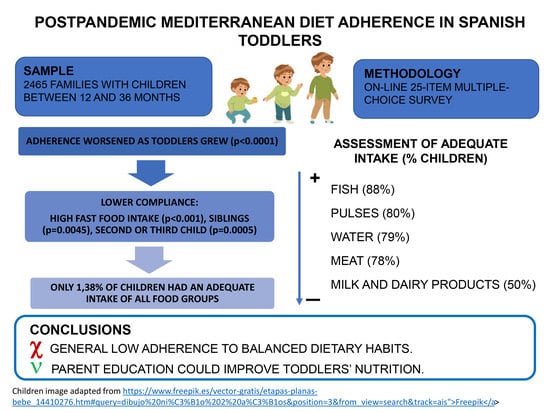
Post-Pandemic Feeding Patterns and Mediterranean Diet Adherence in Spanish Toddlers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Survey Questionnaire
2.3. Assessment of Adherence to Adequate Intake
2.4. Statistical Analysis
3. Results
3.1. Survey Results
3.1.1. Family Profile
3.1.2. History of Breastfeeding and Different Milk Intake
3.1.3. Feeding Patterns and Frequency of Different Food Groups Intakes
3.2. Adherence to Correct Dietary Habits and the Mediterranean Diet
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Item | N (%) |
|---|---|
| Family unit/caregivers | |
| Heteroparental | 2114 (88.05) |
| Single parent family (mother) | 145 (6.04) |
| Homoparental (Two mothers) | 129 (5.37) |
| Homoparental (Two fathers) | 7 (0.29) |
| Single parent family(father) | 6 (0.25) |
| Siblings | |
| None | 1490 (63.40) |
| 1 | 439 (18.68) |
| 2 | 316 (13.45) |
| ≥3 | 105 (4.67) |
| Birth order | |
| First | 1895 (79.26) |
| Second | 398 (16.64) |
| Third or higher | 98 (4.10) |
| Sex at birth | |
| Male | 1304 (52.90) |
| Female | 1161 (47.10) |
| Age | |
| 12–18 months | 1055 (42.80) |
| 19–24 months | 657 (26.55) |
| ≥25 months | 763 (30.55) |
References
- Dalmau Sierra, J.; Moráis López, A. Feeding of children 1–3 years old. In White Book of Nutrition of Children in Spain; Rivero Urgell, M., Moreno Aznar, L.A., Dalmau Serra, J., Moreno Villares, J.M., Aliaga Pérez, A., García Perea, A., Varela Moreiras, G., Ávila Torres, J.M., Eds.; Prensas de la Universidad de Zaragoza: Zaragoza, Spain, 2015; pp. 109–114. [Google Scholar]
- Kimura, N.; Keys, A. Coronary heart disease in seven countries. X. Rural southern Japan. Circulation 1970, 41 (Suppl. 4), I101–I112. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- García-Cabrera, S.; Herrera-Fernández, N.; Rodríguez-Hernández, C.; Nissensohn, M.; Román-Viña, B.; Serra-Majem, L. Kidmed test; prevalence of low adherence to the Mediterranean diet in children and young; a systematic review. Nutr. Hosp. 2015, 32, 2390–2399. [Google Scholar] [CrossRef] [PubMed]
- Quarta, S.; Massaro, M.; Chervenkov, M.; Ivanova, T.; Dimitrova, D.; Jorge, R.; Andrade, V.; Philippou, E.; Zisimou, C.; Maksimova, V.; et al. Persistent moderate-to-weak Mediterranean diet adherence and low scoring for plant-based foods across several southern European countries: Are we overlooking the Mediterranean diet recommendations? Nutrients 2021, 13, 1432. [Google Scholar] [CrossRef] [PubMed]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Williams, J.; Buoncristiano, M.; Nardone, P.; Rito, A.I.; Spinelli, A.; Hejgaard, T.; Kierkegaard, L.; Nurk, E.; Kunešová, M.; Milanović, S.M.; et al. A snapshot of European children’s eating habits: Results from the fourth round of the WHO European childhood obesity surveillance initiative (COSI). Nutrients 2020, 12, 241. [Google Scholar] [CrossRef]
- BOE.es—BOE-A-2020-3692 Real Decreto 463/2020, de 14 de Marzo, Por El Que Se Declara El Estado de Alarma Para la Gestión de la Situación de Crisis Sanitaria Ocasionada Por El COVID-19. Available online: https://www.boe.es/eli/es/rd/2020/03/14/463 (accessed on 19 May 2021).
- Fernández-Aranda, F.; Munguía, L.; Mestre-Bach, G.; Steward, T.; Etxandi, M.; Baenas, I.; Granero, R.; Sánchez, I.; Ortega, E.; Andreu, A.; et al. COVID Isolation Eating Scale (CIES): Analysis of the impact of confinement in eating disorders and obesity—A collaborative international study. Eur. Eat. Disord. Rev. 2020, 28, 871–883. [Google Scholar] [CrossRef]
- Graell, M.; Morón-Nozaleda, M.G.; Camarneiro, R.; Villaseñor, Á.; Yáñez, S.; Muñoz, R.; Martínez-Núñez, B.; Miguélez-Fernández, C.; Muñoz, M.; Faya, M. Children and adolescents with eating disorders during COVID-19 confinement: Difficulties and future challenges. Eur. Eat. Disord. Rev. 2020, 28, 864–870. [Google Scholar] [CrossRef]
- UNESCO. The Mediterranean Diet. Intangible Heritage. Available online: http://www.unesco.org/archives/multimedia/document-1680-eng-2 (accessed on 13 May 2021).
- Donini, L.M.; Serra-Majem, L.; Bulló, M.; Gil, Á.; Salas-Salvadó, J. The Mediterranean diet: Culture, health and science. Br. J. Nutr. 2015, 113, S1–S3. [Google Scholar] [CrossRef]
- Aranceta-Bartrina, J.; Partearroyo, T.; López-Sobaler, A.M.; Ortega, R.M.; Varela-Moreiras, G.; Serra-Majem, L.; Pérez-Rodrigo, C. Updating the food-based dietary guidelines for the Spanish population: The Spanish society of community nutrition (SENC) proposal. Nutrients 2019, 11, 2675. [Google Scholar] [CrossRef]
- Jardí, C.; Aranda, N.; Bedmar, C.; Arija, V. Excess nutritional risk in infants and toddlers in a Spanish city. Int. J. Vitam. Nutr. Res. 2019, 89, 210–220. [Google Scholar] [CrossRef]
- Ministry of Agriculture, Fisheries and Food of Spain. Report on Food Consumption in Spain. 2019. Available online: https://www.mapa.gob.es/es/alimentacion/temas/consumo-tendencias/informe2019_v2_tcm30-540250.pdf (accessed on 13 May 2021).
- Hernández-López, I.; Ortiz-Solà, J.; Alamprese, C.; Barros, L.; Shelef, O.; Basheer, L.; Rivera, A.; Abadias, M.; Aguiló-Aguayo, I. Valorization of Local Legumes and Nuts as Key Components of the Mediterranean Diet. Foods 2022, 11, 3858. [Google Scholar] [CrossRef]
- Harris, J.L.; Romo-Palafox, M.J.; Gershman, H.; Kagan, I.; Duffy, V. Healthy Snacks and Drinks for Toddlers: A Qualitative Study of Caregivers’ Understanding of Expert Recommendations and Perceived Barriers to Adherence. Nutrients 2023, 15, 1006. [Google Scholar] [CrossRef]
- Dalmau, J.; Peña-Quintana, L.; Moráis, A.; Martínez, V.; Varea, V.; Martínez, M.J.; Soler, B. Quantitative analysis of nutrient intake in children under 3 years old. ALSALMA study. An. Pediatr. 2015, 82, 255–266. [Google Scholar] [CrossRef]
- Madrigal, C.; Soto-Méndez, M.J.; Hernández-Ruiz, Á.; Valero, T.; Lara Villoslada, F.; Leis, R.; Martínez de Victoria, E.; Moreno, J.M.; Ortega, R.M.; Ruiz- López, M.D.; et al. Dietary intake, nutritional adequacy, and food sources of protein and relationships with personal and family factors in Spanish children aged one to <10 years: Findings of the EsNuPi study. Nutrients 2021, 13, 1062. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Martínez, R.; Mafla-España, M.A.; Cauli, O. Mediterranean Diet Adherence in Community-Dwelling Older Adults in Spain: Social Determinants Related to the Family. Nutrients 2022, 14, 5141. [Google Scholar] [CrossRef]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific Opinion on Dietary Reference Values for protein. EFSA J. 2012, 10, 2557, Updated 2015. [Google Scholar] [CrossRef]
- Balan, I.M.; Gherman, E.D.; Gherman, R.; Brad, I.; Pascalau, R.; Popescu, G.; Trasca, T.I. Sustainable Nutrition for Increased Food Security Related to Romanian Consumers’ Behavior. Nutrients 2022, 14, 4892. [Google Scholar] [CrossRef] [PubMed]
- Cardamone, E.; Di Benedetto, R.; Lorenzoni, G.; Gallipoli, S.; Ghidina, M.; Zobec, F.; Iacoponi, F.; Gregori, D.; Silano, M. Adherence to Mediterranean diet in Italy (ARIANNA) cross-sectional survey: Study protocol. BMJ Open 2023, 13, e067534. [Google Scholar] [CrossRef]
- Wärnberg, J.; Pérez-Farinós, N.; Benavente-Marín, J.C.; Gómez, S.F.; Labayen, I.G.; Zapico, A.; Gusi, N.; Aznar, S.; Alcaraz, P.E.; González-Valeiro, M.; et al. Screen Time and Parents’ Education Level Are Associated with Poor Adherence to the Mediterranean Diet in Spanish Children and Adolescents: The PASOS Study. J. Clin. Med. 2021, 10, 795. [Google Scholar] [CrossRef]
- Arenaza, L.; Medrano, M.; Oses, M.; Amasene, M.; Díez, I.; Rodríguez-Vigil, B.; Labayen, I. The Effect of a Family-Based Lifestyle Education Program on Dietary Habits, Hepatic Fat and Adiposity Markers in 8–12-Year-Old Children with Overweight/Obesity. Nutrients 2020, 12, 1443. [Google Scholar] [CrossRef] [PubMed]
- Ghisolfi, J.; Fantino, M.; Turck, D.; De Courcy, G.P.; Vidailhet, M. Nutrient intakes of children aged 1–2 years as a function of milk consumption, cows’ milk or growing-up milk. Public Health Nutr. 2013, 16, 524–534. [Google Scholar] [CrossRef]
- Diamantis, D.V.; Katsas, K.; Kalogiannis, D.; Kouvari, M.; Linos, A. Health-Related Quality of Life in Childhood and Adolescence: The Interrelation with Level of Adherence to Mediterranean Diet and Dietary Trajectories: Highlights from the DIATROFI Program (2021–2022). Nutrients 2023, 15, 1829. [Google Scholar] [CrossRef]
- Juton, C.; Berruezo, P.; Rajmil, L.; Lerin, C.; Fíto, M.; Homs, C.; Según, G.; Gómez, S.F.; Schröder, H. Prospective Association between Adherence to the Mediterranean Diet and Health-Related Quality of Life in Spanish Children. Nutrients 2022, 14, 5304. [Google Scholar] [CrossRef] [PubMed]
- D’Ascenzi, F.; Sciaccaluga, C.; Cameli, M.; Cecere, A.; Ciccone, M.M.; Di Francesco, S.; Ganau, A.; Imbalzano, E.; Liga, R.; Palermo, P.; et al. When should cardiovascular prevention begin? The importance of antenatal, perinatal and primordial prevention. Eur. J. Prev. Cardiol. 2021, 28, 361–369. [Google Scholar] [CrossRef]
- Drozdz, D.; Alvarez-Pitti, J.; Wójcik, M.; Borghi, C.; Gabbianelli, R.; Mazur, A.; Herceg-Čavrak, V.; Lopez-Valcarcel, B.G.; Brzeziński, M.; Lurbe, E.; et al. Obesity and Cardiometabolic Risk Factors: From Childhood to Adulthood. Nutrients 2021, 13, 4176. [Google Scholar] [CrossRef]
- Capra, M.E.; Pederiva, C.; Viggiano, C.; De Santis, R.; Banderali, G.; Biasucci, G. Nutritional Approach to Prevention and Treatment of Cardiovascular Disease in Childhood. Nutrients 2021, 13, 2359. [Google Scholar] [CrossRef]
- Funtikova, A.N.; Navarro, E.; Bawaked, R.A.; Fíto, M.; Schröder, H. Impact of diet on cardiometabolic health in children and adolescents. Nutr. J. 2015, 14, 118. [Google Scholar] [CrossRef]
- Lovell, A.L.; Davies, P.S.W.; Hill, R.J.; Milne, T.; Matsuyama, M.; Jiang, Y.; Chen, R.X.; Grant, C.C.; Wall, C.R. A comparison of the effect of a Growing Up Milk-Lite (GUMLi) v. cows’ milk on longitudinal dietary patterns and nutrient intakes in children aged 12–23 months: The GUMLi randomised controlled trial. Br. J. Nutr. 2019, 121, 678–687. [Google Scholar] [CrossRef]
- Choi, B.C.K.; Pak, A.W.P. A catalog of biases in questionnaires. Prev. Chronic Dis. 2005, 2, A13. [Google Scholar]
- Ghisolfi, J.; Vidailhet, M.; Fantino, M.; Bocquet, A.; Bresson, J.L.; Briend, A.; Chouraqui, J.P.; Darmaun, D.; Dupont, C.; Frelut, M.L.; et al. Cows’ milk or growing-up milk: What should we recommend for children between 1 and 3 years of age? Arch. Pediatr. 2011, 18, 355–358. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.D.; Zhu, Y.; Vanage, V.; Jain, N.; Holschuh, N.; Agler, A.H. Association between ready-to-eat cereal consumption and nutrient intake, nutritional adequacy, and diet quality among infants, toddlers, and children in the national health and nutrition examination survey 2015–2016. Nutrients 2019, 11, 1989. [Google Scholar] [CrossRef]
- Mahmood, L.; Flores-Barrantes, P.; Moreno, L.A.; Manios, Y.; Gonzalez-Gil, E.M. The influence of parental dietary behaviors and practices on children’s eating habits. Nutrients 2021, 13, 1138. [Google Scholar] [CrossRef] [PubMed]
- Blissett, J. Relationships between parenting style, feeding style and feeding practices and fruit and vegetable consumption in early childhood. Appetite 2011, 57, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Program of Feeding, Nutrition and Gastronomy for Pre-School Education (PANGEI). Available online: https://sede.educacion.gob.es/publiventa/d/20892/19/1 (accessed on 19 April 2021).
- Grosso, G.; Galvano, F. Mediterranean diet adherence in children and adolescents in southern European countries. NFS J. 2016, 3, 13–19. [Google Scholar] [CrossRef]
- Balan, I.M.; Gherman, E.D.; Brad, I.; Gherman, R.; Horablaga, A.; Trasca, T.I. Metabolic Food Waste as Food Insecurity Factor-Causes and Preventions. Foods 2022, 11, 2179. [Google Scholar] [CrossRef] [PubMed]

|
| Item | N (%) * |
|---|---|
| Breastfeeding duration | |
| No breastfeeding | 361 (14.92) |
| Less than 6 months | 665 (27.49) |
| Between 6 and 12 months | 490 (20.26) |
| More than 12 months | 903 (37.33) |
| Age of infant formula introduction | |
| From birth | 427 (20.66) |
| Before 6 months | 1015 (49.10) |
| Between 6 and 12 months | 413 (19.98) |
| Between 13 and 18 months | 177 (8.56) |
| Between 19 and 24 months | 20 (0.97) |
| More than 24 months | 15 (0.73) |
| Milk type being consumed | |
| Breastfeeding | 517 (20.97) |
| Infant formula (formula 1) | 26 (1.05) |
| Follow-on formula (formula 2) | 204 (8.28) |
| Growing-up milk (formula 3) | 543 (22.03) |
| Cow’s milk | 1132 (45.92) |
| Plant-based 1 milk | 25 (1.01) |
| No milk | 18 (0.73) |
| Item | N (%) * |
|---|---|
| Usually, your child eats… | |
| …too much | 127 (5.15) |
| …well | 1950 (79.11) |
| …little | 307 (12.45) |
| …nothing or almost nothing, he/she is a bad eater | 81 (3.29) |
| How often does your child have lunch or dinner with an adult/adults? | |
| Every day | 1316 (53.39) |
| A few days a week | 835 (33.87) |
| Never | 233 (9.45) |
| Only at weekends | 81 (3.29) |
| How often does your family have fast food? | |
| Never | 1187 (48.15) |
| Once or twice a week | 1235 (50.10) |
| Three or four times a week | 36 (1.46) |
| Five or more times a week | 7 (0.28) |
| Water (1 glass) | |
| Never | 18 (0.73) |
| Once or twice a day | 501 (20.32) |
| Three or four times a day | 986 (40.00) |
| Five or more times a day | 960 (38.95) |
| Milk (1 glass) | |
| Never | 202 (8.19) |
| Once or twice a day | 1596 (64.75) |
| Three or four times a day | 556 (22.56) |
| Five or more times a day | 111 (4.50) |
| Dairy products (yoghourt, cheese, and other) (1 cup, 1 glass, or 2 slices) | |
| Never | 55 (2.23) |
| Once or twice a week | 266 (10.79) |
| Three or more times a week | 505 (20.49) |
| Once or twice a day | 1399 (56.75) |
| Three or more times a day | 240 (9.74) |
| Milk and dairy products | |
| Never | 13 (0.53) |
| Once or twice a week | 33 (1.34) |
| Three or more times a week | 53 (2.15) |
| Once or twice a day | 544 (22.07) |
| Three to four times a day | 1184 (48.03) |
| Four or more times a day | 24 (0.97) |
| Five or more times a day | 614 (24.91) |
| Vegetables (salads and vegetables) (1 dish) | |
| Never | 82 (3.33) |
| Once or twice a week | 368 (14.93) |
| Three or four times a week | 576 (23.37) |
| Once a day | 901 (36.55) |
| More than once a day | 538 (21.83) |
| Fruit (fresh or canned) | |
| Never | 79 (3.20) |
| Once or twice a week | 189 (7.67) |
| Three or four times a week | 322 (13.06) |
| Once a day | 1021 (41.42) |
| More than once a day | 854 (34.65) |
| Cereals (baby food, breakfast cereals, bread) (1 bowl or 2 slices) | |
| Never | 157 (6.37) |
| Once a day | 1417 (57.48) |
| Twice or three times a day | 840 (34.08) |
| More than three times a day | 51 (2.07) |
| Pasta, white rice, or potatoes (1 dish) | |
| Never | 56 (2.27) |
| Once or twice a week | 1103 (44.75) |
| Three or four times a week | 953 (38.66) |
| Once a day | 353 (14.32) |
| Pulses (lentils, beans, chickpeas) (1 dish) | |
| Never | 111 (4.50) |
| Once or twice a month | 388 (15.74) |
| Once or twice a week | 1539 (62.43) |
| Three or four times a week | 391 (15.86) |
| Once a day | 36 (1.46) |
| Meat (minced meat, red meat, chicken, and turkey) (1 fillet) | |
| Never | 40 (1.62) |
| Once or twice a month | 75 (3.04) |
| Once or twice a week | 681 (27.63) |
| Three or four times a week | 1239 (50.26) |
| Once a day | 430 (17.44) |
| Fish (fish and seafood) (1 fillet) | |
| Never | 63 (2.56) |
| Once or twice a month | 227 (9.21) |
| Once or twice a week | 1255 (50.91) |
| Three or four times a week | 801 (32.49) |
| Once a day | 119 (4.83) |
| Eggs (1 egg) | |
| Never | 128 (5.19) |
| Once or twice a month | 283 (11.48) |
| Once or twice a week | 1690 (68.56) |
| Three or four times a week | 323 (13.10) |
| Once a day | 41 (1.66) |
| Sugary drinks (soft drinks, processed fruit juices) (1 glass) | |
| Never | 1625 (65.92) |
| Once or twice a month | 279 (11.32) |
| Once or twice a week | 295 (11.97) |
| Three or four times a week | 126 (5.11) |
| Once a day | 140 (5.68) |
| Cookies, processed baked goods, chocolate, candies | |
| Never | 558 (22.64) |
| Once or twice a month | 443 (17.97) |
| Once or twice a week | 727 (29.49) |
| Three or four times a week | 335 (13.59) |
| Once a day | 402 (16.31) |
| Product Type, n (%) | Age | Total | p Value | ||
|---|---|---|---|---|---|
| 12–18 mo. | 19–24 mo. | ≥25 mo. | |||
| Water | 753 (71.37) | 549 (83.56) | 644 (85.20) | 1946 (78.95) | <0.001 |
| Milk/dairy products | 479 (45.40) | 335 (50.99) | 370 (49.14) | 1184 (48.03) | <0.001 |
| Vegetables/salads | 727 (68.91) | 370 (56.32) | 342 (45.42) | 1439 (58.38) | 0.862 |
| Fruits | 831 (78.77) | 512 (77.93) | 532 (70.65) | 1875 (76.06) | 0.010 |
| Bread/cereals | 415 (39.37) | 231 (35.16) | 245 (32.54) | 891 (36.15) | <0.001 |
| Pasta/rice/potatoes | 527 (49.95) | 371 (56.47) | 408 (54.18) | 1306 (52.98) | <0.001 |
| Pulses | 819 (77.63) | 544 (82.80) | 603 (80.08) | 1966 (79.76) | 0.708 |
| Meat | 823 (78.01) | 507 (77.17) | 590 (78.35) | 1920 (77.89) | 0.033 |
| Fish | 946 (89.67) | 577 (87.82) | 652 (86.59) | 2175 (88.24) | 0.023 |
| Eggs | 717 (67.96) | 448 (68.19) | 525 (69.72) | 1690 (68.56) | 0.124 |
| Soft drinks/fruit juices | 932 (88.34) | 486 (73.97) | 486 (65.54) | 1904 (77.24) | 0.067 |
| Cookies/processed baked goods | 846 (80.19) | 432 (65.75) | 450 (59.76) | 1728 (70.10) | <0.001 |
| Average adequate intake | 8.36 ± 1.84 | 8.16 ± 1.98 | 7.76 ± 1.93 | 8.12 ± 1.92 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reyes-Domínguez, A.I.; Bernabeu-Sendra, J.; Rodríguez-Sinovas, C.; Santamaria-Orleans, A.; de Castellar-Sanso, R.; Martinez-Perez, J. Post-Pandemic Feeding Patterns and Mediterranean Diet Adherence in Spanish Toddlers. Nutrients 2023, 15, 2049. https://doi.org/10.3390/nu15092049
Reyes-Domínguez AI, Bernabeu-Sendra J, Rodríguez-Sinovas C, Santamaria-Orleans A, de Castellar-Sanso R, Martinez-Perez J. Post-Pandemic Feeding Patterns and Mediterranean Diet Adherence in Spanish Toddlers. Nutrients. 2023; 15(9):2049. https://doi.org/10.3390/nu15092049
Chicago/Turabian StyleReyes-Domínguez, Ana Isabel, Javier Bernabeu-Sendra, Cristina Rodríguez-Sinovas, Alicia Santamaria-Orleans, Roser de Castellar-Sanso, and Jorge Martinez-Perez. 2023. "Post-Pandemic Feeding Patterns and Mediterranean Diet Adherence in Spanish Toddlers" Nutrients 15, no. 9: 2049. https://doi.org/10.3390/nu15092049
APA StyleReyes-Domínguez, A. I., Bernabeu-Sendra, J., Rodríguez-Sinovas, C., Santamaria-Orleans, A., de Castellar-Sanso, R., & Martinez-Perez, J. (2023). Post-Pandemic Feeding Patterns and Mediterranean Diet Adherence in Spanish Toddlers. Nutrients, 15(9), 2049. https://doi.org/10.3390/nu15092049