Impact of the COVID-19 Pandemic on Nutrition, Sleep, Physical Activity, and Mood Disorders of Polish Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Inclusion Criteria
- The age of the child in the range of 6–14 years
- A child attending grades 1–8 of elementary school
- Written consent of the parent expressed through participation in the study.
- Participation in the study was anonymous and entirely voluntary.
2.3. Research Tool
2.4. Statistical Analysis
3. Results
3.1. Socio-Demographic Information
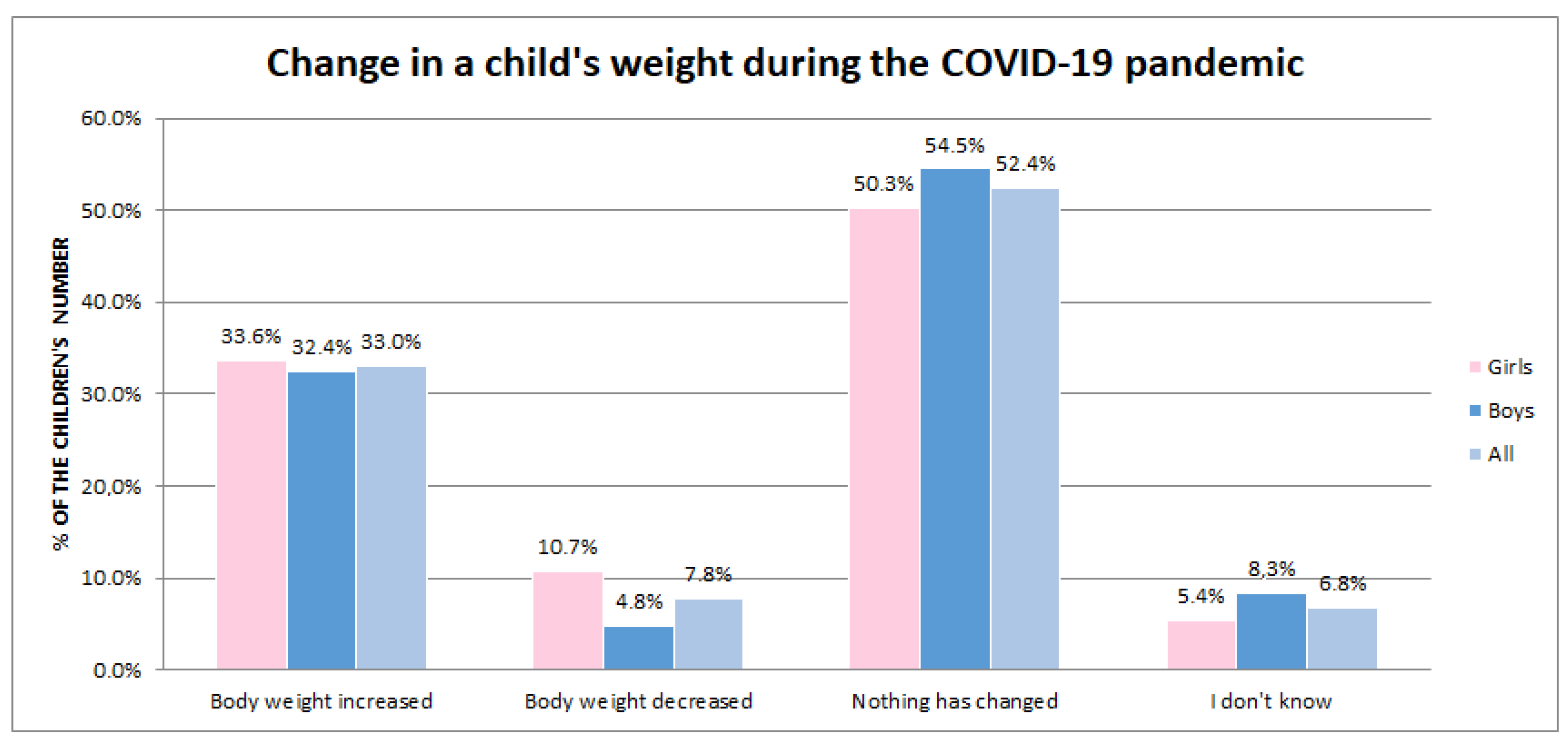
3.2. BMI and Weight Changes in Children during the COVID-19 Pandemic
3.3. Comparisons of Children’s Dietary and Lifestyle Behaviors before and during the COVID-19 Pandemic
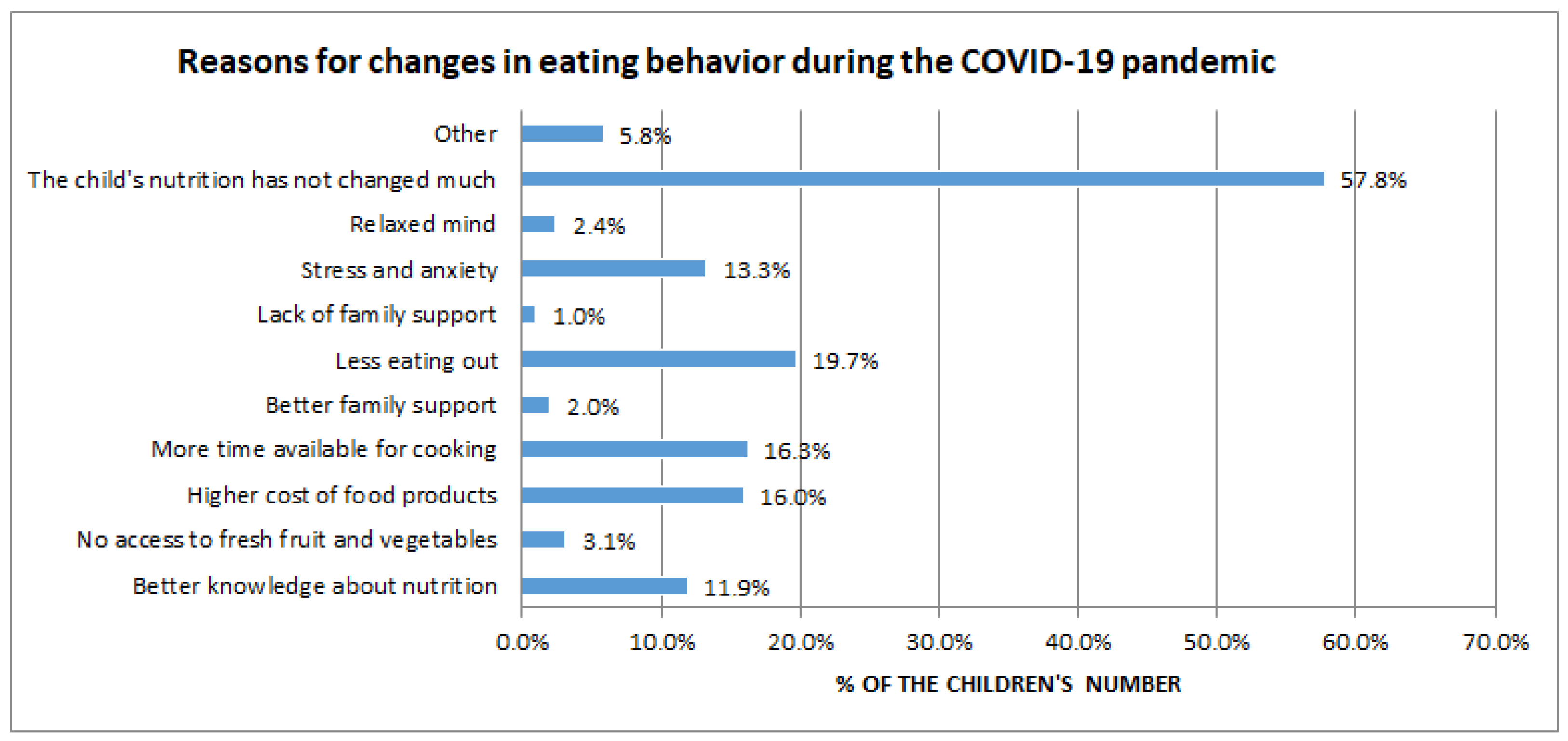
3.4. Causes of Changes in Children’s Eating Behavior and Lifestyle as a Result of the COVID-19 Pandemic
4. Discussion
Strengths and Limitations
5. Conclusions
- pandemic COVID-19 changed the body weight of almost half of the children surveyed, with more weight gains than weight losses;
- there was an increase in the consumption of salty snacks and high-sugar products and sweetened beverages;
- a consequence of the COVID-19 pandemic was a deterioration in dietary habits through a reduction in children’s intake of essential dietary components, i.e., fruit and vegetables and milk and dairy products.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Muralidar, S.; Ambi, S.; Sekaran, S.; Krishnan, U.M. The emergence of COVID-19 as a global pandemic: Understanding the epidemiology, immune response and potential therapeutic targets of SARS-CoV-2. Biochimie 2020, 179, 85–100. [Google Scholar] [CrossRef] [PubMed]
- López-Bueno, R.; López-Sánchez, G.F.; Casajús, J.A.; Calatayud, J.; Tully, M.A.; Smith, L. Potential health-related behaviors for pre-school and school-aged children during COVID-19 lockdown: A narrative review. Prev. Med. 2021, 143, 106349. [Google Scholar] [CrossRef]
- Coronavirus Disease (COVID-19) Situation Reports. (b. d.). World Health Organization (WHO). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 3 March 2023).
- Zhang, X.; Zhu, W.; Kang, S.; Qiu, L.; Lu, Z.; Sun, Y. Association between physical activity and mood states of children and adolescents in social isolation during the COVID-19 epidemic. Int. J. Environ. Res. Public Health 2020, 17, 7666. [Google Scholar] [CrossRef]
- WHO European Childhood Obesity Surveillance Initiative (COSI). (b. d.). World Health Organization (WHO). Available online: https://www.who.int/europe/initiatives/who-european-childhood-obesity-surveillance-initiative-(cosi) (accessed on 3 March 2023).
- Cuschieri, S.; Grech, S. COVID-19: A one-way ticket to a global childhood obesity crisis? J. Diabetes Metab. Disord. 2020, 19, 2027–2030. [Google Scholar] [CrossRef]
- Almousa, L.A.; Alagal, R.I. Effects of the COVID-19 pandemic on diet and physical activity and the possible influence factors among Saudi in Riyadh. Front. Nutr. 2022, 9, 1029744. [Google Scholar] [CrossRef]
- Rozmiarek, M.; León-Guereño, P.; Tapia-Serrano, M.Á.; Thuany, M.; Gomes, T.N.; Płoszaj, K.; Firek, W.; Malchrowicz-Mośko, E. Motivation and Eco-Attitudes among Night Runners during the COVID-19 Pandemic. Sustainability 2022, 14, 1512. [Google Scholar] [CrossRef]
- Manolis, A.S.; Manolis, A.A.; Manolis, T.A.; Apostolaki, N.E.; Melita, H. COVID-19 infection and body weight: A deleterious liaison in a J-curve relationship. Obes. Res. Clin. Pract. 2021, 15, 523–535. [Google Scholar] [CrossRef] [PubMed]
- Rcińska, M.; Rutkowska, N.; Skowronek, M.; Matusik, P.; Zachurzok, A. Desirable and undesirable lifestyle changes in Polish children resulting from the COVID-19 pandemic. Pediatr. Pol. 2022, 97, 213–220. [Google Scholar] [CrossRef]
- Zemrani, B.; Gehri, M.; Masserey, E.; Knob, C.; Pellaton, R. A hidden side of the COVID-19 pandemic in children: The double burden of undernutrition and overnutrition. Int. J. Equity Health 2021, 20, 44. [Google Scholar] [CrossRef] [PubMed]
- Bahatheg, R.O. Young children’s nutrition during the COVID-19 pandemic lockdown: A comparative study. Early Child. Educ. J. 2021, 49, 915–923. [Google Scholar] [CrossRef]
- Rossi, L.; Behme, N.; Breuer, C. Physical Activity of Children and Adolescents during the COVID-19 Pandemic-A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 11440. [Google Scholar] [CrossRef]
- Available online: https://stat.gov.pl/obszary-tematyczne/ludnosc/ludnosc/ludnosc-stan-i-struktura-ludnosci-oraz-ruch-naturalny-w-przekroju-terytorialnym-w-2022-r-stan-w-dniu-30-czerwca-2022,6,33.html (accessed on 1 March 2023).
- Chopra, S.; Ranjan, P.; Malhotra, A.; Sahu, A.; Dwivedi, S.N.; Baitha, U.; Goel, A.; Kumar, A. Development and validation of a questionnaire to evaluate the impact of COVID-19 on lifestyle-related behaviors: Eating habits, activity, and sleep behavior. Public Health Nutr. 2021, 24, 1275–1290. [Google Scholar] [CrossRef] [PubMed]
- Kulaga, Z.; Różdżyńska-Świątkowska, A.; Grajda, A.; Gurzkowska, B.; Wojtyło, M.; Góźdź, M.; Świąder-Leśniak, A.; Litwin, M. Centile grids for assessment of growth and nutritional status of Polish children and adolescents from birth to 18 years of age. Med. Stand./Pediatr. 2015, 12, 119–135. [Google Scholar]
- Lee, S.W. Methods for testing statistical differences between groups in medical research: Statistical standard and guideline of Life Cycle Committee. Life Cycle 2022, 2, e1. [Google Scholar] [CrossRef]
- Azrak, M.Á.; Fasano, M.V.; Avico, A.J.; Sala, M.; Casado, C.; Padula, M.; Krugetr, A.L.; Malpeli, A.; Andreoli, M.F. Prolonged body weight gain, lifestyle changes and health-related quality of life in children during the COVID-19 pandemic lockdown: A follow-up study. Eur. J. Clin. Nutr. 2022, 1–8, Advance online publication. [Google Scholar] [CrossRef]
- Androutsos, O.; Perperidi, M.; Georgiou, C.; Chouliaras, G. Lifestyle changes and determinants of children’s and adolescents’ body weight increase during the first COVID-19 lockdown in Greece: The COV-EAT study. Nutrients 2021, 13, 930. [Google Scholar] [CrossRef]
- Pujia, R.; Ferro, Y.; Maurotti, S.; Khoory, J.; Gazzaruso, C.; Pujia, A.; Montalcini, T.; Mazza, E. The effects of COVID-19 on the eating habits of children and adolescents in Italy: A pilot survey study. Nutrients 2021, 13, 2641. [Google Scholar] [CrossRef]
- Sharma, S.V.; Chuang, R.J.; Rushing, M.; Naylor, B.; Ranjit, N.; Pomeroy, M.; Markham, C. Social determinants of health-related needs during COVID-19 among low-income households with children. Prev. Chronic Dis. 2020, 17, E119. [Google Scholar] [CrossRef] [PubMed]
- Kolota, A.; Glabska, D. COVID-19 Pandemic, and remote education contributes to improved nutritional behaviors and increased screen time in a Polish population-based sample of primary school adolescents: Diet and activity of youth during COVID-19 (DAY-19) study. Nutrients 2021, 13, 1596. [Google Scholar] [CrossRef]
- Koletzko, B.; Holzapfel, C.; Schneider, U.; Hauner, H. Lifestyle and body weight consequences of the COVID-19 pandemic in children: Increasing disparity. Ann. Nutr. Metab. 2021, 77, 1–3. [Google Scholar] [CrossRef]
- Siachpazidou, D.I.; Kotsiou, O.S.; Chatziparasidis, G.; Papagiannis, D.; Vavougios, G.; Gogou, E.; Stavrou, V.; Gourgoulialnis, K. Action and reaction of pre-primary and primary school-age children to restrictions during the COVID-19 pandemic in Greece. J. Pers. Med. 2021, 11, 451. [Google Scholar] [CrossRef]
- Radwan, A.; Radwan, E.; Radwan, W. Eating habits among primary and secondary school students in the Gaza Strip, Palestine: A cross-sectional study during the COVID-19 pandemic. Appetite 2021, 163, 105222. [Google Scholar] [CrossRef]
- Hourani, H.A.; Alkhatib, B.; Abdullah, M. Impact of COVID-19 lockdown on body weight, eating habits, and physical activity of Jordanian children and adolescents. Disaster Med. Public Health Prep. 2021, 19, 1855–1863. [Google Scholar] [CrossRef] [PubMed]
- Luszczki, E.; Bartosiewicz, A.; Pezdan-Śliż, I.; Kuchciak, M.; Jagielski, P.; Oleksy, Ł.; Stolarczyk, A.; Dereń, K. Children’s eating habits, physical activity, sleep, and media usage before and during the COVID-19 pandemic in Poland. Nutrients 2021, 13, 2447. [Google Scholar] [CrossRef]
- Fasano, M.V.; Padula, M.; Azrak, M.Á.; Avico, A.J.; Sala, M.; Andreoli, M.F. Consequences of lockdown during COVID-19 pandemic in lifestyle and emotional state of children in Argentina. Front. Pediatr. 2021, 9, 660033. [Google Scholar] [CrossRef] [PubMed]
- Ventura, P.S.; Ortigoza, A.F.; Castillo, Y.; Bosch, Z.; Casals, S.; Girbau, C.; Siurana, J.M.; Alrce, A.; Torres, M.; Herrero, F.J. Children’s health habits and COVID-19 lockdown in Catalonia: Implications for obesity and non-communicable diseases. Nutrients 2021, 13, 1657. [Google Scholar] [CrossRef]
- Francisco, R.; Pedro, M.; Delvecchio, E.; Etspada, J.P.; Morales, A.; Mazzeschi, C.; Orgilés, M. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Front. Psychiatry 2020, 11, 570164. [Google Scholar] [CrossRef]
- Tillmann, S.; Tobin, D.; Avison, W.; Gilliland, J. Mental health benefits of interactions with nature in children and teenagers: A systematic review. J. Epidemiol. Community Health 2018, 72, 958–966. [Google Scholar] [CrossRef] [PubMed]
- Saurabh, K.; Ranjan, S. Compliance and psychological impact of quarantine in children and adolescents due to covid-19 pandemic. Indian J. Pediatr. 2020, 87, 532–536. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, C.S.; Sandre, P.C.; Portugal, L.C.L.; Mázala-De-Oliveira, T.; da Silva Chagas, L.; Raony, Í.; Ferreira, E.S.; Giestal-De-Araujo, E.; dos Santos, A.A.; Bomfim, P.O.-S. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 106, 110171. [Google Scholar] [CrossRef]
- Wądołowska, L.; Drywień, M.; Hamułka, J.; Socha, P.; Borawska, M.; Friedrich, M.; Lange, E. Dietary recommendations during the covid-19 pandemic. Statement of the committee of human nutrition science of the Polish academy of sciences. Rocz. Państwowego Zakładu Hig. 2021, 72, 209–220. [Google Scholar] [CrossRef]
- De Faria Coelho-Ravagnani, C.; Corgosinho, F.C.; Sanches, F.F.Z.; Prado, C.M.M.; Laviano, A.; Mota, J.F. Dietary recommendations during the COVID-19 pandemic: An extract. Nutr. Rev. 2021, 79, 382–393. [Google Scholar] [CrossRef]
- Iannattone, S.; Raffagnato, A.; Zanato, S.; Traverso, A.; Tascini, B.; Del Col, L.; Miscioscia, M.; Gatta, M. Children with Psychopathology and Their Parents Facing the Covid-19 Pandemic: A Case-Control Study. Clin. Neuropsychiatry 2021, 18, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Wypych-Ślusarska, A.; Grot, M.; Nigowski, M. Zachowania mające na celu wzmocnienie odporności w okresie pandemii COVID-19. Med. Środowiskowa 2021, 24, 5–10. [Google Scholar] [CrossRef]
- Białek-Dratwa, A.; Szczepańska, E.; Grajek, M.; Całyniuk, B.; Staśkiewicz, W. Health Behaviors and Associated Feelings of Remote Workers During the COVID-19 Pandemic—Silesia (Poland). Front. Public Health 2022, 10, 774509. [Google Scholar] [CrossRef] [PubMed]
- Krupa-Kotara, K.; Grajek, M.; Murzyn, A.; Słoma-Krześlak, M.; Sobczyk, K.; Białek-Dratwa, A.; Kowalski, O. Proper Dietary and Supplementation Patterns as a COVID-19 Protective Factor (Cross-Sectional Study-Silesia, Poland). Life 2022, 12, 1976. [Google Scholar] [CrossRef] [PubMed]


| Variable | N (%) | p-Value | |
|---|---|---|---|
| Gender | Girls | 149 (50.7) | >0.05 * |
| Boys | 145 (49.3) | ||
| Grade | 1–3 (6–8 y.) | 108 (36.7) | |
| 4–6 (9–11 y.) | 99 (33.7) | ||
| 7–8 (12–14 y.) | 87 (29.6) | ||
| Place of residence | City | 155 (52.7) | |
| Country | 139 (47.3) |
| Level of Frequency of Consumption of 5 Regular Meals before the COVID-19 Pandemic | Level of Frequency of Consumption of 5 Regular Meals during the COVID-19 Pandemic | ||||||
|---|---|---|---|---|---|---|---|
| Never | 1–2 Times a Week | 3–4 Times a Week | 5–6 Times a Week | Daily | Total (%) | p-Value (Chi2 NW) | |
| Never | 5 (62.50%) | 2 (25.00%) | 0 (0.00%) | 1 (12.50%) | 0 (0.00%) | 8 (100%) | p < 0.001 |
| 1–2 times a week | 2 (11.11%) | 10 (55.56%) | 3 (16.67%) | 1 (5.56%) | 2 (11.11%) | 18 (100%) | |
| 3–4 times a week | 1 (1.69%) | 8 (13.56%) | 31 (52.54%) | 14 (23.73%) | 5 (8.47%) | 59 (100%) | |
| 5–6 times a week | 2 (3.92%) | 5 (9.80%) | 10 (19.61%) | 26 (50.98%) | 8 (15.69%) | 51 (100%) | |
| Daily | 1 (0.63%) | 4 (2.53%) | 11 (6.96%) | 16 (10.13%) | 126 (79.75%) | 158 (100%) | |
| The Frequency Level of Fruit and Vegetable Consumption before the COVID-19 Pandemic | The Frequency Level of Fruit and Vegetable Consumption during the COVID-19 Pandemic | ||||||
|---|---|---|---|---|---|---|---|
| Never | 1–2 Times a Week | 3–4 Times a Week | 5–6 Times a Week | Daily | Total (%) | p-Value (Chi2 NW) | |
| Never | 5 (83.33%) | 1 (16.67%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 6 (100%) | p < 0.001 |
| 1–2 times a week | 1 (2.56%) | 26 (66.67%) | 9 (23.08%) | 3 (7.69%) | 0 (0.00%) | 39 (100%) | |
| 3–4 times a week | 1 (2.08%) | 10 (12.99%) | 50 (64.94%) | 16 (20.78%) | 1 (1.30%) | 77 (100%) | |
| 5–6 times a week | 0 (0.00%) | 7 (12.50%) | 19 (33.93%) | 26 (46.43%) | 4 (7.14%) | 56 (100%) | |
| Daily | 0 (0.00%) | 3 (2.59%) | 12 (10.34%) | 9 (7.76%) | 92 (79.31%) | 116 (100%) | |
| Level of Frequency of Salty Snack Consumption before the COVID-19 Pandemic | Level of Frequency of Salty Snack Consumption during the COVID-19 Pandemic | ||||||
|---|---|---|---|---|---|---|---|
| Never | 1–2 Times a Week | 3–4 Times a Week | 5–6 Times a Week | Daily | Total (%) | p-Value (Chi2 NW) | |
| Never | 28 (73.68%) | 8 (21.05%) | 1 (2.63%) | 1 (2.63%) | 0 (0.00%) | 38 (100%) | p < 0.001 |
| 1–2 times a week | 7 (3.63%) | 141(73.06%) | 35 (18.13%) | 9 (4.66%) | 1 (0.52%) | 193 (100%) | |
| 3–4 times a week | 1 (2.08%) | 11 (22.92%) | 28 (58.33%) | 2 (4.17%) | 6 (12.50%) | 48 (100%) | |
| 5–6 times a week | 0 (0.00%) | 1 (16.67%) | 3 (50.00%) | 2 (33.33%) | 0 (0.00%) | 6 (100%) | |
| Daily | 0 (0.00%) | 2 (22.22%) | 0 (0.00%) | 0 (0.00%) | 7 (77.78%) | 9 (100%) | |
| Level of Frequency of Exercise/Moderate Intensity Sports before the COVID-19 Pandemic | Level of Frequency of Moderate-Intensity Exercise/Sports during the COVID-19 Pandemic | ||||||
|---|---|---|---|---|---|---|---|
| Never | 1–2 Times a Week | 3–4 Times a Week | 5–6 Times a Week | Daily | Total (%) | p-Value (Chi2 NW) | |
| Never | 18 (69.23%) | 7 (26.92%) | 1 (3.85%) | 0 (0.00%) | 0 (0.00%) | 26 (100%) | p < 0.001 |
| 1–2 times a week | 13 (15.85%) | 60 (73.17%) | 6 (7.32%) | 1 (1.22%) | 2 (2.44%) | 82 (100%) | |
| 3–4 times a week | 3 (3.06%) | 38 (38.78%) | 44(44.90%) | 9 (9.18%) | 4 (4.08%) | 98 (100%) | |
| 5–6 times a week | 1 (2.63%) | 5 (13.16%) | 17 (44.74%) | 13 (34.21%) | 2 (5.26%) | 38 (100%) | |
| Daily | 3 (6.00%) | 9 (18.00%) | 10 (20.00%) | 5 (10.00%) | 23 (46.00%) | 50 (100%) | |
| Time Spent in front of TV/Phone/Computer Screen before the COVID-19 Pandemic | Time Spent in front of TV/Phone/Computer Screen during the COVID-19 Pandemic | |||||
|---|---|---|---|---|---|---|
| Less Than an Hour | 1–2 h | 3–4 h | More Than 4 h | Total (%) | p-Value (Chi2 NW) | |
| Less than an hour | 28 (45.90%) | 18 (29.51%) | 7 (11.48%) | 8 (13.11%) | 61 (100%) | p < 0.001 |
| 1–2 h | 3 (2.19%) | 57 (41.61%) | 53 (38.69%) | 24 (17.52%) | 137 (100%) | |
| 3–4 h | 0 (0.00%) | 4 (4.94%) | 45 (55.56%) | 32 (39.51%) | 81 (100%) | |
| More than 4 h | 0 (0.00%) | 0 (0.00%) | 4 (26.67%) | 11 (73.33%) | 15 (100%) | |
| Time Allotted for Sleep before the COVID-19 Pandemic | Time Spent Sleeping during the COVID-19 Pandemic | ||||
|---|---|---|---|---|---|
| Less Than 6 h | 6–8 h | More Than 8 h | Total (%) | p-Value (Chi2 NW) | |
| Less than 6 h | 3 (50.00%) | 2 (33.33%) | 1 (16.67%) | 6 (100%) | p < 0.001 |
| 6–8 h | 12 (8.51%) | 120 (85.11%) | 9 (6.38%) | 141 (100%) | |
| More than 8 h | 0 (0.00%) | 35 (23.81%) | 112 (76.19%) | 147 (100%) | |
| Level of Perceived Stress/Anxiety of the Pandemic COVID-19 | Level of Perceived Stress/Anxiety of the Pandemic COVID-19 | |||||
|---|---|---|---|---|---|---|
| Did Not Feel It at All | Sometimes | Often | Very Often | Total (%) | p-Value (Chi2 NW) | |
| Did not feel It at all | 44 (55.00%) | 29 (36.25%) | 6 (7.50%) | 1 (1.25%) | 80 (100%) | p < 0.001 |
| Sometimes | 6 (3.00%) | 154 (77.00%) | 33 (16.50%) | 7 (3.50%) | 200 (100%) | |
| Often | 0 (0.00%) | 3 (27.27%) | 7 (63.64%) | 1 (9.09%) | 11 (100%) | |
| Very often | 1 (33.33%) | 1 (3.33%) | 0 (0.00%) | 1 (33.33%) | 3 (100%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krupa-Kotara, K.; Wojtas, G.; Grajek, M.; Grot, M.; Rozmiarek, M.; Wypych-Ślusarska, A.; Oleksiuk, K.; Głogowska-Ligus, J.; Słowiński, J. Impact of the COVID-19 Pandemic on Nutrition, Sleep, Physical Activity, and Mood Disorders of Polish Children. Nutrients 2023, 15, 1928. https://doi.org/10.3390/nu15081928
Krupa-Kotara K, Wojtas G, Grajek M, Grot M, Rozmiarek M, Wypych-Ślusarska A, Oleksiuk K, Głogowska-Ligus J, Słowiński J. Impact of the COVID-19 Pandemic on Nutrition, Sleep, Physical Activity, and Mood Disorders of Polish Children. Nutrients. 2023; 15(8):1928. https://doi.org/10.3390/nu15081928
Chicago/Turabian StyleKrupa-Kotara, Karolina, Gabriela Wojtas, Mateusz Grajek, Martina Grot, Mateusz Rozmiarek, Agata Wypych-Ślusarska, Klaudia Oleksiuk, Joanna Głogowska-Ligus, and Jerzy Słowiński. 2023. "Impact of the COVID-19 Pandemic on Nutrition, Sleep, Physical Activity, and Mood Disorders of Polish Children" Nutrients 15, no. 8: 1928. https://doi.org/10.3390/nu15081928
APA StyleKrupa-Kotara, K., Wojtas, G., Grajek, M., Grot, M., Rozmiarek, M., Wypych-Ślusarska, A., Oleksiuk, K., Głogowska-Ligus, J., & Słowiński, J. (2023). Impact of the COVID-19 Pandemic on Nutrition, Sleep, Physical Activity, and Mood Disorders of Polish Children. Nutrients, 15(8), 1928. https://doi.org/10.3390/nu15081928










