The Mediterranean Diet and Age-Related Eye Diseases: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Protocol Registration
2.2. Search Strategy
2.3. Eligible Criteria
2.4. Study Selection and Data Extraction
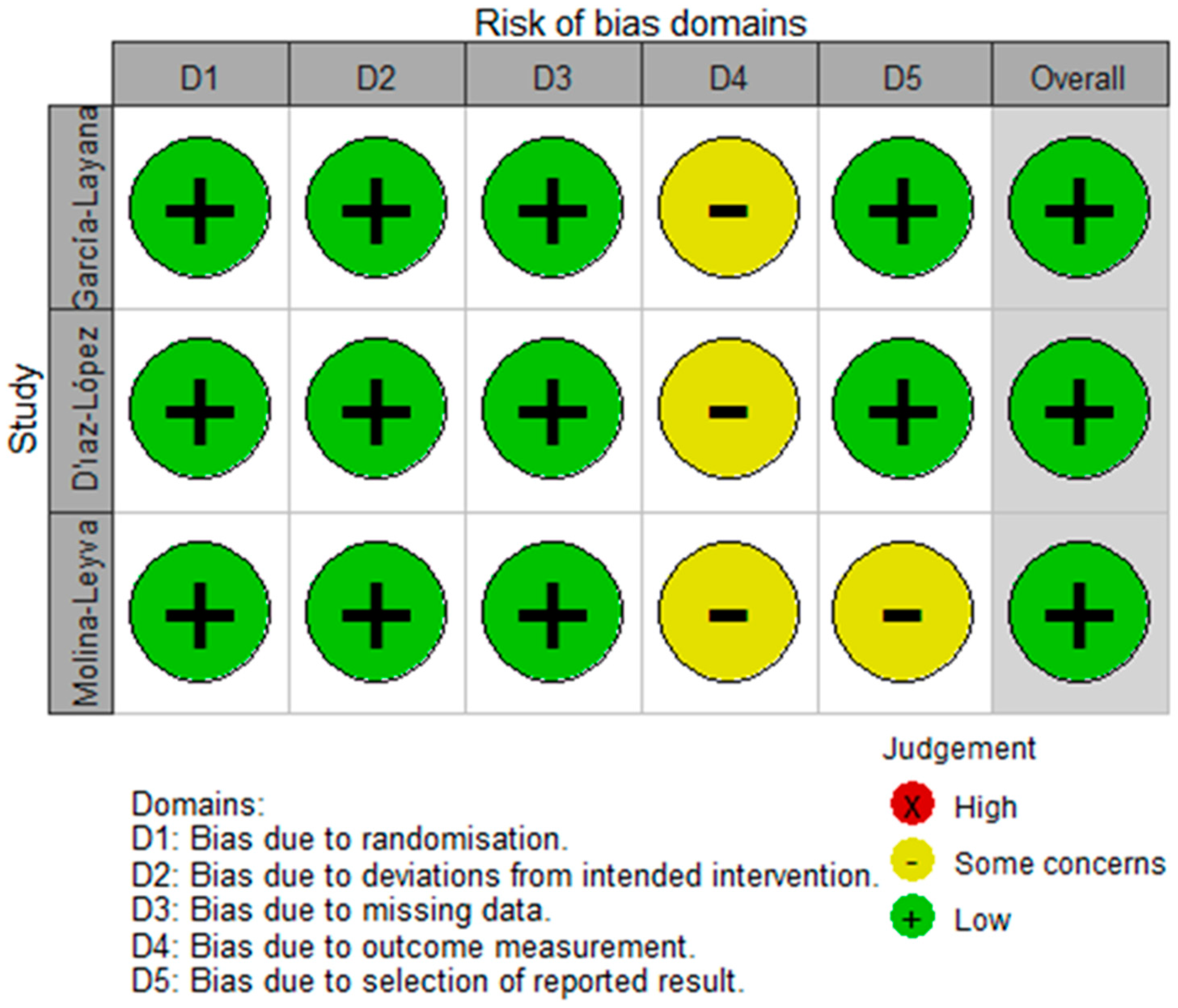
2.5. Study Quality Assessment
3. Results
3.1. Study Selection
3.2. Baseline Characteristics
3.3. Assessment Method of MD Adherence
3.4. Diagnosis and Grading Method of ARED
3.5. MD and AMD
3.6. MD and DES
3.7. MD and Other AREDs (Cataract, Glaucoma and DR)
3.8. Quality Control Score
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roska, B.; Sahel, J.A. Restoring vision. Nature 2018, 557, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Trends in prevalence of blindness and distance and near vision impairment over 30 years: An analysis for the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, e130–e143. [CrossRef]
- Voleti, V.B.; Hubschman, J.P. Age-related eye disease. Maturitas 2013, 75, 29–33. [Google Scholar] [CrossRef]
- O’Neil, E.C.; Henderson, M.; Massaro-Giordano, M.; Bunya, V.Y. Advances in dry eye disease treatment. Curr. Opin. Ophthalmol. 2019, 30, 166–178. [Google Scholar] [CrossRef]
- Chew, E.Y. Dietary Intake of Omega-3 Fatty Acids From Fish and Risk of Diabetic Retinopathy. JAMA 2017, 317, 2226–2227. [Google Scholar] [CrossRef]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and Mediterranean Diet: A Review. Nutrients 2019, 11, 2059. [Google Scholar] [CrossRef]
- Petersson, S.D.; Philippou, E. Mediterranean Diet, Cognitive Function, and Dementia: A Systematic Review of the Evidence. Adv. Nutr. 2016, 7, 889–904. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet; a Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef] [PubMed]
- Agrón, E.; Mares, J.; Chew, E.Y.; Keenan, T.D.L. Adherence to a Mediterranean Diet and Geographic Atrophy Enlargement Rate: Age-Related Eye Disease Study 2 Report 29. Ophthalmol. Retin. 2022, 6, 762–770. [Google Scholar] [CrossRef]
- Keenan, T.D.; Agrón, E.; Mares, J.; Clemons, T.E.; van Asten, F.; Swaroop, A.; Chew, E.Y. Adherence to the Mediterranean Diet and Progression to Late Age-Related Macular Degeneration in the Age-Related Eye Disease Studies 1 and 2. Ophthalmology 2020, 127, 1515–1528. [Google Scholar] [CrossRef]
- Merle, B.M.J.; Rosner, B.; Seddon, J.M. Genetic Susceptibility, Diet Quality, and Two-Step Progression in Drusen Size. Investig. Ophthalmol. Vis. Sci. 2020, 61, 17. [Google Scholar] [CrossRef]
- Merle, B.M.J.; Colijn, J.M.; Cougnard-Grégoire, A.; de Koning-Backus, A.P.M.; Delyfer, M.N.; Kiefte-de Jong, J.C.; Meester-Smoor, M.; Féart, C.; Verzijden, T.; Samieri, C.; et al. Mediterranean Diet and Incidence of Advanced Age-Related Macular Degeneration: The EYE-RISK Consortium. Ophthalmology 2019, 126, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Merle, B.M.; Silver, R.E.; Rosner, B.; Seddon, J.M. Adherence to a Mediterranean diet, genetic susceptibility, and progression to advanced macular degeneration: A prospective cohort study. Am. J. Clin. Nutr. 2015, 102, 1196–1206. [Google Scholar] [CrossRef] [PubMed]
- Viau, S.; Maire, M.A.; Pasquis, B.; Grégoire, S.; Acar, N.; Bron, A.M.; Bretillon, L.; Creuzot-Garcher, C.P.; Joffre, C. Efficacy of a 2-month dietary supplementation with polyunsaturated fatty acids in dry eye induced by scopolamine in a rat model. Graefes Arch. Clin. Exp. Ophthalmol. 2009, 247, 1039–1050. [Google Scholar] [CrossRef] [PubMed]
- Ziemanski, J.F.; Wolters, L.R.; Jones-Jordan, L.; Nichols, J.J.; Nichols, K.K. Relation Between Dietary Essential Fatty Acid Intake and Dry Eye Disease and Meibomian Gland Dysfunction in Postmenopausal Women. Am. J. Ophthalmol. 2018, 189, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Eisenhauer, B.; Natoli, S.; Liew, G.; Flood, V.M. Lutein and Zeaxanthin-Food Sources, Bioavailability and Dietary Variety in Age-Related Macular Degeneration Protection. Nutrients 2017, 9, 120. [Google Scholar] [CrossRef]
- Mrowicka, M.; Mrowicki, J.; Kucharska, E.; Majsterek, I. Lutein and Zeaxanthin and Their Roles in Age-Related Macular Degeneration-Neurodegenerative Disease. Nutrients 2022, 14, 827. [Google Scholar] [CrossRef]
- Finicelli, M.; Squillaro, T.; Di Cristo, F.; Di Salle, A.; Melone, M.A.B.; Galderisi, U.; Peluso, G. Metabolic syndrome, Mediterranean diet, and polyphenols: Evidence and perspectives. J. Cell Physiol. 2019, 234, 5807–5826. [Google Scholar] [CrossRef] [PubMed]
- Mares, J.A.; Voland, R.P.; Sondel, S.A.; Millen, A.E.; Larowe, T.; Moeller, S.M.; Klein, M.L.; Blodi, B.A.; Chappell, R.J.; Tinker, L.; et al. Healthy lifestyles related to subsequent prevalence of age-related macular degeneration. Arch. Ophthalmol. 2011, 129, 470–480. [Google Scholar] [CrossRef]
- Hogg, R.E.; Woodside, J.V.; McGrath, A.; Young, I.S.; Vioque, J.L.; Chakravarthy, U.; de Jong, P.T.; Rahu, M.; Seland, J.; Soubrane, G.; et al. Mediterranean Diet Score and Its Association with Age-Related Macular Degeneration: The European Eye Study. Ophthalmology 2017, 124, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef]
- Modesti, P.A.; Reboldi, G.; Cappuccio, F.P.; Agyemang, C.; Remuzzi, G.; Rapi, S.; Perruolo, E.; Parati, G. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0147601. [Google Scholar] [CrossRef]
- Mu, Y.; Zhao, L.; He, H.; Zhao, H.; Li, J. The efficacy of ileostomy after laparoscopic rectal cancer surgery: A meta-analysis. World J. Surg. Oncol. 2021, 19, 318. [Google Scholar] [CrossRef]
- Shu, X.; Mai, Q.Q.; Blatz, M.; Price, R.; Wang, X.D.; Zhao, K. Direct and Indirect Restorations for Endodontically Treated Teeth: A Systematic Review and Meta-analysis, IAAD 2017 Consensus Conference Paper. J. Adhes. Dent. 2018, 20, 183–194. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Nunes, S.; Alves, D.; Barreto, P.; Raimundo, M.; da Luz Cachulo, M.; Farinha, C.; Laíns, I.; Rodrigues, J.; Almeida, C.; Ribeiro, L.; et al. Adherence to a Mediterranean diet and its association with age-related macular degeneration. The Coimbra Eye Study-Report 4. Nutrition 2018, 51–52, 6–12. [Google Scholar] [CrossRef]
- Raimundo, M.; Mira, F.; Cachulo, M.L.; Barreto, P.; Ribeiro, L.; Farinha, C.; Laíns, I.; Nunes, S.; Alves, D.; Figueira, J.; et al. Adherence to a Mediterranean diet, lifestyle and age-related macular degeneration: The Coimbra Eye Study—report 3. Acta Ophthalmol. 2018, 96, e926–e932. [Google Scholar] [CrossRef] [PubMed]
- García-Layana, A.; Ciufo, G.; Toledo, E.; Martínez-González, M.A.; Corella, D.; Fitó, M.; Estruch, R.; Gómez-Gracia, E.; Fiol, M.; Lapetra, J.; et al. The Effect of a Mediterranean Diet on the Incidence of Cataract Surgery. Nutrients 2017, 9, 453. [Google Scholar] [CrossRef] [PubMed]
- Díaz-López, A.; Babio, N.; Martínez-González, M.A.; Corella, D.; Amor, A.J.; Fitó, M.; Estruch, R.; Arós, F.; Gómez-Gracia, E.; Fiol, M.; et al. Mediterranean Diet, Retinopathy, Nephropathy, and Microvascular Diabetes Complications: A Post Hoc Analysis of a Randomized Trial. Diabetes Care 2015, 38, 2134–2141. [Google Scholar] [CrossRef] [PubMed]
- Ghaemi, F.; Firouzabadi, F.D.; Moosaie, F.; Shadnoush, M.; Poopak, A.; Kermanchi, J.; Abhari, S.M.F.; Forouzanfar, R.; Mansournia, M.A.; Khosravi, A.; et al. Effects of a Mediterranean diet on the development of diabetic complications: A longitudinal study from the nationwide diabetes report of the National Program for Prevention and Control of Diabetes (NPPCD 2016-2020). Maturitas 2021, 153, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Carubbi, F.; Alunno, A.; Mai, F.; Mercuri, A.; Centorame, D.; Cipollone, J.; Mariani, F.M.; Rossi, M.; Bartoloni, E.; Grassi, D.; et al. Adherence to the Mediterranean diet and the impact on clinical features in primary Sjögren’s syndrome. Clin. Exp. Rheumatol. 2021, 39 (Suppl. 133), 190–196. [Google Scholar] [CrossRef] [PubMed]
- Galor, A.; Gardener, H.; Pouyeh, B.; Feuer, W.; Florez, H. Effect of a Mediterranean dietary pattern and vitamin D levels on Dry Eye syndrome. Cornea 2014, 33, 437–441. [Google Scholar] [CrossRef]
- MacHowicz, A.; Hall, I.; De Pablo, P.; Rauz, S.; Richards, A.; Higham, J.; Poveda-Gallego, A.; Imamura, F.; Bowman, S.J.; Barone, F.; et al. Mediterranean diet and risk of Sjögren’s syndrome. Clin. Exp. Rheumatol. 2021, 38, S216–S221. [Google Scholar]
- Molina-Leyva, I.; Molina-Leyva, A.; Riquelme-Gallego, B.; Cano-Ibáñez, N.; García-Molina, L.; Bueno-Cavanillas, A. Effectiveness of Mediterranean Diet Implementation in Dry Eye Parameters: A Study of PREDIMED-PLUS Trial. Nutrients 2020, 12, 1289. [Google Scholar] [CrossRef]
- Moreno-Montañés, J.; Gándara, E.; Gutierrez-Ruiz, I.; Moreno-Galarraga, L.; Ruiz-Canela, M.; Bes-Rastrollo, M.; Martínez-González, M.; Fernandez-Montero, A. Healthy Lifestyle Score and Incidence of Glaucoma: The Sun Project. Nutrients 2022, 14, 779. [Google Scholar] [CrossRef]
- Vergroesen, J.E.; de Crom, T.O.E.; van Duijn, C.M.; Voortman, T.; Klaver, C.C.W.; Ramdas, W.D. MIND diet lowers risk of open-angle glaucoma: The Rotterdam Study. Eur. J. Nutr. 2023, 62, 477–487. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Fernández-Jarne, E.; Serrano-Martínez, M.; Wright, M.; Gomez-Gracia, E. Development of a short dietary intake questionnaire for the quantitative estimation of adherence to a cardioprotective Mediterranean diet. Eur. J. Clin. Nutr. 2004, 58, 1550–1552. [Google Scholar] [CrossRef]
- Ikram, M.A.; Brusselle, G.; Ghanbari, M.; Goedegebure, A.; Ikram, M.K.; Kavousi, M.; Kieboom, B.C.T.; Klaver, C.C.W.; de Knegt, R.J.; Luik, A.I.; et al. Objectives, design and main findings until 2020 from the Rotterdam Study. Eur. J. Epidemiol. 2020, 35, 483–517. [Google Scholar] [CrossRef]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Martín-Peláez, S.; Fito, M.; Castaner, O. Mediterranean Diet Effects on Type 2 Diabetes Prevention, Disease Progression, and Related Mechanisms. A Review. Nutrients 2020, 12, 2236. [Google Scholar] [CrossRef]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Gastaldello, A.; Giampieri, F.; Quiles, J.L.; Navarro-Hortal, M.D.; Aparicio, S.; García Villena, E.; Tutusaus Pifarre, K.; De Giuseppe, R.; Grosso, G.; Cianciosi, D.; et al. Adherence to the Mediterranean-Style Eating Pattern and Macular Degeneration: A Systematic Review of Observational Studies. Nutrients 2022, 14, 2028. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Cho, E.; Willett, W.C.; Sastry, S.M.; Schaumberg, D.A. Intakes of Lutein, Zeaxanthin, and Other Carotenoids and Age-Related Macular Degeneration During 2 Decades of Prospective Follow-up. JAMA Ophthalmol. 2015, 133, 1415–1424. [Google Scholar] [CrossRef] [PubMed]
- D’Innocenzo, S.; Biagi, C.; Lanari, M. Obesity and the Mediterranean Diet: A Review of Evidence of the Role and Sustainability of the Mediterranean Diet. Nutrients 2019, 11, 1306. [Google Scholar] [CrossRef] [PubMed]
- Esfahani, A.; Wong, J.M.; Truan, J.; Villa, C.R.; Mirrahimi, A.; Srichaikul, K.; Kendall, C.W. Health effects of mixed fruit and vegetable concentrates: A systematic review of the clinical interventions. J. Am. Coll. Nutr. 2011, 30, 285–294. [Google Scholar] [CrossRef]
- Xiao, Y.; Zhang, Q.; Liao, X.; Elbelt, U.; Weylandt, K.H. The effects of omega-3 fatty acids in type 2 diabetes: A systematic review and meta-analysis. Prostaglandins Leukot Essent Fat. Acids 2022, 182, 102456. [Google Scholar] [CrossRef]
- Marushka, L.; Batal, M.; David, W.; Schwartz, H.; Ing, A.; Fediuk, K.; Sharp, D.; Black, A.; Tikhonov, C.; Chan, H.M. Association between fish consumption, dietary omega-3 fatty acids and persistent organic pollutants intake, and type 2 diabetes in 18 First Nations in Ontario, Canada. Environ. Res. 2017, 156, 725–737. [Google Scholar] [CrossRef]
- Yanai, R.; Mulki, L.; Hasegawa, E.; Takeuchi, K.; Sweigard, H.; Suzuki, J.; Gaissert, P.; Vavvas, D.G.; Sonoda, K.H.; Rothe, M.; et al. Cytochrome P450-generated metabolites derived from ω-3 fatty acids attenuate neovascularization. Proc. Natl. Acad. Sci. USA 2014, 111, 9603–9608. [Google Scholar] [CrossRef]
- You, Y.S.; Qu, N.B.; Yu, X.N. Alcohol consumption and dry eye syndrome: A Meta-analysis. Int. J. Ophthalmol. 2016, 9, 1487–1492. [Google Scholar] [CrossRef] [PubMed]
- Saccà, S.C.; Cutolo, C.A.; Ferrari, D.; Corazza, P.; Traverso, C.E. The Eye, Oxidative Damage and Polyunsaturated Fatty Acids. Nutrients 2018, 10, 668. [Google Scholar] [CrossRef] [PubMed]
- Anastasopoulos, E.; Founti, P.; Topouzis, F. Update on pseudoexfoliation syndrome pathogenesis and associations with intraocular pressure, glaucoma and systemic diseases. Curr. Opin. Ophthalmol. 2015, 26, 82–89. [Google Scholar] [CrossRef] [PubMed]

| Disease | Author (Year) | Country | Size (Male) | Age (Years) | Study Design | Follow-Up (Years) | Outcome of Interest | Case Definition | Measurement Indexes | Risk Factor | Summary of Main Findings (Including Secondary Outcomes) | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AMD | Mares (2011) [20] | USA | 1313 (0) | 55–74 | Cross- sectional | - | Presence | stereoscopic fundus photographs | Wisconsin AMD Grading System | aMED (quartered) | Early AMD (OR = 0.34 [0.08–0.89], p = 0.046) | 8 |
| AMD | Merle (2015) [14] | USA | 2525 (1124) | 55–80 | Prospective | 8.7 | Progression | retinal stereoscopic images | CARMS | aMED (trichotomous) | Advanced AMD (HR = 0.74 [0.61–0.91], p = 0.007) | 9 |
| AMD | Nunes (2018) [28] | Portugal | 1992 (879) | >55 | Case-control | - | Presence | digital mydriatic color fundus photograph | International Classification and Grading System | mediSCORE (dichotomous) | AMD (OR = 0.73 [0.58–0.93], p = 0.009) | 6 |
| AMD | Raimundo (2018) [29] | Portugal | 883 (385) | >55 | Case-control | - | Presence | digital mydriatic color fundus photograph | International Classification and Grading System | mediSCORE (dichotomous) | AMD (OR = 0.62 [0.38–0.97], p = 0.04) | 7 |
| AMD | Hogg (2017) [21] | Several European countries | 2262 (1028) | >65 | Cross- sectional | - | Presence | stereoscopic digitized color fundus images | International classification and grading system | MDS from Martinez-Gonzalez et al. (2004) [39] (quartered) | Neovascular AMD (OR = 0.53 [0.27–1.04], p = 0.01); large drusen (OR = 0.80 [0.65–0.68], p = 0.01); early AMD and atrophic AMD (negative) | 7 |
| AMD | Merle (2019) [13] | France & Neverland | 4996 (2022) | RS-Ⅰ > 55 Alienor > 73 | Prospective | RS-Ⅰ (9.9) Alienor (4.1) | Progression | fundus photographs | Modification of the Wisconsin Age-Related System and International Classification | mediSCORE (trichotomous) | Advanced AMD (HR = 0.53 [0.33–0.84], p = 0.009); atrophic AMD (HR = 0.42 [0.20–0.90], p = 0.04); neovascular AMD (negative) | 6 |
| AMD | Merle (2020) [12] | USA | 1838 (1328) | 55–80 | Prospective | 10.2 | Progression | Retinal stereoscopic color photographs | Drusen size grade | aMED (dichotomous) | Drusen progression (HR = 0.83 [0.68–0.99], p = 0.049); | 9 |
| AMD | Keenan (2020) [11] | USA | 7756 (4385) | 55–80 | Retrospective | 10.2 | Progression | Color fundus photographs | Wisconsin AMD Grading System | Modified aMED (trichotomous) | Late AMD (HR = 0.78 [0.71–0.85], p < 0.0001); geographic atrophy (HR = 0.71 [0.63–0.80], p < 0.0001); neovascular AMD (HR = 0.84 [0.75–0.95], p = 0.005); large drusen (HR = 0.79 [0.68–0.93], p = 0.04) | 8 |
| AMD | Agrón (2022) [10] | USA | 4203 | 50–85 | Retrospective | 3.1 | Progression | Digital stereoscopic color fundus photographs | Square root of geographic atrophy area | Modified aMED (trichotomous) | Geographic atrophy enlargement (p = 0.008, T3; 0.256 mm/year [0.236–0.276], T2: 0.290 mm/year [0.268–0.311], T1: 0.298 mm/year [0.280–0.317]) | 7 |
| DES | Galor (2014) [34] | USA | 258 (258) | >50 | Cross-sectional | - | Presence | - | DES severity score | mediSCORE (continuous) | DES (OR, 1.25 [1.06–1.47], p = 0.007) and increased disease severity of DES (p = 0.03) | 5 |
| DES | Leyva (2020) [36] | Spain | 34 (13) | M (55–75) F (60–75) | RCT | - | Dry eye parameters and symptoms | External eye examination | Dry Eye Scoring System; Ocular Surface Disease Index | MD intervention | Relieved dry eye symptoms in DESS test score, −0.35 ± 0.15 (p = 0.025) and OSDI, −1.75 ± 0.9 (p = 0.039) | * |
| DES | Carubbi (2021) [33] | Italia | 93 (5) | 61.8 (mean) | Cross-sectional | - | - | - | ESSDAI and ESSPRI | PREDIMED, MEDLIFE (continuous) | Decreased disease activity measured by ESSDAI (Spearman’s rho = −0.27, p = 0.009) and ClinESSDAI (Spearman’s rho = −0.26, p = 0.01) | 4 |
| DES | Machowicz (2020) [35] | UK | 133 (9) | >18 | Case-control | - | Presence | - | EULAR and ESSDAI | Modified mediSCORE (continuous) | pSS (OR = 0.81 [0.66–0.99], p = 0.038) | 6 |
| Cataract | Layana (2017) [30] | Spain | 5802 (2598) | M (55–80); F (60–80) | RCT | 5.7 | Incidence | Surgery medical records | - | MD intervention (vs. low-fat diet) | Cataract surgery (negative) | * |
| Glaucoma | Montañés (2022) [37] | Spain | 18,420 (7332) | 37.7 (mean) | Prospective | 12 | Incidence | Self-reported diagnosis by ophthalmologist | - | Modified mediSCORE excluding alcohol; SHLS (quartered) | Glaucoma of MD only (negative) and glaucoma of SHLS (HR = 0.51 [0.28–0.93]) | 8 |
| Glaucoma | Vergroesen (2023) [38] | Neverland | 1020 (468) | >45 | Case-control | 5 | Presence | Eye examination | - | MDS from Ikram et al. 2020 (continuous) [40]; MIND diet | OAG of MD (nagative) and OAG of MIND (OR = 0.80 [0.66–0.96], p = 0.02) | 6 |
| DR | D’ıaz-López (2015) [31] | Spain | 3614 (1707) | M(55–80); F(60–80) | RCT | 6.0 | Incidence | Nonmydriatic fundus camera | - | MD intervention (vs. low-fat diet), Biomarkers (urine hydroxytyrosol, a-linolenic acid) (quintiled) | DR for the MedDiet + EVOO (HR = 0.56 [0.32–0.97]) and the MedDiet + nuts (negative); DR for adherence to MD measured by biomarkers (HR, 0.34 [0.13–0.89]; p = 0.001) | * |
| DR | Ghaemi (2021) [32] | Iran | 22,187 (6705) | T1D (50.7) T2D (59.9) (mean) | Prospective | 2–11 | Incidence | - | International Classification of Diseases | MDS from Schroder et al. 2011 [41] (dichotomous) | DR in T1DM (OR = 0.32 [0.24–0.44], p < 0.001) and DR in T2DM (OR = 0.68 [0.61–0.71], p < 0.001) | 8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Y.; Xie, Y.; Yuan, Y.; Xiong, R.; Hu, Y.; Ning, K.; Ha, J.; Wang, W.; Han, X.; He, M. The Mediterranean Diet and Age-Related Eye Diseases: A Systematic Review. Nutrients 2023, 15, 2043. https://doi.org/10.3390/nu15092043
Wu Y, Xie Y, Yuan Y, Xiong R, Hu Y, Ning K, Ha J, Wang W, Han X, He M. The Mediterranean Diet and Age-Related Eye Diseases: A Systematic Review. Nutrients. 2023; 15(9):2043. https://doi.org/10.3390/nu15092043
Chicago/Turabian StyleWu, Yi, Ye Xie, Yixiong Yuan, Ruilin Xiong, Yuxin Hu, Kang Ning, Jason Ha, Wei Wang, Xiaotong Han, and Mingguang He. 2023. "The Mediterranean Diet and Age-Related Eye Diseases: A Systematic Review" Nutrients 15, no. 9: 2043. https://doi.org/10.3390/nu15092043
APA StyleWu, Y., Xie, Y., Yuan, Y., Xiong, R., Hu, Y., Ning, K., Ha, J., Wang, W., Han, X., & He, M. (2023). The Mediterranean Diet and Age-Related Eye Diseases: A Systematic Review. Nutrients, 15(9), 2043. https://doi.org/10.3390/nu15092043






