Adverse Effects on the Thyroid of Chinese Pregnant Women Exposed to Long-Term Iodine Excess: Optimal and Safe Tolerable Upper Intake Levels of Iodine
Abstract
1. Introduction
2. Materials and Methods
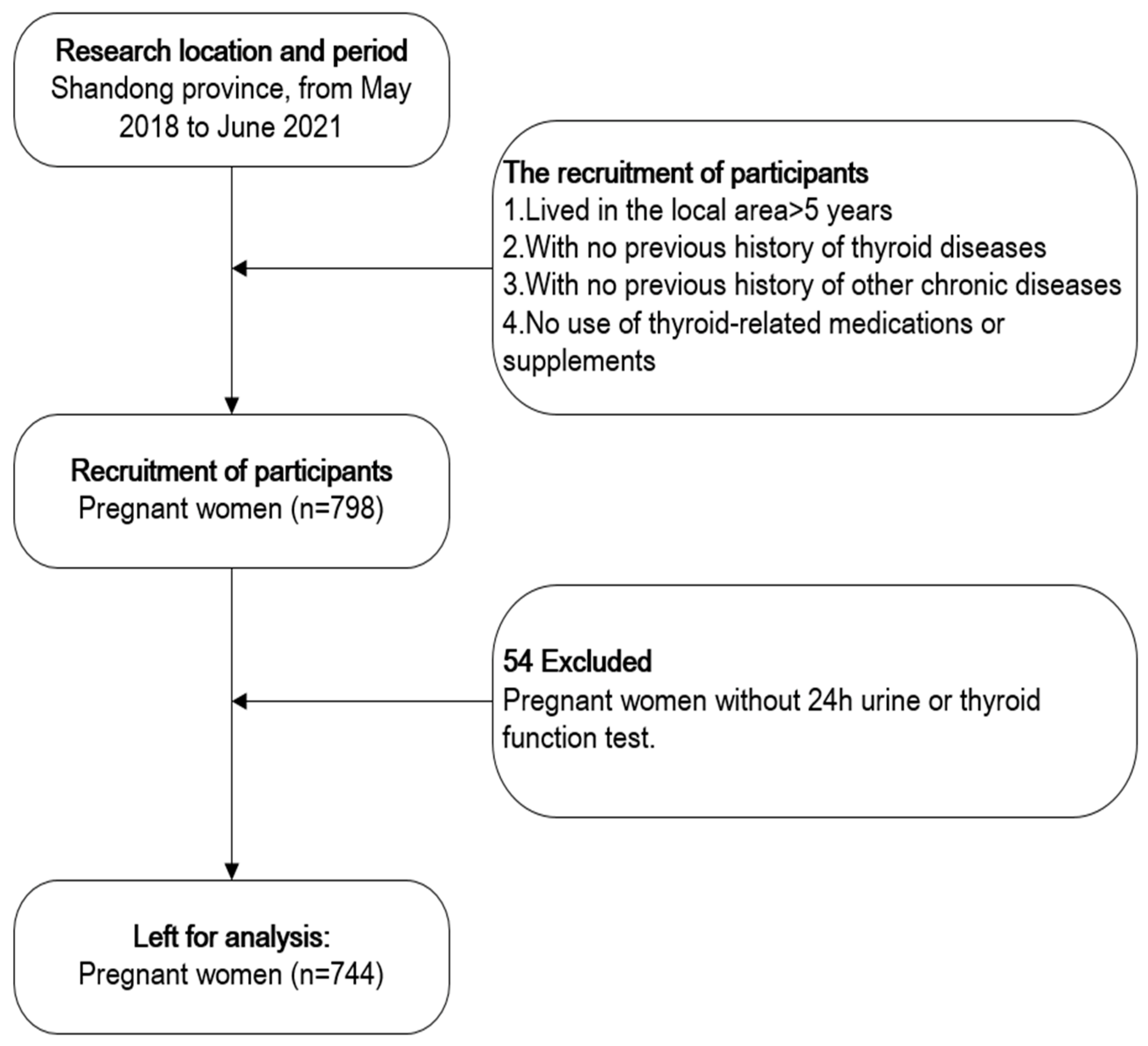
2.1. Study Population
2.2. Baseline Data Collection
2.3. Urine Sample Collection and Analysis
2.4. Iodine Intake Estimation
2.5. Blood Sample Collection and Analysis
2.6. Thyroid Volume Measurements and Thyroid Nodules
2.7. Statistical Analysis
3. Results
3.1. Basic Information
3.2. Thyroid Dysfunction in Relation to Participant Characteristics
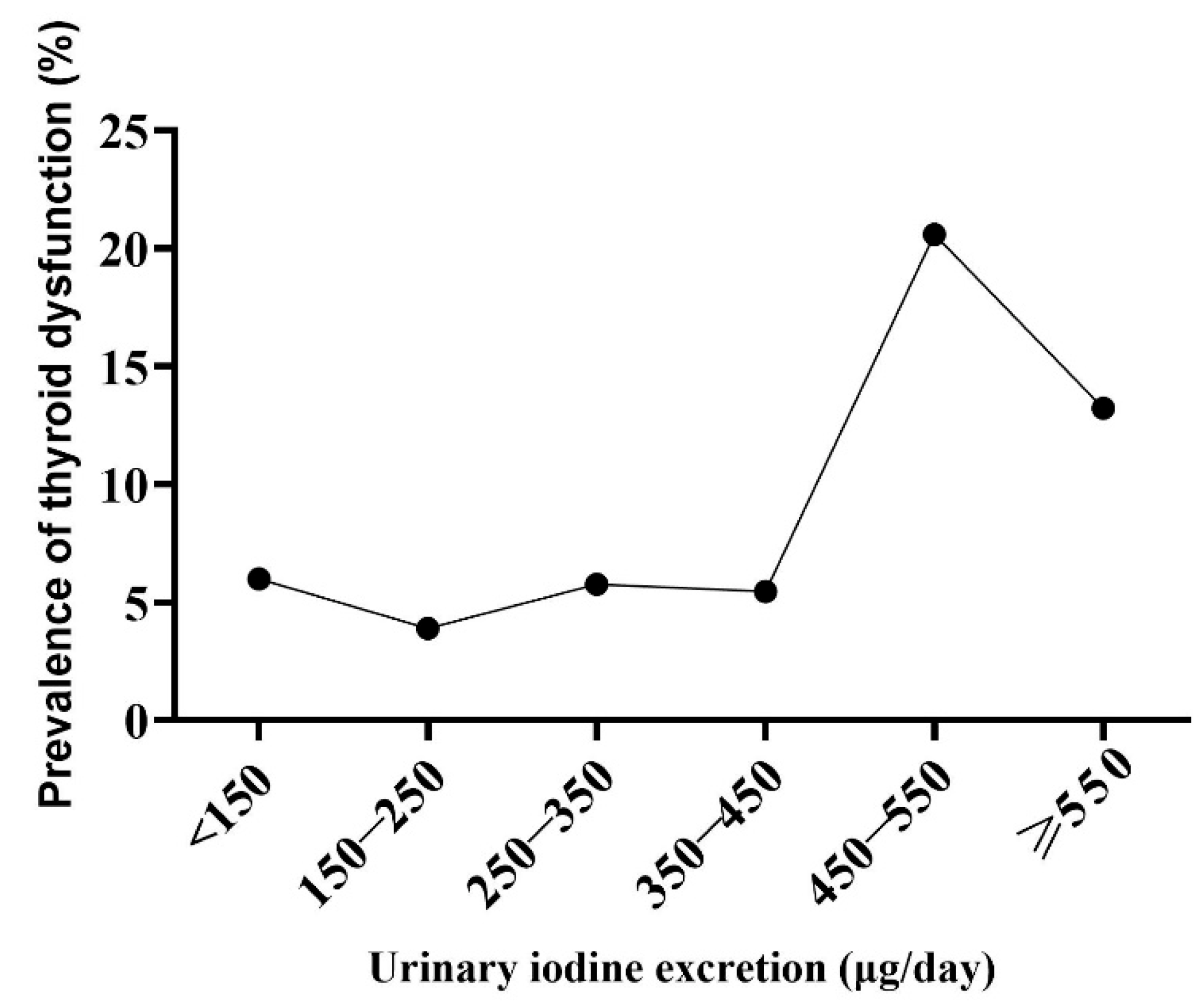
3.3. The Relationship between UIE and Thyroid Dysfunction
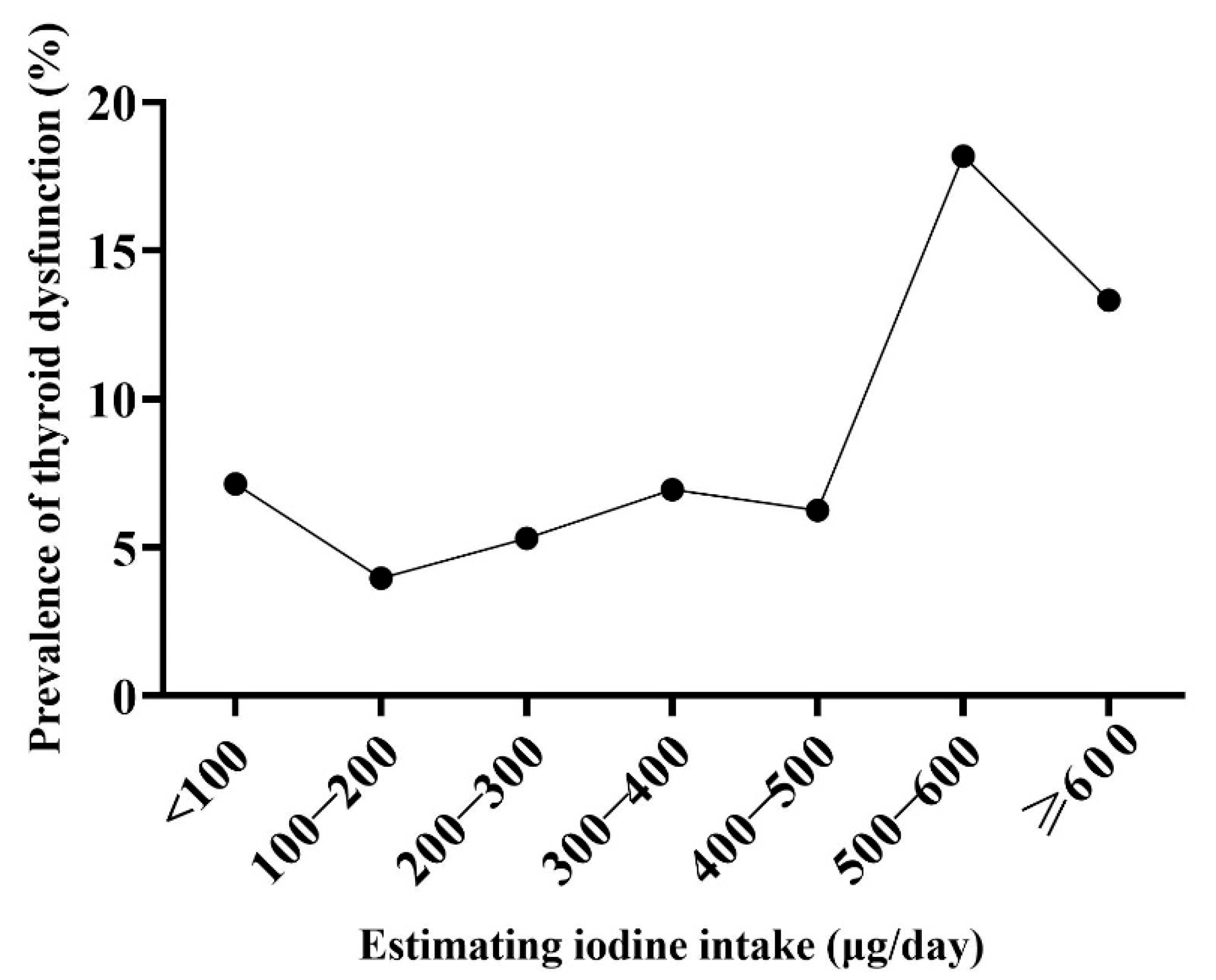
3.4. The Relationship between EII and Thyroid Dysfunction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sang, Z.; Chen, W.; Shen, J.; Tan, L.; Zhao, N.; Liu, H.; Wen, S.; Wei, W.; Zhang, G.; Zhang, W. Long-term exposure to excessive iodine from water is associated with thyroid dysfunction in children. J. Nutr. 2013, 143, 2038–2043. [Google Scholar]
- Zimmermann, M.B.; Boelaert, K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 2015, 3, 286–295. [Google Scholar] [CrossRef]
- Wang, B.; He, W.; Li, Q.; Jia, X.; Yao, Q.; Song, R.; Qin, Q.; Zhang, J.A. U-shaped relationship between iodine status and thyroid autoimmunity risk in adults. Eur. J. Endocrinol. 2019, 181, 255–266. [Google Scholar] [CrossRef]
- Pearce, E.N.; Lazarus, J.H.; Moreno-Reyes, R.; Zimmermann, M.B. Consequences of iodine deficiency and excess in pregnant women: An overview of current knowns and unknowns. Am. J. Clin. Nutr. 2016, 104 (Suppl. 3), 918S–923S. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Sang, Z.; Tan, L.; Zhang, S.; Dong, F.; Chu, Z.; Wei, W.; Zhao, N.; Zhang, G.; Yao, Z.; et al. Neonatal thyroid function born to mothers living with long-term excessive iodine intake from drinking water. Clin. Endocrinol. 2015, 83, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Sang, Z.; Wei, W.; Zhao, N.; Zhang, G.; Chen, W.; Liu, H.; Shen, J.; Liu, J.; Yan, Y.; Zhang, W. Thyroid dysfunction during late gestation is associated with excessive iodine intake in pregnant women. J. Clin. Endocrinol. Metab. 2012, 97, E1363–E1369. [Google Scholar] [CrossRef]
- Velasco, I.; Bath, S.C.; Rayman, M.P. Iodine as Essential Nutrient during the First 1000 Days of Life. Nutrients 2018, 10, 290. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programs Managers, 3rd ed.; World Health Organization: Geneva, Switzerland, 2007.
- European Food Safety Authority. Tolerable Upper Intake Levels for Vitamins and Minerals; EFSA: Parma, Italy, 2006. [Google Scholar]
- The Scientififc Advisory Committee on Nutrition. Sacn Statement on Iodine and Health; SACN: London, UK, 2014. [Google Scholar]
- Farebrother, J.; Zimmermann, M.B.; Andersson, M. Excess iodine intake: Sources, assessment, and effects on thyroid function. Ann. N. Y. Acad. Sci. 2019, 1446, 44–65. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Nutrient Reference Values for Australia and New Zealand: Including Recommended Dietary Intakes; NHMRC: Canberra, ACT, Australia, 2006. [Google Scholar]
- Medicine, I.O. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc; The National Academies Press: Washington, DC, USA, 2001; p. 800. [Google Scholar]
- Sasaki, S.; Shibata, K.; Tabata, I.; Nakamura, T.; Morita, A.; Yoshiike, N. Overview of the Dietary Reference Intakes for Japanese; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2020.
- Society, C.N. Chinese Dietary Reference Intakes Handbook (2013); Science Press: Beijing, China, 2014. [Google Scholar]
- Jahreis, G.; Hausmann, W.; Kiessling, G.; Franke, K.; Leiterer, M. Bioavailability of iodine from normal diets rich in dairy products--results of balance studies in women. Exp. Clin. Endocrinol. Diabetes 2001, 109, 163–167. [Google Scholar] [CrossRef]
- Brunn, J.; Block, U.; Ruf, G.; Bos, I.; Kunze, W.P.; Scriba, P.C. Volumetric analysis of thyroid lobes by real-time ultrasound (author’s transl). Dtsch. Med. Wochenschr. 1981, 106, 1338–1340. [Google Scholar] [CrossRef] [PubMed]
- Alexander, E.K.; Pearce, E.N.; Brent, G.A.; Brown, R.S.; Chen, H.; Dosiou, C.; Grobman, W.A.; Laurberg, P.; Lazarus, J.H.; Mandel, S.J.; et al. 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 2017, 27, 315–389. [Google Scholar] [CrossRef]
- Wolff, J.; Chaikoff, I.L. Plasma inorganic iodide as a homeostatic regulator of thyroid function. J. Biol. Chem. 1948, 174, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Connelly, K.J.; Boston, B.A.; Pearce, E.N.; Sesser, D.; Snyder, D.; Braverman, L.E.; Pino, S.; LaFranchi, S.H. Congenital hypothyroidism caused by excess prenatal maternal iodine ingestion. J. Pediatr. 2012, 161, 760–762. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Teng, W.P.; Li, J.X.; Wang, W.W.; Shan, Z.Y. Effects of maternal subclinical hypothyroidism on obstetrical outcomes during early pregnancy. J. Endocrinol. Investig. 2012, 35, 322–325. [Google Scholar]
- Haddow, J.E.; Palomaki, G.E.; Allan, W.C.; Williams, J.R.; Knight, G.J.; Gagnon, J.; O’Heir, C.E.; Mitchell, M.L.; Hermos, R.J.; Waisbren, S.E.; et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N. Engl. J. Med. 1999, 341, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Li, Q.; Cui, W.; Wang, X.; Gao, Q.; Zhong, C.; Sun, G.; Chen, X.; Xiong, G.; Yang, X.; et al. Maternal Iodine Insufficiency and Excess Are Associated with Adverse Effects on Fetal Growth: A Prospective Cohort Study in Wuhan, China. J. Nutr. 2018, 148, 1814–1820. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.J.; Condo, D.; Ryan, P.; Skeaff, S.A.; Howell, S.; Anderson, P.J.; McPhee, A.J.; Makrides, M. Association Between Maternal Iodine Intake in Pregnancy and Childhood Neurodevelopment at Age 18 Months. Am. J. Epidemiol. 2019, 188, 332–338. [Google Scholar] [CrossRef]
- Institute of Medicine. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids; The National Academies Press: Washington, DC, USA, 2000. [Google Scholar]
- Bartalena, L.; Bogazzi, F.; Braverman, L.E.; Martino, E. Effects of amiodarone administration during pregnancy on neonatal thyroid function and subsequent neurodevelopment. J. Endocrinol. Investig. 2001, 24, 116–130. [Google Scholar] [CrossRef]
- Zimmermann, M.B.; Andersson, M. Assessment of iodine nutrition in populations: Past, present, and future. Nutr. Rev. 2012, 70, 553–570. [Google Scholar] [CrossRef]
- Konig, F.; Andersson, M.; Hotz, K.; Aeberli, I.; Zimmermann, M.B. Ten repeat collections for urinary iodine from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women. J. Nutr. 2011, 141, 2049–2054. [Google Scholar] [CrossRef]
- Luo, J.; Li, C.; Zhang, X.; Shan, Z.; Teng, W. Reference Intervals of the Ratio of Urine Iodine to Creatinine in Pregnant Women in an Iodine-Replete Area of China. Biol. Trace Elem. Res. 2021, 199, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhu, X.; Shen, J.; Zhang, W. Selective solid-phase extraction of catecholamines from plasma using nanofibers doped with crown ether and their quantitation by HPLC with electrochemical detection. Anal. Bioanal. Chem. 2016, 408, 4987–4994. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhang, Y.; Hao, Y.; Wang, W.; Tan, L.; Bian, J.; Pearce, E.N.; Zimmermann, M.B.; Shen, J.; Zhang, W. Adverse effects on thyroid of Chinese children exposed to long-term iodine excess: Optimal and safe Tolerable Upper Intake Levels of iodine for 7- to 14-y-old children. Am. J. Clin. Nutr. 2018, 107, 780–788. [Google Scholar] [CrossRef] [PubMed]
- Perrine, C.G.; Cogswell, M.E.; Swanson, C.A.; Sullivan, K.M.; Chen, T.C.; Carriquiry, A.L.; Dodd, K.W.; Caldwell, K.L.; Wang, C.Y. Comparison of population iodine estimates from 24-hour urine and timed-spot urine samples. Thyroid 2014, 24, 748–757. [Google Scholar] [CrossRef] [PubMed]
- Secretariat, W.H.O.; Andersson, M.; de Benoist, B.; Delange, F.; Zupan, J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: Conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007, 10, 1606–1611. [Google Scholar] [CrossRef]
- Shi, X.; Han, C.; Li, C.; Mao, J.; Wang, W.; Xie, X.; Li, C.; Xu, B.; Meng, T.; Du, J.; et al. Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: A cross-sectional study of 7190 pregnant women in China. J. Clin. Endocrinol. Metab. 2015, 100, 1630–1638. [Google Scholar] [CrossRef]
| Indicators | 1st Trimester | 2nd Trimester | 3rd Trimester |
|---|---|---|---|
| TSH | 0.03–4.51 mIU/L | 0.05–4.50 mIU/L | 0.47–4.54 mIU/L |
| FT4 | 11.8–21.00 pmol/L | 10.6–17.60 pmol/L | 9.2–16.70 pmol/L |
| Variables | 1st Trimester | 2nd Trimester | 3rd Trimester | Total | p |
|---|---|---|---|---|---|
| n | 80 | 449 | 215 | 744 | - |
| Age (years) | 29.6 ± 5.2 | 30.9 ± 5.6 | 30.1 ± 5.7 | 30.5 ± 5.6 | 0.049 a |
| BMI (kg/m2) | 23.4 ± 4.3 | 24.9 ± 4.0 | 27.2 ± 3.5 | 25.4 ± 4.1 | <0.001 a |
| UIC (μg/L) | 194 (100.8, 424.9) | 145.8 (82.6, 256.3) | 143.8 (90.5, 264.9) | 150.2 (87.6, 268) | 0.019 b |
| UIE (μg/day) | 240 (112.0, 491.5) | 197.8 (114.0, 358.0) | 207 (121.5, 426.1) | 204.2 (116.0, 387) | 0.143 b |
| Tvol (mL) | 9.2 (7.0, 10.4) | 8.8 (6.8, 11.5) | 8.8 (6.7, 10.9) | 8.8 (6.8, 11.1) | 0.492 b |
| TSH (mIU/L) | 1.5 (0.9, 2.2) | 1.5 (1.0, 2.1) | 1.7 (1.1, 2.4) | 1.6 (1.0, 2.2) | 0.026 b |
| FT4 (pmol/L) | 16.6 (15.1, 17.8) | 14.9 (13.4, 16.3) | 14.2 (13.1, 15.4) | 14.8 (13.5, 16.2) | <0.001 b |
| UIE, μg/day | Subclinical Hypothyroidism, n (%) | Hypothyroxinemia, n (%) | Thyroid Dysfunction, n (%) | Thyroid Nodules, n (%) |
|---|---|---|---|---|
| <150 | 9 (3.4) | 7 (2.6) | 16 (6.0) | 71 (27.5) |
| 150–250 | 3 (1.7) | 4 (2.2) | 7 (3.9) | 45 (25.4) |
| 250–350 | 4 (4.6) | 1 (1.1) | 5 (5.7) | 21 (25.0) |
| 350–450 | 2 (3.6) | 1 (1.8) | 3 (5.5) | 20 (37.7) |
| 450–550 | 3 (8.8) | 4 (11.8) | 7 (20.6) | 6 (19.4) |
| ≥550 | 10 (8.3) | 6 (5.0) | 16 (13.2) | 31 (26.5) |
| total | 31 (4.2) | 23 (3.1) | 54 (7.3) | 194 (26.9) |
| p | 0.068 | 0.035 | 0.001 | 0.484 |
| EII, μg/day | Subclinical Hypothyroidism, n (%) | Hypothyroxinemia, n (%) | Thyroid Dysfunction, n (%) | Thyroid Nodules, n (%) |
|---|---|---|---|---|
| <100 | 4 (3.6) | 4 (3.6) | 8 (7.1) | 30 (28.6) |
| 100–200 | 5 (2.2) | 4 (1.8) | 9 (4.0) | 59 (26.3) |
| 200–300 | 4 (3) | 3 (2.3) | 7 (5.3) | 35 (27.1) |
| 300–400 | 3 (4.2) | 2 (2.8) | 5 (6.9) | 17 (23.9) |
| 400–500 | 2 (4.2) | 1 (2.1) | 3 (6.3) | 17 (37.8) |
| 500–600 | 3 (9.1) | 3 (9.1) | 6 (18.2) | 6 (20.0) |
| ≥600 | 10 (8.3) | 6 (5.0) | 16 (13.3) | 30 (25.9) |
| total | 31 (4.2) | 23 (3.1) | 54 (7.3) | 194 (26.9) |
| p | 0.128 | 0.292 | 0.01 | 0.677 |
| Groups | Unadjusted | Adjusted * | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Model 1: UIE (μg/day) | ||||
| <150 | 1.6 | 0.6–3.9 | 1.7 | 0.7–4.6 |
| 150–250 | Ref | - | Ref | - |
| 250–350 | 1.5 | 0.5–4.9 | 1.4 | 0.4–5.0 |
| 350–450 | 1.4 | 0.4–5.7 | 1.7 | 0.4–7.0 |
| 450–550 | 6.4 | 2.1–19.7 | 5.7 | 1.7–19.2 |
| ≥550 | 3.8 | 1.5–9.5 | 3.9 | 1.5–10.3 |
| Model 2: EII (μg/day) | ||||
| <100 | 1.9 | 0.7–5.0 | 2.0 | 0.7–5.6 |
| 100–200 | Ref | - | Ref | - |
| 200–300 | 1.4 | 0.5–3.7 | 1.3 | 0.4–3.8 |
| 300–400 | 1.8 | 0.6–5.6 | 1.5 | 0.4–5.2 |
| 400–500 | 1.6 | 0.4–6.2 | 1.9 | 0.5–7.3 |
| 500–600 | 5.4 | 1.8–16.3 | 4.3 | 1.3–14.4 |
| ≥600 | 3.7 | 1.6–8.7 | 3.6 | 1.5–8.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, W.; Guo, W.; Zhang, N.; Gao, M.; Zhang, K.; Pearce, E.N.; Li, S.; Ren, Z.; Yang, Y.; Wang, C.; et al. Adverse Effects on the Thyroid of Chinese Pregnant Women Exposed to Long-Term Iodine Excess: Optimal and Safe Tolerable Upper Intake Levels of Iodine. Nutrients 2023, 15, 1635. https://doi.org/10.3390/nu15071635
Wu W, Guo W, Zhang N, Gao M, Zhang K, Pearce EN, Li S, Ren Z, Yang Y, Wang C, et al. Adverse Effects on the Thyroid of Chinese Pregnant Women Exposed to Long-Term Iodine Excess: Optimal and Safe Tolerable Upper Intake Levels of Iodine. Nutrients. 2023; 15(7):1635. https://doi.org/10.3390/nu15071635
Chicago/Turabian StyleWu, Wen, Wenxing Guo, Naifan Zhang, Min Gao, Kexin Zhang, Elizabeth N. Pearce, Shaohan Li, Zhiyuan Ren, Ying Yang, Chunxi Wang, and et al. 2023. "Adverse Effects on the Thyroid of Chinese Pregnant Women Exposed to Long-Term Iodine Excess: Optimal and Safe Tolerable Upper Intake Levels of Iodine" Nutrients 15, no. 7: 1635. https://doi.org/10.3390/nu15071635
APA StyleWu, W., Guo, W., Zhang, N., Gao, M., Zhang, K., Pearce, E. N., Li, S., Ren, Z., Yang, Y., Wang, C., & Zhang, W. (2023). Adverse Effects on the Thyroid of Chinese Pregnant Women Exposed to Long-Term Iodine Excess: Optimal and Safe Tolerable Upper Intake Levels of Iodine. Nutrients, 15(7), 1635. https://doi.org/10.3390/nu15071635







