Do Food and Nutrition Policies in Ethiopia Support the Prevention of Non-Communicable Diseases through Population-Level Salt Reduction Measures? A Policy Content Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Setting
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction and Analysis
3. Results
3.1. Description of Documents Reviewed
3.2. Comprehensiveness of Policy Measures
3.2.1. Alignment with Diet-Related NCDs
3.2.2. Extent to Which Food and Nutrition Issues Are Addressed
3.2.3. Content Relevant to Salt Reduction
3.3. Policy Salience and Implementation Potential
3.3.1. Policy Authority
3.3.2. Budget and Systems of Accountability
3.4. Equity, Gender and Human Rights Orientation
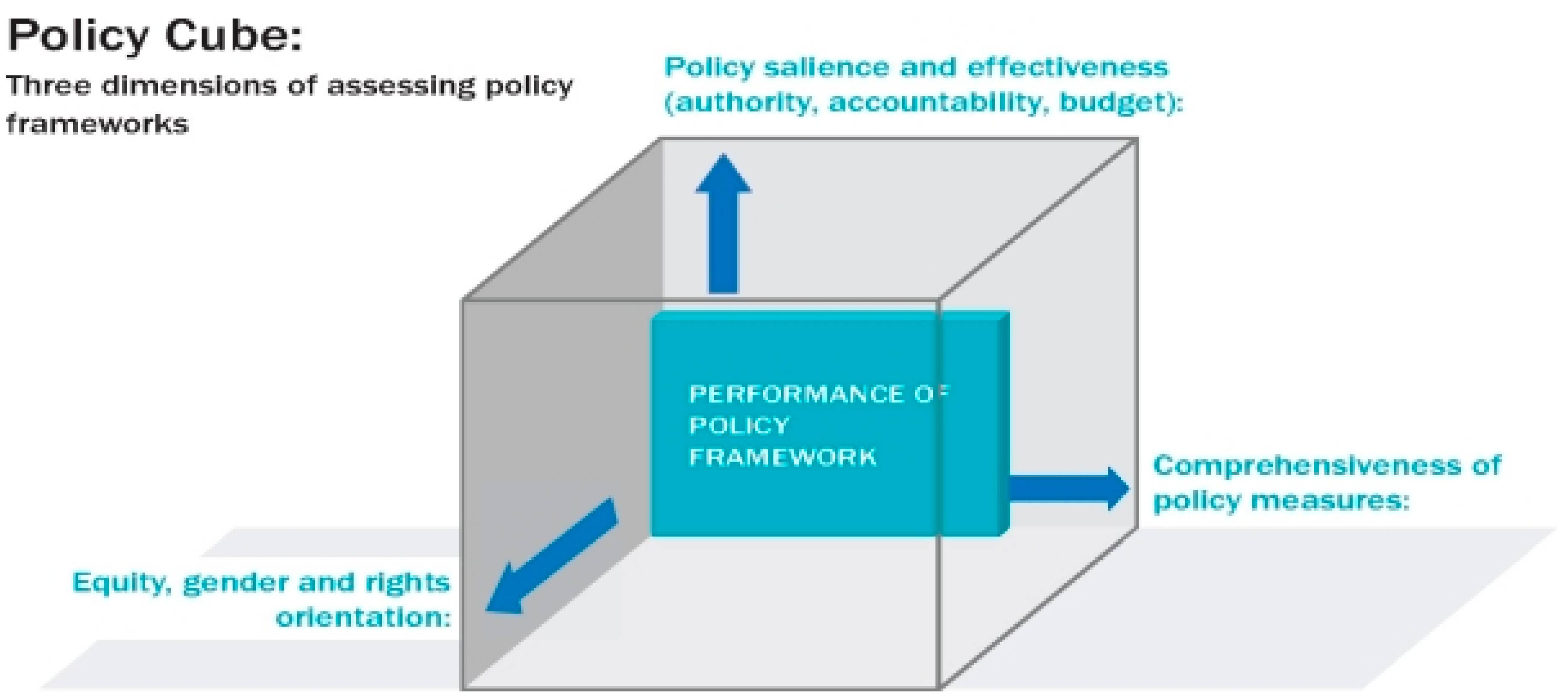
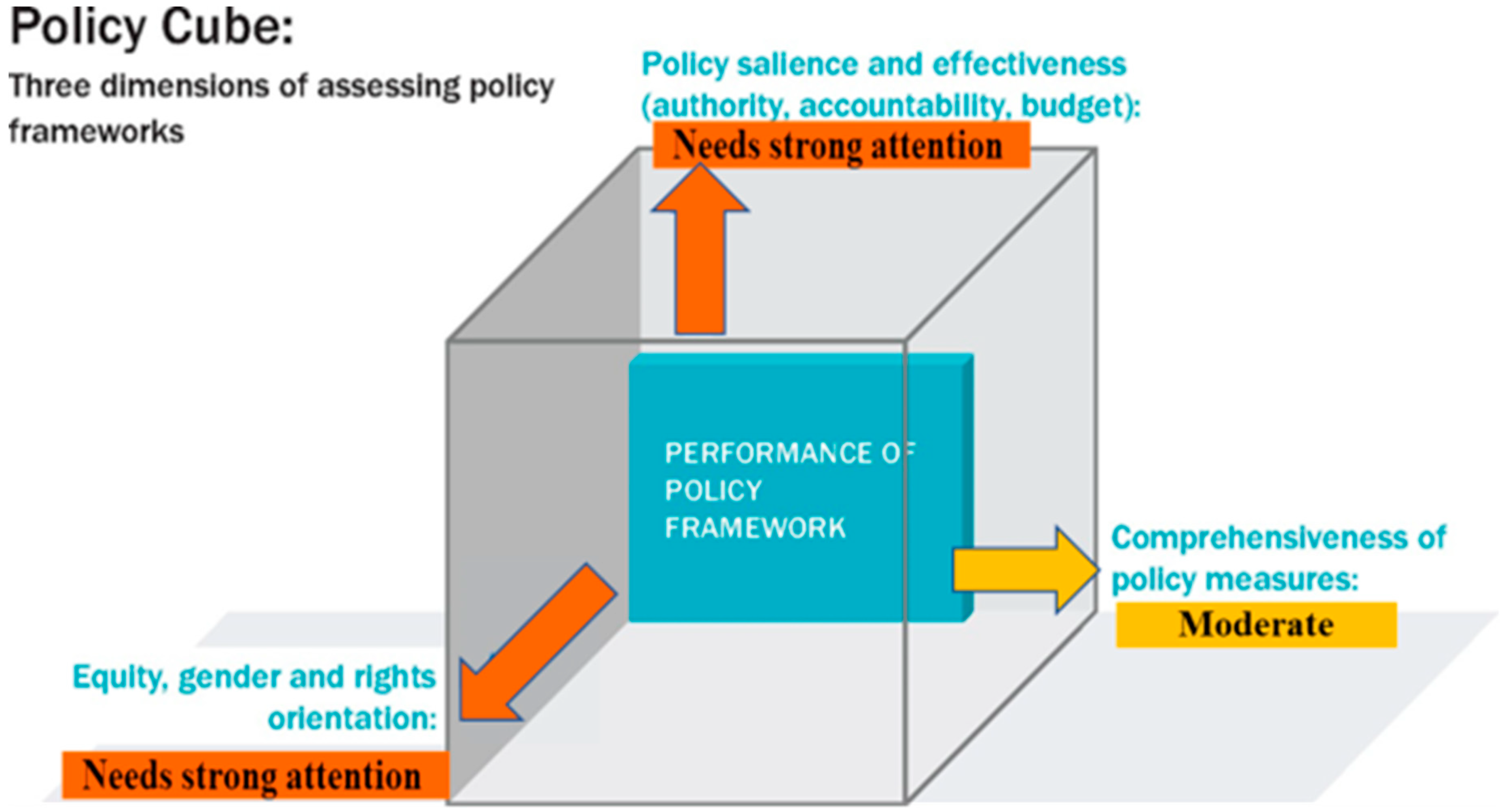
Summarizing the Findings in a Policy Cube
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- NCD Countdown Collaborators. NCD Countdown 2030: Worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal Target 3.4. Lancet 2018, 392, 1072–1088. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Estimates 2016: Deaths by Cause Age, Sex, by Country and by Region 2000–2016; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Nyirenda, M.J. Non-communicable diseases in sub-Saharan Africa: Understanding the drivers of the epidemic to inform intervention strategies. Int. Health 2016, 8, 157–158. [Google Scholar] [CrossRef] [PubMed]
- Holmes, M.D.; Dalal, S.; Volmink, J.; Adebamowo, C.A.; Njelekela, M.; Fawzi, W.W.; Willett, W.; Adami, H.-O.; Holmes, M.D. Non-communicable diseases in sub-Saharan Africa: The case for cohort studies. PLoS Med. 2010, 7, e1000244. [Google Scholar] [CrossRef]
- Shiferaw, F.L.M.; Misganaw, A.; Feleke, Y.; Gelibo, T.; Getachew, T.; Defar, A.; Assefa, A.; Bekele, A.; Amenu, K.; Teklie, H.; et al. Non-communicable Diseases in Ethiopia: Disease burden, gaps in health care delivery and strategic directions. Ethiop. J. Dev. 2018, 32, 3. [Google Scholar]
- Misganaw, A.H.T.; Deribe, K.; Tessema, G.A.; Deribew, A.; Melaku, Y.A.; Amare, A.T.; Abera, S.F.; Gedefaw, M.; Dessalegn, M.; Lakew, Y.; et al. National mortality burden due to communicable, non-communicable, and other diseases in Ethiopia, 1990–2015: Findings from the Global Burden of Disease Study 2015. Popul. Health Metr. 2017, 15, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Bollyky, T.J.T.T.; Cohen, M.; Dieleman, J.L. Lower-income countries that face the most rapid shift in noncommunicable disease burden are also the least prepared. Health Aff. 2017, 36, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.V.T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; Atkinson, C.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2010, 380, 2224–2260. [Google Scholar] [CrossRef]
- Stanaway, J.D.A.A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; et al. Global, regional, and national comparative risk assessment of 84 behavioral, environmental, and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Institute for Health Metrics and Evaluation. GBD Compare Seattle, WA Washington: IHME. 2021. Available online: https://vizhub.healthdata.org/gbd-compare/ (accessed on 24 January 2023).
- Graudal, N.A.; Hubeck-Graudal, T.; Jürgens, G. Effects of Low-Sodium Diet vs. High-Sodium Diet on Blood Pressure, Renin, Aldosterone, Catecholamines, Cholesterol, and Triglyceride (Cochrane Review). Am. J. Hypertens. 2012, 25, 1–15. [Google Scholar] [CrossRef]
- He, F.J.; Li, J.; MacGregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef]
- Huang, L.; Trieu, K.; Yoshimura, S.; Neal, B.; Woodward, M.; Campbell, N.R.; Li, Q.; Lackland, D.T.; Leung, A.A.; Anderson, C.A.M.; et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: Systematic review and meta-analysis of randomised trials. BMJ 2020, 368, m315. [Google Scholar] [CrossRef] [PubMed]
- Collaborators GRF. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2016, 390, 10100. [Google Scholar]
- World Health Organisation. Global Health Observatory: Raised Blood Pressure: World Health Organisation. 2010. Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3155#:~:text=Worldwide%2C%20raised%20blood%20pressure%20is%20estimated%20to%20cause,disease%20and%20ischemic%20as%20well%20as%20hemorrhagic%20stroke (accessed on 24 January 2023).
- Campbell, N.; Correa-Rotter, R.; Neal, B.; Cappuccio, F.P. New evidence relating to the health impact of reducing salt intake. Metab. Dis. 2011, 2011, 617–619. [Google Scholar] [CrossRef]
- Antonios, T.F.; MacGregor, G.A. Salt—More Adverse Effects. Lancet 1996, 348, 250–251. [Google Scholar] [CrossRef]
- Nordin, B.C.; Need, A.G.; Morris, H.A.; Horowitz, M. The nature and significance of the relationship between urinary sodium and urinary calcium in women. J. Nutr. 1993, 123, 1615–1622. [Google Scholar] [CrossRef]
- World Healh Organisation. 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases: Prevent and Control Cardiovascular Diseases, Cancers, Chronic Respiratory Diseases and Diabetes: Wolrd Health Organisation. 2009. Available online: https://apps.who.int/iris/handle/10665/44009#:~:text=Plan%20de%20Accio%CC%81n%202008-2013%20de%20la%20estrategia%20mundial,cardiovascular%20diseases%2C%20cancers%2C%20chronic%20respiratory%20diseases%20and%20diabetes (accessed on 24 January 2023).
- Health Societies. The NCD Policy Cube: Representing the Strength of Policy Environments to Combat NCDs: Health Societies. Available online: https://www.healthysocieties2030.org/ncds/ncd-policy-cube (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia. Food and Nutrition Policy Ethiopia. 2018. Available online: https://www.nipn.ephi.gov.et/sites/default/files/2020-05/Food%20and%20Nutrition%20Policy.pdf (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia. National Health Policy Ethiopia. 2019. Available online: https://www.scribd.com/document/358431814/Ethiopian-National-Health-Policy-PDF# (accessed on 24 January 2023).
- Buse, K.A.W.; Akhter, S.; Phuong, L.B.; Chemli, H.; Dahal, M.; Feroz, A.; Hofiani, S.; Pradhan, N.A.; Anwar, I.; Skhiri, H.A.; et al. The state of diet-related NCD policies in Afghanistan, Bangladesh, Nepal, Pakistan, Tunisia and Vietnam: A comparative assessment that introduces a ‘policy cube’ approach. Health Policy Plan. 2020, 35, 503–521. [Google Scholar] [CrossRef] [PubMed]
- Federal Democratic Republic of Ethiopia. Food, Medicine and Health Care Administration and Control Proclamation. 2010. Available online: http://www.fmhaca.gov.et/wp-content/uploads/2020/06/Food-and-Medicine-Administration-Proclamation-1112.pdf/ (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia Ministry of Health. Second Generation Health Extension Program Ethiopia: Ministry of Health Ethiopia. 2015. Available online: https://publications.jsi.com/JSIInternet/Inc/Common/_download_pub.cfm?id=16833&lid=3#:~:text=The%20components%20of%20the%20health%20extension%20program%20varies,the%20community%20level%20and%20institutionalizing%20the%20WDA%20platform (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia Ministry of Agriculture and Nutrition. Nutrition Sensitive Agriculture Strategic Plan: Ministry of Agriculture and Natural Resource. 2016. Available online: https://faolex.fao.org/docs/pdf/eth174139.pdf (accessed on 24 January 2023).
- Federal Ministry of Health. National Strategic Plan for the Prevention and Control of Major Non-communicable Diseases Addis Ababa: Ministry of Health Ethiopia. 2020. Available online: https://www.iccp-portal.org/system/files/plans/ETH_B3_s21_National_Strategic_Plan_for_Prevention_and_Control_of_NCDs2021.pdf (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia. National Nutrition Program II Ethiopia: Ministry of Health—Ethiopia. 2016. Available online: https://faolex.fao.org/docs/pdf/eth190946.pdf (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia Ministry of Health. Health Sector Development Programme IV: United Nations. 2010. Available online: https://leap.unep.org/countries/et/national-legislation/health-sector-development-program-iv-201011-201415#:~:text=This%20Health%20Sector%20Development%20Program%20%28HSDP%29%20IV%20is,Vision%20of%20%22seeing%20healthy%2C%20productive%2C%20and%20prosperous%20Ethiopians%22 (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia. National Nutrition Programme June 2013–June 2015 Ethiopia. Government of the Federal Democratic Republic of Ethiopia. 2015. Available online: https://extranet.who.int/nutrition/gina/sites/default/filesstore/ETH%202013%20National%20Nutrition%20Programme.pdf (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia. National Cancer Control Plan 2016–2020. 2015. Available online: https://www.iccp-portal.org/system/files/plans/NCCP%20Ethiopia%20Final%20.pdf (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia Ministry of Health. National Strategic Action Plan (NSAP) for Prevention & Control of Non-Communicable Diseases in Ethiopia: 2014–2016: Ministry of Health Ethiopia. 2016. Available online: http://dataverse.nipn.ephi.gov.et/bitstream/handle/123456789/1425/final-NSAP.pdf?sequence=1 (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia Ministry of Health. National Health Promotion and Communication Strategy 2016–2020. Ethiopia: Federal Ministry of Health. 2016. Available online: https://www.medbox.org/document/national-health-promotion-and-communication-strategy-2016-2020#GO (accessed on 24 January 2023).
- Ministry of Education. National School Health and Nutrition Strategy UNESCO. 2012. Available online: https://healtheducationresources.unesco.org/library/documents/national-school-health-and-nutrition-strategy (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia Ministry of Agriculture and Nutrition. Agriculture and Natural Resources Sector Growth and Transformation Plan II: United Nations. 2016. Available online: https://leap.unep.org/countries/et/national-legislation/agriculture-and-natural-resources-sector-growth-and#:~:text=The%20ANR%20GTP%20II%20is%20a%20nationwide%20sectoral,Growth%20and%20Transformation%20Plan%20%28GTP%29%20of%20the%20country (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia Ministry of Agriculture. Agricultural Growth Program II: Global Agriculture and Food Security Program. 2015. Available online: https://www.gafspfund.org/projects/agricultural-growth-project-ii-agp-ii (accessed on 24 January 2023).
- Federal Democratic Republic of Ethiopia Ministry of Health. Ethiopian Nutrition Advocacy Plan: USAID. 2013. Available online: https://www.fantaproject.org/sites/default/files/resources/Ethiopia-Nutrition-Advocacy-Apr2013.pdf (accessed on 24 January 2023).
- An, R.; Patel, D.; Segal, D.; Sturm, R. Eating better for less: A national discount program for healthy food purchases in South Africa. American journal of health behavior. Am. J. Health Behav. 2013, 37, 56–61. [Google Scholar] [CrossRef]
- Federal Democratic Republic of Ethiopia Ministry of Health. Health Sector Transformation Plan I Ethiopia: The Federal Democratic Republic of Ethiopia Ministry of Health. 2015. Available online: https://www.medbox.org/document/ethiopia-health-sector-transformation-plan-201516-201920-2008-2012-efy#GO (accessed on 24 January 2023).
- Liu, W.; Zhou, L.; Yin, W.; Wang, J.; Zuo, X. Global, Regional, and National Burden of Chronic Kidney Disease attributable to high Sodium Intake from 1990 to 2019. Front. Nutr. 2023, 10, 1078371. [Google Scholar] [CrossRef]
- Premuzic, V.M.B.; Krtalic, B.; Gellineo, L.; Knezevic, T.; Jelakovic, A.; Dapic, K.; Matasin, M.; Ivkovic, V.; Fucek, M.; Josipovic, J.; et al. New Onset Chronic Kidney Diease Is Associated with High Sodium Intake in Population with Low Potassium Consumption. J. Hypertens. 2019, 37, e249. [Google Scholar] [CrossRef]
- Kaldor, J.C.; Thow, A.M.; Schönfeldt, H. Using regulation to limit salt intake and prevent non-communicable diseases: Lessons from South Africa’s experience. Public Health Nutr. 2019, 22, 1316–1325. [Google Scholar]
- Frieden, T.R.; Cobb, L.K.; Leidig, R.C.; Mehta, S.; Kass, D. Reducing premature mortality from cardiovascular and other non-communicable diseases by one third: Achieving sustainable development goal indicator 3.4. 1. Glob. Heart 2020, 15, 50. [Google Scholar] [CrossRef] [PubMed]
- Vital Strategies. New Campaign Encourages Ethiopians TO Cut Salt Consumption in Half and Prevent Unhealthy Diets Ethopia: World Health Organisation. 2021. Available online: https://www.afro.who.int/news/ethiopia-launches-national-salt-reduction-media-campaign-combat-hypertension-and-heart-disease#:~:text=Ethiopia%20has%20launched%20a%20national%20salt%20reduction%20media,collaboration%20with%20WHO%20and%20Resolve%20to%20Save%20Lives (accessed on 24 January 2023).
- Baum, F.; Fisher, M. Why behavioural health promotion endures despite its failure to reduce health inequities. Sociol. Health and Illn. 2014, 36, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Gluckman, P.D.; Hanson, M.A.; Buklijas, T. A conceptual framework for the developmental origins of health and disease. J. Dev. Orig. Health Dis. 2010, 1, 6–18. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Political declaration of the High-Level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases; World Health Organisation: New York, NY, USA, 2011. [Google Scholar]
- Rasanathan, K.; Bennett, S.; Atkins, V.; Beschel, R.; Carrasquilla, G.; Charles, J.; Dasgupta, R.; Emerson, K.; Glandon, D.; Kanchanachitra, C.; et al. Governing multisectoral action for health in low-and middle-income countries. PLoS Med. 2017, 14, e1002285. [Google Scholar]
- Kraak, V.I.; Swinburn, B.; Lawrence, M.; Harrison, P. An accountability framework to promote healthy food environments. Public health nutrition. Public Health Nutr. 2014, 17, 2467–2483. [Google Scholar] [CrossRef] [PubMed]
- Zuccala, E.; Horton, R. Reframing the NCD agenda: A matter of justice and equity. Lancet 2020, 396, 939–940. [Google Scholar] [CrossRef]
- Federal Democratic Republic of Ethiopia. National Nutrition Program Ethiopia: Ministry of Health—Ethiopia. 2016. Available online: https://www.moh.gov.et/site/initiatives-4-col/Nutrition (accessed on 24 January 2023).
- Barker, D.J. The fetal and infant origins of adult disease. BMJ 1990, 301, 1111. [Google Scholar] [CrossRef]
- Monk, C.; Georgieff, M.K.; Osterholm, E.A. Maternal prenatal distress and poor nutrition–mutually influencing risk factors affecting infant neurocognitive development. J. Child Psychol. Psychiatry 2012, 54, 115–130. [Google Scholar] [CrossRef]
- Federal Democratic Republic of Ethiopia Constitution. The Constitution of the Federal Democratic Republic of Ethiopia Addis Ababa. 1995. Available online: https://www.refworld.org/docid/3ae6b5a84.html (accessed on 24 January 2023).
- Grover, A. Thematic Study on the Realization of the Right to Health of Older Persons/by the Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health, Anand Grover: United Nations. 2011. Available online: https://digitallibrary.un.org/record/710913 (accessed on 24 January 2023).
| Type of Document | Document Title | Period Covered | Published by | Source (Where Publicly Availiable) |
|---|---|---|---|---|
| Policy | National Food and Nutrition Policy [21] | 2018–2030 | Government of Ethiopia | Accessed: 1 January 2023 https://www.nipn.ephi.gov.et/sites/default/files/2020-05/Food%20and%20Nutrition%20Policy.pdf |
| Ethiopia National Health Policy [22] | 2019–2029 | Ministry of Health | Accessed: 1 January 2023 https://www.scribd.com/document/358431814/Ethiopian-National-Health-Policy-PDF# | |
| Proclamation | Food, Medicine and Health Care Administration and Control Proclamation No. 661/2009 [24] | 2010–2020 | Ethiopian Food and Drug Authority | |
| Program | National Nutrition Program II [28] | 2016–2021 | Ministry of Health | Accessed: 1 January 2023 https://faolex.fao.org/docs/pdf/eth190946.pdf |
| Second Generation Health Extension Program (HEP) [25] | 2016–2026 | Ministry of Health | Accessed: 1 January 2023 https://publications.jsi.com/JSIInternet/Inc/Common/_download_pub.cfm?id=16833&lid=3#:~:text=The%20components%20of%20the%20health%20extension%20program%20varies,the%20community%20level%20and%20institutionalizing%20the%20WDA%20platform | |
| Health sector development program IV [29] | 2011–2016 | Ministry of Health | Accessed: 1 January 2023 https://leap.unep.org/countries/et/national-legislation/health-sector-development-program-iv-201011-201415#:~:text=This%20Health%20Sector%20Development%20Program%20%28HSDP%29%20IV%20is,Vision%20of%20%22seeing%20healthy%2C%20productive%2C%20and%20prosperous%20Ethiopians%22 | |
| National Nutrition Program—I [30] | 2013–2015 | Ministry of Health | Accessed: 1 January 2023 https://extranet.who.int/nutrition/gina/sites/default/filesstore/FJI%202014%20SSF%20Strategy.pdf | |
| National Plan or Strategy | National Strategic Plan for the Prevention and Control of Major Non-Communicable Diseases [27] | 2021–2025 | Ministry of Health | Accessed: 1 January 2023 https://www.researchgate.net/publication/313109049_Guidelines_on_Clinical_and_Programmatic_Management_of_Major_Non_Communicable_Diseases/link/5c29140ba6fdccfc70731577/download |
| Nutrition Sensitive Agriculture Strategic Plan [26] | 2016–2021 | Ministry of Agriculture | Accessed: 1 January 2023 https://faolex.fao.org/docs/pdf/eth174139.pdf | |
| National Cancer Control Plan [31] | 2016–2021 | Ministry of Health | Accessed: 1 January 2023 https://apps.who.int/iris/handle/10665/44009#:~:text=Plan%20de%20Accio%CC%81n%202008-2013%20de%20la%20estrategia%20mundial,cardiovascular%20diseases%2C%20cancers%2C%20chronic%20respiratory%20diseases%20and%20diabetes | |
| National Strategic Action plan (NSAP) for prevention and control of non-communicable diseases in Ethiopia [32] | 2014–2016 | Ministry of Health | Accessed: 1 January 2023 https://faolex.fao.org/docs/pdf/eth174139.pdf | |
| The National Health Promotion and Communication Strategy [33] | 2016–2020 | Ministry of Health | Accessed: 1 January 2023 https://extranet.who.int/nutrition/gina/sites/default/filesstore/FJI%202014%20SSF%20Strategy.pdf | |
| National school health and nutrition strategy [34] | 2013–2018 | Ministries of Education, Health and Agriculture | Accessed: 1 January 2023 https://healtheducationresources.unesco.org/library/documents/national-school-health-and-nutrition-strategy | |
| Agriculture and Natural Resources Sector Growth and Transformation Plan II [35] | 2015–2020 | Ministry of Agriculture and Natural Resources | Accessed: 1 January 2023 https://www.medbox.org/document/ethiopia-health-sector-transformation-plan-201516-201920-2008-2012-efy#GO | |
| Agricultural growth program II [36] | 2015–2020 | Ministry of Agriculture and Natural Resources | Accessed: 1 January 2023 https://www.gafspfund.org/projects/agricultural-growth-project-ii-agp-ii | |
| Ethiopia Nutrition Advocacy Plan [37] | 2013–2018 | Ministry of Health | Accessed: 1 January 2023 https://www.fantaproject.org/sites/default/files/resources/Ethiopia-Nutrition-Advocacy-Apr2013.pdf | |
| Guideline | Guidelines on Clinical and Programmatic Management of Major Non-Communicable Diseases [33] | 2016–2021 | Ministry of Health | Accessed: 1 January 2023 https://www.researchgate.net/publication/313109049_Guidelines_on_Clinical_and_Programmatic_Management_of_Major_Non_Communicable_Diseases/link/5c29140ba6fdccfc70731577/download |
| SN | Policy Title, Policy Type, Time Frame, Policy Authority, Reference | NCD Policy Cube Components | ||
|---|---|---|---|---|
| Comprehensiveness of Policies | Policy Salience and Effectiveness | Equity, Gender and Human Rights Orientation | ||
| 1 | National Food and Nutrition Policy a,M 2018–2030 [21] |
|
|
|
| 2 | National Nutrition Program II c,M 2016–2021 [28] |
|
|
|
| 3 | Health Sector Transformation Plan d,M 2016–2021 [39] |
|
|
|
| 4 | Guidelines on Clinical and Programmatic Management of Major NCDs e,L 2016–2021 [33] |
|
|
|
| 5 | National Cancer Control Plan d,M 2016–2021 [31] |
|
|
|
| 6 | Second Generation Health Extension Program (HEP) c,M 2016–2026 [25] |
|
|
|
| 7 | National Strategic Plan for the Prevention and Control of Major Non-Communicable Diseases 2020/21–2024/25 [27] |
|
|
|
| 8 | National Strategic Action plan (NSAP) for prevention and control of non-communicable diseases in Ethiopia d,M 2014–2016 [32] |
|
|
|
| 9 | Ethiopia Nutrition Advocacy Plan d,L 2013–2018 [37] |
|
|
|
| 10 | National Nutrition Program—I c,M 2013–2015 [30] |
|
|
|
| 11 | Ethiopia National Health Policy a,M 2019–2029 [22] |
|
|
|
| 12 | Health sector development program IV c,M 2011–2016 [29] |
|
|
|
| 13 | Food, Medicine and Health Care Administration and Control Proclamation No. 661/2009 b,H 2010–2020 [24] |
|
|
|
| 14 | The National Health Promotion and Communication Strategy c,M 2016–2020 [33] |
|
|
|
| 15 | National school health and nutrition strategy c,M 2013–2018 [34] |
|
|
|
| 16 | Nutrition Sensitive Agriculture Strategic Plan c,M 2016–2021 [26] |
|
|
|
| 17 | Agriculture and Natural Resources Sector Growth and Transformation Plan II c,M 2015–2020 [35] |
|
|
|
| 18 | Agricultural growth program II (AGP-II) c,M 2015–2020 [36] |
|
|
|
| Hierarchy | Type of Document |
|---|---|
| Highest level of authority | Food, Medicine and Health Care Administration and Control Proclamation No. 661/2009 [24] |
| Moderate level of authority | Nutrition Sensitive agriculture Strategic Plan [26] |
| The National Health Promotion and Communication Strategy [33] | |
| National school health and nutrition strategy [34] | |
| Agriculture and Natural Resources Sector Growth and Transformation Plan II [35] | |
| Agricultural growth program II [36] | |
| National Nutrition Program II [31] | |
| Second Generation HEP [25] | |
| National Nutrition Program I [30] | |
| Health Sector Development Program IV [29] | |
| National food and nutrition policy | |
| Ethiopia National Health Policy [22] | |
| Health Sector Transformation Plan [39] | |
| National cancer control plan [32] | |
| NSAP for prevention and control of non-communicable diseases in Ethiopia [32] | |
| National Strategic Plan for the Prevention and Control of MajorNon-Communicable Diseases [27] | |
| Lowest level of authority | Guidelines on Clinical and Programmatic Management of Major Non-Communicable Diseases [33] |
| Ethiopia Nutrition Advocacy Plan [37] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tekle, D.Y.; Rosewarne, E.; Santos, J.A.; Trieu, K.; Buse, K.; Palu, A.; Thow, A.M.; Jan, S.; Webster, J. Do Food and Nutrition Policies in Ethiopia Support the Prevention of Non-Communicable Diseases through Population-Level Salt Reduction Measures? A Policy Content Analysis. Nutrients 2023, 15, 1745. https://doi.org/10.3390/nu15071745
Tekle DY, Rosewarne E, Santos JA, Trieu K, Buse K, Palu A, Thow AM, Jan S, Webster J. Do Food and Nutrition Policies in Ethiopia Support the Prevention of Non-Communicable Diseases through Population-Level Salt Reduction Measures? A Policy Content Analysis. Nutrients. 2023; 15(7):1745. https://doi.org/10.3390/nu15071745
Chicago/Turabian StyleTekle, Dejen Yemane, Emalie Rosewarne, Joseph Alvin Santos, Kathy Trieu, Kent Buse, Aliyah Palu, Anne Marie Thow, Stephen Jan, and Jacqui Webster. 2023. "Do Food and Nutrition Policies in Ethiopia Support the Prevention of Non-Communicable Diseases through Population-Level Salt Reduction Measures? A Policy Content Analysis" Nutrients 15, no. 7: 1745. https://doi.org/10.3390/nu15071745
APA StyleTekle, D. Y., Rosewarne, E., Santos, J. A., Trieu, K., Buse, K., Palu, A., Thow, A. M., Jan, S., & Webster, J. (2023). Do Food and Nutrition Policies in Ethiopia Support the Prevention of Non-Communicable Diseases through Population-Level Salt Reduction Measures? A Policy Content Analysis. Nutrients, 15(7), 1745. https://doi.org/10.3390/nu15071745






