Assessment of Hydration, Nutritional Status and Arterial Stiffness in Hypertensive Chronic Kidney Disease Patients
Abstract
1. Introduction
2. Materials and Methods
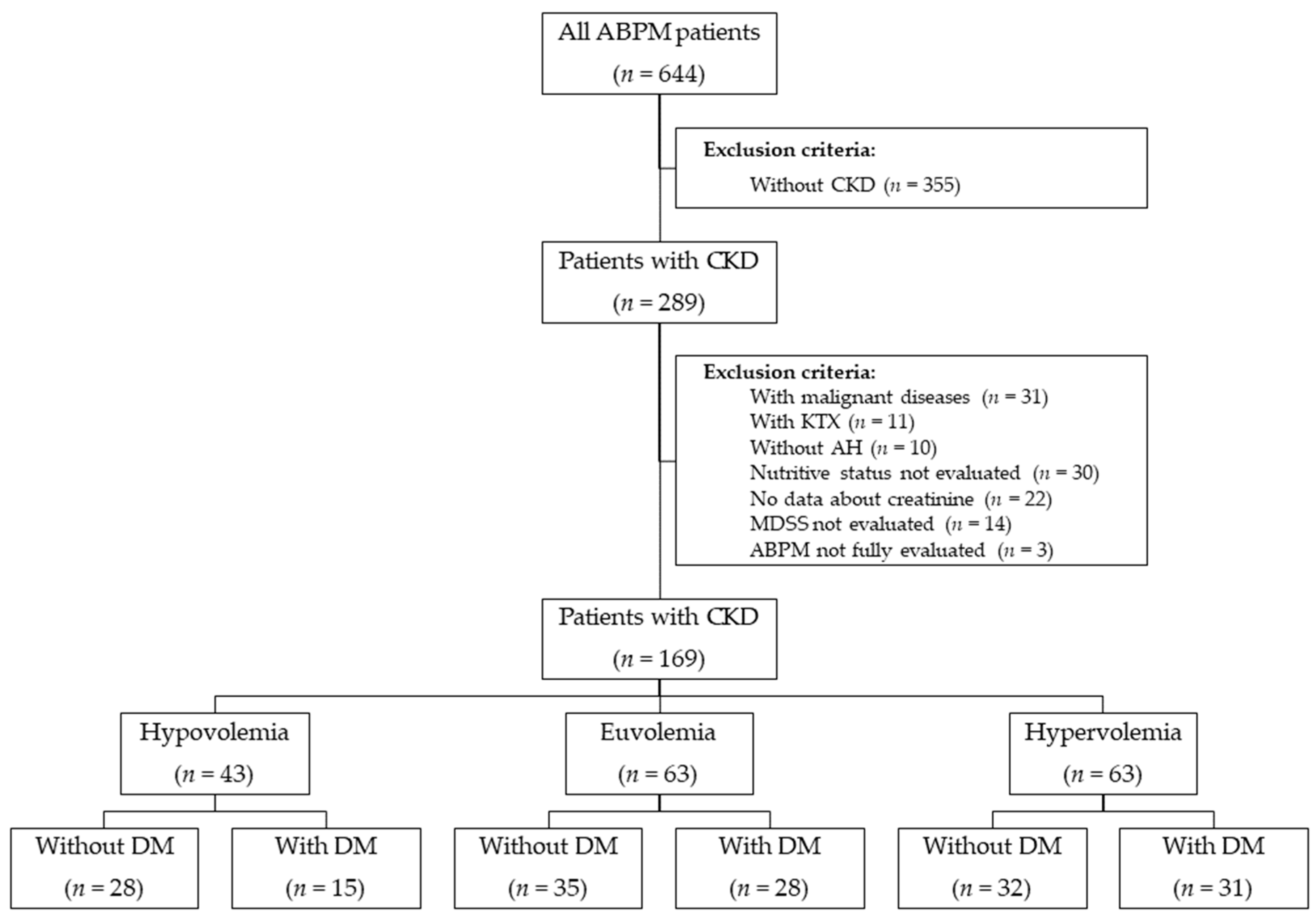
2.1. Study Population and Design
2.2. Body Composition and Fluid Status Measurements
2.3. Blood Pressure and Arterial Stiffness Measurements
2.4. Mediterranean Diet Serving Score (MDSS)
2.5. Medical History, Clinical and Laboratory Parameters
2.6. Statistical Analysis
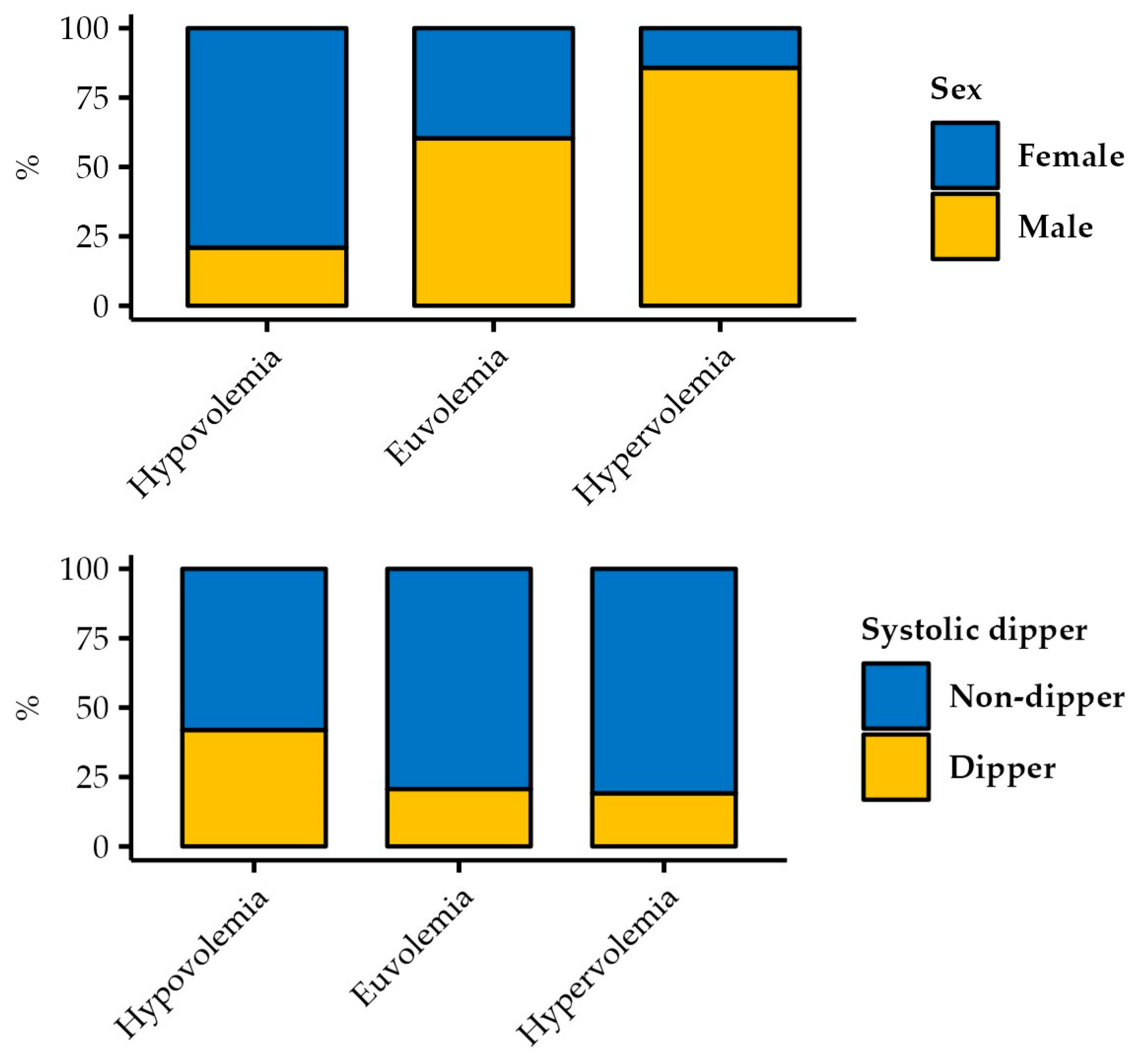
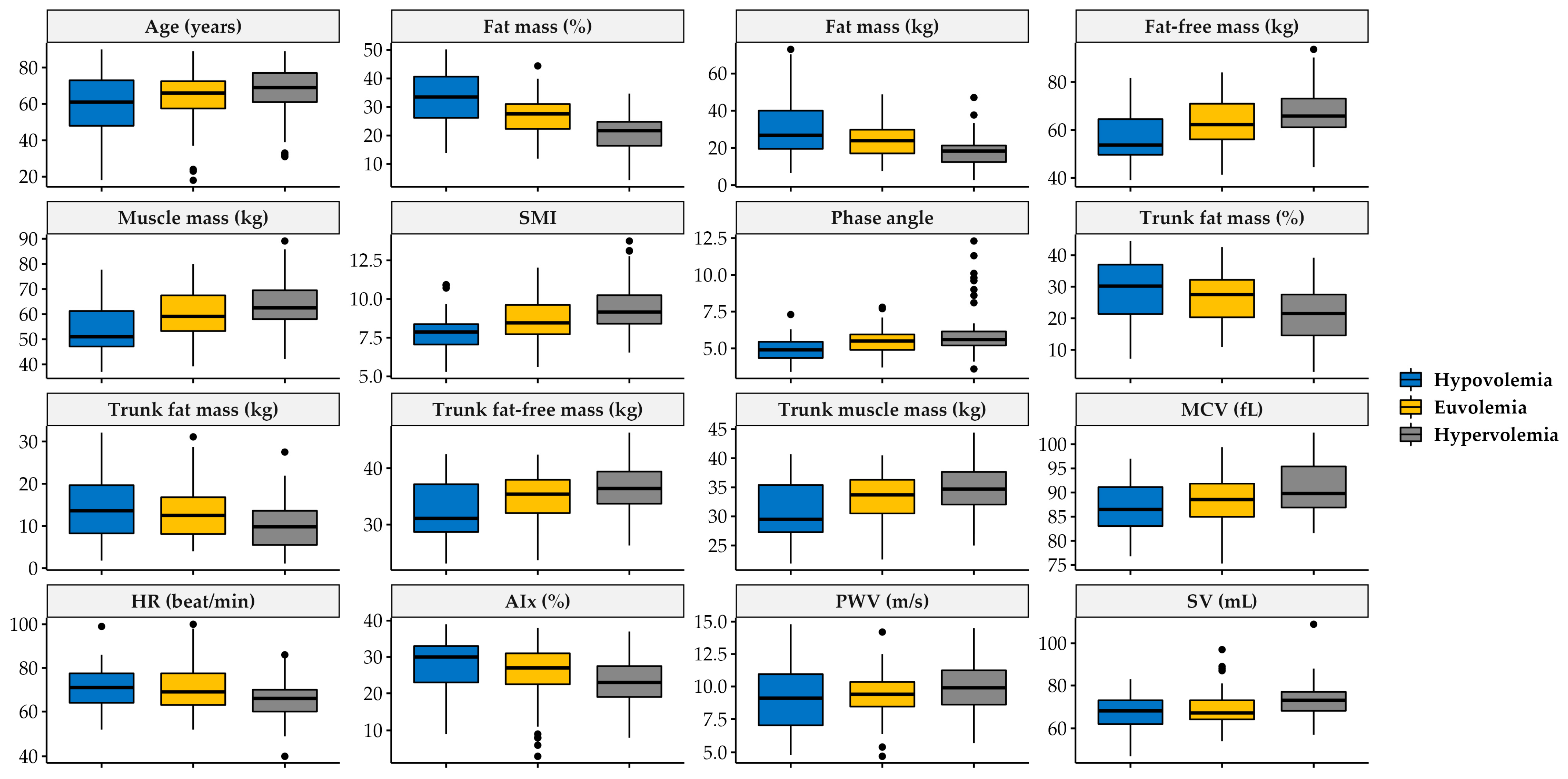
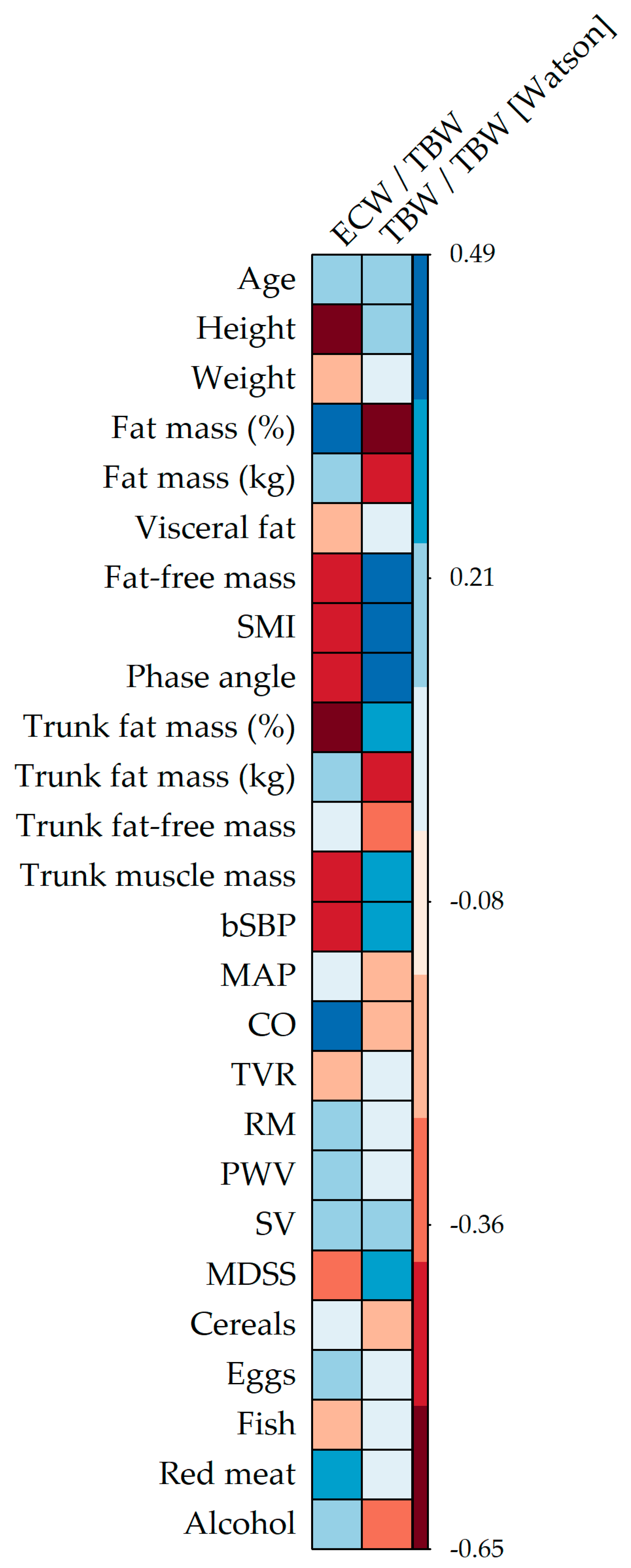
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yilmaz, A.; Yilmaz, B.; Küçükseymen, S.; Özpelit, E.; Pekel, N. Association of overhydration and cardiac dysfunction in patients have chronic kidney disease but not yet dialysis. Néphrologie Thérapeutique 2016, 12, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Tai, R.; Ohashi, Y.; Mizuiri, S.; Aikawa, A.; Sakai, K. Association between ratio of measured extracellular volume to expected body fluid volume and renal outcomes in patients with chronic kidney disease: A retrospective single-center cohort study. BMC Nephrol. 2014, 15, 189. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.-C.; Tsai, J.-C.; Chiu, Y.-W.; Kuo, H.-T.; Chen, S.-C.; Hwang, S.-J.; Chen, T.-H.; Kuo, M.-C.; Chen, H.-C. Is fluid overload more important than diabetes in renal progression in late chronic kidney disease? PLoS ONE 2013, 8, e82566. [Google Scholar] [CrossRef] [PubMed]
- Tzamaloukas, A.H.; Khitan, Z.J.; Glew, R.H.; Roumelioti, M.E.; Rondon-Berrios, H.; Elisaf, M.S.; Raj, D.S.; Owen, J.; Sun, Y.; Siamopoulos, K.C.; et al. Serum sodium concentration and tonicity in hyperglycemic crises: Major influences and treatment implications. J. Am. Heart Assoc. 2019, 8, e011786. [Google Scholar] [CrossRef]
- Tsai, Y.-C.; Tsai, J.-C.; Chen, S.-C.; Chiu, Y.-W.; Hwang, S.-J.; Hung, C.-C.; Chen, T.-H.; Kuo, M.-C.; Chen, H.-C. Association of fluid overload with kidney disease progression in advanced CKD: A prospective cohort study. Am. J. Kidney Dis. 2014, 63, 68–75. [Google Scholar] [CrossRef]
- Di Loreto, V.; Moreno, H.S.; Puche, R.C.; Locatto, M.E. Severe hyperglycemia: A determinant factor for hypofiltration in alloxan diabetic rats. Acta Diabetol. 2004, 41, 56–62. [Google Scholar] [CrossRef]
- Brownlee, M. Glycation Products and the Pathogenesis of Diabetic Complications. Diabetes Care 1992, 15, 1835–1843. [Google Scholar] [CrossRef]
- Low, S.; Pek, S.; Liu, Y.L.; Moh, A.; Ang, K.; Tang, W.E.; Lim, Z.; Subramaniam, T.; Sum, C.F.; Lim, C.L.; et al. Higher extracellular water to total body water ratio was associated with chronic kidney disease progression in type 2 diabetes. J. Diabetes Its Complicat. 2021, 35, 107930. [Google Scholar] [CrossRef]
- Palmer, B.F.; Clegg, D.J. Fluid overload as a therapeutic target for the preservative management of chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 2020, 29, 22–28. [Google Scholar] [CrossRef]
- Chen, S.-C.; Chang, J.-M.; Liu, W.-C.; Tsai, Y.-C.; Tsai, J.-C.; Hsu, P.-C.; Lin, T.-H.; Lin, M.-Y.; Su, H.-M.; Hwang, S.-J.; et al. Brachial-ankle pulse wave velocity and rate of renal function decline and mortality in chronic kidney disease. Clin. J. Am. Soc. Nephrol. 2011, 6, 724–732. [Google Scholar] [CrossRef]
- Park, S.; Lee, C.J.; Jhee, J.H.; Yun, H.R.; Kim, H.; Jung, S.Y.; Kee, Y.K.; Yoon, C.Y.; Park, J.T.; Kim, H.C.; et al. Extracellular fluid excess is significantly associated with coronary artery calcification in patients with chronic kidney disease. J. Am. Heart Assoc. 2018, 7, e008935. [Google Scholar] [CrossRef] [PubMed]
- Tonelli, M.; Wiebe, N.; Culleton, B.; House, A.; Rabbat, C.; Fok, M.; McAlister, F.; Garg, A.X. Chronic kidney disease and mortality risk. J. Am. Soc. Nephrol. 2006, 17, 2034–2047. [Google Scholar] [CrossRef]
- Ortiz, A.; Covic, A.; Fliser, D.; Fouque, D.; Goldsmith, D.; Kanbay, M.; Mallamaci, F.; Massy, Z.A.; Rossignol, P.; Vanholder, R.; et al. Epidemiology, contributors to, and clinical trials of mortality risk in chronic kidney failure. Lancet 2014, 383, 1831–1843. [Google Scholar] [CrossRef]
- Ekinci, C.; Karabork, M.; Siriopol, D.; Dincer, N.; Covic, A.; Kanbay, M. Effects of volume overload and current techniques for the assessment of fluid status in patients with renal disease. Blood Purif. 2018, 46, 34–47. [Google Scholar] [CrossRef] [PubMed]
- Mitsides, N.; McHugh, D.; Swiecicka, A.; Mitra, R.; Brenchley, P.; Parker, G.J.; Mitra, S. Extracellular resistance is sensitive to tissue sodium status; implications for bioimpedance-derived fluid volume parameters in chronic kidney disease. J. Nephrol. 2019, 33, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Ohashi, Y.; Otani, T.; Tai, R.; Tanaka, Y.; Sakai, K.; Aikawa, A. Assessment of body composition using dry mass index and ratio of total body water to estimated volume based on bioelectrical impedance analysis in chronic kidney disease patients. J. Ren. Nutr. 2013, 23, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Watson, P.E.; Watson, I.D.; Batt, R.D. Total body water volumes for adult males and females estimated from simple anthropometric measurements. Am. J. Clin. Nutr. 1980, 33, 27–39. [Google Scholar] [CrossRef]
- Pérez-Torres, A.; Caverni-Muñoz, A.; González García, E. Mediterranean Diet and Chronic Kidney Disease (CKD): A Practical Approach. Nutrients 2023, 15, 97. [Google Scholar] [CrossRef]
- Chauveau, P.; Aparicio, M.; Bellizzi, V.; Campbell, K.; Hong, X.; Johansson, L.; Kolko, A.; Molina, P.; Sezer, S.; Wanner, C.; et al. Mediterranean diet as the diet of choice for patients with chronic kidney disease. Nephrol. Dial. Transplant. 2018, 33, 725–735. [Google Scholar] [CrossRef]
- Karaaslan, D.C.; Afsar, B.; Kanbay, M. Is relative overhydration measurement by bioimpedance spectroscopy useful in reducing morbidity and mortality in chronic kidney disease? Clin. Kidney J. 2018, 11, 370–371. [Google Scholar] [CrossRef]
- Vega, A.; Abad, S.; Macías, N.; Aragoncillo, I.; García-Prieto, A.; Linares, T.; Torres, E.; Hernández, A.; Luño, J. Any grade of relative overhydration is associated with long-term mortality in patients with stages 4 and 5 non-dialysis chronic kidney disease. Clin. Kidney J. 2018, 11, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Hur, E.; Usta, M.; Toz, H.; Asci, G.; Wabel, P.; Kahvecioglu, S.; Kayikcioglu, M.; Demirci, M.S.; Ozkahya, M.; Duman, S.; et al. Effect of fluid management guided by bioimpedance spectroscopy on cardiovascular parameters in hemodialysis patients: A randomized controlled trial. Am. J. Kidney Dis. 2013, 61, 957–965. [Google Scholar] [CrossRef]
- Onofriescu, M.; Hogas, S.; Voroneanu, L.; Apetrii, M.; Nistor, I.; Kanbay, M.; Covic, A.C. Bioimpedance-guided fluid management in maintenance hemodialysis: A pilot randomized controlled trial. Am. J. Kidney Dis. 2014, 64, 111–118. [Google Scholar] [CrossRef]
- Mc780—User Manual. Available online: https://tanita.eu/media/wysiwyg/manuals/medical-approved-body-composition-monitors/mc-780-portable-instruction-manual.pdf (accessed on 12 January 2022).
- IEM Mobil-O-Graph—User Mannual. Available online: https://medaval.ie/docs/manuals/IEM-Mobil-O-Graph-Manual.pdf (accessed on 26 January 2021).
- Monteagudo, C.; Mariscal-Arcas, M.; Rivas, A.; Lorenzo-Tovar, M.L.; Tur, J.A.; Olea-Serrano, F. Proposal of a Mediterranean Diet Serving Score. PLoS ONE 2015, 10, e0128594. [Google Scholar] [CrossRef] [PubMed]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria. 2020. Available online: https://www.r-project.org/ (accessed on 24 April 2020).
- Khan, Y.H.; Sarriff, A.; Adnan, A.S.; Khan, A.H.; Mallhi, T.H. Chronic Kidney Disease, Fluid Overload and Diuretics: A Complicated Triangle. PLoS ONE 2016, 11, e0159335. [Google Scholar] [CrossRef]
- Usama, H.; Cimini, M.; Handelman, G.J.; Raimann, J.G.; Li, L.; Abbas, S.R.; Kotanko, P.; Levin, N.W.; Finkelstein, F.O.; Zhu, F. Identification of fluid overload in elderly patients with chronic kidney disease using bioimpedance techniques. J. Appl. Physiol. 2022, 133, 205–213. [Google Scholar]
- Ekingen, T.; Sob, C.; Hartmann, C.; Rühli, F.J.; Matthes, K.L.; Staub, K.; Bender, N. Associations between hydration status, body composition, sociodemographic and lifestyle factors in the general population: A cross-sectional study. BMC Public Health 2022, 22, 900. [Google Scholar] [CrossRef]
- Mayne, K.J.; Shemilt, R.; Keane, D.F.; Lees, J.S.; Mark, P.B.; Herrington, W.G. Bioimpedance Indices of Fluid Overload and Cardiorenal Outcomes in Heart Failure and Chronic Kidney Disease: A Systematic Review. J. Card. Fail. 2022, 28, 1628–1641. [Google Scholar] [CrossRef]
- Akamatsu, Y.; Kusakabe, T.; Arai, H.; Yamamoto, Y.; Nakao, K.; Ikeue, K.; Ishihara, Y.; Tagami, T.; Yasoda, A.; Ishii, K.; et al. Phase angle from bioelectrical impedance analysis is a useful indicator of muscle quality. J. Cachexia Sarcopenia Muscle 2022, 13, 180–189. [Google Scholar] [CrossRef]
- McEniery, C.M.; Hall, Y.I.R.; Qasem, A.; Wilkinson, I.B.; Cockcroft, J.R. Normal Vascular Aging: Differential Effects on Wave Reflection and Aortic Pulse Wave Velocity: The Anglo-Cardiff Collaborative Trial (ACCT). J. Am. Coll. Cardiol. 2005, 46, 1753–1760. [Google Scholar] [CrossRef] [PubMed]
- Al-Sofiani, M.E.; Ganji, S.S.; Kalyani, R.R. Body composition changes in diabetes and aging. J. Diabetes Its Complicat. 2019, 33, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Zatterale, F.; Longo, M.; Naderi, J.; Raciti, G.A.; Desiderio, A.; Miele, C.; Beguinot, F. Chronic Adipose Tissue Inflammation Linking Obesity to Insulin Resistance and Type 2 Diabetes. Front. Physiol. 2020, 10, 1607. [Google Scholar] [CrossRef] [PubMed]
- De Rosa, S.; Arcidiacono, B.; Chiefari, E.; Brunetti, A.; Indolfi, C.; Foti, D.P. Type 2 Diabetes Mellitus and Cardiovascular Disease: Genetic and Epigenetic Links. Front. Endocrinol. 2018, 9, 2. [Google Scholar] [CrossRef] [PubMed]
- Pop-Busui, R. Cardiac autonomic neuropathy in diabetes: A clinical perspective. Diabetes Care 2010, 33, 434–441. [Google Scholar] [CrossRef]
- Balcıoğlu, A.S.; Müderrisoğlu, H. Diabetes and cardiac autonomic neuropathy: Clinical manifestations, cardiovascular consequences, diagnosis and treatment. World J. Diabetes 2015, 6, 80–91. [Google Scholar] [CrossRef]
- Park, C.; Pagnini, F.; Langer, E. Glucose metabolism responds to perceived sugar intake more than actual sugar intake. Sci. Rep. 2020, 10, 15633. [Google Scholar] [CrossRef]
- Mamo, Y.; Bekele, F.; Nigussie, T.; Zewudie, A. Determinants of poor glycemic control among adult patients with type 2 diabetes mellitus in Jimma University Medical Center, Jimma zone, south west Ethiopia: A case control study. BMC Endocr. Disord. 2019, 19, 91. [Google Scholar] [CrossRef]
- Tzamaloukas, A.H.; Konstantinov, N.K.; Sun, Y.; Ing, T.S.; Dorin, R.I.; Malhotra, D.; Murata, G.H.; Shapiro, J.I. Principles of Quantitative Fluid and Cation Replacement in Extreme Hyperglycemia. Cureus 2013, 5, e110. [Google Scholar] [CrossRef]
- Meeuwsen, S.; Horgan, G.W.; Elia, M. The relationship between BMI and percent body fat, measured by bioelectrical impedance, in a large adult sample is curvilinear and influenced by age and sex. Clin. Nutr. 2010, 29, 560–566. [Google Scholar] [CrossRef]
- Bredella, M.A. Sex Differences in Body Composition. Adv. Exp. Med. Biol. 2017, 1043, 9–27. [Google Scholar] [CrossRef] [PubMed]
- Sarzani, R.; Laureti, G.; Gezzi, A.; Spannella, F.; Giulietti, F. Single-pill fixed-dose drug combinations to reduce blood pressure: The right pill for the right patient. Ther. Adv. Chronic Dis. 2022, 13. [Google Scholar] [CrossRef] [PubMed]
- Parati, G.; Kjeldsen, S.; Coca, A.; Cushman, W.C.; Wang, J. Adherence to Single-Pill Versus Free-Equivalent Combination Therapy in Hypertension: A Systematic Review and Meta-Analysis. Hypertension 2021, 77, 692–705. [Google Scholar] [CrossRef]
| Category | Hypovolemia | Euvolemia | Hypervolemia | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Without DM (n = 28) | With DM (n = 15) | p * | Without DM (n = 35) | With DM (n = 28) | p * | Without DM (n = 32) | With DM (n = 31) | p * | |
| BMI (kg/m2), median (IQR) | 27.77 (6.46) | 33.47 (9.01) | 0.021 | 27.2 (7.05) | 28.6 (3.85) | 0.083 | 27.2 (4.38) | 28.44 (4.2) | 0.256 |
| Visceral fat level, median (IQR) | 7.5 (4.25) | 10 (9) | 0.050 | 9.31 (4.48) | 12 (5.57) | 0.038 | 9.09 (4.08) | 10.61 (4.07) | 0.144 |
| Metabolic age (years), median (IQR) | 52.21 (17.19) | 63.87 (12.02) | 0.025 | 52.94 (15.5) | 62.82 (15.69) | 0.015 | 53.12 (13.77) | 58.06 (12.26) | 0.138 |
| SMI, median (IQR) | 7.48 (1.01) | 8.49 (1.49) | 0.012 | 8.41 (1.24) | 8.98 (1.4) | 0.089 | 9.16 (1.76) | 9.16 (2.09) | 0.532 |
| Trunk fat-free mass (kg), mean (SD) | 31.28 (4.96) | 34.43 (4.56) | 0.048 | 35 (5.95) | 35.85 (5.12) | 0.515 | 36.65 (4.02) | 36.46 (4.04) | 0.851 |
| FBG (mmol/L), median (IQR) | 5.25 (1.12) | 8.95 (6.85) | 0.001 | 5.6 (1.47) | 7.95 (1.93) | 0.002 | 6.25 (1.05) | 7.3 (1.7) | 0.017 |
| HbA1c (%), median (IQR) | 5.1 (NA) | 8 (2.23) | 0.301 | 6.05 (0.64) | 7.07 (1.07) | 0.212 | 5.79 (0.91) | 7.05 (0.95) | 0.014 |
| Leukocyte count (×109/L), median (IQR) | 8 (3.55) | 11.05 (8.15) | 0.223 | 7.45 (2.55) | 8 (1.85) | 0.098 | 6.8 (1.7) | 8.4 (3.4) | 0.016 |
| Presence of CVA disease, #n (%) | 1 (3.85) | 6 (40) | 0.011 | 6 (17.14) | 13 (46.43) | 0.025 | 10 (31.25) | 9 (29.03) | 1.000 |
| bDBP (mmHg), mean (SD) | 78 (11.44) | 78.2 (6.04) | 0.950 | 84.31 (10.61) | 74.18 (9.26) | <0.001 | 77.75 (13.57) | 78.71 (9.02) | 0.743 |
| MAP (mmHg), median (IQR) | 102.5 (13.9) | 105.07 (11.27) | 0.543 | 106.74 (10.2) | 98.54 (10.97) | 0.003 | 100.94 (13.8) | 106 (14.15) | 0.156 |
| PP (mmHg), median (IQR) | 52 (14.25) | 55 (11.5) | 0.339 | 47 (9.5) | 51 (12.75) | 0.098 | 50 (9.75) | 54 (18.5) | 0.018 |
| cSBP (mmHg), median (IQR) | 116 (20) | 121 (10) | 0.251 | 122.34 (10.69) | 115.82 (14.11) | 0.041 | 117.5 (18.75) | 121 (18) | 0.259 |
| cDBP (mmHg), mean (SD) | 80.04 (12.14) | 80.27 (6.16) | 0.945 | 86.23 (10.61) | 75.57 (9.6) | <0.001 | 79.34 (13.78) | 80.35 (9.76) | 0.739 |
| TVR (s/cm2), median (IQR) | 1753 (274.25) | 1733 (148) | 0.889 | 1807.97 (158.36) | 1713.21 (192.58) | 0.036 | 1766.5 (216.75) | 1707 (271) | 0.978 |
| Non-adherence to the MeDi, n (%) | 28 (100) | 15 (100) | 0.047 | 32 (91.43) | 24 (85.71) | 0.754 | 28 (87.5) | 28 (90.32) | 1.000 |
| Adherence to sweets recommendation, n (%) | 12 (42.86) | 12 (80) | 0.044 | 17 (48.57) | 19 (67.86) | 0.200 | 18 (56.25) | 26 (83.87) | 0.035 |
| Predictor | Beta | SE | p |
|---|---|---|---|
| Sex (female) * | −0.049 | 0.012 | <0.001 |
| Age (years) | 0.001 | 0.001 | 0.561 |
| BMI (kg/m2) * | −0.002 | 0.001 | 0.024 |
| PWV (m/s) | −0.001 | 0.008 | 0.866 |
| SV (mL) | 0.000 | 0.001 | 0.589 |
| Systolic dipper | −0.017 | 0.013 | 0.189 |
| BB use | 0.023 | 0.012 | 0.051 |
| ACE inhibitors use | −0.018 | 0.012 | 0.128 |
| ARB use | 0.007 | 0.017 | 0.686 |
| Moxonidine use | 0.015 | 0.012 | 0.208 |
| Diuretics use * | 0.026 | 0.012 | 0.028 |
| Oral hypoglycemic medication use* | 0.024 | 0.012 | 0.040 |
| ≥2 antihypertensives as a single-pill combination * | −0.037 | 0.014 | 0.009 |
| Adherence to recommended vegetable consumption | 0.009 | 0.014 | 0.526 |
| Adherence to recommended eggs consumption | −0.018 | 0.011 | 0.098 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radić, J.; Kolak, E.; Vučković, M.; Gelemanović, A.; Đogaš, H.; Bučan Nenadić, D.; Radić, M. Assessment of Hydration, Nutritional Status and Arterial Stiffness in Hypertensive Chronic Kidney Disease Patients. Nutrients 2023, 15, 2045. https://doi.org/10.3390/nu15092045
Radić J, Kolak E, Vučković M, Gelemanović A, Đogaš H, Bučan Nenadić D, Radić M. Assessment of Hydration, Nutritional Status and Arterial Stiffness in Hypertensive Chronic Kidney Disease Patients. Nutrients. 2023; 15(9):2045. https://doi.org/10.3390/nu15092045
Chicago/Turabian StyleRadić, Josipa, Ela Kolak, Marijana Vučković, Andrea Gelemanović, Hana Đogaš, Dora Bučan Nenadić, and Mislav Radić. 2023. "Assessment of Hydration, Nutritional Status and Arterial Stiffness in Hypertensive Chronic Kidney Disease Patients" Nutrients 15, no. 9: 2045. https://doi.org/10.3390/nu15092045
APA StyleRadić, J., Kolak, E., Vučković, M., Gelemanović, A., Đogaš, H., Bučan Nenadić, D., & Radić, M. (2023). Assessment of Hydration, Nutritional Status and Arterial Stiffness in Hypertensive Chronic Kidney Disease Patients. Nutrients, 15(9), 2045. https://doi.org/10.3390/nu15092045








