Abstract
Excessive inflammatory response has been implicated in severe respiratory forms of coronavirus disease 2019 (COVID-19). Trace elements such as zinc, selenium, and copper are known to modulate inflammation and immunity. This study aimed to assess the relationships between antioxidant vitamins and mineral trace elements levels as well as COVID-19 severity in older adults hospitalized. In this observational retrospective cohort study, the levels of zinc, selenium, copper, vitamin A, β-carotene, and vitamin E were measured in 94 patients within the first 15 days of hospitalization. The outcomes were in-hospital mortality secondary to COVID-19 or severe COVID-19. A logistic regression analysis was conducted to test whether the levels of vitamins and minerals were independently associated with severity. In this cohort (average age of 78 years), severe forms (46%) were associated with lower zinc (p = 0.012) and β-carotene (p < 0.001) concentrations, and in-hospital mortality (15%) was associated with lower zinc (p = 0.009), selenium (p = 0.014), vitamin A (p = 0.001), and β-carotene (p = 0.002) concentrations. In regression analysis, severe forms remained independently associated with lower zinc (aOR 2.13, p = 0.018) concentrations, and death was associated with lower vitamin A (aOR = 0.165, p = 0.021) concentrations. Low plasma concentrations of zinc and vitamin A were associated with poor prognosis in older people hospitalized with COVID-19.
1. Introduction
The rapid spread across the world of a new coronavirus from the first quarter of 2020 has overwhelmed many healthcare systems, even in developed countries. This virus, transmitted largely by respiratory droplets and to a lesser extent by mucosal contact, named SARS-CoV-2 (severe acute respiratory syndrome coronavirus-2) because of the frequency of its severe respiratory forms, can also lead to digestive (anorexia, diarrhea…), vascular (heart attack…) and neurological (stroke, delirium…) symptoms []. These forms leading to acute respiratory distress syndrome requiring high-flow oxygen therapy or mechanical ventilation were associated with major mortality in the absence of specific treatment during the first wave of the disease, between March and June 2020 in Europe []. Thus, in 2020, coronavirus disease 2019 (COVID-19) has become the third leading cause of death behind cardiovascular pathologies and cancers in many countries such as in the United States or in France [,]. Age over 65 years, male gender, and comorbidities are major risk factors for severe forms and death during COVID-19 infection [,].
The susceptibility of the elderly to severe forms of COVID-19 was demonstrated from the beginning of the pandemic and relies notably on the presence of pathologies such as diabetes, hypertension, or obesity []. The particular criticality of COVID-19 in the elderly also implies immuno-senescence, which is a progressive process favored by comorbidities and certain nutritional deficits, leading both to a reduction in responses to new pathogens and also to excessive inflammatory responses [,]. Thus, cytokine storm, an uncontrolled secretion of chemokines and pro-inflammatory cytokines, can lead to multiple organ failure particularly respiratory with acute respiratory distress syndrome (ARDS), and it was recognized as the leading cause of death during the first wave of COVID [,]. Moreover, every stage of the immune response, both humoral and cellular, is dependent on nutritional factors []. Beyond protein-energy malnutrition, levels of various micronutrients are associated with the immune response in the event of COVID-19 [,]. Thus, micronutrients with antioxidant properties such as the metal and trace elements (zinc, iron, selenium and copper) and vitamins A, C, E, D, B (B6, B9, B12) and C are known to support adequate immune response [,]. For example, vitamin A contributes to the protection of mucosal and epithelium integrity, and it has regulatory functions on humoral and cellular immune responses, while zinc is a major factor in the growth, development, and maintenance of immune responses, especially against viral infections such as COVID-1- [,,]. At the same time, insufficient intake and altered status of these nutrients concern a large proportion of the Western population, in particular the elderly []. In the absence of a vaccine or specific treatment during the first wave, certain anti-oxidant micronutrients were thus quickly proposed to optimize immunity against COVID-19 [].
However, apart from vitamin D, studies involving the associations between plasma antioxidant or mineral micronutrients levels and the clinical outcomes of COVID-19 infection are still scarce [,]. We conducted a retrospective cohort study during the first wave of the pandemic to document the possible relationship between antioxidant levels and COVID-19 severity in older adults over 50 years hospitalized for COVID-19. The objectives of our study were (i) to identify associations between plasma minerals and antioxidant micronutrients levels at hospital admission and COVID-19 severe forms defined by the presence of one of the following criteria: high oxygen requirement, intubation, or death; and death related to COVID-19 during the hospital stay, (ii) to identify associations between plasma minerals and antioxidant micronutrients levels and age or inflammation level measured by C-reactive protein (CRP).
2. Materials and Methods
2.1. Study Design and Population Characteristics
The present study was a sub-study of the observational study “MicroCovAging” (micronutrients status in aging patients with COVID-19) conducted at the Hospices Civils de Lyon (HCL), in Lyon, France, and it focused on the potential link between plasma antioxidant micronutrients levels and COVID-19 severity. Micronutrients analysis was conducted on frozen tube bottoms (plasma heparinized samples) coming from routine sampling during COVID-19 patient hospitalizations, thanks to the COVID-19 biobank hosted at HCL Biological Resource Centre. Thus, the micronutrient assays as well as the routine assays (albumin, CRP in particular) were carried out on the same day.
Two hundred and thirty patients aged ≥50 years and hospitalized for active SARS-CoV-2 infection proven by Real-Time Polymerase Chain Reaction (RT-PCR) in the Lyon public hospitals were consecutively included during the first wave of the pandemic (admission date from 1 March 2020 to 30 June 2020). The patients were therefore affected by the Wuhan-Hu-1 strain of the SARS-CoV-2 and had not been exposed to any specific vaccine. Two patients were excluded from the data analysis due to a withdrawal of consent (see flow chart in Figure 1).
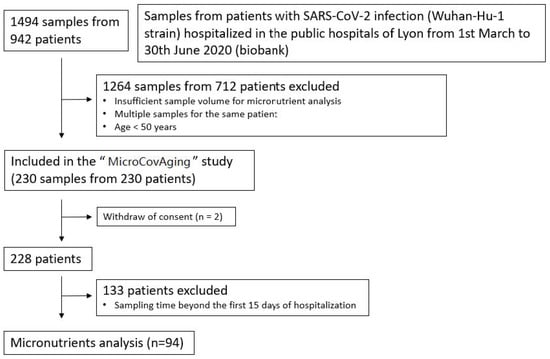
Figure 1.
Flow chart of the patients included in the study.
2.2. Ethical Consideration
The study was approved by the scientific and ethical committee of the HCL and was reported on the clinicaltrials.gov website (NCT04877509). Medical doctors informed patients of the study during hospitalization or by post, thanks to a generic information sheet dedicated to COVID-19 research at the HCL. All patients received an information note accompanied by a non-objection form and had one month to express their opposition. The processing of personal data carried out for this study falls within the scope of “Reference Methodology No. 4” (MR-004) of the Commission Nationale de l’Informatique et des Libertés (CNIL).
2.3. Data Collection
The NOSO-COR project, a prospective anonymous inpatient COVID-19 database also carried by the HCL, gave us access to patient demographics, clinical features and treatments []. Biochemical biomarkers (CRP, albumin, vitamin D) were obtained by routine testing during hospitalization.
2.4. Micronutrients Levels
Among plasma micronutrients, 6 were selected with regard to their potential importance based on knowledge from previous pathophysiological studies: minerals zinc, selenium, copper; and vitamins A, β-carotene, and E [,,,,]. Only assays of the 94 patients whose samples have been collected during the first 15 days of hospitalization were considered for the analysis of the associations between plasma antioxidant or mineral micronutrients levels at hospital admission and COVID-19 severe forms and death. We have chosen to focus on the first 15 days of hospitalization in order to limit the biases linked on the one hand to phenomena of hyper-consumption possibly linked to the severity and duration of the disease and on the other hand to possible supplements after this period. Regarding the secondary objective (associations between plasma antioxidant micronutrients levels and age or inflammation level measured by CRP levels), the analyses were first carried out on the 94 patients and then extended to the population of 228 patients.
Levels of selenium were determined by Inductively Coupled Plasma–Mass Spectrometry (ICP–MS) on an Elan DRCe instrument (PerkinElmer) in Dynamic Reaction Cell (DRC) mode using oxygen as the reaction gas and with 78Se as the isotope of choice. The internal standard was rhodium. Inductively Coupled Plasma–Optical Emission Spectrometry (ICP–OES) (5110 instrument, Agilent, Santa Clara, CA, USA) was used to determine the levels of plasma copper and zinc. The emission wavelengths were 213.857 nm and 327.395 nm, respectively.
Vitamin A, vitamin E and β-carotene concentrations were measured by high-performance liquid chromatography coupled to spectrophotometric detection with an H-Class Waters chromatographic system (Waters, St Quentin-en-Yvelines, France). Before analysis by chromatography, vitamin A, vitamin E, and β-carotene were extracted from plasma heparinized samples conserved at <−18 °C. Briefly, for the extraction, plasma was mixed during 10 min with internal standard and ethanol and then during 30 min with water and hexane. After centrifugation during 10 min at 5300× g, the upper organic layer was evaporated under nitrogen flux. Dry residue was dissolved in methanol/ethanol mix (85/15, v/v) and injected in the chromatographic system. Separation was performed on a kinetex 2.6 µ polar C18 (Phenomenex, Le Pecq, France) using a gradient elution with acetonitrile/methanol/isopropanol (78/20/2, v/v/v) as solvent A and acetonitrile/methanol/isopropanol (40/40/20, v/v/v) as solvent B for a total run of 13 min. The gradient was as follows: 0 min (100% A and 0% B), 2 min (0% A and 100% B), and 8.5 min (100% A and 0% B) with a constant flow of 0.2 mL/min. The wavelengths used for vitamin A, vitamin E, and β-carotene determination were 325 nm, 292 nm and 450 nm, respectively. Quantification was performed by using Empower3_HF1_Enterprise software (version 7.30.00.00, Waters). The laboratory regularly participates in external audits attesting to the reliability of the measurements of trace elements and vitamins.
2.5. Study Clinical Endpoints of COVID-19 Disease Severity
The clinical endpoints of the study were: (i) the in-hospital mortality directly related to COVID-19 and (ii) the onset of severe forms of COVID-19. Two independent physicians carried out the assignment of causes of death via a medical evaluation. The severe forms of COVID-19 were defined as any of the following criteria: high oxygen requirement (i.e., oxygen flow > 5 L/min), intubation, or death related to COVID-19 during the hospital stay. ICU admissions as such were not included as a severe form criterion because older patients were frequently ineligible for ICU admission (age over 80 years, or Rockwood Clinical Frailty scale greater than 5, or patient refusal of an ICU transfer) [].
2.6. Statistical Analysis
Since the quantitative variables distribution significantly deviated from a normal distribution (p < 0.001) (except for body mass index (BMI) and albumin), we expressed results as medians and interquartile ranges (IQR) and used a non-parametric test for all comparisons (Mann–Whitney U-test). The test used for data distribution to test for normality was the Kolmogorov–Smirnov test. Logistic regression models were performed to separately explain each clinical endpoint (death or severe forms) according to a series of variables considered in the literature as risk factors for a severe form of COVID-19 (age, BMI, gender, CRP and albumin). Thus, logistic regression analysis took into account: age (≤75 vs. >70 years old), gender, BMI (<35 kg/m2/≥35 kg/m2), CRP and albumin levels. As we have previously shown within the same cohort that vitamin D supplementation taken during the 3 months preceding the infection onset may have a protective effect on the development of severe COVID-19 forms in older adults, pre-hospital vitamin D supplementation (yes/no) was also considered []. For continuous covariates, the results of the logistic regression analysis are traditionally presented as the odds ratio reflecting the increase in risk of an event occurring for a one unit increase in the continuous variable. To improve clinical relevance and facilitate interpretation, depending on the micronutrient studied, we calculated the OR for a more clinically relevant increase or decrease than one unit. Thus, the legend of the table shows for which variation of the dosage the odds ratio has been calculated. All tests were two-tailed, and the significance level was defined when p value < 0.05. Statistical analyses were performed using SAS 9.4 software (2013, SAS Institute Inc., Cary, NC, USA).
3. Results
3.1. Patient Demographics and Comorbidities
Table 1 shows the baseline characteristics of the 228 enrolled patients hospitalized with SARS-CoV-2 infection confirmed by RT-PCR. The median age was 78 years (IQR, 68–87), with a male predominance (56%). Twenty-five percent of patients lived in an institution before their hospitalization. Multiple comorbidities were present in 63% of the patients: 56% had arterial hypertension, 36% had other cardiovascular diseases, 32% had diabetes mellitus (types 1 and 2), 19% had neuro-cognitive disorders, 14% had renal diseases, 13% had pulmonary diseases, 12% had cancer and 7% had a BMI greater than 35 kg/m2.

Table 1.
Baseline demographics, comorbidities, biomarkers, and clinical outcomes of the 228 patients, including the 94 patients with micronutrients analysis collected during the first 15 days of hospitalization.
The full enrolled population in the “MicroCovAging” study has similar characteristics to those of the sub-population of patients (n = 94) whose samples for micronutrients analysis have been collected during the first 15 days (median: 8 days; IQR: 5–12 days) of hospitalization (Fisher’s exact tests non-significant).
3.2. Clinical Outcomes
Among the 228 patients, 105 (46%) developed a severe form of COVID-19, 84 (37%) were admitted to the ICU and 35 (15%) deaths related to COVID-19 occurred during hospitalization (Table 1). Sixteen deceased patients (16/35) died before ICU admission or were ineligible for ICU admission.
Age of 70 years and over was associated with COVID-19 mortality (91% vs. 72%, p = 0.004). Male patients were overrepresented among severe forms of COVID-19 (sex ratio = 2.2, p < 0.001), admission to ICU (sex ratio = 2.5, p < 0.001) and COVID-19 mortality (sex ratio = 4.0, p = 0.003). Patients with grade 2 and 3 obesity (BMI ≥ 35 kg/m2) were overrepresented in severe forms (12% vs. 3%, p = 0.02).
3.3. Association between Plasma Antioxidant and Mineral Micronutrients Levels and Clinical Outcomes
Among the 94 patients with micronutrients analysis collected during the first 15 days of hospitalization, severe forms were associated with lower zinc (0.55 vs. 0.66 mg/L, p = 0.012), β-carotene (0.28 vs. 0.42 µmol/L, p < 0.001) concentrations; and death with lower zinc (0.51 vs. 0.62 mg/L; p = 0.009), selenium (53 vs. 65 µg/L, p = 0.014), vitamin A (0.79 vs. 1.38 µmol/L, p = 0.001), β-carotene (0.24 vs. 0.37 µmol/L, p = 0.002), and vitamin E concentrations (23 vs. 27 µmol/L, p = 0.047) (Table 2 and Table 3).

Table 2.
Plasma antioxidant micronutrients levels and COVID-19 severity among the 94 patients with micronutrients analysis collected during the first 15 days of hospitalization.

Table 3.
Univariate logistic regression analysis of the association between plasma micronutrients levels and COVID-19-related deaths and severe forms in the 94 patients.
In multivariate analysis, severe forms remained independently associated with lower zinc (aOR 2.13, p = 0.018) concentrations; death was associated with lower vitamin A (aOR = 0.165, p = 0.021) concentrations (Table 4). Whatever the micronutrient considered, the increase in albumin was accompanied by a reduction in the risk of a severe form without a significant effect of age or BMI (see Supplementary Materials). However, age > 75 years and BMI ≥ 35 kg/m2 were the factors regularly associated with mortality.

Table 4.
Multivariate logistic regression analysis of the association between plasma micronutrients levels and COVID-19-related deaths and severe forms (adjusted on age, sex, CRP, albumin, BMI and vitamin D supplementation) in the 94 patients.
3.4. Association between Plasma Antioxidant Micronutrients Levels and CRP Levels or Age
Among the 94 patients, a significant negative relationship was observed with CRP for zinc (r = −0.591, p < 0.001), selenium (r = −0.357, p = 0.002), vitamin A (r = −0.561, p < 0.001), β-carotene (r = −0.397, p < 0.001), and vitamin E (r = −0.245, p = 0.019); conversely, a positive relationship was observed for copper (r = 0.362, p < 0.001). Increasing age was associated with lower zinc (r = −0.234, p = 0.023) and selenium (r = −0.281, p = 0.014), but it was non-significant with vitamin A, vitamin E and β-carotene concentrations. These results were similar to those obtained by extending the analysis to the total population of 228 patients: a significant negative relationship was observed with CRP for zinc (r = −0.338, p < 0.001), selenium (r = −0.352, p < 0.0001), vitamin A (r = −0.543, p < 0.001), β-carotene (r = −0.421, p < 0.001), and vitamin E (r = −0.173, p = 0.01); conversely, a positive relationship was observed for copper (r= 0.368, p < 0.001). Increasing age was associated with lower zinc (r = −0.234, p = 0.023), selenium (r = −0.302, p < 0.001), vitamin A (r = 0.217, p < 0.001), and vitamin E (p = −0.193, p = 0.003) but higher β-carotene (r = 0.194, p = 0.03) concentrations.
4. Discussion
In this observational study, we have shown an association between low plasma zinc level (measured within 15 days of admission) and the risk of severe form as well as an association between low plasma level of vitamin A and mortality related to COVID-19 independently of well-recognized risk factors such as age, sex or obesity. In addition, age above 70 was associated with lower plasma levels of zinc, selenium, vitamin A and vitamin E. Finally, plasma zinc, selenium, vitamin A, β-carotene and vitamin A levels were inversely proportional to CRP levels.
Our results are consistent with those of the literature concerning a link between prognosis in respiratory infections and plasma levels of certain micronutrients, vitamin A and zinc being frequently cited. In a representative population of 34,000 participants, lower plasma levels of vitamins A, C, D, and α-tocopherol vitamin E were associated with increased respiratory morbidity and/or mortality in U.S. adults []. In a 9-year longitudinal study, low levels of selenium were associated with shorter survival in the elderly []. Low plasma levels of zinc and vitamin A have been associated with poor prognosis in COVID-19 with an increased risk of ICU admission, longer disease duration or higher mortality [,,]. In a population of 34 patients hospitalized for COVID-19, a deficiency in selenium, vitamin D, vitamin A, and zinc was present in 51%, 40%, 39%, and 39%, respectively []. Moreover, a lower risk for severe COVID-19 was associated with higher levels of vitamin A (aOR 0.18, 95% CI 0.05–0.69, p = 0.01), zinc (aOR 0.73, 95% CI 0.55–0.98, p = 0.03), and folic acid (aOR 0.88, 95% CI 0.78–0.98, p = 0.02). Low zinc levels (<0.5 mg/L) at admission have been associated with more severe clinical presentation and higher mortality in SARS-CoV-2 Infection []. Selenium deficiency seems particularly frequent in patients hospitalized for COVID-19, which can concern up to 42% of them []. In another cohort of COVID-19, non-survivors were characterized by an overrepresentation of a simultaneous zinc and selenium transporter selenoprotein p (SELENOP) deficiency []. A Spanish observational study found that patients with low levels of zinc or vitamin A more often required ICU admission during the first wave of the pandemic and that low levels of vitamin A were associated with the risk of orotracheal intubation []. However, the results are divergent, and some studies have not found a link between selenium and survival during COVID-19 [].
One major hypothesis may be that micronutrients deficiency results in altered immune responses and thus in an impaired secretion of cytokines and antibody response leading to impaired defenses against viral infections []. Low selenium status has been also associated with poor musculoskeletal function, which can promote respiratory dysfunction []. Zinc is a cofactor of >300 enzymes and plays a critical role in both innate and adaptive immune responses []. Zinc deficiency may also trigger elevating inflammatory response by promoting aberrant immune cell activation []. Vitamin A plays a regulatory role in both innate and adaptive (cellular and humoral) immunity []. Indirectly, micronutrient deficiencies can also promote bacterial superinfections (respiratory but also urinary), which are frequently observed during hospitalization for COVID-19, and they may aggravate respiratory damages or increase mortality [].
Among patients admitted to an ICU for COVID-19, there was 20% of the over 70-year-olds and only 5% of the over 80-year-olds. This underrepresentation of the elderly in the ICU fundamentally differs from the profile of patients hospitalized with COVID-19 and reflects the exclusion from the ICU of the oldest and comorbid patients favored by insufficient ICU capacities during the first wave as well as by their ability to recover [].
In our study, age over 70 was associated with lower micronutrient levels, which is consistent with the literature. In a systematic review in 2020, Vural et al. found significant proportions (25 to 50%) of populations either community-based or institutionalized, showing insufficiency for zinc, selenium, iron, iodine and copper []. Insufficient intake related to both quantitative and qualitative alteration of the diet in the older population may promote low levels of micronutrients together with protein-energy malnutrition in this population []. The fact that zinc and vitamin A remain factors independently associated with severe forms and mortality in our study, even after adjustment for albuminemia, shows that the dosage of certain micronutrients could also provide additional prognostic information to protein-energetic malnutrition.
Our results have shown an inverse correlation between the level of inflammation measured by CRP and the plasma level of most micronutrients. This relationship can be explained in both directions: either by an excess of consumption in case of a severe inflammatory response or by a pre-existing deficit influencing the inflammatory response. In a prospective study of critically ill adults, Koekkoek et al. have shown that 24 ICU patients presented with lower plasma levels of selenium, β-carotene, vitamin C, and vitamin E than 21 age-matched healthy controls []. Moreover, immune dysfunction and systemic inflammation can be promoted by zinc deficiency []. The low level of micronutrients such selenium or zinc, observed in COVID-19 populations compared to control populations, does not necessarily imply pre-existing deficiencies favoring the occurrence of the disease [,]. As has been shown in the treatment of certain cancers, it is also possible that COVID-19 itself leads to an alteration in micronutrient status []. For example, the combination of hypoxia and IL-6 suppresses selenoprotein expression (such as glutathione peroxidase), causing whole-body selenium status decline and an increased generation of reactive oxygen species []. More generally, redistribution, altered protein binding, increased losses (through urine, blood, sweat, ascites, pleural fluid), increased metabolic use, and dilution secondary to fluid resuscitation may explain low micronutrient levels in ICU []. More likely, the low levels of micronutrients observed in critically ill patients could be the result of a variable combination of pre-existing deficiencies, disease-related or treatment-related perturbations [].
This study also raises the issue of supplementation. Interventions based on micronutrient supplementation in the general population have so far shown unconvincing effects. Some reviews plead for supplementation with micronutrients as a safe, effective, and low-cost strategy to help support optimal immune function, especially against acute respiratory tract infections [,]. These outcomes differ from other studies where the supplementation of ICU patients (mostly sepsis or ARDS) with antioxidant micronutrients demonstrate neutral outcomes and even harm []. The support in micronutrients goes above all through a balanced diet with regular intake of fruits and vegetables and complete cereals even also for some of them by supplements (such as vitamin D) [,]. Selenium and zinc supplementation may improve immune response in critically ill patients with acute respiratory distress syndrome related to COVID-19 []. Interestingly, in a recent meta-analysis, zinc supplementation in COVID-19 appeared to be associated with a trend toward reduced mortality (RR 0.79, 95% CI 0.60–1.03, p = 0.08) [].
Limitations and Strengths of the Study
Our study has some limitations. First, the level of evidence of our study is limited by its observational retrospective nature, but the brutal occurrence of the pandemic did not give us the possibility of adopting a more demanding design. Secondly, we only demonstrated a significant and independent association with the prognosis for two of the six micronutrients considered, which may be partly linked to low power related to the limited number of patients, but reinforces the relevance of the results obtained. The design of the study and the limited clinical data collected did not allow us to analyze other factors such as secondary infections or organ decompensation (cardiac, renal, etc.), which can themselves be the cause of an excess of morbidity or mortality and potentially affect micronutrient or CRP levels []. Moreover, some patients, especially those treated in the ICU, could have been supplemented with micronutrients, although there were no recommendations at that time. The retrospective design inherent to the sudden onset of the first wave of the COVID-19 epidemic did not allow us to collect this information in an exhaustive manner. Nevertheless, the doses used always correspond to the recommended daily doses and were therefore unlikely to affect plasma levels in such a short time.
However, this study has several strengths. This is one of the few studies to focus on the impact of micronutrients on the prognosis of COVID-19 disease, while most of the studies have essentially considered protein-energy malnutrition. In addition, this study included older to very old populations and therefore, it is particularly representative of the populations affected by severe forms of COVID-19. Moreover, the richness of the data collected allowed us to identify an association between various micronutrients and prognosis, which is truly independent of many confounding factors such as age, sex, albumin or obesity.
5. Conclusions
Low plasma concentrations of zinc and vitamin A were associated with poor prognosis in elderly people hospitalized with COVID-19 during the first wave of the pandemic. These results, in agreement with other observational studies in the literature, emphasize that the nutritional challenges of COVID-19 involve both micro and macronutrient issues. The simultaneous analysis of a panel of micronutrients reinforces the interest of our study.
Although literature data remain rare concerning the elderly population and insufficient to distinguish between insufficient intake and increased consumption in the acute phase, these results may plead for the specific supplementation of elderly patients in order to strengthen their anti-viral defenses, limit cytokine storm and improve prognosis.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15061516/s1, Table S1: Logistic regression analysis of association between the 41 severe COVID-19 and serum antioxidant micronutrients levels.
Author Contributions
Conceptualization, F.P., K.G., C.C., E.B., M.B. (Muriel Bost) and M.B. (Marc Bonnefoy); methodology, M.S.-E., F.P., C.C., E.B., M.B. (Muriel Bost) and M.B. (Marc Bonnefoy); formal analysis, F.P. and J.H.; investigation, M.S.-E., F.P. and L.B.; resources, K.G., P.V. and L.H.; data curation, F.P.; writing—original draft preparation, F.P., C.L. and M.B. (Marc Bonnefoy); writing—review and editing, P.V., C.L., L.H. and T.G.; visualization, F.P. and C.L.; supervision, E.B., M.B. (Muriel Bost) and M.B. (Marc Bonnefoy); project administration, F.P.; funding acquisition, K.G., E.B., M.B. (Muriel Bost) and M.B. (Marc Bonnefoy). All authors have read and agreed to the published version of the manuscript.
Funding
This research received financial support from the Hospices Civils de Lyon (Lyon, France) within the framework of the Clinical Biology Department Call for Proposal (grant number NCT04877509) and the APC was funded by Hospices Civils de Lyon (Lyon, France).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the ethical committee of the Hospices Civils de Lyon (protocol code 21_5067, the 30 December 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical considerations, regarding personal information and respecting what was written in the generic information sheet dedicated to COVID-19 research at the Hospices Civils de Lyon (Lyon, France).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Salahshoori, I.; Mobaraki-Asl, N.; Seyfaee, A.; Mirzaei Nasirabad, N.; Dehghan, Z.; Faraji, M.; Ganjkhani, M.; Babapoor, A.; Shadmehr, S.Z.; Hamrang, A. Overview of COVID-19 Disease: Virology, Epidemiology, Prevention Diagnosis, Treatment, and Vaccines. Biologics 2021, 1, 2–40. [Google Scholar] [CrossRef]
- Lambermont, B.; Rousseau, A.-F.; Seidel, L.; Thys, M.; Cavalleri, J.; Delanaye, P.; Chase, J.G.; Gillet, P.; Misset, B. Outcome Improvement Between the First Two Waves of the Coronavirus Disease 2019 Pandemic in a Single Tertiary-Care Hospital in Belgium. Crit. Care Explor. 2021, 3, e0438. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.S.; Cheng, D.; Martin, J. Impact of COVID-19 on Excess Mortality, Life Expectancy, and Years of Life Lost in the United States. PLoS ONE 2021, 16, e0256835. [Google Scholar] [CrossRef] [PubMed]
- Demetriou, C.A.; Achilleos, S.; Quattrocchi, A.; Gabel, J.; Critselis, E.; Constantinou, C.; Nicolaou, N.; Ambrosio, G.; Bennett, C.M.; Le Meur, N.; et al. Impact of the COVID-19 Pandemic on Total, Sex- and Age-Specific All-Cause Mortality in 20 Countries Worldwide during 2020: Results from the C-MOR Project. Int. J. Epidemiol. 2022, dyac170. [Google Scholar] [CrossRef]
- Dessie, Z.G.; Zewotir, T. Mortality-Related Risk Factors of COVID-19: A Systematic Review and Meta-Analysis of 42 Studies and 423,117 Patients. BMC Infect. Dis. 2021, 21, 855. [Google Scholar] [CrossRef]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors Associated with COVID-19-Related Death Using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef]
- Fitero, A.; Bungau, S.G.; Tit, D.M.; Endres, L.; Khan, S.A.; Bungau, A.F.; Romanul, I.; Vesa, C.M.; Radu, A.-F.; Tarce, A.G.; et al. Comorbidities, Associated Diseases, and Risk Assessment in COVID-19—A Systematic Review. Int. J. Clin. Pract. 2022, 2022, e1571826. [Google Scholar] [CrossRef]
- Bajaj, V.; Gadi, N.; Spihlman, A.P.; Wu, S.C.; Choi, C.H.; Moulton, V.R. Aging, Immunity, and COVID-19: How Age Influences the Host Immune Response to Coronavirus Infections? Front. Physiol. 2021, 11, 571416. [Google Scholar] [CrossRef]
- Mueller, A.L.; McNamara, M.S.; Sinclair, D.A. Why Does COVID-19 Disproportionately Affect Older People? Aging 2020, 12, 9959–9981. [Google Scholar] [CrossRef]
- Cortes-Telles, A.; Gutiérrez-Solis, A.L.; Álvarez-Sánchez, V.A.; González-Garay, A.G.; Lugo, R.; Avila-Nava, A. Dynamic Inflammatory Response among Routine Laboratory Biomarkers and Their Predictive Ability for Mortality in Patients with Severe COVID-19. Front. Med. 2022, 9, 1047304. [Google Scholar] [CrossRef]
- Kabir, M.T.; Uddin, M.S.; Hossain, M.F.; Abdulhakim, J.A.; Alam, M.A.; Ashraf, G.M.; Bungau, S.G.; Bin-Jumah, M.N.; Abdel-Daim, M.M.; Aleya, L. NCOVID-19 Pandemic: From Molecular Pathogenesis to Potential Investigational Therapeutics. Front. Cell Dev. Biol. 2020, 8, 616. [Google Scholar] [CrossRef]
- Tourkochristou, E.; Triantos, C.; Mouzaki, A. The Influence of Nutritional Factors on Immunological Outcomes. Front. Immunol. 2021, 12, 665968. [Google Scholar] [CrossRef]
- Damayanthi, H.D.W.T.; Prabani, K.I.P. Nutritional Determinants and COVID-19 Outcomes of Older Patients with COVID-19: A Systematic Review. Arch. Gerontol. Geriatr. 2021, 95, 104411. [Google Scholar] [CrossRef]
- Richardson, D.P.; Lovegrove, J.A. Nutritional Status of Micronutrients as a Possible and Modifiable Risk Factor for COVID-19: A UK Perspective. Br. J. Nutr. 2021, 125, 678–684. [Google Scholar] [CrossRef]
- Munteanu, C.; Schwartz, B. The Relationship between Nutrition and the Immune System. Front. Nutr. 2022, 9, 1082500. [Google Scholar] [CrossRef]
- Gombart, A.F.; Pierre, A.; Maggini, S. A Review of Micronutrients and the Immune System–Working in Harmony to Reduce the Risk of Infection. Nutrients 2020, 12, 236. [Google Scholar] [CrossRef]
- Huang, Z.; Liu, Y.; Qi, G.; Brand, D.; Zheng, S.G. Role of Vitamin A in the Immune System. J. Clin. Med. 2018, 7, 258. [Google Scholar] [CrossRef]
- Read, S.A.; Obeid, S.; Ahlenstiel, C.; Ahlenstiel, G. The Role of Zinc in Antiviral Immunity. Adv. Nutr. 2019, 10, 696–710. [Google Scholar] [CrossRef]
- Renata, R.-B.N.; Arely, G.-R.A.; Gabriela, L.-M.A.; Esther, M.-L.M. Immunomodulatory Role of Microelements in COVID-19 Outcome: A Relationship with Nutritional Status. Biol. Trace Elem. Res. 2023, 201, 1596–1614. [Google Scholar] [CrossRef]
- Baudry, J.; Kopp, J.F.; Boeing, H.; Kipp, A.P.; Schwerdtle, T.; Schulze, M.B. Changes of Trace Element Status during Aging: Results of the EPIC-Potsdam Cohort Study. Eur. J. Nutr. 2020, 59, 3045–3058. [Google Scholar] [CrossRef]
- Kaur, I.; Behl, T.; Sehgal, A.; Singh, S.; Sharma, N.; Subramanian, V.; Fuloria, S.; Fuloria, N.K.; Sekar, M.; Dailah, H.G.; et al. A Motley of Possible Therapies of the COVID-19: Reminiscing the Origin of the Pandemic. Environ. Sci. Pollut. Res. 2022, 29, 67685–67703. [Google Scholar] [CrossRef] [PubMed]
- Lanham-New, S.A.; Webb, A.R.; Cashman, K.D.; Buttriss, J.L.; Fallowfield, J.L.; Masud, T.; Hewison, M.; Mathers, J.C.; Kiely, M.; Welch, A.A.; et al. Vitamin D and SARS-CoV-2 Virus/COVID-19 Disease. BMJ Nutr. Prev. Health 2020, 3, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Parant, F.; Bouloy, J.; Haesebaert, J.; Bendim’red, L.; Goldet, K.; Vanhems, P.; Henaff, L.; Gilbert, T.; Cuerq, C.; Blond, E.; et al. Vitamin D and COVID-19 Severity in Hospitalized Older Patients: Potential Benefit of Prehospital Vitamin D Supplementation. Nutrients 2022, 14, 1641. [Google Scholar] [CrossRef] [PubMed]
- Saadatian-Elahi, M.; Picot, V.; Hénaff, L.; Pradel, F.K.; Escuret, V.; Dananché, C.; Elias, C.; Endtz, H.P.; Vanhems, P. Protocol for a Prospective, Observational, Hospital-Based Multicentre Study of Nosocomial SARS-CoV-2 Transmission: NOSO-COR Project. BMJ Open 2020, 10, e039088. [Google Scholar] [CrossRef] [PubMed]
- Culbertson, E.M.; Culotta, V.C. Copper in Infectious Disease: Using Both Sides of the Penny. Semin. Cell Dev. Biol. 2021, 115, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Pechlivanidou, E.; Vlachakis, D.; Tsarouhas, K.; Panidis, D.; Tsitsimpikou, C.; Darviri, C.; Kouretas, D.; Bacopoulou, F. The Prognostic Role of Micronutrient Status and Supplements in COVID-19 Outcomes: A Systematic Review. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2022, 162, 112901. [Google Scholar] [CrossRef]
- Fischer Walker, C.; Black, R.E. Zinc and the Risk for Infectious Disease. Annu. Rev. Nutr. 2004, 24, 255–275. [Google Scholar] [CrossRef]
- Krinsky, N.I.; Johnson, E.J. Carotenoid Actions and Their Relation to Health and Disease. Mol. Asp. Med. 2005, 26, 459–516. [Google Scholar] [CrossRef]
- Martinez, S.S.; Huang, Y.; Acuna, L.; Laverde, E.; Trujillo, D.; Barbieri, M.A.; Tamargo, J.; Campa, A.; Baum, M.K. Role of Selenium in Viral Infections with a Major Focus on SARS-CoV-2. Int. J. Mol. Sci. 2021, 23, 280. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A Global Clinical Measure of Fitness and Frailty in Elderly People. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef]
- Salo, P.M.; Mendy, A.; Wilkerson, J.; Molsberry, S.A.; Feinstein, L.; London, S.J.; Fessler, M.B.; Thorne, P.S.; Zeldin, D.C. Serum Antioxidant Vitamins and Respiratory Morbidity and Mortality: A Pooled Analysis. Respir. Res. 2022, 23, 150. [Google Scholar] [CrossRef]
- Akbaraly, N.T.; Arnaud, J.; Hininger-Favier, I.; Gourlet, V.; Roussel, A.-M.; Berr, C. Selenium and Mortality in the Elderly: Results from the EVA Study. Clin. Chem. 2005, 51, 2117–2123. [Google Scholar] [CrossRef]
- Heller, R.A.; Sun, Q.; Hackler, J.; Seelig, J.; Seibert, L.; Cherkezov, A.; Minich, W.B.; Seemann, P.; Diegmann, J.; Pilz, M.; et al. Prediction of Survival Odds in COVID-19 by Zinc, Age and Selenoprotein P as Composite Biomarker. Redox Biol. 2021, 38, 101764. [Google Scholar] [CrossRef]
- Vogel-González, M.; Talló-Parra, M.; Herrera-Fernández, V.; Pérez-Vilaró, G.; Chillón, M.; Nogués, X.; Gómez-Zorrilla, S.; López-Montesinos, I.; Arnau-Barrés, I.; Sorli-Redó, M.L.; et al. Low Zinc Levels at Admission Associates with Poor Clinical Outcomes in SARS-CoV-2 Infection. Nutrients 2021, 13, 562. [Google Scholar] [CrossRef]
- Tomasa-Irriguible, T.-M.; Bielsa-Berrocal, L.; Bordejé-Laguna, L.; Tural-Llàcher, C.; Barallat, J.; Manresa-Domínguez, J.-M.; Torán-Monserrat, P. Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave. Metabolites 2021, 11, 565. [Google Scholar] [CrossRef]
- Voelkle, M.; Gregoriano, C.; Neyer, P.; Koch, D.; Kutz, A.; Bernasconi, L.; Conen, A.; Mueller, B.; Schuetz, P. Prevalence of Micronutrient Deficiencies in Patients Hospitalized with COVID-19: An Observational Cohort Study. Nutrients 2022, 14, 1862. [Google Scholar] [CrossRef]
- Im, J.H.; Je, Y.S.; Baek, J.; Chung, M.-H.; Kwon, H.Y.; Lee, J.-S. Nutritional Status of Patients with COVID-19. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2020, 100, 390–393. [Google Scholar] [CrossRef]
- Younesian, O.; Khodabakhshi, B.; Abdolahi, N.; Norouzi, A.; Behnampour, N.; Hosseinzadeh, S.; Alarzi, S.S.H.; Joshaghani, H. Decreased Serum Selenium Levels of COVID-19 Patients in Comparison with Healthy Individuals. Biol. Trace Elem. Res. 2022, 200, 1562–1567. [Google Scholar] [CrossRef]
- Muthuvattur Pallath, M.; Ahirwar, A.K.; Chandra Tripathi, S.; Asia, P.; Sakarde, A.; Gopal, N. COVID-19 and Nutritional Deficiency: A Review of Existing Knowledge. Horm. Mol. Biol. Clin. Investig. 2021, 42, 77–85. [Google Scholar] [CrossRef]
- Rederstorff, M.; Krol, A.; Lescure, A. Understanding the Importance of Selenium and Selenoproteins in Muscle Function. Cell. Mol. Life Sci. 2006, 63, 52–59. [Google Scholar] [CrossRef]
- Katona, P.; Katona-Apte, J. The Interaction between Nutrition and Infection. Clin. Infect. Dis. 2008, 46, 1582–1588. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.P.; Rinaldi, N.A.; Ho, E. Zinc Deficiency Enhanced Inflammatory Response by Increasing Immune Cell Activation and Inducing IL6 Promoter Demethylation. Mol. Nutr. Food Res. 2015, 59, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Skalny, A.V.; Rink, L.; Ajsuvakova, O.P.; Aschner, M.; Gritsenko, V.A.; Alekseenko, S.I.; Svistunov, A.A.; Petrakis, D.; Spandidos, D.A.; Aaseth, J.; et al. Zinc and Respiratory Tract Infections: Perspectives for COVID-19 (Review). Int. J. Mol. Med. 2020, 46, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Pouw, N.; van de Maat, J.; Veerman, K.; Ten Oever, J.; Janssen, N.; Abbink, E.; Reijers, M.; de Mast, Q.; Hoefsloot, W.; van Crevel, R.; et al. Clinical Characteristics and Outcomes of 952 Hospitalized COVID-19 Patients in The Netherlands: A Retrospective Cohort Study. PLoS ONE 2021, 16, e0248713. [Google Scholar] [CrossRef] [PubMed]
- Vural, Z.; Avery, A.; Kalogiros, D.I.; Coneyworth, L.J.; Welham, S.J.M. Trace Mineral Intake and Deficiencies in Older Adults Living in the Community and Institutions: A Systematic Review. Nutrients 2020, 12, 1072. [Google Scholar] [CrossRef]
- Homem, S.G.; Moreira, E.A.M.; da Silva, A.F.; Barni, G.C.; da Rosa, J.S.; de Lima Oliveira, D.; Tomio, C.; de Freitas, M.B.; Portari, G.V.; Furkim, A.M.; et al. Relationship between Oropharyngeal Dysphagia, Nutritional Status, Antioxidant Vitamins and the Inflammatory Response in Adults and Elderly: A Cross-Sectional Study. Clin. Nutr. ESPEN 2020, 38, 211–217. [Google Scholar] [CrossRef]
- Koekkoek, W.A.C.; Hettinga, K.; de Vries, J.H.M.; Zanten, A.R.H. van Micronutrient Deficiencies in Critical Illness. Clin. Nutr. 2021, 40, 3780–3786. [Google Scholar] [CrossRef]
- Majeed, M.; Nagabhushanam, K.; Gowda, S.; Mundkur, L. An Exploratory Study of Selenium Status in Healthy Individuals and in Patients with COVID-19 in a South Indian Population: The Case for Adequate Selenium Status. Nutrition 2021, 82, 111053. [Google Scholar] [CrossRef]
- Elham, A.S.; Azam, K.; Azam, J.; Mostafa, L.; Nasrin, B.; Marzieh, N. Serum Vitamin D, Calcium, and Zinc Levels in Patients with COVID-19. Clin. Nutr. ESPEN 2021, 43, 276–282. [Google Scholar] [CrossRef]
- Rosa, C.; Franca, C.; Lanes Vieira, S.; Carvalho, A.; Penna, A.; Nogueira, C.; Lessa, S.; Ramalho, A. Reduction of Serum Concentrations and Synergy between Retinol, β-Carotene, and Zinc According to Cancer Staging and Different Treatment Modalities Prior to Radiation Therapy in Women with Breast Cancer. Nutrients 2019, 11, 2953. [Google Scholar] [CrossRef]
- Moghaddam, A.; Heller, R.A.; Sun, Q.; Seelig, J.; Cherkezov, A.; Seibert, L.; Hackler, J.; Seemann, P.; Diegmann, J.; Pilz, M.; et al. Selenium Deficiency is Associated with Mortality Risk from COVID-19. Nutrients 2020, 12, 2098. [Google Scholar] [CrossRef]
- Koekkoek, W.A.C.; van Zanten, A.R.H. Antioxidant Vitamins and Trace Elements in Critical Illness. Nutr. Clin. Pract. 2016, 31, 457–474. [Google Scholar] [CrossRef]
- Casaer, M.P.; Bellomo, R. Micronutrient Deficiency in Critical Illness: An Invisible Foe? Intensive Care Med. 2019, 45, 1136–1139. [Google Scholar] [CrossRef]
- Calder, P.C.; Carr, A.C.; Gombart, A.F.; Eggersdorfer, M. Optimal Nutritional Status for a Well-Functioning Immune System is an Important Factor to Protect against Viral Infections. Nutrients 2020, 12, 1181. [Google Scholar] [CrossRef]
- El Sabbagh, E.; El-Sayed, M.; Elbaz, T. Vitamins and Minerals: A Means for Surviving the COVID-19 Pandemic or Just a Myth? J. Infect. Dev. Ctries. 2022, 16, 782–786. [Google Scholar] [CrossRef]
- de Faria Coelho-Ravagnani, C.; Corgosinho, F.C.; Sanches, F.L.F.Z.; Prado, C.M.M.; Laviano, A.; Mota, J.F. Dietary Recommendations during the COVID-19 Pandemic. Nutr. Rev. 2020, 79, 382–393. [Google Scholar] [CrossRef]
- Trujillo-Mayol, I.; Guerra-Valle, M.; Casas-Forero, N.; Sobral, M.M.C.; Viegas, O.; Alarcón-Enos, J.; Ferreira, I.M.; Pinho, O. Western Dietary Pattern Antioxidant Intakes and Oxidative Stress: Importance During the SARS-CoV-2/COVID-19 Pandemic. Adv. Nutr. 2021, 12, 670–681. [Google Scholar] [CrossRef] [PubMed]
- Notz, Q.; Herrmann, J.; Schlesinger, T.; Helmer, P.; Sudowe, S.; Sun, Q.; Hackler, J.; Roeder, D.; Lotz, C.; Meybohm, P.; et al. Clinical Significance of Micronutrient Supplementation in Critically Ill COVID-19 Patients with Severe ARDS. Nutrients 2021, 13, 2113. [Google Scholar] [CrossRef] [PubMed]
- Beran, A.; Mhanna, M.; Srour, O.; Ayesh, H.; Stewart, J.M.; Hjouj, M.; Khokher, W.; Mhanna, A.S.; Ghazaleh, D.; Khader, Y.; et al. Clinical Significance of Micronutrient Supplements in Patients with Coronavirus Disease 2019: A Comprehensive Systematic Review and Meta-Analysis. Clin. Nutr. ESPEN 2022, 48, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Ostermann, M.; Summers, J.; Lei, K.; Card, D.; Harrington, D.J.; Sherwood, R.; Turner, C.; Dalton, N.; Peacock, J.; Bear, D.E. Micronutrients in Critically Ill Patients with Severe Acute Kidney Injury—A Prospective Study. Sci. Rep. 2020, 10, 1505. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).