Short-Term L-Citrulline Supplementation Does Not Affect Inspiratory Muscle Oxygenation and Respiratory Performance in Older Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
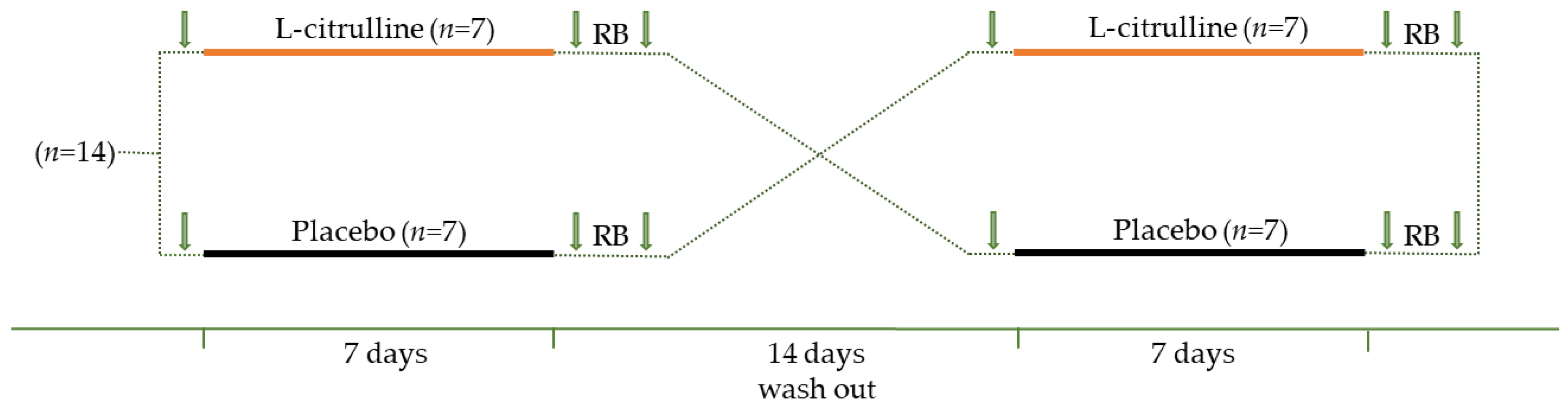
2.2. Study Design
2.3. Maximal Inspiratory Pressure and Perceived Exertion
2.4. Pulmonary Function
2.5. Fractional Exhaled NO•
2.6. Near-Infrared Spectroscopy Measurement
2.7. Statistical Analysis
3. Results
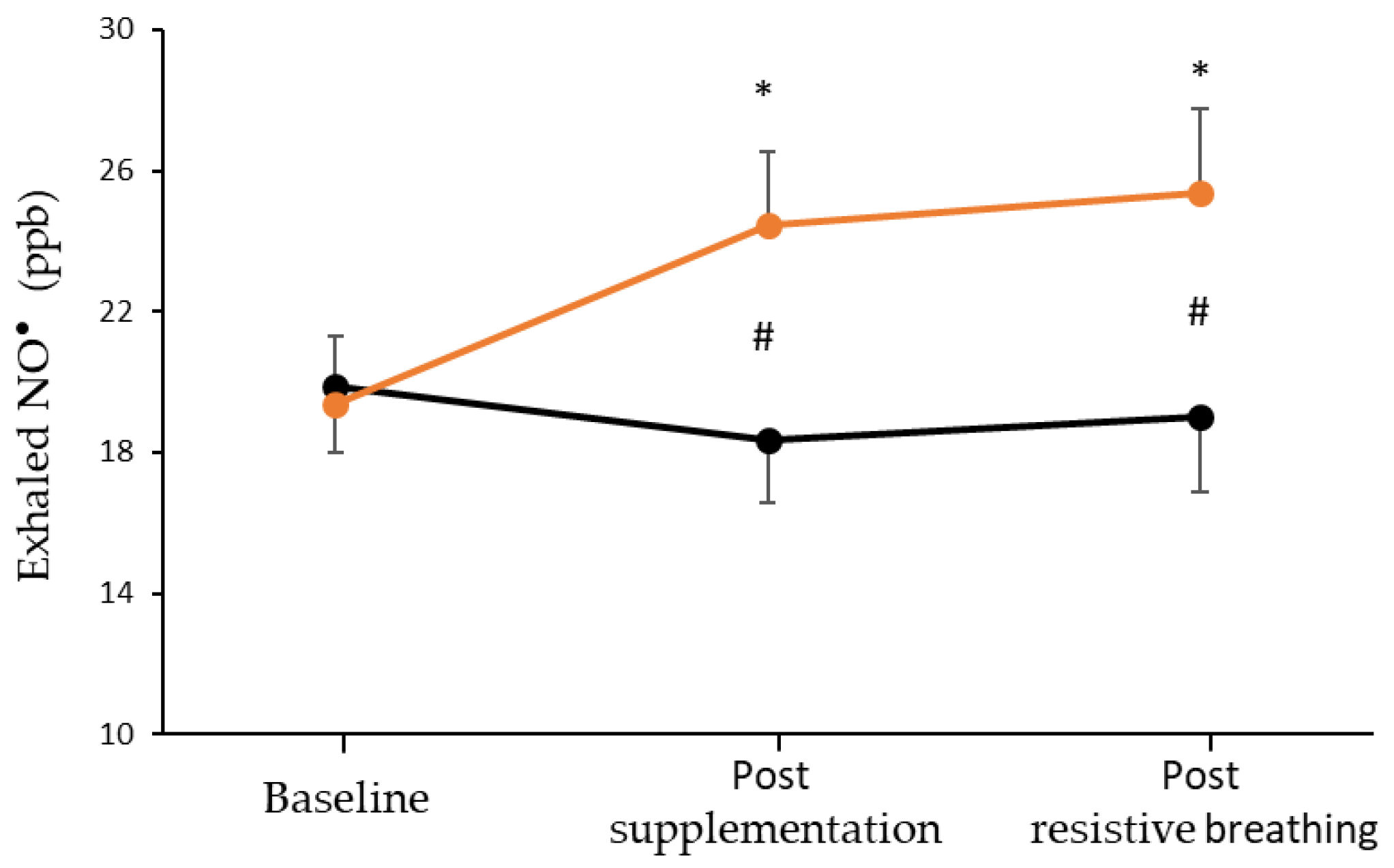
3.1. Fractional Exhaled NO•
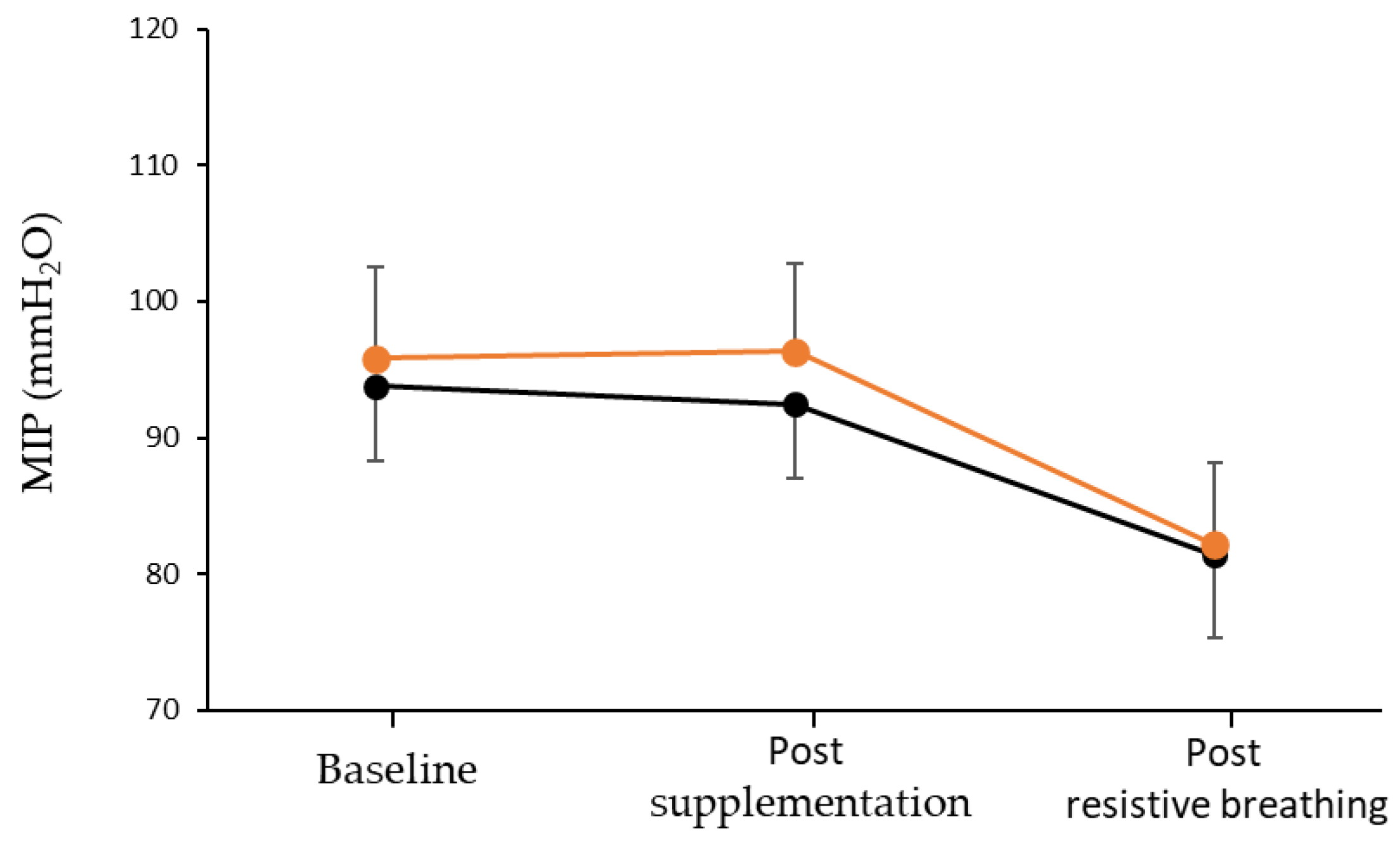
3.2. Inspiratory Muscles Performance, Perceived Exertion, and Fatigue
3.3. Respiratory Muscles Capacity and Sternocleidomastoid Muscle Oxygenation
4. Discussion
4.1. L-Citrulline Supplementation and NO• Bioavailability
4.2. Inspiratory Muscle Performance and Resistance to Fatigue
4.3. Sternocleidomastoid Muscle Oxygenation and Blood Flow
4.4. NO• Precursors and Vascular Function
4.5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ghimire, K.; Altmann, H.M.; Straub, A.C.; Isenberg, J.S. Nitric oxide: What’s new to NO? Am. J. Physiol. Cell. Physiol. 2017, 312, C254–C262. [Google Scholar] [CrossRef] [PubMed]
- Margaritelis, N.V.; Paschalis, V.; Theodorou, A.A.; Kyparos, A.; Nikolaidis, M.G. Redox basis of exercise physiology. Redox Biol. 2020, 35, 101499. [Google Scholar] [CrossRef] [PubMed]
- Stamler, J.S.; Meissner, G. Physiology of nitric oxide in skeletal muscle. Physiol. Rev. 2001, 81, 209–237. [Google Scholar] [CrossRef]
- Bailey, S.J.; Jones, A.M. Nitric Oxide Biochemistry and Exercise Performance in Humans. Influence of Nitrate Supplementation. In Oxidative Eustress in Exercise Physiology; Gobley, J.N., Davison, G.W., Eds.; CRC Press: Boca Raton, FL, USA, 2022. [Google Scholar]
- Jones, A.M.; Vanhatalo, A.; Seals, D.R.; Rossman, M.J.; Piknova, B.; Jonvik, K.L. Dietary Nitrate and Nitric Oxide Metabolism: Mouth, Circulation, Skeletal Muscle, and Exercise Performance. Med. Sci. Sports Exerc. 2021, 53, 280–294. [Google Scholar] [CrossRef]
- Reid, M.B.; Kobzik, L.; Bredt, D.S.; Stamler, J.S. Nitric oxide modulates excitation-contraction coupling in the diaphragm. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 1998, 119, 211–218. [Google Scholar] [CrossRef]
- Hellsten, Y.; Nyberg, M.; Jensen, L.G.; Mortensen, S.P. Vasodilator interactions in skeletal muscle blood flow regulation. J. Physiol. 2012, 590, 6297–6305. [Google Scholar] [CrossRef]
- Hirai, D.M.; Copp, S.W.; Ferguson, S.K.; Holdsworth, C.T.; McCullough, D.J.; Behnke, B.J.; Musch, T.I.; Poole, D.C. Exercise training and muscle microvascular oxygenation: Functional role of nitric oxide. J. Appl. Physiol. 2012, 113, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Chatzinikolaou, P.N.; Margaritelis, N.V.; Chatzinikolaou, A.N.; Paschalis, V.; Theodorou, A.A.; Vrabas, I.S.; Kyparos, A.; Nikolaidis, M.G. Oxygen Transport. A Redox O2dyssey. In Oxidative Eustress in Exercise Physiology; Cobley, J.N., Davison, G.W., Eds.; CRC Press: Boca Raton, FL, USA, 2022. [Google Scholar]
- Brown, G.C. Regulation of mitochondrial respiration by nitric oxide inhibition of cytochrome c oxidase. Biochim. Biophys. Acta 2001, 1504, 46–57. [Google Scholar] [CrossRef]
- Poderoso, J.J.; Helfenberger, K.; Poderoso, C. The effect of nitric oxide on mitochondrial respiration. Nitric. Oxide 2019, 88, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Spencer, T.; Posterino, G.S. Sequential effects of GSNO and H2O2 on the Ca2+ sensitivity of the contractile apparatus of fast- and slow-twitch skeletal muscle fibers from the rat. Am. J. Physiol. Cell. Physiol. 2009, 296, C1015–C1023. [Google Scholar] [CrossRef]
- Blottner, D.; Luck, G. Nitric oxide synthase (NOS) in mouse skeletal muscle development and differentiated myoblasts. Cell. Tissue Res. 1998, 292, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Sibisi, N.C.; Snyman, C.; Myburgh, K.H.; Niesler, C.U. Evaluating the role of nitric oxide in myogenesis in vitro. Biochimie 2022, 196, 216–224. [Google Scholar] [CrossRef]
- Papanikolaou, K.; Veskoukis, A.S.; Draganidis, D.; Baloyiannis, I.; Deli, C.K.; Poulios, A.; Jamurtas, A.Z.; Fatouros, I.G. Redox-dependent regulation of satellite cells following aseptic muscle trauma: Implications for sports performance and nutrition. Free Radic. Biol. Med. 2020, 161, 125–138. [Google Scholar] [CrossRef]
- Hong, Y.H.; Betik, A.C.; McConell, G.K. Role of nitric oxide in skeletal muscle glucose uptake during exercise. Exp. Physiol. 2014, 99, 1569–1573. [Google Scholar] [CrossRef]
- McConell, G.K.; Kingwell, B.A. Does nitric oxide regulate skeletal muscle glucose uptake during exercise? Exerc. Sport. Sci. Rev. 2006, 34, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Kerksick, C.M.; Wilborn, C.D.; Roberts, M.D.; Smith-Ryan, A.; Kleiner, S.M.; Jager, R.; Collins, R.; Cooke, M.; Davis, J.N.; Galvan, E.; et al. ISSN exercise & sports nutrition review update: Research & recommendations. J. Int. Soc. Sports Nutr. 2018, 15, 38. [Google Scholar] [CrossRef]
- Gonzalez, A.M.; Townsend, J.R.; Pinzone, A.G.; Hoffman, J.R. Supplementation with Nitric Oxide Precursors for Strength Performance: A Review of the Current Literature. Nutrients 2023, 15, 660. [Google Scholar] [CrossRef]
- Bescos, R.; Sureda, A.; Tur, J.A.; Pons, A. The effect of nitric-oxide-related supplements on human performance. Sports Med. 2012, 42, 99–117. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, A.M.; Trexler, E.T. Effects of Citrulline Supplementation on Exercise Performance in Humans: A Review of the Current Literature. J. Strength. Cond. Res. 2020, 34, 1480–1495. [Google Scholar] [CrossRef]
- Sureda, A.; Pons, A. Arginine and citrulline supplementation in sports and exercise: Ergogenic nutrients? Med. Sport. Sci. 2012, 59, 18–28. [Google Scholar] [CrossRef]
- Viribay, A.; Fernandez-Landa, J.; Castaneda-Babarro, A.; Collado, P.S.; Fernandez-Lazaro, D.; Mielgo-Ayuso, J. Effects of Citrulline Supplementation on Different Aerobic Exercise Performance Outcomes: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 3479. [Google Scholar] [CrossRef] [PubMed]
- Ashley, J.; Kim, Y.; Gonzales, J.U. Impact of l-citrulline supplementation on oxygen uptake kinetics during walking. Appl. Physiol. Nutr. Metab. 2018, 43, 631–637. [Google Scholar] [CrossRef]
- Bailey, S.J.; Blackwell, J.R.; Lord, T.; Vanhatalo, A.; Winyard, P.G.; Jones, A.M. l-Citrulline supplementation improves O2 uptake kinetics and high-intensity exercise performance in humans. J. Appl. Physiol. 2015, 119, 385–395. [Google Scholar] [CrossRef]
- Buckinx, F.; Carvalho, L.P.; Marcangeli, V.; Dulac, M.; Gouspillou, G.; Gaudreau, P.; Noirez, P.; Aubertin-Leheudre, M. High intensity interval training combined with L-citrulline supplementation: Effects on physical performance in healthy older adults. Exp. Gerontol. 2020, 140, 111036. [Google Scholar]
- Gonzales, J.U.; Raymond, A.; Ashley, J.; Kim, Y. Does l-citrulline supplementation improve exercise blood flow in older adults? Exp. Physiol. 2017, 102, 1661–1671. [Google Scholar] [CrossRef]
- Martinez-Sanchez, A.; Ramos-Campo, D.J.; Fernandez-Lobato, B.; Rubio-Arias, J.A.; Alacid, F.; Aguayo, E. Biochemical, physiological, and performance response of a functional watermelon juice enriched in L-citrulline during a half-marathon race. Food Nutr. Res. 2017, 61, 1330098. [Google Scholar] [CrossRef]
- Stanelle, S.T.; McLaughlin, K.L.; Crouse, S.F. One Week of L-Citrulline Supplementation Improves Performance in Trained Cyclists. J. Strength. Cond. Res. 2020, 34, 647–652. [Google Scholar] [CrossRef]
- Suzuki, T.; Morita, M.; Kobayashi, Y.; Kamimura, A. Oral L-citrulline supplementation enhances cycling time trial performance in healthy trained men: Double-blind randomized placebo-controlled 2-way crossover study. J. Int. Soc. Sports Nutr. 2016, 13, 6. [Google Scholar] [CrossRef]
- Curis, E.; Nicolis, I.; Moinard, C.; Osowska, S.; Zerrouk, N.; Benazeth, S.; Cynober, L. Almost all about citrulline in mammals. Amino Acids 2005, 29, 177–205. [Google Scholar] [CrossRef] [PubMed]
- van de Poll, M.C.; Siroen, M.P.; van Leeuwen, P.A.; Soeters, P.B.; Melis, G.C.; Boelens, P.G.; Deutz, N.E.; Dejong, C.H. Interorgan amino acid exchange in humans: Consequences for arginine and citrulline metabolism. Am. J. Clin. Nutr. 2007, 85, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Schwedhelm, E.; Maas, R.; Freese, R.; Jung, D.; Lukacs, Z.; Jambrecina, A.; Spickler, W.; Schulze, F.; Boger, R.H. Pharmacokinetic and pharmacodynamic properties of oral L-citrulline and L-arginine: Impact on nitric oxide metabolism. Br. J. Clin. Pharmacol. 2008, 65, 51–59. [Google Scholar] [CrossRef]
- Moinard, C.; Maccario, J.; Walrand, S.; Lasserre, V.; Marc, J.; Boirie, Y.; Cynober, L. Arginine behaviour after arginine or citrulline administration in older subjects. Br. J. Nutr. 2016, 115, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Aguayo, E.; Martínez-Sánchez, A.; Fernández-Lobato, B.; Alacid, F. L-Citrulline: A Non-Essential Amino Acid with Important Roles in Human Health. Appl. Sci. 2021, 11, 3293. [Google Scholar] [CrossRef]
- Allerton, T.D.; Proctor, D.N.; Stephens, J.M.; Dugas, T.R.; Spielmann, G.; Irving, B.A. l-Citrulline Supplementation: Impact on Cardiometabolic Health. Nutrients 2018, 10, 921. [Google Scholar] [CrossRef]
- Windmueller, H.G.; Spaeth, A.E. Source and fate of circulating citrulline. Am. J. Physiol. 1981, 241, E473–E480. [Google Scholar] [CrossRef]
- Marini, J.C.; Agarwal, U.; Didelija, I.C.; Azamian, M.; Stoll, B.; Nagamani, S.C. Plasma Glutamine Is a Minor Precursor for the Synthesis of Citrulline: A Multispecies Study. J. Nutr. 2017, 147, 549–555. [Google Scholar] [CrossRef]
- Rimando, A.M.; Perkins-Veazie, P.M. Determination of citrulline in watermelon rind. J. Chromatogr. A 2005, 1078, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Tarazona-Diaz, M.P.; Viegas, J.; Moldao-Martins, M.; Aguayo, E. Bioactive compounds from flesh and by-product of fresh-cut watermelon cultivars. J. Sci. Food Agric. 2011, 91, 805–812. [Google Scholar] [CrossRef]
- Lundberg, J.O.; Weitzberg, E. Nitric oxide signaling in health and disease. Cell 2022, 185, 2853–2878. [Google Scholar] [CrossRef] [PubMed]
- Dinenno, F.A.; Jones, P.P.; Seals, D.R.; Tanaka, H. Limb blood flow and vascular conductance are reduced with age in healthy humans: Relation to elevations in sympathetic nerve activity and declines in oxygen demand. Circulation 1999, 100, 164–170. [Google Scholar] [CrossRef]
- Lauer, T.; Heiss, C.; Balzer, J.; Kehmeier, E.; Mangold, S.; Leyendecker, T.; Rottler, J.; Meyer, C.; Merx, M.W.; Kelm, M.; et al. Age-dependent endothelial dysfunction is associated with failure to increase plasma nitrite in response to exercise. Basic. Res. Cardiol. 2008, 103, 291–297. [Google Scholar] [CrossRef]
- Lawrenson, L.; Poole, J.G.; Kim, J.; Brown, C.; Patel, P.; Richardson, R.S. Vascular and metabolic response to isolated small muscle mass exercise: Effect of age. Am. J. Physiol. Heart Circ. Physiol. 2003, 285, H1023–H1031. [Google Scholar] [CrossRef] [PubMed]
- Poole, J.G.; Lawrenson, L.; Kim, J.; Brown, C.; Richardson, R.S. Vascular and metabolic response to cycle exercise in sedentary humans: Effect of age. Am. J. Physiol. Heart Circ. Physiol. 2003, 284, H1251–H1259. [Google Scholar] [CrossRef]
- Conley, K.E.; Jubrias, S.A.; Esselman, P.C. Oxidative capacity and ageing in human muscle. J. Physiol. 2000, 526 Pt 1, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Freire, M.; Scalzo, P.; D’Agostino, J.; Moore, Z.A.; Diaz-Ruiz, A.; Fabbri, E.; Zane, A.; Chen, B.; Becker, K.G.; Lehrmann, E.; et al. Skeletal muscle ex vivo mitochondrial respiration parallels decline in vivo oxidative capacity, cardiorespiratory fitness, and muscle strength: The Baltimore Longitudinal Study of Aging. Aging Cell. 2018, 17, e12725. [Google Scholar] [CrossRef]
- Astrand, I.; Astrand, P.O.; Hallback, I.; Kilbom, A. Reduction in maximal oxygen uptake with age. J. Appl. Physiol. 1973, 35, 649–654. [Google Scholar] [CrossRef]
- Janssen, I.; Heymsfield, S.B.; Wang, Z.M.; Ross, R. Skeletal muscle mass and distribution in 468 men and women aged 18-88 yr. J. Appl. Physiol. 2000, 89, 81–88. [Google Scholar] [CrossRef]
- Rowell, L.B. Ideas about control of skeletal and cardiac muscle blood flow (1876–2003): Cycles of revision and new vision. J. Appl. Physiol. 2004, 97, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Saltin, B. Exercise hyperaemia: Magnitude and aspects on regulation in humans. J. Physiol. 2007, 583, 819–823. [Google Scholar] [CrossRef]
- Dominelli, P.B.; Archiza, B.; Ramsook, A.H.; Mitchell, R.A.; Peters, C.M.; Molgat-Seon, Y.; Henderson, W.R.; Koehle, M.S.; Boushel, R.; Sheel, A.W. Effects of respiratory muscle work on respiratory and locomotor blood flow during exercise. Exp. Physiol. 2017, 102, 1535–1547. [Google Scholar] [CrossRef]
- Romer, L.M.; Lovering, A.T.; Haverkamp, H.C.; Pegelow, D.F.; Dempsey, J.A. Effect of inspiratory muscle work on peripheral fatigue of locomotor muscles in healthy humans. J. Physiol. 2006, 571, 425–439. [Google Scholar] [CrossRef]
- Theodorou, A.A.; Zinelis, P.T.; Malliou, V.J.; Chatzinikolaou, P.N.; Margaritelis, N.V.; Mandalidis, D.; Geladas, N.D.; Paschalis, V. Acute L-Citrulline Supplementation Increases Nitric Oxide Bioavailability but Not Inspiratory Muscle Oxygenation and Respiratory Performance. Nutrients 2021, 13, 3311. [Google Scholar] [CrossRef]
- Hudson, A.L.; Gandevia, S.C.; Butler, J.E. The effect of lung volume on the co-ordinated recruitment of scalene and sternomastoid muscles in humans. J. Physiol. 2007, 584, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Yokoba, M.; Abe, T.; Katagiri, M.; Tomita, T.; Easton, P.A. Respiratory muscle electromyogram and mouth pressure during isometric contraction. Respir. Physiol. Neurobiol. 2003, 137, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Moinard, C.; Nicolis, I.; Neveux, N.; Darquy, S.; Benazeth, S.; Cynober, L. Dose-ranging effects of citrulline administration on plasma amino acids and hormonal patterns in healthy subjects: The Citrudose pharmacokinetic study. Br. J. Nutr. 2008, 99, 855–862. [Google Scholar] [CrossRef]
- Borg, G. Borg’s Perceived Exertion and Pain Scales; Human Kinetics: Champaign, IL, USA, 1998. [Google Scholar]
- Dolopikou, C.F.; Kourtzidis, I.A.; Margaritelis, N.V.; Vrabas, I.S.; Koidou, I.; Kyparos, A.; Theodorou, A.A.; Paschalis, V.; Nikolaidis, M.G. Acute nicotinamide riboside supplementation improves redox homeostasis and exercise performance in old individuals: A double-blind cross-over study. Eur. J. Nutr. 2020, 59, 505–515. [Google Scholar] [CrossRef]
- Margaritelis, N.V.; Paschalis, V.; Theodorou, A.A.; Kyparos, A.; Nikolaidis, M.G. Antioxidants in Personalized Nutrition and Exercise. Adv. Nutr. 2018, 9, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Wijnands, K.A.; Meesters, D.M.; van Barneveld, K.W.; Visschers, R.G.; Briede, J.J.; Vandendriessche, B.; van Eijk, H.M.; Bessems, B.A.; van den Hoven, N.; von Wintersdorff, C.J.; et al. Citrulline Supplementation Improves Organ Perfusion and Arginine Availability under Conditions with Enhanced Arginase Activity. Nutrients 2015, 7, 5217–5238. [Google Scholar] [CrossRef] [PubMed]
- Kadach, S.; Piknova, B.; Black, M.I.; Park, J.W.; Wylie, L.J.; Stoyanov, Z.; Thomas, S.M.; McMahon, N.F.; Vanhatalo, A.; Schechter, A.N.; et al. Time course of human skeletal muscle nitrate and nitrite concentration changes following dietary nitrate ingestion. Nitric Oxide 2022, 121, 1–10. [Google Scholar] [CrossRef]
- Abu-Alghayth, M.; Vanhatalo, A.; Wylie, L.J.; McDonagh, S.T.; Thompson, C.; Kadach, S.; Kerr, P.; Smallwood, M.J.; Jones, A.M.; Winyard, P.G. S-nitrosothiols, and other products of nitrate metabolism, are increased in multiple human blood compartments following ingestion of beetroot juice. Redox Biol. 2021, 43, 101974. [Google Scholar] [CrossRef]
- Esen, O.; Eser, M.C.; Abdioglu, M.; Benesova, D.; Gabrys, T.; Karayigit, R. Eight Days of L-Citrulline or L-Arginine Supplementation Did Not Improve 200-m and 100-m Swimming Time Trials. Int. J. Environ. Res. Public. Health 2022, 19, 4462. [Google Scholar] [CrossRef]
- Ochiai, M.; Hayashi, T.; Morita, M.; Ina, K.; Maeda, M.; Watanabe, F.; Morishita, K. Short-term effects of L-citrulline supplementation on arterial stiffness in middle-aged men. Int. J. Cardiol. 2012, 155, 257–261. [Google Scholar] [CrossRef]
- Legrand, A.; Schneider, E.; Gevenois, P.A.; De Troyer, A. Respiratory effects of the scalene and sternomastoid muscles in humans. J. Appl. Physiol. 2003, 94, 1467–1472. [Google Scholar] [CrossRef]
- Enoka, R.M.; Duchateau, J. Muscle fatigue: What, why and how it influences muscle function. J. Physiol. 2008, 586, 11–23. [Google Scholar] [CrossRef]
- Wan, J.J.; Qin, Z.; Wang, P.Y.; Sun, Y.; Liu, X. Muscle fatigue: General understanding and treatment. Exp. Mol. Med. 2017, 49, e384. [Google Scholar] [CrossRef] [PubMed]
- Romer, L.M.; Polkey, M.I. Exercise-induced respiratory muscle fatigue: Implications for performance. J. Appl. Physiol. 2008, 104, 879–888. [Google Scholar] [CrossRef] [PubMed]
- Sheel, A.W.; Derchak, P.A.; Morgan, B.J.; Pegelow, D.F.; Jacques, A.J.; Dempsey, J.A. Fatiguing inspiratory muscle work causes reflex reduction in resting leg blood flow in humans. J. Physiol. 2001, 537, 277–289. [Google Scholar] [CrossRef]
- Shadgan, B.; Guenette, J.A.; Sheel, A.W.; Reid, W.D. Sternocleidomastoid muscle deoxygenation in response to incremental inspiratory threshold loading measured by near infrared spectroscopy. Respir. Physiol. Neurobiol. 2011, 178, 202–209. [Google Scholar] [CrossRef]
- Simmonds, M.J.; Detterich, J.A.; Connes, P. Nitric oxide, vasodilation and the red blood cell. Biorheology 2014, 51, 121–134. [Google Scholar] [CrossRef] [PubMed]
- Tejero, J.; Shiva, S.; Gladwin, M.T. Sources of Vascular Nitric Oxide and Reactive Oxygen Species and Their Regulation. Physiol. Rev. 2019, 99, 311–379. [Google Scholar] [CrossRef]
- Park, H.Y.; Kim, S.W.; Seo, J.; Jung, Y.P.; Kim, H.; Kim, A.J.; Kim, S.; Lim, K. Dietary Arginine and Citrulline Supplements for Cardiovascular Health and Athletic Performance: A Narrative Review. Nutrients 2023, 15, 1268. [Google Scholar] [CrossRef]
- Ast, J.; Jablecka, A.; Bogdanski, P.; Smolarek, I.; Krauss, H.; Chmara, E. Evaluation of the antihypertensive effect of L-arginine supplementation in patients with mild hypertension assessed with ambulatory blood pressure monitoring. Med. Sci. Monit. 2010, 16, CR266–CR271. [Google Scholar] [CrossRef]
- Figueroa, A.; Alvarez-Alvarado, S.; Jaime, S.J.; Kalfon, R. l-Citrulline supplementation attenuates blood pressure, wave reflection and arterial stiffness responses to metaboreflex and cold stress in overweight men. Br. J. Nutr. 2016, 116, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, A.; Trivino, J.A.; Sanchez-Gonzalez, M.A.; Vicil, F. Oral L-citrulline supplementation attenuates blood pressure response to cold pressor test in young men. Am. J. Hypertens. 2010, 23, 12–16. [Google Scholar] [CrossRef]
- Lucotti, P.; Monti, L.; Setola, E.; La Canna, G.; Castiglioni, A.; Rossodivita, A.; Pala, M.G.; Formica, F.; Paolini, G.; Catapano, A.L.; et al. Oral L-arginine supplementation improves endothelial function and ameliorates insulin sensitivity and inflammation in cardiopathic nondiabetic patients after an aortocoronary bypass. Metabolism 2009, 58, 1270–1276. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.Y.; Qin, L.Q.; Zhang, Z.; Zhao, Y.; Wang, J.; Arigoni, F.; Zhang, W. Effect of oral L-arginine supplementation on blood pressure: A meta-analysis of randomized, double-blind, placebo-controlled trials. Am. Heart J. 2011, 162, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Smeets, E.; Mensink, R.P.; Joris, P.J. Effects of L-citrulline supplementation and watermelon consumption on longer-term and postprandial vascular function and cardiometabolic risk markers: A meta-analysis of randomized controlled trials in adults. Br. J. Nutr. 2021, 128, 1–34. [Google Scholar] [CrossRef] [PubMed]


| n = 14 | |||
|---|---|---|---|
| Age (yr) | 63.1 | ± | 5.5 |
| Height (cm) | 174 | ± | 3.9 |
| Weight (kg) | 78.8 | ± | 6.8 |
| BMI (kg/m2) | 26.1 | ± | 2.5 |
| Body fat (%) | 26.4 | ± | 2.6 |
| Waist circumference (cm) | 98.4 | ± | 5.5 |
| Hip circumference (cm) | 103.7 | ± | 6.6 |
| Waist-to-hip ratio | 0.95 | ± | 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theodorou, A.A.; Chatzinikolaou, P.N.; Margaritelis, N.V.; Christodoulou, F.; Tsatalas, T.; Paschalis, V. Short-Term L-Citrulline Supplementation Does Not Affect Inspiratory Muscle Oxygenation and Respiratory Performance in Older Adults. Nutrients 2023, 15, 1951. https://doi.org/10.3390/nu15081951
Theodorou AA, Chatzinikolaou PN, Margaritelis NV, Christodoulou F, Tsatalas T, Paschalis V. Short-Term L-Citrulline Supplementation Does Not Affect Inspiratory Muscle Oxygenation and Respiratory Performance in Older Adults. Nutrients. 2023; 15(8):1951. https://doi.org/10.3390/nu15081951
Chicago/Turabian StyleTheodorou, Anastasios A., Panagiotis N. Chatzinikolaou, Nikos V. Margaritelis, Filippos Christodoulou, Themistoklis Tsatalas, and Vassilis Paschalis. 2023. "Short-Term L-Citrulline Supplementation Does Not Affect Inspiratory Muscle Oxygenation and Respiratory Performance in Older Adults" Nutrients 15, no. 8: 1951. https://doi.org/10.3390/nu15081951
APA StyleTheodorou, A. A., Chatzinikolaou, P. N., Margaritelis, N. V., Christodoulou, F., Tsatalas, T., & Paschalis, V. (2023). Short-Term L-Citrulline Supplementation Does Not Affect Inspiratory Muscle Oxygenation and Respiratory Performance in Older Adults. Nutrients, 15(8), 1951. https://doi.org/10.3390/nu15081951









