google Scholar] [CrossRef]
- Yun, T.K. Brief introduction of Panax ginseng C.A. Meyer. J. Korean Med. Sci. 2001, 16, S3–S5. [Google Scholar] [CrossRef]
- Xu, C.; Wang, W.; Wang, B.; Zhang, T.; Cui, X.; Pu, Y.; Li, N. Analytical methods and biological activities of Panax notoginseng saponins: Recent trends. J. Ethnopharmacol. 2019, 236, 443–465. [Google Scholar] [CrossRef]
- Global Notoginseng Suppliers. Available online: https://www.thetradevision.com/global/notoginseng-suppliers (accessed on 25 January 2024).
- Global Notoginseng Root Extract Market Report. Available online: https://www.marketresearchintellect.com/product/global-notoginseng-root-extract-market-size-and-forecast (accessed on 25 January 2024).
- Liu, H.; Lu, X.; Hu, Y.; Fan, X. Chemical constituents of Panax ginseng and Panax notoginseng explain why they differ in therapeutic efficacy. Pharmacol. Res. 2020, 161, 105263. [Google Scholar] [CrossRef]
- Chen, W.; Dang, Y.; Zhu, C. Simultaneous determination of three major bioactive saponins of Panax notoginseng using liquid chromatography-tandem mass spectrometry and a pharmacokinetic study. Chin. Med. 2010, 5, 12. [Google Scholar] [CrossRef]
- Wang, T.; Guo, R.; Zhou, G.; Zhou, X.; Kou, Z.; Sui, F.; Li, C.; Tang, L.; Wang, Z. Traditional uses, botany, phytochemistry, pharmacology and toxicology of Panax notoginseng (Burk.) F.H. Chen: A review. J. Ethnopharmacol. 2016, 188, 234–258. [Google Scholar] [CrossRef]
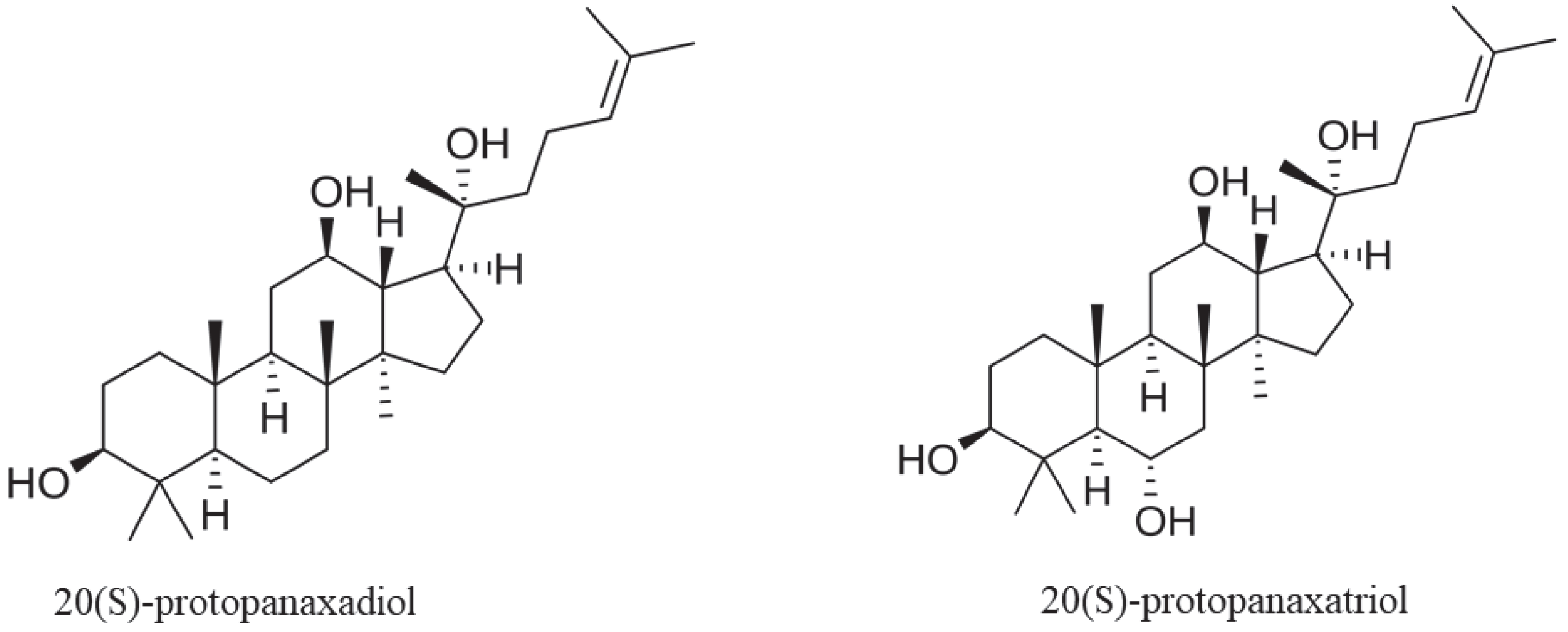
- Yang, W.Z.; Hu, Y.; Wu, W.Y.; Ye, M.; Guo, D.A. Saponins in the genus Panax L. (Araliaceae): A systematic review of their chemical diversity. Phytochemistry 2014, 106, 7–24. [Google Scholar] [CrossRef]
- Kim, D.H. Chemical Diversity of Panax ginseng, Panax quinquifolium, and Panax notoginseng. J. Ginseng Res. 2012, 36, 1–15. [Google Scholar] [CrossRef]
- Liu, J.; Wang, Y.; Qiu, L.; Yu, Y.; Wang, C. Saponins of Panax notoginseng: Chemistry, cellular targets and therapeutic opportunities in cardiovascular diseases. Expert. Opin. Investig. Drugs. 2014, 23, 523–539. [Google Scholar] [CrossRef]
- Xiong, Y.; Halima, M.; Che, X.; Zhang, Y.; Schaaf, M.J.M.; Li, M.; Gao, M.; Guo, L.; Huang, Y.; Cui, X.; et al. Steamed Panax notoginseng and its saponins inhibit the migration and induce the apoptosis of neutrophils in a zebrafish tail-fin amputation model. Front. Pharmacol. 2022, 13, 946900. [Google Scholar] [CrossRef]
- Sun, S.; Qi, L.W.; Du, G.J.; Mehendale, S.R.; Wang, C.Z.; Yuan, C.S. Red notoginseng: Higher ginsenoside content and stronger anticancer potential than Asian and American ginseng. Food. Chem. 2011, 125, 1299–1305. [Google Scholar] [CrossRef]
- Xiong, Y.; Chen, L.; Man, J.; Hu, Y.; Cui, X. Chemical and bioactive comparison of Panax notoginseng root and rhizome in raw and steamed forms. J. Ginseng Res. 2019, 43, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Zuo, Z.; Xu, F.; Wang, Y. Study of the suitable climate factors and geographical origins traceability of Panax notoginseng based on correlation analysis and spectral images combined with machine learning. Front. Plant. Sci. 2023, 13, 1009727. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Zhu, M.; Feng, Y.; Xu, H. Panax notoginseng-microbiota interactions: From plant cultivation to medicinal application. Phytomedicine 2023, 119, 154978. [Google Scholar] [CrossRef] [PubMed]
- Dennehy, C.E.; Tsourounis, C.T. Dietary supplements & herbal medications. In Basic & Clinical Pharmacology, 15th ed.; Katzung, B.G., Vanderah, T.W., Eds.; McGraw-Hill: New York, NY, USA, 2021; pp. 1179–1194. [Google Scholar]
- Lee, J.; Lee, E.; Kim, D.; Lee, J.; Yoo, J.; Koh, B. Studies on absorption, distribution and metabolism of ginseng in humans after oral administration. J. Ethnopharmacol. 2009, 122, 143–148. [Google Scholar] [CrossRef]
- Wang, H.Y.; Qi, L.W.; Wang, C.Z.; Li, P. Bioactivity enhancement of herbal supplements by intestinal microbiota focusing on ginsenosides. Am. J. Chin. Med. 2011, 39, 1103–1115. [Google Scholar] [CrossRef]
- Hu, Z.; Yang, J.; Cheng, C.; Huang, Y.; Du, F.; Wang, F.; Niu, W.; Xu, F.; Jiang, R.; Gao, X.; et al. Combinatorial metabolism notably affects human systemic exposure to ginsenosides from orally administered extract of Panax notoginseng roots (Sanqi). Drug. Metab. Dispos. 2013, 41, 1457–1469. [Google Scholar] [CrossRef]
- Wang, S.; Song, F.; Gu, H.; Shu, Z.; Wei, X.; Zhang, K.; Zhou, Y.; Jiang, L.; Wang, Z.; Li, J.; et al. Assess the diversity of gut microbiota among healthy adults for forensic application. Microb. Cell. Fact. 2022, 21, 46. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.Y.; Niu, W.; Olaleye, O.E.; Du, F.F.; Wang, F.Q.; Huang, Y.H.; Yuan, L.; Li, Y.F.; Liu, G.P.; Xu, F.; et al. Comparison of intramuscular and intravenous pharmacokinetics of ginsenosides in humans after dosing XueShuanTong, a lyophilized extract of Panax notoginseng roots. J. Ethnopharmacol. 2020, 253, 112658. [Google Scholar] [CrossRef]
- Pintusophon, S.; Niu, W.; Duan, X.N.; Olaleye, O.E.; Huang, Y.H.; Wang, F.Q.; Li, Y.F.; Yang, J.L.; Li, C. Intravenous formulation of Panax notoginseng root extract: Human pharmacokinetics of ginsenosides and potential for perpetrating drug interactions. Acta. Pharmacol. Sin. 2019, 40, 1351–1363. [Google Scholar] [CrossRef]
- Qi, L.W.; Wang, C.Z.; Du, G.J.; Zhang, Z.Y.; Calway, T.; Yuan, C.S. Metabolism of ginseng and its interactions with drugs. Curr. Drug. Metab. 2011, 12, 818–822. [Google Scholar] [CrossRef]
- Rhule, A.; Rase, B.; Smith, J.R.; Shepherd, D.M. Toll-like receptor ligand-induced activation of murine DC2.4 cells is attenuated by Panax notoginseng. J. Ethnopharmacol. 2008, 116, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.H.; Kuang, N.; Hu, W.Y.; Yin, D.; Wei, Y.Y.; Hu, T.J. The effect of Panax notoginseng saponins on oxidative stress induced by PCV2 infection in immune cells: In vitro and in vivo studies. J. Vet. Sci. 2020, 21, e61. [Google Scholar] [CrossRef]
- Yi, H.; Yu, Z.; Wang, Q.; Sun, Y.; Peng, J.; Cai, Y.; Ma, J.; Chen, Y.; Qin, C.; Cai, M.; et al. Panax notoginseng saponins suppress type 2 porcine reproductive and respiratory syndrome virus replication in vitro and enhance the immune effect of the live vaccine JXA1-R in piglets. Front. Vet. Sci. 2022, 9, 886058. [Google Scholar] [CrossRef]
- Zhao, D.; Chen, X.; Wang, L.; Zhang, J.; Lv, R.; Tan, L.; Chen, Y.; Tao, R.; Li, X.; Chen, Y.; et al. Improvement influenza vaccine immune responses with traditional Chinese medicine and its active ingredients. Front. Microbiol. 2023, 14, 1111886. [Google Scholar] [CrossRef]
- Chang, S.H.; Choi, Y.; Park, J.A.; Jung, D.S.; Shin, J.; Yang, J.H.; Ko, S.Y.; Kim, S.W.; Kim, J.K. Anti-inflammatory effects of BT-201, an n-butanol extract of Panax notoginseng, observed in vitro and in a collagen-induced arthritis model. Clin. Nutr. 2007, 26, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Sun, X.; Xie, Y.; Du, A.; Chen, M.; Lai, S.; Wei, X.; Ji, L.; Wang, C. Panax notoginseng saponins alleviate diabetic retinopathy by inhibiting retinal inflammation: Association with the NF-κB signaling pathway. J. Ethnopharmacol. 2024, 319, 117135. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Lu, P.; Liu, J.; Yang, L.; Li, Y.; Chen, Y.; Wang, Y.; Wan, J.; Zhao, Y. 20(S)- Protopanaxadiol saponins isolated from Panax notoginseng target the binding of HMGB1 to TLR4 against inflammation in experimental ulcerative colitis. Phytother. Res. 2023, 37, 4690–4705. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, Y.; Gao, M.; Cui, X.; Yang, Y.; van Duijn, B.; Wang, M.; Hu, Y.; Wang, C.; Xiong, Y. Steamed Panax notoginseng attenuates anemia in mice with blood deficiency syndrome via regulating hematopoietic factors and JAK-STAT pathway. Front. Pharmacol. 2020, 10, 1578. [Google Scholar] [CrossRef]
- Lau, A.J.; Toh, D.F.; Chua, T.K.; Pang, Y.K.; Woo, S.O.; Koh, H.L. Antiplatelet and anticoagulant effects of Panax notoginseng: Comparison of raw and steamed Panax notoginseng with Panax ginseng and Panax quinquefolium. J. Ethnopharmacol. 2009, 125, 380–386. [Google Scholar] [CrossRef]
- Kwon, H.W.; Shin, J.H.; Rhee, M.H.; Park, C.E.; Lee, D.H. Anti-thrombotic effects of ginsenoside Rk3 by regulating cAMP and PI3K/MAPK pathway on human platelets. J. Ginseng Res. 2023, 47, 706–713. [Google Scholar] [CrossRef]
- Kwon, H.W. Inhibitory effect of 20(S)-Ginsenoside Rg3 on human platelet aggregation and intracellular Ca2+ levels via cyclic adenosine monophosphate dependent manner. Prev. Nutr. Food. Sci. 2018, 23, 317–325. [Google Scholar] [CrossRef]
- Xiong, L.; Qi, Z.; Zheng, B.; Li, Z.; Wang, F.; Liu, J.; Li, P. Inhibitory effect of triterpenoids from Panax ginseng on coagulation factor X. Molecules 2017, 22, 649. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Jiang, L.; Xu, C.; Luo, D.; Zeng, C.; Liu, P.; Yue, M.; Liu, Y.; Hu, X.; Hu, H. Ginsenoside Rg1 inhibits platelet activation and arterial thrombosis. Thromb. Res. 2014, 133, 57–65. [Google Scholar] [CrossRef]
- Long, L.; Yu, Z.; Qu, H.; Wang, N.; Guo, M.; Zhou, X.; Fu, C.; Gao, Z. Prediction of the network pharmacology-based mechanism for attenuation of atherosclerosis in apolipoprotein E knockout mice by Panax notoginseng saponins. Evid. Based Complement. Alternat. Med. 2020, 2020, 8574702. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Hao, F.; Zhang, H.; Cao, D.; Lu, X.; Li, X. Panax notoginseng saponins promote endothelial progenitor cell mobilization and attenuate atherosclerotic lesions in apolipoprotein E knockout mice. Cell. Physiol. Biochem. 2013, 32, 814–826. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Liu, Z.; Hu, X.; Liu, X.; Gui, L.; Cai, Z.; Dai, C. Protective effect of Panax Notoginseng saponins on apolipoprotein-E-deficient atherosclerosis-prone mice. Curr. Pharm. Des. 2022, 28, 671–677. [Google Scholar] [CrossRef]
- Wang, D.; Lv, L.; Xu, Y.; Jiang, K.; Chen, F.; Qian, J.; Chen, M.; Liu, G.; Xiang, Y. Cardioprotection of Panax Notoginseng saponins against acute myocardial infarction and heart failure through inducing autophagy. Biomed. Pharmacother. 2021, 136, 111287. [Google Scholar] [CrossRef]
- Wang, C.; Chen, H.; Ma, S.T.; Mao, B.B.; Chen, Y.; Xu, H.N.; Yu, H. A network pharmacology approach for exploring the mechanisms of Panax notoginseng saponins in ischaemic stroke. Evid. Based Complement. Alternat. Med. 2021, 2021, 5582782. [Google Scholar] [CrossRef] [PubMed]
- Son, H.Y.; Han, H.S.; Jung, H.W.; Park, Y.K. Panax notoginseng attenuates the infarct volume in rat ischemic brain and the inflammatory response of microglia. J. Pharmacol. Sci. 2009, 109, 368–379. [Google Scholar] [CrossRef]
- Shi, Y.; Zhou, X.; Yang, R.; Ying, S.; Wang, L. Panax notoginseng protects the rat brain function from traumatic brain injury by inhibiting autophagy via mammalian targeting of rapamycin. Aging 2021, 13, 11207–11217. [Google Scholar] [CrossRef]
- Jiang, T.; Zhou, X.; Jiang, H.; Ying, R.; Zhang, Z.; Cai, D.; Wu, Y.; Fang, H.; Wang, L. Efficacy of Sanqi (Radix Notoginseng) in treating cerebral hemorrhage in rats with traumatic brain injury. J. Tradit. Chin. Med. 2021, 41, 262–269. [Google Scholar]
- Zhou, N.; Tang, Y.; Keep, R.F.; Ma, X.; Xiang, J. Antioxidative effects of Panax notoginseng saponins in brain cells. Phytomedicine 2014, 21, 1189–1195. [Google Scholar] [CrossRef] [PubMed]
- Catino, S.; Paciello, F.; Miceli, F.; Rolesi, R.; Troiani, D.; Calabrese, V.; Santangelo, R.; Mancuso, C. Ferulic Acid Regulates the Nrf2/Heme Oxygenase-1 System and Counteracts Trimethyltin-Induced Neuronal Damage in the Human Neuroblastoma Cell Line SH-SY5Y. Front. Pharmacol. 2016, 6, 305. [Google Scholar] [CrossRef] [PubMed]
- Fetoni, A.R.; Paciello, F.; Rolesi, R.; Eramo, S.L.; Mancuso, C.; Troiani, D.; Paludetti, G. Rosmarinic acid up-regulates the noise-activated Nrf2/HO-1 pathway and protects against noise-induced injury in rat cochlea. Free Radic. Biol. Med. 2015, 85, 269–281. [Google Scholar] [CrossRef]
- Calabrese, V.; Mancuso, C.; Ravagna, A.; Perluigi, M.; Cini, C.; De Marco, C.; Butterfield, D.A.; Stella, A.M. In vivo induction of heat shock proteins in the substantia nigra following L-DOPA administration is associated with increased activity of mitochondrial complex I and nitrosative stress in rats: Regulation by glutathione redox state. J. Neurochem. 2007, 101, 709–717. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, C. The brain heme oxygenase/biliverdin reductase system as a target in drug research and development. Expert. Opin. Ther. Targets. 2022, 26, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.J.; Nie, B.M.; Chen, H.Z.; Lu, Y. Panaxynol induces neurite outgrowth in PC12D cells via cAMP- and MAP kinase-dependent mechanisms. Chem. Biol. Interact. 2006, 159, 58–64. [Google Scholar] [CrossRef]
- Jiang, Y.; Li, S.; Xie, X.; Li, H.; Huang, P.; Li, B.; Huo, L.; Zhong, J.; Li, Y.; Xia, X. Exploring the mechanism of Panax notoginseng saponins against Alzheimer’s disease by network pharmacology and experimental validation. Evid. Based Complement. Alternat. Med. 2021, 2021, 5730812. [Google Scholar] [CrossRef]
- Li, Z.; Li, H.; Zhao, C.; Lv, C.; Zhong, C.; Xin, W.; Zhang, W. Protective effect of notoginsenoside R1 on an APP/PS1 mouse model of Alzheimer’s disease by up-regulating insulin degrading enzyme and inhibiting Aβ accumulation. CNS. Neurol. Disord. Drug. Targets. 2015, 14, 360–369. [Google Scholar] [CrossRef]
- Fang, F.; Chen, X.; Huang, T.; Lue, L.F.; Luddy, J.S.; Yan, S.S. Multi-faced neuroprotective effects of Ginsenoside Rg1 in an Alzheimer mouse model. Biochim. Biophys. Acta 2012, 1822, 286–292. [Google Scholar] [CrossRef]
- Luo, F.C.; Wang, S.D.; Qi, L.; Song, J.Y.; Lv, T.; Bai, J. Protective effect of panaxatriol saponins extracted from Panax notoginseng against MPTP-induced neurotoxicity in vivo. J. Ethnopharmacol. 2011, 133, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, V.; Cornelius, C.; Mancuso, C.; Pennisi, G.; Calafato, S.; Bellia, F.; Bates, T.E.; Giuffrida Stella, A.M.; Schapira, T.; Dinkova Kostova, A.T.; et al. Cellular stress response: A novel target for chemoprevention and nutritional neuroprotection in aging, neurodegenerative disorders and longevity. Neurochem. Res. 2008, 33, 2444–2471. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, R.; Yu, J.; Koizumi, H.; Ouchi, Y.; Okabe, T. Ginsenoside Rb1 prevents MPP(+)-induced apoptosis in PC12 cells by stimulating estrogen receptors with consequent activation of ERK1/2, Akt and inhibition of SAPK/JNK, p38 MAPK. Evid. Based Complement. Alternat. Med. 2012, 2012, 693717. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhou, C.; Miao, L.; Tan, Y.; Zhou, Y.; Cheong, M.S.; Huang, Y.; Wang, Y.; Yu, H.; Cheang, W.S. Panax notoginseng protects against diabetes-associated endothelial dysfunction: Comparison between ethanolic extract and total saponin. Oxid. Med. Cell. Longev. 2021, 2021, 4722797. [Google Scholar] [CrossRef]
- Du, Y.G.; Wang, L.P.; Qian, J.W.; Zhang, K.N.; Chai, K.F. Panax notoginseng saponins protect kidney from diabetes by up-regulating silent information regulator 1 and activating antioxidant proteins in rats. Chin. J. Integr. Med. 2016, 22, 910–917. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Wang, N.; Tan, H.Y.; Li, S.; Zhang, C.; Zhang, Z.; Feng, Y. Panax notoginseng saponins modulate the gut microbiota to promote thermogenesis and beige adipocyte reconstruction via leptin-mediated AMPKα/STAT3 signaling in diet-induced obesity. Theranostics 2020, 10, 11302–11323. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Wang, P.; Cui, J.; Wang, W.; Chen, Y.; Zhang, T. Panax notoginseng saponins attenuate lung cancer growth in part through modulating the level of Met/miR-222 axis. J. Ethnopharmacol. 2016, 193, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Hawthorne, B.; Lund, K.; Freggiaro, S.; Kaga, R.; Meng, J. The mechanism of the cytotoxic effect of Panax notoginseng extracts on prostate cancer cells. Biomed. Pharmacother. 2022, 149, 112887. [Google Scholar] [CrossRef] [PubMed]
- Toh, D.F.; Patel, D.N.; Chan, E.C.; Teo, A.; Neo, S.Y.; Koh, H.L. Anti-proliferative effects of raw and steamed extracts of Panax notoginseng and its ginsenoside constituents on human liver cancer cells. Chin. Med. 2011, 6, 4. [Google Scholar] [CrossRef]
- Yan, Z.; Yang, R.; Jiang, Y.; Yang, Z.; Yang, J.; Zhao, Q.; Lu, Y. Induction of apoptosis in human promyelocytic leukemia HL60 cells by panaxynol and panaxydol. Molecules 2011, 16, 5561–5573. [Google Scholar] [CrossRef]
- Lee, C.Y.; Hsieh, S.L.; Hsieh, S.; Tsai, C.C.; Hsieh, L.C.; Kuo, Y.H.; Wu, C.C. Inhibition of human colorectal cancer metastasis by notoginsenoside R1, an important compound from Panax notoginseng. Oncol. Rep. 2017, 37, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, S.L.; Hsieh, S.; Kuo, Y.H.; Wang, J.J.; Wang, J.C.; Wu, C.C. Effects of Panax notoginseng on the metastasis of human colorectal cancer cells. Am. J. Chin. Med. 2016, 44, 851–870. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.Z.; Luo, X.; Zhang, B.; Song, W.X.; Ni, M.; Mehendale, S.; Xie, J.T.; Aung, H.H.; He, T.C.; Yuan, C.S. Notoginseng enhances anti-cancer effect of 5-fluorouracil on human colorectal cancer cells. Cancer Chemother. Pharmacol. 2007, 60, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Cui, J.; Du, X.; Yang, Q.; Jia, C.; Xiong, M.; Yu, X.; Li, L.; Wang, W.; Chen, Y.; et al. Panax notoginseng saponins (PNS) inhibits breast cancer metastasis. J. Ethnopharmacol. 2014, 154, 663–671. [Google Scholar] [CrossRef]
- He, L.; Chen, X.; Zhou, M.; Zhang, D.; Yang, J.; Yang, M.; Zhou, D. Radix/rhizoma notoginseng extract (sanchitongtshu) for ischemic stroke: A randomized controlled study. Phytomedicine 2011, 18, 437–442. [Google Scholar] [CrossRef] [PubMed]
- Geng, H.; Zhang, L.; Xin, C.; Zhang, C.; Xie, Y. Xuesaitong oral preparation as adjuvant therapy for treating acute cerebral infarction: A systematic review and meta-analysis of randomized controlled trials. J. Ethnopharmacol. 2022, 285, 114849. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.; Cen, K.; Liu, W.; Liu, F.; Liu, R.; Sun, Y.; Zhao, Y.; Chang, J.; Zhu, L. Xuesaitong exerts long-term neuroprotection for stroke recovery by inhibiting the ROCKII pathway, in vitro and in vivo. J. Ethnopharmacol. 2021, 272, 113943. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Song, H.; Zhang, C.; Wang, A.; Zhang, B.; Xiong, C.; Zhuang, X.; Zang, Y.; Li, C.; Fang, Q.; et al. Efficacy and safety of Panax notoginseng saponins in the treatment of adults with ischemic stroke in China: A randomized clinical trial. JAMA Netw. Open 2023, 6, e2317574. [Google Scholar] [CrossRef]
- Duan, L.; Xiong, X.; Hu, J.; Liu, Y.; Wang, J. Efficacy and safety of oral Panax notoginseng saponins for unstable angina patients: A meta-analysis and systematic review. Phytomedicine 2018, 47, 23–33. [Google Scholar] [CrossRef]
- Wang, W.; Yang, L.; Song, L.; Guo, M.; Li, C.; Yang, B.; Wang, M.; Kou, N.; Gao, J.; Qu, H.; et al. Combination of Panax notoginseng saponins and aspirin potentiates platelet inhibition with alleviated gastric injury via modulating arachidonic acid metabolism. Biomed. Pharmacother. 2021, 134, 111165. [Google Scholar] [CrossRef]
- Xie, Y.; Wang, C. Herb-drug interactions between Panax notoginseng or its biologically active compounds and therapeutic drugs: A comprehensive pharmacodynamic and pharmacokinetic review. J. Ethnopharmacol. 2023, 307, 116156. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lu, Y.Y.; Jia, J.; Fang, M.; Zhao, L.; Jiang, Y.; Shi, Y.; Tu, P.F.; Guo, X.Y. A novel system for evaluating the inhibition effect of drugs on cytochrome P450 enzymes in vitro based on human-induced hepatocytes (hiHeps). Front. Pharmacol. 2021, 12, 748658. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Chen, D.; Lin, X.X.; Peng, S.F.; Xiao, M.F.; Huang, W.H.; Wang, Y.C.; Peng, J.B.; Zhang, W.; Ouyang, D.S.; et al. Screening of drug metabolizing enzymes for the ginsenoside compound K in vitro: An efficient anti-cancer substance originating from Panax Ginseng. PLoS ONE 2016, 11, e0147183. [Google Scholar] [CrossRef]
- Fang, Z.Z.; Cao, Y.F.; Hu, C.M.; Hong, M.; Sun, X.Y.; Ge, G.B.; Liu, Y.; Zhang, Y.Y.; Yang, L.; Sun, H.Z. Structure-inhibition relationship of ginsenosides towards UDP-glucuronosyltransferases (UGTs). Toxicol. Appl. Pharmacol. 2013, 267, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhou, F.; Niu, F.; Lu, M.; Wu, X.; Sun, J.; Wang, G. Stereoselective regulations of P-glycoprotein by ginsenoside Rh2 epimers and the potential mechanisms from the view of pharmacokinetics. PLoS ONE 2012, 7, e35768. [Google Scholar] [CrossRef]
- Chen, X.Y.; Qian, F.; Wang, Y.Y.; Liu, Y.; Sun, Y.; Zha, W.B.; Hao, K.; Zhou, F.; Wang, G.J.; Zhang, J.W. Ginsenoside 20(S)-Rh2 promotes cellular pharmacokinetics and intracellular antibacterial activity of levofloxacin against Staphylococcus aureus through drug efflux inhibition and subcellular stabilization. Acta Pharmacol. Sin. 2021, 42, 1930–1941. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Zhu, C.; Long, J.; Lu, C.; Pan, X.; Wu, C. PLGA microsphere-based composite hydrogel for dual delivery of ciprofloxacin and ginsenoside Rh2 to treat Staphylococcus aureus-induced skin infections. Drug Deliv. 2020, 27, 632–641. [Google Scholar] [CrossRef]
- Zhang, J.; Sun, Y.; Wang, Y.; Lu, M.; He, J.; Liu, J.; Chen, Q.; Zhang, X.; Zhou, F.; Wang, G.; et al. Non-antibiotic agent ginsenoside 20(S)-Rh2 enhanced the antibacterial effects of ciprofloxacin in vitro and in vivo as a potential NorA inhibitor. Eur. J. Pharmacol. 2014, 740, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Tian, Z.; Pang, H.; Du, S.; Lu, Y.; Zhang, L.; Wu, H.; Guo, S.; Wang, M.; Zhang, Q. Effect of Panax notoginseng saponins on the pharmacokinetics of aspirin in rats. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2017, 1040, 136–143. [Google Scholar] [CrossRef]
- Deng, S.; Wong, C.K.C.; Lai, H.C.; Wong, A.S.T. Ginsenoside-Rb1 targets chemotherapy-resistant ovarian cancer stem cells via simultaneous inhibition of Wnt/β-catenin signaling and epithelial-to-mesenchymal transition. Oncotarget 2017, 8, 25897–25914. [Google Scholar] [CrossRef]
- Chian, S.; Zhao, Y.; Xu, M.; Yu, X.; Ke, X.; Gao, R.; Yin, L. Ginsenoside Rd reverses cisplatin resistance in non-small-cell lung cancer A549 cells by downregulating the nuclear factor erythroid 2-related factor 2 pathway. Anticancer Drugs 2019, 30, 838–845. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Huang, J.; Gao, F.; Yin, Z.; Zhang, R. Ginsenoside RG1 augments doxorubicin-induced apoptotic cell death in MDA-MB-231 breast cancer cell lines. J. Biochem. Mol. Toxicol. 2022, 36, e22945. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Wang, Y.; Liu, H.; Mu, H.; Lu, Y.; Zhang, J.; Huang, J. Oral administration of Ginsenoside Rg1 prevents cardiac toxicity induced by doxorubicin in mice through anti-apoptosis. Oncotarget 2017, 8, 83792–83801. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.R.; Li, T.; Zhang, L.; Hu, Z.Y.; Zhou, L.; Shan, L.T.; Huang, J.W.; Li, L. Acute developmental toxicity of Panax notoginseng in zebrafish larvae. Chin. J. Integr. Med. 2023, 29, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Zhao, M.; Li, Z. Immunotoxicity of Panax notoginseng in Sprague-Dawley rats. Chin. J. Public Health 2020, 36, 82–85. [Google Scholar] [CrossRef]
- Zhang, K.; Sun, C.; Hu, Y.; Yang, J.; Wu, C. Network pharmacology reveals pharmacological effect and mechanism of Panax notoginseng (Burk.) F. H. Chen on reproductive and genetic toxicity in male mice. J. Ethnopharmacol. 2021, 270, 113792. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.K. Ginseng abuse syndrome. Problems with the panacea. JAMA 1979, 241, 1614–1615. [Google Scholar] [CrossRef]
- Turck, D.; Castenmiller, J.; De Henauw, S.; Hirsch-Ernst, K.I.; Kearney, J.; Maciuk, A.; Mangelsdorf, I.; McArdle, H.J.; Naska, A.; Pelaez, C.; et al. Safety of a botanical extract derived from Panax notoginseng and Astragalus membranaceus (AstraGin™) as a novel food pursuant to Regulation (EU) 2015/2283. EFSA J. 2020, 18, e06099. [Google Scholar] [CrossRef]
| Sources | Cmax (µM) | Tmax (h) | AUC0-t (µM∙h) | T1/2 (h) | Reference |
|---|---|---|---|---|---|
| Ginsenoside Rb1 | |||||
| Sanqui extract PO a | |||||
| Female | 0.021 ± 0.009 | 7.8 ± 3.7 | 0.67 ± 0.30 | 33–57 | [32] |
| Male | 0.035 ± 0.038 | 11.8 ± 2.9 | 0.83 ± 0.42 | ||
| Xueshuantong b | |||||
| Intramuscular | 6.06 ± 0.65 | 5.3 ± 2.4 | 254.42 ± 26.65 | 46.3 ± 9.6 | [34] |
| Intravenous c | 8.83 ± 1.38 | 1.5 | 227.25 ± 16.12 | 57.0 ± 14.5 | |
| Xueshuantong d | |||||
| Female 250 mg | 19.5 ± 2.2 | 2.5 | 492.4 ± 46.7 | 39.9 ± 4.7 | [35] |
| Male 250 mg | 16.3 ± 3.7 | 425.5 ± 68.0 | 43.5 ± 6.5 | ||
| Female 500 mg | 28.9 ± 3.2 | 887.4 ± 97.5 | 41.0 ± 7.6 | ||
| Male 500 mg | 26.3 ± 2.6 | 737.7 ± 99.3 | 42.9 ± 7.5 | ||
| Compound K | |||||
| Sanqui extract PO a | |||||
| Female | 0.324 ± 0.15 | 17.3 ± 6.4 | 5.71 ± 2.39 | NC | [32] |
| Male | 0.249 ± 0.18 | 10.9 ± 8.7 | 3.79 ± 2.91 | ||
| Ginsenoside | Mechanism(s) | Reference(s) |
|---|---|---|
| Rk3 |
Inactivation of the integrin αIIb/β3 and reduction of fibrinogen binding. Inhibition of MAPK and PI3K/Akt phosphorylation leads to reduced production of TXA2. | [46] |
| Rg3 |
Increased cAMP levels. Suppressed thrombin-induced elevation of intracellular calcium levels. Inhibition of factor Xa. | [47,48] |
| Rg1 |
Inhibition of thrombin-induced ERK phosphorylation. Decreased rate of clot retraction. | [49] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mancuso, C. Panax notoginseng: Pharmacological Aspects and Toxicological Issues. Nutrients 2024, 16, 2120. https://doi.org/10.3390/nu16132120
Mancuso C. Panax notoginseng: Pharmacological Aspects and Toxicological Issues. Nutrients. 2024; 16(13):2120. https://doi.org/10.3390/nu16132120
Chicago/Turabian StyleMancuso, Cesare. 2024. "Panax notoginseng: Pharmacological Aspects and Toxicological Issues" Nutrients 16, no. 13: 2120. https://doi.org/10.3390/nu16132120
APA StyleMancuso, C. (2024). Panax notoginseng: Pharmacological Aspects and Toxicological Issues. Nutrients, 16(13), 2120. https://doi.org/10.3390/nu16132120





