Citrulline, Intestinal Fatty Acid-Binding Protein and the Acute Gastrointestinal Injury Score as Predictors of Gastrointestinal Failure in Patients with Sepsis and Septic Shock
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Data Collection
- AGI score I: (the patient is at risk of developing GI dysfunction) the function of the digestive tract is partially impaired; GI symptoms are associated with a known cause and transient;
- AGI score II: (the patient developed GI dysfunction) the GI tract is unable to function properly to meet patient’s needs for nutrients and fluids;
- AGI score III: (the patient developed GI failure) severe GI damage which does not respond to normal treatment and the general condition of the patient is not improving;
- AGI score IV: (the patient developed GI failure with severe impact on distant organ function) persistent, long-term damage, resulting in worsening of multi-organ dysfunction syndrome or shock; life-threatening and requiring surgical intervention.
2.2. Control Group
2.3. Sample Collection and Measurement of the Biomarkers
2.4. Statistical Analysis
3. Results
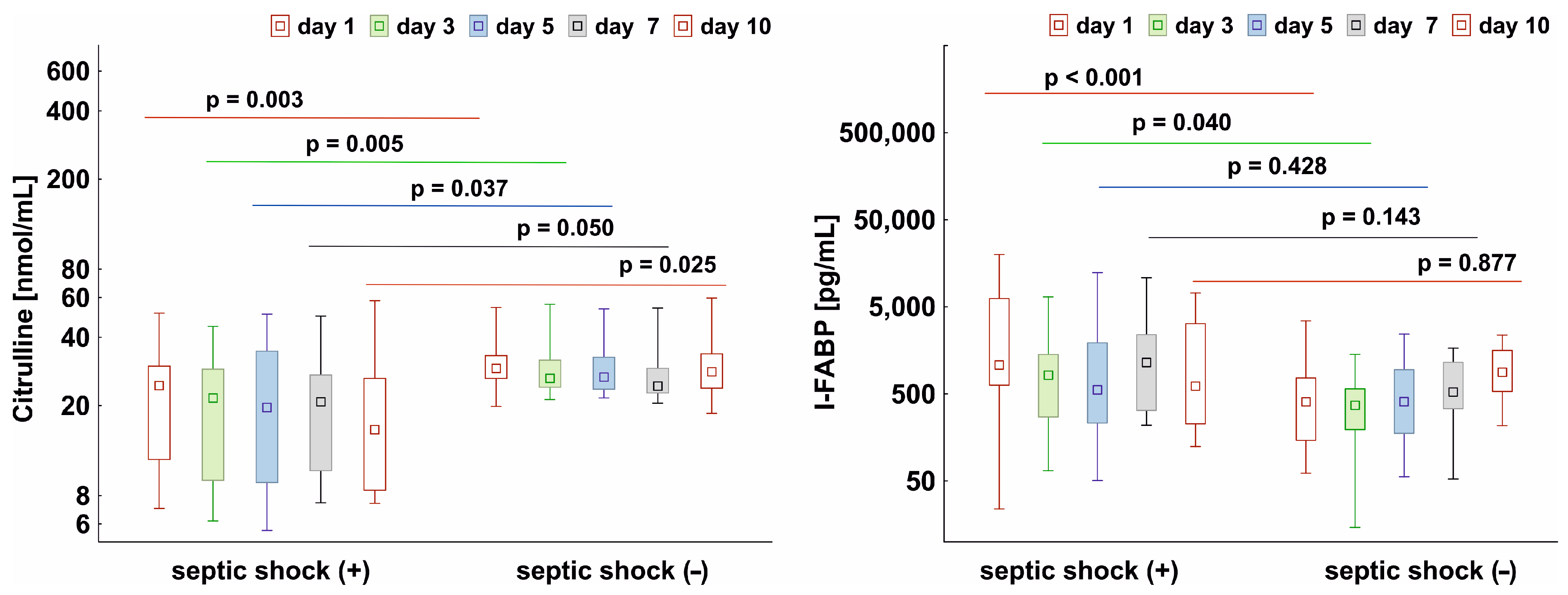
3.1. Levels of Citrulline and I-FABP in Septic Patients with and without Shock
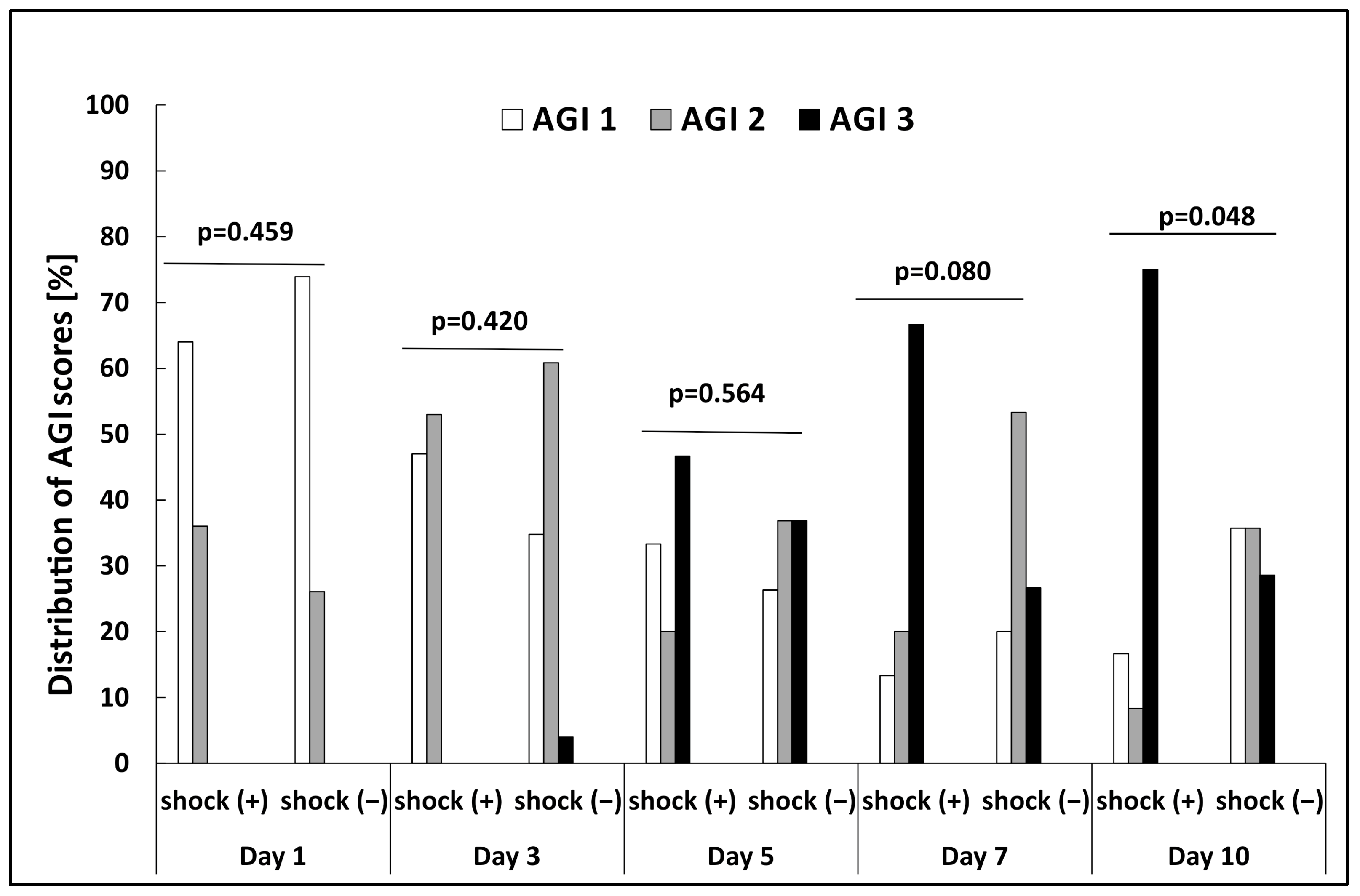
3.2. The Relationship between AGI Score and Biomarker Levels
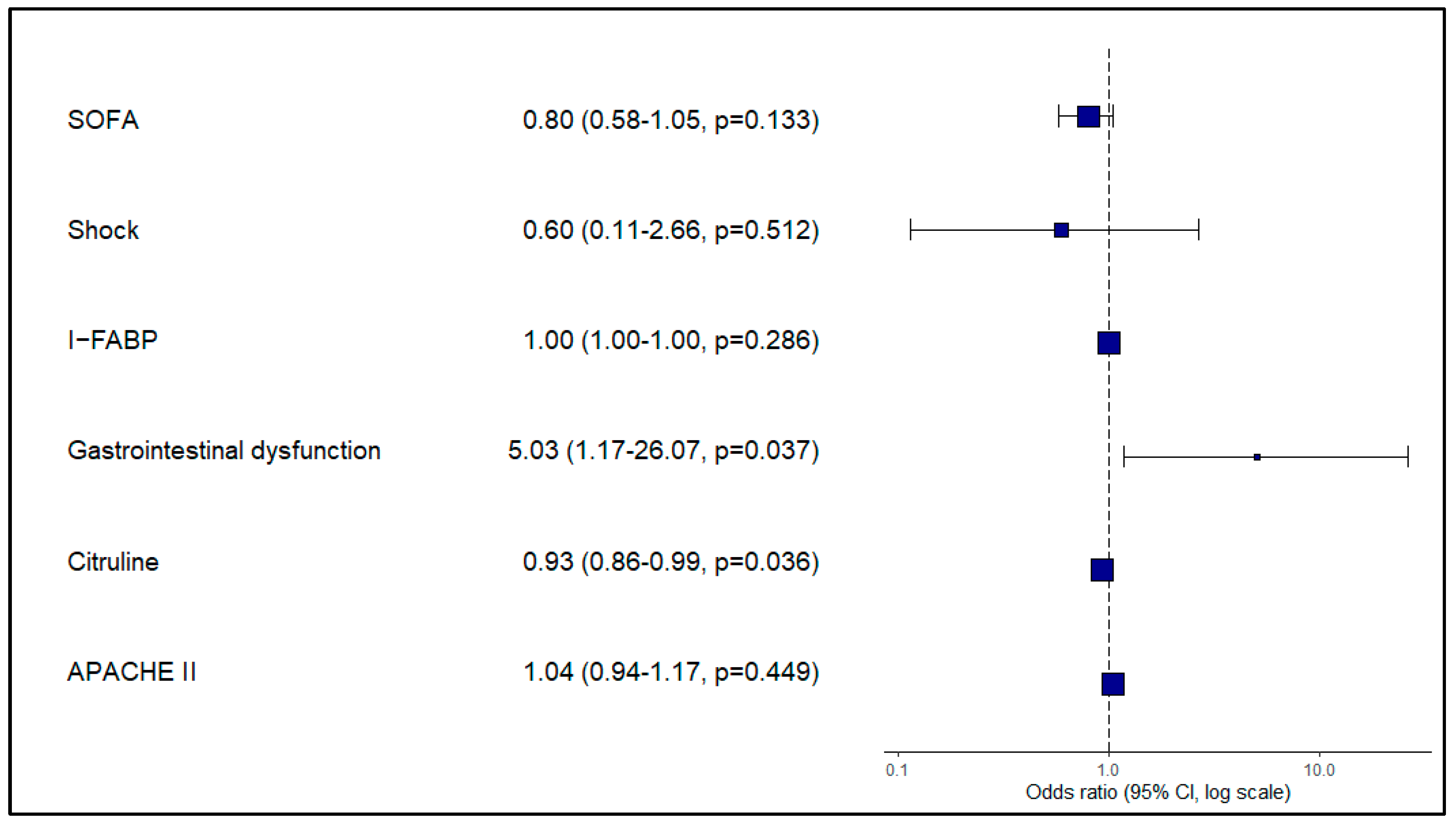
3.3. Biomarker Levels as a Tool for Predicting the Development of GI Failure
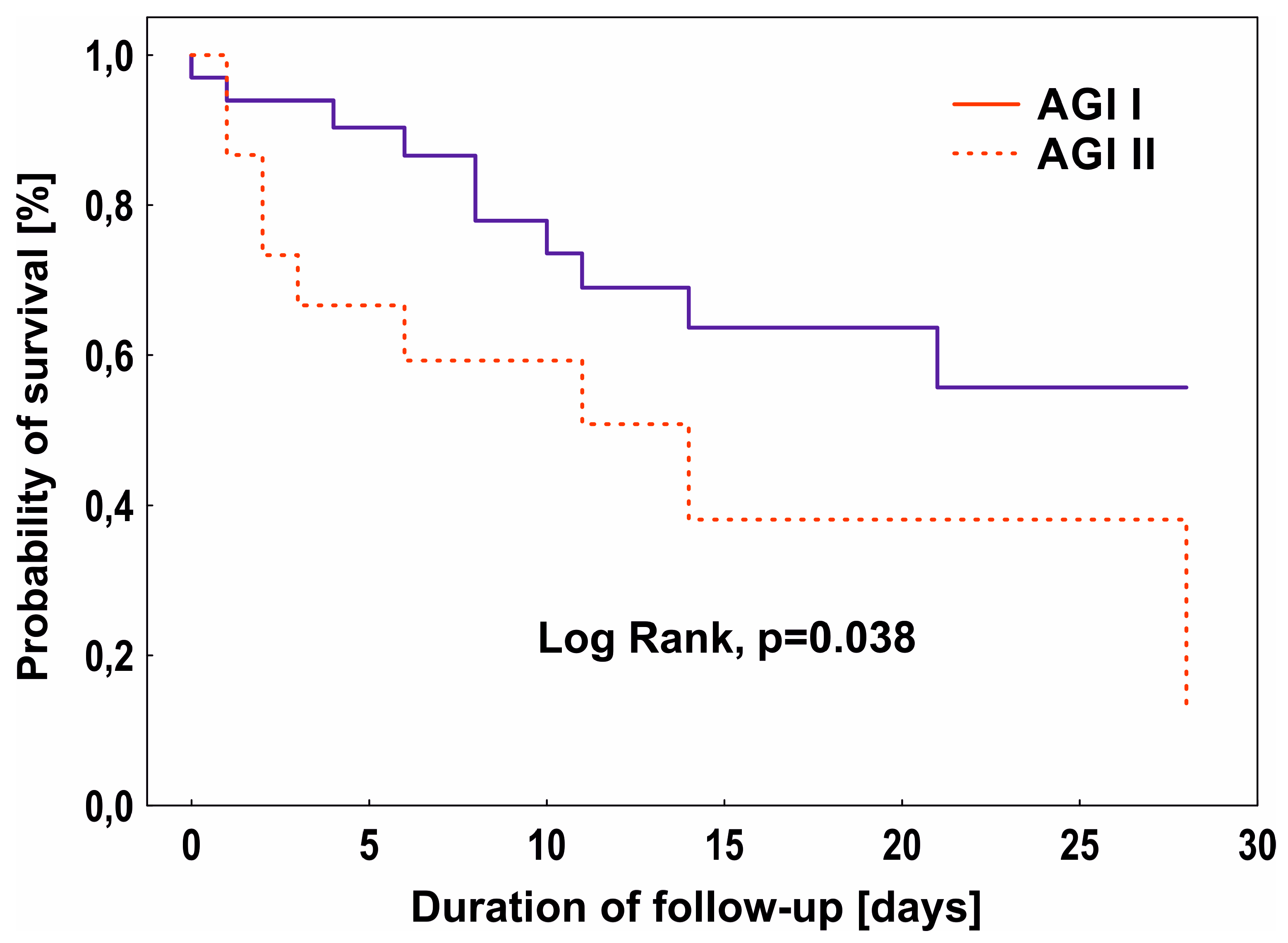
3.4. AGI Score, Biomarkers, and 28-Day Mortality
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Hu, B.; Sun, R.; Wu, A.; Ni, Y.; Liu, J.; Guo, F.; Ying, L.; Ge, G.; Ding, A.; Shi, Y.; et al. Severity of Acute Gastrointestinal Injury Grade Is a Predictor of All-Cause Mortality in Critically Ill Patients: A Multicenter, Prospective, Observational Study. Crit. Care 2017, 21, 188. [Google Scholar] [CrossRef] [PubMed]
- Adelman, M.W.; Woodworth, M.H.; Langelier, C.; Busch, L.M.; Kempker, J.A.; Kraft, C.S.; Kraft, C.S.; Martin, G.S.; Martin, G.S. The Gut Microbiome’s Role in the Development, Maintenance, and Outcomes of Sepsis. Crit. Care 2020, 24, 278. [Google Scholar] [CrossRef] [PubMed]
- Fay, K.T.; Klingensmith, N.J.; Chen, C.W.; Zhang, W.; Sun, Y.; Morrow, K.N.; Liang, Z.; Burd, E.M.; Ford, M.L.; Coopersmith, C.M. The Gut Microbiome Alters Immunophenotype and Survival from Sepsis. FASEB J. 2019, 33, 11258–11269. [Google Scholar] [CrossRef] [PubMed]
- Adamik, B.; Gozdzik, W.; Jakubczyk, D.; Welna, M.; Kübler, A. Coagulation Abnormalities Identified by Thromboelastometry in Patients with Severe Sepsis: The Relationship to Endotoxemia and Mortality. Blood Coagul. Fibrinolysis 2017, 28, 163–170. [Google Scholar] [CrossRef]
- Bray, M.A.; Sartain, S.E.; Gollamudi, J.; Rumbaut, R.E. Microvascular Thrombosis: Experimental and Clinical Implications. Transl. Res. 2020, 225, 105–130. [Google Scholar] [CrossRef]
- Dempfle, C.E. Coagulopathy of Sepsis. Thromb. Haemost. 2004, 91, 213–224. [Google Scholar] [CrossRef]
- de Backer, D.; Creteur, J.; Preiser, J.C.; Dubois, M.J.; Vincent, J.L. Microvascular Blood Flow Is Altered in Patients with Sepsis. Am. J. Respir. Crit. Care Med. 2002, 166, 98–104. [Google Scholar] [CrossRef]
- Ellis, C.G.; Jagger, J.; Sharpe, M. The Microcirculation as a Functional System. Crit. Care 2005, 9, S3–S8. [Google Scholar] [CrossRef]
- Altshuler, A.E.; Lamadrid, I.; Li, D.; Ma, S.R.; Kurre, L.; Schmid-Schönbein, G.W.; Penn, A.H. Transmural Intestinal Wall Permeability in Severe Ischemia after Enteral Protease Inhibition. PLoS ONE 2014, 9, e96655. [Google Scholar] [CrossRef]
- Jiang, L.-Y.; Zhang, M.; Zhou, T.-E.; Yang, Z.-F.; Wen, L.-Q.; Chang, J.-X. Changes of the Immunological Barrier of Intestinal Mucosa in Rats with Sepsis. World J. Emerg. Med. 2010, 1, 138–143. [Google Scholar] [PubMed]
- Reintam Blaser, A.; Preiser, J.C.; Fruhwald, S.; Wilmer, A.; Wernerman, J.; Benstoem, C.; Casaer, M.P.; Starkopf, J.; van Zanten, A.; Rooyackers, O.; et al. Gastrointestinal Dysfunction in the Critically Ill: A Systematic Scoping Review and Research Agenda Proposed by the Section of Metabolism, Endocrinology and Nutrition of the European Society of Intensive Care Medicine. Crit. Care 2020, 24, 224. [Google Scholar] [CrossRef]
- Doudakmanis, C.; Bouliaris, K.; Kolla, C.; Efthimiou, M.; Koukoulis, G.D. Bacterial Translocation in Patients Undergoing Major Gastrointestinal Surgery and Its Role in Postoperative Sepsis. World J. Gastrointest. Pathophysiol. 2021, 12, 106–114. [Google Scholar] [CrossRef]
- Crapser, J.; Ritzel, R.; Verma, R.; Venna, V.R.; Liu, F.; Chauhan, A.; Koellhoffer, E.; Patel, A.; Ricker, A.; Maas, K.; et al. Ischemic Stroke Induces Gut Permeability and Enhances Bacterial Translocation Leading to Sepsis in Aged Mice. Aging 2016, 8, 1049–1063. [Google Scholar] [CrossRef]
- Blaser, A.R.; Malbrain, M.L.N.G.; Starkopf, J.; Fruhwald, S.; Jakob, S.M.; de Waele, J.; Braun, J.P.; Poeze, M.; Spies, C. Gastrointestinal Function in Intensive Care Patients: Terminology, Definitions and Management. Recommendations of the ESICM Working Group on Abdominal Problems. Intensive Care Med. 2012, 38, 384–394. [Google Scholar] [CrossRef]
- Reintam Blaser, A.; Padar, M.; Mändul, M.; Elke, G.; Engel, C.; Fischer, K.; Giabicani, M.; Gold, T.; Hess, B.; Hiesmayr, M.; et al. Development of the Gastrointestinal Dysfunction Score (GIDS) for Critically Ill Patients—A Prospective Multicenter Observational Study (ISOFA Study). Clin. Nutr. 2021, 40, 4932–4940. [Google Scholar] [CrossRef]
- Curis, E.; Nicolis, I.; Moinard, C.; Osowska, S.; Zerrouk, N.; Bénazeth, S.; Cynober, L. Almost All about Citrulline in Mammals. Amino Acids 2005, 29, 177–205. [Google Scholar] [CrossRef]
- Noordally, S.O.; Sohawon, S.; Semlali, H.; Michely, D.; Devriendt, J.; Gottignies, P. Is There a Correlation between Circulating Levels of Citrulline and Intestinal Dysfunction in the Critically Ill? Nutr. Clin. Pract. 2012, 27, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Fagoni, N.; Piva, S.; Marino, R.; Chiarini, G.; Ferrari, D.; Grespi, E.; Bertuetti, R.; Barbieri, S.; Latronico, N.; Rasulo, F. The IN-PANCIA Study: Clinical Evaluation of Gastrointestinal Dysfunction and Failure, Multiple Organ Failure, and Levels of Citrulline in Critically Ill Patients. J. Intensive Care Med. 2020, 35, 279–283. [Google Scholar] [CrossRef]
- Crenn, P.; Neveux, N.; Chevret, S.; Jaffray, P.; Cynober, L.; Melchior, J.C.; Annane, D. Plasma L-Citrulline Concentrations and Its Relationship with Inflammation at the Onset of Septic Shock: A Pilot Study. J. Crit. Care 2014, 29, 315.e1–315.e6. [Google Scholar] [CrossRef] [PubMed]
- Piton, G.; Manzon, C.; Monnet, E.; Cypriani, B.; Barbot, O.; Navellou, J.C.; Carbonnel, F.; Capellier, G. Plasma Citrulline Kinetics and Prognostic Value in Critically Ill Patients. Intensive Care Med. 2010, 36, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Luiking, Y.C.; Poeze, M.; Ramsay, G.; Deutz, N.E.P. Reduced Citrulline Production in Sepsis Is Related to Diminished de Novo Arginine and Nitric Oxide Production. Am. J. Clin. Nutr. 2009, 89, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Kanda, T.; Fujii, H.; Tani, T.; Murakami, H.; Suda, T.; Sakai, Y.; Ono, T.; Hatakeyama, K. Intestinal Fatty Acid-Binding Protein Is a Useful Diagnostic Marker for Mesenteric Infarction in Humans. Gastroenterology 1996, 110, 339–343. [Google Scholar] [CrossRef]
- Derikx, J.P.M.; Poeze, M.; van Bijnen, A.A.; Buurman, W.A.; Heineman, E. Evidence for Intestinal and Liver Epithelial Cell Injury in the Early Phase of Sepsis. Shock 2007, 28, 544–548. [Google Scholar] [CrossRef] [PubMed]
- Padar, M.; Starkopf, J.; Starkopf, L.; Forbes, A.; Hiesmayr, M.; Jakob, S.M.; Rooijackers, O.; Wernerman, J.; Ojavee, S.E.; Reintam Blaser, A. Enteral Nutrition and Dynamics of Citrulline and Intestinal Fatty Acid-Binding Protein in Adult ICU Patients. Clin. Nutr. ESPEN 2021, 45, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Sekino, M.; Funaoka, H.; Sato, S.; Okada, K.; Inoue, H.; Yano, R.; Matsumoto, S.; Ichinomiya, T.; Higashijima, U.; Matsumoto, S.; et al. Intestinal Fatty Acid-Binding Protein Level as a Predictor of 28-Day Mortality and Bowel Ischemia in Patients with Septic Shock: A Preliminary Study. J. Crit. Care 2017, 42, 92–100. [Google Scholar] [CrossRef]
- Tyszko, M.; Lipińska-Gediga, M.; Lemańska-Perek, A.; Kobylińska, K.; Gozdzik, W.; Adamik, B. Intestinal Fatty Acid Binding Protein (I-FABP) as a Prognostic Marker in Critically Ill COVID-19 Patients. Pathogens 2022, 11, 1526. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef]
- Piton, G.; Capellier, G. Biomarkers of Gut Barrier Failure in the ICU. Curr. Opin. Crit. Care 2016, 22, 152–160. [Google Scholar] [CrossRef]
- Jenkins, B.; Calder, P.C.; Marino, L.V. A Scoping Review Considering Potential Biomarkers or Functional Measures of Gastrointestinal Dysfunction and Enteral Feeding Intolerance in Critically Ill Adults. Clin. Nutr. ESPEN 2022, 52, 331–339. [Google Scholar] [CrossRef]
- Li, H.; Chen, Y.; Huo, F.; Wang, Y.; Zhang, D. Association between Acute Gastrointestinal Injury and Biomarkers of Intestinal Barrier Function in Critically Ill Patients. BMC Gastroenterol. 2017, 17, 45. [Google Scholar] [CrossRef] [PubMed]
- Pelsers, M.M.A.L.; Namiot, Z.; Kisielewski, W.; Namiot, A.; Januszkiewicz, M.; Hermens, W.T.; Glatz, J.F.C. Intestinal-Type and Liver-Type Fatty Acid-Binding Protein in the Intestine. Tissue Distribution and Clinical Utility. Clin. Biochem. 2003, 36, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J.M.; Sacchettini, J.; Marks, C.; Marks, W.H. Human Intestinal Fatty Acid Binding Protein: Report of an Assay with Studies in Normal Volunteers and Intestinal Ischemia. Surgery 1997, 121, 335–342. [Google Scholar] [CrossRef]
- Heida, F.H.; Hulscher, J.B.F.; Schurink, M.; Timmer, A.; Kooi, E.M.W.; Bos, A.F.; Bruggink, J.L.M.; Kasper, D.C.; Pones, M.; Benkoe, T. Intestinal Fatty Acid-Binding Protein Levels in Necrotizing Enterocolitis Correlate with Extent of Necrotic Bowel: Results from a Multicenter Study. J. Pediatr. Surg. 2015, 50, 1115–1118. [Google Scholar] [CrossRef] [PubMed]
- Kanda, T.; Tsukahara, A.; Ueki, K.; Sakai, Y.; Tani, T.; Nishimura, A.; Yamazaki, T.; Tamiya, Y.; Tada, T.; Hirota, M.; et al. Diagnosis of Ischemic Small Bowel Disease by Measurement of Serum Intestinal Fatty Acid-Binding Protein in Patients with Acute Abdomen: A Multicenter, Observer-Blinded Validation Study. J. Gastroenterol. 2011, 46, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Voth, M.; Duchene, M.; Auner, B.; Lustenberger, T.; Relja, B.; Marzi, I. I-FABP Is a Novel Marker for the Detection of Intestinal Injury in Severely Injured Trauma Patients. World J. Surg. 2017, 41, 3120–3127. [Google Scholar] [CrossRef]
- Crenn, P.; Coudray-Lucas, C.; Thuillier, F.; Cynober, L.; Messing, B. Postabsorptive Plasma Citrulline Concentration Is a Marker of Absorptive Enterocyte Mass and Intestinal Failure in Humans. Gastroenterology 2000, 119, 1496–1505. [Google Scholar] [CrossRef]
- Elkhatib, I.; Buchman, A.L. Plasma Citrulline Concentration as a Marker for Disease Activity in Patients With Crohn’s Disease. J. Clin. Gastroenterol. 2012, 46, 308–310. [Google Scholar] [CrossRef]
- Shen, L.J.; Guan, Y.Y.; Wu, X.P.; Wang, Q.; Wang, L.; Xiao, T.; Wu, H.R.; Wang, J.G. Serum Citrulline as a Diagnostic Marker of Sepsis-Induced Intestinal Dysfunction. Clin. Res. Hepatol. Gastroenterol. 2015, 39, 230–236. [Google Scholar] [CrossRef]
- Blasco-Alonso, J.; Sánchezyáñez, P.; Rosa Camacho, V.; Camacho Alonso, J.M.; Yahyaoui Macías, R.; Gil-Gómez, R.; Milano Manso, G. Citrulline and Arginine Kinetics and Its Value as a Prognostic Factor in Pediatric Critically Ill Patients. An. Pediatría 2015, 83, 257–263. [Google Scholar] [CrossRef]
- Sarikaya, M.; Ergül, B.; Doğan, Z.; Filik, L.; Can, M.; Arslan, L. Intestinal Fatty Acid Binding Protein (I-FABP) as a Promising Test for Crohn’s Disease: A Preliminary Study. Clin. Lab. 2015, 61, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Ockner, R.K.; Manning, J.A. Fatty Acid Binding Protein in Small Intestine. Identification, Isolation, and Evidence for Its Role in Cellular Fatty Acid Transport. J. Clin. Investig. 1974, 54, 326–338. [Google Scholar] [CrossRef]
- Pelsers, M.M.A.L.; Hermens, W.T.; Glatz, J.F.C. Fatty Acid-Binding Proteins as Plasma Markers of Tissue Injury. Clin. Chim. Acta 2005, 352, 15–35. [Google Scholar] [CrossRef]
- de Haan, J.J.; Lubbers, T.; Derikx, J.P.; Relja, B.; Henrich, D.; Greve, J.W.; Marzi, I.; Buurman, W.A. Rapid Development of Intestinal Cell Damage Following Severe Trauma: A Prospective Observational Cohort Study. Crit. Care 2009, 13, R86. [Google Scholar] [CrossRef] [PubMed]
- Piton, G.; Belon, F.; Cypriani, B.; Regnard, J.; Puyraveau, M.; Manzon, C.; Navellou, J.C.; Capellier, G. Enterocyte Damage in Critically Ill Patients Is Associated with Shock Condition and 28-Day Mortality. Crit. Care Med. 2013, 41, 2169–2176. [Google Scholar] [CrossRef]
- Zhang, D.; Li, H.; Li, Y.; Qu, L. Gut Rest Strategy and Trophic Feeding in the Acute Phase of Critical Illness with Acute Gastrointestinal Injury. Nutr. Res. Rev. 2019, 32, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.K.; Liu, Y.; Zou, L.; Zhang, W.H.; Wang, Y.; Kan, X.H.; Chen, J.D.; Li, J.J.; Shi, Q.K.; Yuan, S.T. Acute Gastrointestinal Injury in Critically Ill Patients with COVID-19 in Wuhan, China. World J. Gastroenterol. 2020, 26, 6087–6097. [Google Scholar] [CrossRef]
- Drakos, P.; Volteas, P.; Cleri, N.A.; Alkadaa, L.N.; Asencio, A.A.; Oganov, A.; Pryor, A.; Talamini, M.; Rubano, J.; Bannazadeh, M.; et al. Acute Gastrointestinal Injury and Feeding Intolerance as Prognostic Factors in Critically Ill COVID-19 Patients. J. Gastrointest. Surg. 2022, 26, 181–190. [Google Scholar] [CrossRef]
- Ahn, J.W.; Scallan Walter, E.; White, A.E.; McQueen, R.B.; Hoffmann, S. Identifying Sepsis From Foodborne Hospitalization: Incidence and Hospitalization Cost by Pathogen. Clin. Infect. Dis. 2022, 75, 857–866. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, Q.; Jiang, L.; Xie, B.; Ji, X.; Lu, J.; Jiang, R.; Lei, S.; Mao, S.; Ying, L.; et al. Effectiveness of Enteral Feeding Protocol on Clinical Outcomes in Critically Ill Patients: A Study Protocol for before-and-after Design. Ann. Transl. Med. 2016, 4, 308. [Google Scholar] [CrossRef]
- Teng, J.; Xiang, L.; Long, H.; Gao, C.; Lei, L.; Zhang, Y. The Serum Citrulline and D-Lactate Are Associated with Gastrointestinal Dysfunction and Failure in Critically Ill Patients. Int. J. Gen. Med. 2021, 14, 4125–4134. [Google Scholar] [CrossRef] [PubMed]
- Klanovicz, T.M.; Franzosi, O.S.; Nunes, D.S.L.; Loss, S.H.; Batassini, É.; Turra, E.E.; Teixeira, C.; Vieira, S.R.R. Acute Gastrointestinal Failure Is Associated with Worse Hemodynamic and Perfusion Parameters over 48 h after Admission in Patients with Septic Shock: Retrospective Cohort Study. Nutr. Clin. Pract. 2022. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Li, Y.; Ding, L.; Fu, Y.; Dong, X.; Li, H. Prevalence and Outcome of Acute Gastrointestinal Injury in Critically Ill Patients: A Systematic Review and Meta-Analysis. Medicine 2018, 97, e12970. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Control | Septic Patients | ||
|---|---|---|---|---|
| N = 10 | Shock (+), N = 30 | Shock (−), N = 28 | p * | |
| Age, years | 67.5 (61.0–70.0) | 66.0 (60.0–73.0) | 61.5 (55.5–72.5) | 0.198 |
| Male, n (%) | 7.0 (70.0) | 18.0 (60.0) | 16.0 (57.0) | 0.825 |
| BMI, kg/m2 | 27.0 (24.0– 29.1) | 27.8 (25.2–30.9) | 26.1 (24.3–29.7) | 0.171 |
| APACHE II score | 10.5 (10–11) | 28.0 (24.0–32.0) | 24 (18–28) | 0.046 |
| SOFA score | 2 (1–3) | 10 (8.0–13.0) | 9 (8–12) | 0.388 |
| ICU admission n (%): | 0.360 | |||
| Medical | 0.0 | 18.0 (60.0) | 20.0 (71.0) | |
| Surgical | 10.0 (100.0) | 12.0 (40.0) | 8.0 (29) | |
| Lactate [mmol/L] | 0.9 (0.7–1.1) | 4.6 (2.6–8.2) | 1.7 (1.2–1.8) | <0.001 |
| PLT [103/uL] | 159.0 (137.0–181.0) | 210.0 (124.0–309.0) | 174.5 (120.0–364.5) | 0.803 |
| Fibrinogen [g/L] | 2.9 (3.6–6.5) | 4.6 (3.6–6.0) | 5.6 (3.7–6.6) | 0.481 |
| D-dimer [mg/L] | 0.7 (0.4–2.1) | 6.2 (3.9–15.7) | 6.2 (2.7–10.1) | 0.395 |
| WBC [103/uL] | 12.6 (11.2–16.1) | 17.1 (11.3–27.6) | 13.3 (9.1–21.1) | 0.543 |
| CRP [mg/L] | 61.6 (35.5–106.7) | 194.6 (104.1–328.4) | 255.6 (164.5–344.5) | 0.358 |
| PCT [ng/mL] | 0.1 (0.0–0.1) | 10.6 (3.6–34.2) | 8.7 (3.5–23.4) | 0.528 |
| Treatment n (%): | ||||
| CRRT | 0.0 | 12.0 (40.0) | 6.0 (21.0) | 0.126 |
| Mechanical ventilation | 10.0 (100) | 19.0 (63.0) | 22.0 (79.0) | 0.202 |
| ICU LOS [day] | 2.0 (2.0–3.0) | 7.5 (2.0–17.5) | 11 (5.0–21.0) | 0.093 |
| Mortality, 28 days (%) | 0.0 | 50.0 | 25.0 | 0.049 |
| Day 1 | Day 3 | Day 5 | Day 7 | Day 10 | |
|---|---|---|---|---|---|
| Citrulline [nmol/mL] | |||||
| AGI I | 27.36 | 25.03 | 26.72 | 24.11 | 33.81 |
| (13.36–30.58) | (23.30–30.92) | (23.63–46.54) | (23.42–24.40) | (27.55–35.22) | |
| AGI II | 31.00 | 27.56 | 32.66 | 29.20 | 29.40 |
| (27.26–33.30) | (25.62–36.87) | (25.62–36.87) | (21.33–31.45) | (23.84–47.95) | |
| AGI III | 24.59 | 23.42 | 22.14 | 21.50 | 18.46 |
| (12.30–26.85) | (12.64–27.47) | (9.92–26.81) | (10.32–25.88) | (8.88–26.33) | |
| * p | 0.244 | 0.197 | 0.053 | 0.205 | 0.037 |
| # p | <0.001 | 0.018 | 0.005 | 0.027 | 0.022 |
| I-FABP [pg/mL] | |||||
| AGI I | 476.61 | 400.71 | 546.00 | 493.21 | 2125.36 |
| (146.33–1095.36) | (303.84–812.14) | (155.27–1633.57) | (484.00–610.67) | (694.00–3204.29) | |
| AGI II | 956.33 | 414.67 | 421.33 | 1146.33 | 937.87 |
| (429.67–2191.00) | (254.67–1002.54) | (286.33–2432.86) | (431.00–1443.00) | (373.00–1139.67) | |
| AGI III | 832.57 | 283.76 | 416.78 | 550.35 | 698.10 |
| (125.80–1148.27) | (198.17–831.07) | (173.33–690.00) | (322.33–1673.00) | (225.71–1479.29) | |
| * p | 0.693 | 0.424 | 0.793 | 0.753 | 0.231 |
| # p | 0.293 | 0.447 | 0.451 | 0.887 | 0.650 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tyszko, M.; Lemańska-Perek, A.; Śmiechowicz, J.; Tomaszewska, P.; Biecek, P.; Gozdzik, W.; Adamik, B. Citrulline, Intestinal Fatty Acid-Binding Protein and the Acute Gastrointestinal Injury Score as Predictors of Gastrointestinal Failure in Patients with Sepsis and Septic Shock. Nutrients 2023, 15, 2100. https://doi.org/10.3390/nu15092100
Tyszko M, Lemańska-Perek A, Śmiechowicz J, Tomaszewska P, Biecek P, Gozdzik W, Adamik B. Citrulline, Intestinal Fatty Acid-Binding Protein and the Acute Gastrointestinal Injury Score as Predictors of Gastrointestinal Failure in Patients with Sepsis and Septic Shock. Nutrients. 2023; 15(9):2100. https://doi.org/10.3390/nu15092100
Chicago/Turabian StyleTyszko, Maciej, Anna Lemańska-Perek, Jakub Śmiechowicz, Paulina Tomaszewska, Przemyslaw Biecek, Waldemar Gozdzik, and Barbara Adamik. 2023. "Citrulline, Intestinal Fatty Acid-Binding Protein and the Acute Gastrointestinal Injury Score as Predictors of Gastrointestinal Failure in Patients with Sepsis and Septic Shock" Nutrients 15, no. 9: 2100. https://doi.org/10.3390/nu15092100
APA StyleTyszko, M., Lemańska-Perek, A., Śmiechowicz, J., Tomaszewska, P., Biecek, P., Gozdzik, W., & Adamik, B. (2023). Citrulline, Intestinal Fatty Acid-Binding Protein and the Acute Gastrointestinal Injury Score as Predictors of Gastrointestinal Failure in Patients with Sepsis and Septic Shock. Nutrients, 15(9), 2100. https://doi.org/10.3390/nu15092100








