The Association between Advanced Liver Fibrosis and Mortality Is Modified by Dietary Quality among Korean Adults: Results from the Korea National Health and Nutrition Examination Survey with Mortality Data
Abstract
1. Introduction
2. Materials and Methods
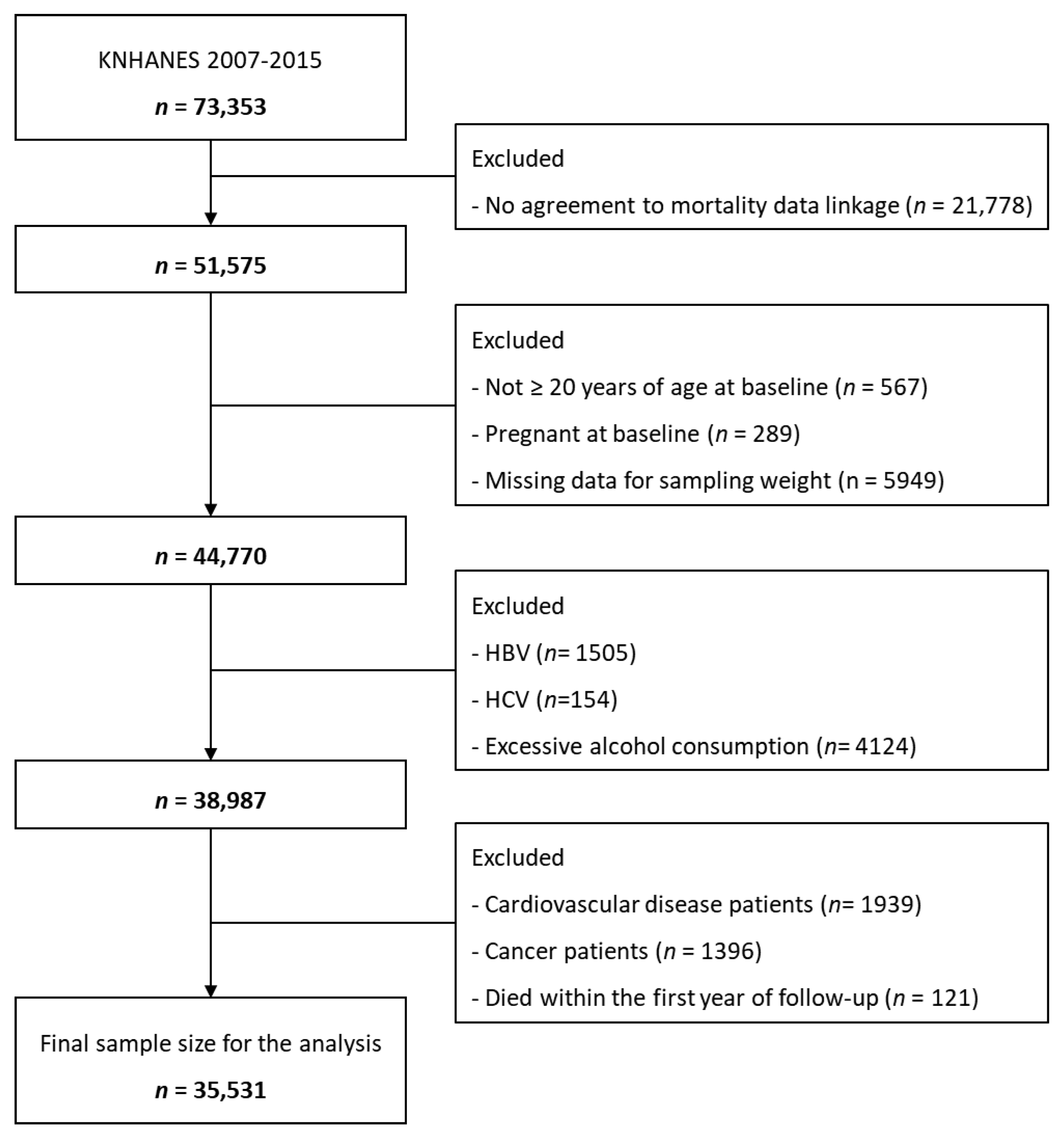
2.1. Study Population
2.2. Definition of Advanced Liver Fibrosis
2.3. Mortality Assessment
2.4. Covariate Assessment
2.5. Diet Quality Assessment
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
3.2. Advanced Liver Fibrosis and Mortality
3.3. Stratified Analysis by Diet Quality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huang, D.Q.; El-Serag, H.B.; Loomba, R. Global epidemiology of NAFLD-related HCC: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 223–238. [Google Scholar] [CrossRef] [PubMed]
- Angulo, P. Nonalcoholic Fatty Liver Disease. N. Engl. J. Med. 2002, 346, 1221–1231. [Google Scholar] [CrossRef] [PubMed]
- Loomba, R.; Friedman, S.L.; Shulman, G.I. Mechanisms and disease consequences of nonalcoholic fatty liver disease. Cell 2021, 184, 2537–2564. [Google Scholar] [CrossRef]
- Kim, D.; Adejumo, A.C.; Yoo, E.R.; Iqbal, U.; Li, A.A.; Pham, E.A.; Cholankeril, G.; Glenn, J.S.; Ahmed, A. Trends in Mortality from Extrahepatic Complications in Patients with Chronic Liver Disease, from 2007 through 2017. Gastroenterology 2019, 157, 1055–1066.e11. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef]
- Wong, V.W.-S.; Adams, L.A.; de Lédinghen, V.; Wong, G.L.-H.; Sookoian, S. Noninvasive biomarkers in NAFLD and NASH—Current progress and future promise. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 461–478. [Google Scholar] [CrossRef] [PubMed]
- Angulo, P.; Hui, J.M.; Marchesini, G.; Bugianesi, E.; George, J.; Farrell, G.C.; Enders, F.; Saksena, S.; Burt, A.D.; Bida, J.P.; et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007, 45, 846–854. [Google Scholar] [CrossRef]
- Shah, A.G.; Lydecker, A.; Murray, K.; Tetri, B.N.; Contos, M.J.; Sanyal, A.J. Comparison of Noninvasive Markers of Fibrosis in Patients with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2009, 7, 1104–1112. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Kim, W.R.; Kim, H.J.; Therneau, T.M. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology 2013, 57, 1357–1365. [Google Scholar] [CrossRef] [PubMed]
- Dulai, P.S.; Singh, S.; Patel, J.; Soni, M.; Prokop, L.J.; Younossi, Z.; Sebastiani, G.; Ekstedt, M.; Hagstrom, H.; Nasr, P.; et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: Systematic review and meta-analysis. Hepatology 2017, 65, 1557–1565. [Google Scholar] [CrossRef]
- Hwang, Y.-C.; Ahn, H.-Y.; Park, S.-W.; Park, C.-Y. Nonalcoholic Fatty Liver Disease Associates with Increased Overall Mortality and Death from Cancer, Cardiovascular Disease, and Liver Disease in Women but Not Men. Clin. Gastroenterol. Hepatol. 2018, 16, 1131–1137.e5. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Corey, K.E.; Lim, J.K. AGA Clinical Practice Update on Lifestyle Modification Using Diet and Exercise to Achieve Weight Loss in the Management of Nonalcoholic Fatty Liver Disease: Expert Review. Gastroenterology 2021, 160, 912–918. [Google Scholar] [CrossRef]
- Ryan, M.C.; Itsiopoulos, C.; Thodis, T.; Ward, G.; Trost, N.; Hofferberth, S.; O’Dea, K.; Desmond, P.V.; Johnson, N.A.; Wilson, A.M. The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. J. Hepatol. 2013, 59, 138–143. [Google Scholar] [CrossRef]
- Zelber-Sagi, S.; Salomone, F.; Mlynarsky, L. The Mediterranean dietary pattern as the diet of choice for non-alcoholic fatty liver disease: Evidence and plausible mechanisms. Liver Int. 2017, 37, 936–949. [Google Scholar] [CrossRef] [PubMed]
- Zelber-Sagi, S.; Ivancovsky-Wajcman, D.; Fliss Isakov, N.; Webb, M.; Orenstein, D.; Shibolet, O.; Kariv, R. High red and processed meat consumption is associated with non-alcoholic fatty liver disease and insulin resistance. J. Hepatol. 2018, 68, 1239–1246. [Google Scholar] [CrossRef]
- Paik, J.M.; Mir, S.; Alqahtani, S.A.; Younossi, Y.; Ong, J.P.; Younossi, Z.M. Dietary Risks for Liver Mortality in NAFLD: Global Burden of Disease Data. Hepatol. Commun. 2022, 6, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Yoo, E.R.; Kim, D.; Vazquez-Montesino, L.M.; Escober, J.A.; Li, A.A.; Tighe, S.P.; Fernandes, C.T.; Cholankeril, G.; Ahmed, A. Diet quality and its association with nonalcoholic fatty liver disease and all-cause and cause-specific mortality. Liver Int. 2020, 40, 815–824. [Google Scholar] [CrossRef] [PubMed]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Yun, S.; Oh, K. The Korea National Health and Nutrition Examination Survey data linked Cause of Death data. Epidemiol. Health 2022, 44, e2022021. [Google Scholar] [CrossRef]
- Vallet-Pichard, A.; Mallet, V.; Nalpas, B.; Verkarre, V.; Nalpas, A.; Dhalluin-Venier, V.; Fontaine, H.; Pol, S. FIB-4: An inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology 2007, 46, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-h.; Kim, S.U.; Song, K.; Park, J.Y.; Kim, D.Y.; Ahn, S.H.; Lee, B.-W.; Kang, E.S.; Cha, B.-S.; Han, K.-H. Sarcopenia is associated with significant liver fibrosis independently of obesity and insulin resistance in nonalcoholic fatty liver disease: Nationwide surveys (KNHANES 2008–2011). Hepatology 2016, 63, 776–786. [Google Scholar] [CrossRef] [PubMed]
- Sumida, Y.; Nakajima, A.; Itoh, Y. Limitations of liver biopsy and non-invasive diagnostic tests for the diagnosis of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J. Gastroenterol. 2014, 20, 475–485. [Google Scholar] [CrossRef]
- Yun, S.; Park, S.; Yook, S.M.; Kim, K.; Shim, J.E.; Hwang, J.Y.; Oh, K. Development of the Korean Healthy Eating Index for adults, based on the Korea National Health and Nutrition Examination Survey. Nutr. Res. Pract. 2022, 16, 233–247. [Google Scholar] [CrossRef] [PubMed]
- Jo, G.; Park, D.; Lee, J.; Kim, R.; Subramanian, S.V.; Oh, H.; Shin, M.-J. Trends in Diet Quality and Cardiometabolic Risk Factors among Korean Adults, 2007–2018. JAMA Netw. Open 2022, 5, e2218297. [Google Scholar] [CrossRef]
- Asadi, Z.; Shafiee, M.; Sadabadi, F.; Heidari-Bakavoli, A.; Moohebati, M.; Khorrami, M.S.; Darroudi, S.; Heidari, S.; Hoori, T.; Tayefi, M.; et al. Association of dietary patterns and risk of cardiovascular disease events in the MASHAD cohort study. J. Hum. Nutr. Diet. 2019, 32, 789–801. [Google Scholar] [CrossRef]
- Lim, S. Eating a Balanced Diet: A Healthy Life through a Balanced Diet in the Age of Longevity. JOMES 2018, 27, 39–45. [Google Scholar] [CrossRef]
- Rondanelli, M.; Klersy, C.; Perna, S.; Faliva, M.A.; Montorfano, G.; Roderi, P.; Colombo, I.; Corsetto, P.A.; Fioravanti, M.; Solerte, S.B.; et al. Effects of two-months balanced diet in metabolically healthy obesity: Lipid correlations with gender and BMI-related differences. Lipids Health Dis. 2015, 14, 139. [Google Scholar] [CrossRef]
- Torres, L.; Schuch, A.; Longo, L.; Valentini, B.B.; Galvão, G.S.; Luchese, E.; Pinzon, C.; Bartels, R.; Álvares-da-Silva, M.R. New FIB-4 and NFS cutoffs to guide sequential non-invasive assessment of liver fibrosis by magnetic resonance elastography in NAFLD. Ann. Hepatol. 2023, 28, 100774. [Google Scholar] [CrossRef] [PubMed]
- Unalp-Arida, A.; Ruhl, C.E. Liver fibrosis scores predict liver disease mortality in the United States population. Hepatology 2017, 66, 84–95. [Google Scholar] [CrossRef]
- Hagström, H.; Nasr, P.; Ekstedt, M.; Stål, P.; Hultcrantz, R.; Kechagias, S. Accuracy of Noninvasive Scoring Systems in Assessing Risk of Death and Liver-Related Endpoints in Patients with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2019, 17, 1148–1156.e4. [Google Scholar] [CrossRef]
- Önnerhag, K.; Hartman, H.; Nilsson, P.M.; Lindgren, S. Non-invasive fibrosis scoring systems can predict future metabolic complications and overall mortality in non-alcoholic fatty liver disease (NAFLD). Scand. J. Gastroenterol. 2019, 54, 328–334. [Google Scholar] [CrossRef]
- Angulo, P.; Bugianesi, E.; Bjornsson, E.S.; Charatcharoenwitthaya, P.; Mills, P.R.; Barrera, F.; Haflidadottir, S.; Day, C.P.; George, J. Simple Noninvasive Systems Predict Long-term Outcomes of Patients with Nonalcoholic Fatty Liver Disease. Gastroenterology 2013, 145, 782–789.e4. [Google Scholar] [CrossRef] [PubMed]
- Yoshihisa, A.; Sato, Y.; Yokokawa, T.; Sato, T.; Suzuki, S.; Oikawa, M.; Kobayashi, A.; Yamaki, T.; Kunii, H.; Nakazato, K.; et al. Liver fibrosis score predicts mortality in heart failure patients with preserved ejection fraction. ESC Heart Fail. 2018, 5, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Byrne, C.D.; Targher, G. NAFLD: A multisystem disease. J. Hepatol. 2015, 62, S47–S64. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, M.C.G.J.; Simons, N.; Stehouwer, C.D.A.; Isaacs, A. Non-alcoholic fatty liver disease and cardiovascular disease: Assessing the evidence for causality. Diabetologia 2020, 63, 253–260. [Google Scholar] [CrossRef]
- Cai, J.; Zhang, X.-J.; Ji, Y.-X.; Zhang, P.; She, Z.-G.; Li, H. Nonalcoholic Fatty Liver Disease Pandemic Fuels the Upsurge in Cardiovascular Diseases. Circ. Res. 2020, 126, 679–704. [Google Scholar] [CrossRef]
- Mantovani, A.; Csermely, A.; Petracca, G.; Beatrice, G.; Corey, K.E.; Simon, T.G.; Byrne, C.D.; Targher, G. Non-alcoholic fatty liver disease and risk of fatal and non-fatal cardiovascular events: An updated systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 903–913. [Google Scholar] [CrossRef]
- Kim, D.; Konyn, P.; Sandhu, K.K.; Dennis, B.B.; Cheung, A.C.; Ahmed, A. Metabolic dysfunction-associated fatty liver disease is associated with increased all-cause mortality in the United States. J. Hepatol. 2021, 75, 1284–1291. [Google Scholar] [CrossRef]
- Simon, T.G.; Roelstraete, B.; Khalili, H.; Hagström, H.; Ludvigsson, J.F. Mortality in biopsy-confirmed nonalcoholic fatty liver disease: Results from a nationwide cohort. Gut 2021, 70, 1375–1382. [Google Scholar] [CrossRef]
- Taylor, R.S.; Taylor, R.J.; Bayliss, S.; Hagström, H.; Nasr, P.; Schattenberg, J.M.; Ishigami, M.; Toyoda, H.; Wai-Sun Wong, V.; Peleg, N.; et al. Association Between Fibrosis Stage and Outcomes of Patients with Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. Gastroenterology 2020, 158, 1611–1625.e2. [Google Scholar] [CrossRef]
- Romero-Gómez, M.; Zelber-Sagi, S.; Trenell, M. Treatment of NAFLD with diet, physical activity and exercise. J. Hepatol. 2017, 67, 829–846. [Google Scholar] [CrossRef]
- Zelber-Sagi, S.; Ratziu, V.; Oren, R. Nutrition and physical activity in NAFLD: An overview of the epidemiological evidence. World J. Gastroenterol. WJG 2011, 17, 3377–3389. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, E.T.; Ohls, J.; Carlson, S.; Fleming, K. The Healthy Eating Index: Design and Applications. J. Am. Diet. Assoc. 1995, 95, 1103–1108. [Google Scholar] [CrossRef]
- Guenther, P.M.; Casavale, K.O.; Reedy, J.; Kirkpatrick, S.I.; Hiza, H.A.B.; Kuczynski, K.J.; Kahle, L.L.; Krebs-Smith, S.M. Update of the Healthy Eating Index: HEI-2010. J. Acad. Nutr. Diet. 2013, 113, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- Hannah, W.N.; Harrison, S.A. Lifestyle and Dietary Interventions in the Management of Nonalcoholic Fatty Liver Disease. Dig. Dis. Sci. 2016, 61, 1365–1374. [Google Scholar] [CrossRef] [PubMed]
- Yki-Järvinen, H. Nutritional Modulation of Non-Alcoholic Fatty Liver Disease and Insulin Resistance. Nutrients 2015, 7, 9127–9138. [Google Scholar] [CrossRef]
- Gerhard, G.T.; Ahmann, A.; Meeuws, K.; McMurry, M.P.; Duell, P.B.; Connor, W.E. Effects of a low-fat diet compared with those of a high-monounsaturated fat diet on body weight, plasma lipids and lipoproteins, and glycemic control in type 2 diabetes. Am. J. Clin. Nutr. 2004, 80, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, A.J.; Chalasani, N.; Kowdley, K.V.; McCullough, A.; Diehl, A.M.; Bass, N.M.; Neuschwander-Tetri, B.A.; Lavine, J.E.; Tonascia, J.; Unalp, A.; et al. Pioglitazone, Vitamin E, or Placebo for Nonalcoholic Steatohepatitis. N. Engl. J. Med. 2010, 362, 1675–1685. [Google Scholar] [CrossRef]
- Violi, F.; Cammisotto, V.; Bartimoccia, S.; Pignatelli, P.; Carnevale, R.; Nocella, C. Gut-derived low-grade endotoxaemia, atherothrombosis and cardiovascular disease. Nat. Rev. Cardiol. 2023, 20, 24–37. [Google Scholar] [CrossRef]
- Wang, H.; Mehal, W.; Nagy, L.E.; Rotman, Y. Immunological mechanisms and therapeutic targets of fatty liver diseases. Cell. Mol. Immunol. 2021, 18, 73–91. [Google Scholar] [CrossRef] [PubMed]
- Carpino, G.; Del Ben, M.; Pastori, D.; Carnevale, R.; Baratta, F.; Overi, D.; Francis, H.; Cardinale, V.; Onori, P.; Safarikia, S.; et al. Increased Liver Localization of Lipopolysaccharides in Human and Experimental NAFLD. Hepatology 2020, 72, 470–485. [Google Scholar] [CrossRef] [PubMed]
- Kessoku, T.; Kobayashi, T.; Imajo, K.; Tanaka, K.; Yamamoto, A.; Takahashi, K.; Kasai, Y.; Ozaki, A.; Iwaki, M.; Nogami, A.; et al. Endotoxins and Non-Alcoholic Fatty Liver Disease. Front. Endocrinol. 2021, 12, 770986. [Google Scholar] [CrossRef] [PubMed]
- Huby, T.; Gautier, E.L. Immune cell-mediated features of non-alcoholic steatohepatitis. Nat. Rev. Immunol. 2022, 22, 429–443. [Google Scholar] [CrossRef]
- Witkowski, M.; Weeks, T.L.; Hazen, S.L. Gut Microbiota and Cardiovascular Disease. Circ. Res. 2020, 127, 553–570. [Google Scholar] [CrossRef] [PubMed]
- Salvador Castell, G.; Serra-Majem, L.; Ribas-Barba, L. What and how much do we eat? 24-hour dietary recall method. Nutr. Hosp. 2015, 31, 46–48. [Google Scholar] [CrossRef]
| All | NFS | FIB-4 | |||||
|---|---|---|---|---|---|---|---|
| <1.54 | ≥1.54 | p-Value | <2.67 | ≥2.67 | p-Value | ||
| N (%) | 35,531 | 22,536 (76.3) | 7009 (23.7) | 30,330 (97.9) | 638 (2.1) | ||
| weighted N (weighted %) | 29,419,312 | 20,202,666 (82.6) | 4,253,682 (17.4) | 25,488,644 (98.7) | 344,085 (1.3) | ||
| Age, years | 45.2 ± 0.1 | 41.2 ± 0.1 | 61.7 ± 0.2 | <0.001 | 44.5 ± 0.1 | 67.1 ± 0.7 | <0.001 |
| Male, N (%) | 12,839 (45.3) | 7561 (44.8) | 3179 (49.9) | <0.001 | 11,021 (46.0) | 341 (54.9) | <0.001 |
| Residential area, N (%) | |||||||
| Urban Rural | 23,472 (71.0) 12,059 (29.0) | 15,408 (72.6) 7128 (27.4) | 4343 (66.7) 2666 (33.3) | <0.001 | 20,339 (71.6) 9991 (28.4) | 378 (63.6) 260 (36.4) | <0.001 |
| Education level, N (%) | |||||||
| ≤Elementary school graduate Middle school graduate High school graduate ≥University graduate | 9114 (18.0) 3601 (9.3) 11,097 (38.2) 9993 (34.5) | 4023 (11.5) 2057 (7.9) 8192 (40.9) 8057 (39.7) | 3316 (42.3) 1047 (15.6) 1529 (25.5) 914 (16.6) | <0.001 | 7187 (16.4) 3102 (9.2) 9829 (38.6) 9072 (35.9) | 352 (54.6) 77 (13.6) 118 (23.1) 52 (8.7) | <0.001 |
| Household income level, N (%) | |||||||
| Lowest Lower-middle Upper-middle Highest | 7176 (15.4) 8868 (25.7) 9441 (29.4) 9525 (29.5) | 3129 (11.2) 5538 (25.4) 6715 (31.4) 6960 (31.9) | 2409 (28.8) 1833 (26.0) 1396 (23.6) 1277 (21.5) | <0.001 | 5571 (14.1) 7566 (25.6) 8359 (30.1) 8502 (30.3) | 293 (42.6) 179 (29.2) 87 (15.9) 67 (12.3) | <0.001 |
| Current smoker, N (%) | 5353 (20.5) | 3625 (21.2) | 911 (15.6) | <0.001 | 4679 (20.8) | 98 (20.2) | 0.785 |
| Current drinker, N (%) | 16,055 (53.0) | 11,092 (55.3) | 2913 (46.5) | <0.001 | 14,139 (53.8) | 272 (46.8) | <0.001 |
| METs, min/wk | 2015.5 ± 28.6 | 2004.8 ± 31.6 | 1884.6 ± 52.9 | 0.021 | 2011.8 ± 29.0 | 1733.6 ± 155.3 | 0.037 |
| KHEI | 52.7 ± 0.1 | 52.7 ± 0.1 | 54.2 ± 0.2 | <0.001 | 52.9 ± 0.1 | 51.2 ± 0.6 | 0.004 |
| Cardiometabolic parameters | |||||||
| Body mass index, kg/m2 | 23.58 ± 0.03 | 23.29 ± 0.03 | 24.95 ± 0.06 | <0.001 | 23.59 ± 0.03 | 23.40 ± 0.19 | 0.353 |
| Waist circumference, cm | 80.6 ± 0.1 | 79.3 ± 0.1 | 85.7 ± 0.2 | <0.001 | 80.5 ± 0.1 | 83.2 ± 0.5 | <0.001 |
| Systolic BP, mmHg | 116.4 ± 0.1 | 114.1 ± 0.1 | 126.0 ± 0.3 | <0.001 | 116.1 ± 0.1 | 127.5 ± 0.9 | <0.001 |
| Diastolic BP, mmHg | 75.3 ± 0.1 | 75.1 ± 0.1 | 77.2 ± 0.2 | <0.001 | 75.5 ± 0.1 | 74.4 ± 0.5 | 0.038 |
| Fasting glucose, mg/dL | 96.8 ± 0.2 | 93.7 ± 0.1 | 110.9 ± 0.4 | <0.001 | 96.8 ± 0.2 | 106.2 ± 1.7 | <0.001 |
| HbA1c, % | 5.78 ± 0.01 | 5.65 ± 0.01 | 6.26 ± 0.02 | <0.001 | 5.77 ± 0.01 | 6.08 ± 0.07 | <0.001 |
| Total cholesterol, mg/dL | 187.8 ± 0.3 | 187.3 ± 0.3 | 191.3 ± 0.5 | <0.001 | 188.0 ± 0.3 | 177.9 ± 1.6 | <0.001 |
| Triglycerides, mg/dL | 127.2 ± 0.7 | 122.1 ± 0.8 | 147.8 ± 1.8 | <0.001 | 127.2 ± 0.8 | 137.8 ± 5.1 | 0.031 |
| HDL cholesterol, mg/dL | 49.6 ± 0.1 | 50.2 ± 0.1 | 47.2 ± 0.2 | <0.001 | 49.7 ± 0.1 | 48.7 ± 0.7 | 0.097 |
| LDL cholesterol, mg/dL | 113.6 ± 0.2 | 113.4 ± 0.3 | 115.7 ± 0.5 | <0.001 | 113.7 ± 0.2 | 103.6 ± 1.7 | <0.001 |
| AST, IU/L | 21.5 ± 0.1 | 20.5 ± 0.1 | 24.6 ± 0.2 | <0.001 | 21.0 ± 0.1 | 45.2 ± 2.0 | <0.001 |
| ALT, IU/L | 21.5 ± 0.1 | 21.1 ± 0.2 | 21.8 ± 0.3 | 0.014 | 21.2 ± 0.1 | 30.3 ± 1.6 | <0.001 |
| Metabolic comorbidities | |||||||
| Hypertension | 9505 (22.2) | 4444 (16.2) | 3562 (48.9) | <0.001 | 7878 (21.4) | 327 (52.4) | <0.001 |
| Diabetes mellitus | 3344 (8.7) | 1154 (4.6) | 1815 (26.7) | <0.001 | 3006 (8.6) | 130 (23.5) | <0.001 |
| Hypercholesterolemia | 4420 (12.0) | 2770 (10.6) | 1392 (20.0) | <0.001 | 4087 (12.1) | 82 (14.8) | 0.125 |
| Weighted Total (N) | Weighted Event (N) | Weighted Follow-Up (PY) | Weighted Incidence Rate (per 1000 PY) | Model 0: HR (95% CI) | Model 1: HR (95% CI) | Model 2: HR (95% CI) | |
|---|---|---|---|---|---|---|---|
| NFS | |||||||
| All-cause mortality | |||||||
| <1.54 | 20,202,666 | 245,688 | 159,100,000 | 1.54 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| ≥1.54 | 4,253,682 | 356,136 | 31,190,946 | 11.42 | 7.71 (6.63–8.97) | 1.31 (1.11–1.54) | 1.20 (1.01–1.43) |
| Cardiovascular mortality | |||||||
| <1.54 | 20,202,666 | 52,108 | 159,100,000 | 0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| ≥1.54 | 4,253,682 | 82,524 | 31,190,946 | 2.65 | 8.44 (6.25–11.39) | 1.31 (0.94–1.83) | 1.29 (0.93–1.78) |
| FIB-4 | |||||||
| All-cause mortality | |||||||
| <2.67 | 25,488,644 | 587,982 | 197,700,000 | 2.97 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| ≥2.67 | 344,085 | 72,898 | 2,325,029 | 31.35 | 11.24 (9.10–13.89) | 1.72 (1.35–2.19) | 1.72 (1.35–2.18) |
| Cardiovascular mortality | |||||||
| <2.67 | 25,488,644 | 133,112 | 197,700,000 | 0.67 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| ≥2.67 | 344,085 | 18,468 | 2,325,029 | 7.94 | 12.60 (8.43–18.83) | 1.88 (1.23–2.88) | 1.82 (1.17–2.84) |
| Weighted Total (N) | Weighted Event (N) | Weighted Follow-Up (PY) | Weighted Incidence Rate (per 1000 PY) | Model 0: HR (95% CI) | Model 1: HR (95% CI) | Model 2: HR (95% CI) | |
|---|---|---|---|---|---|---|---|
| Low NFS + Low FIB-4 | 20,195,527 | 244,931 | 159,100,000 | 1.54 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Low NFS + High FIB-4 or High NFS + Low FIB-4 | 3,944,350 | 292,935 | 29,080,373 | 10.07 | 6.81 (5.82–7.96) | 1.23 (1.04–1.46) | 1.12 (0.94–1.33) |
| High NFS + High FIB-4 | 312,957 | 63,958 | 2,143,873 | 29.83 | 20.88 (16.33–26.69) | 1.91 (1.46–2.51) | 1.85 (1.42–2.43) |
| Low NFS + Low FIB-4 | 20,195,527 | 52,108 | 159,100,000 | 0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Low NFS + High FIB-4 or High NFS + Low FIB-4 | 3,944,350 | 66,555 | 29,080,373 | 2.29 | 7.28 (5.36–9.89) | 1.22 (0.87–1.72) | 1.19 (0.85–1.66) |
| High NFS + High FIB-4 | 312,957 | 15,969 | 2,143,873 | 7.45 | 24.48 (15.04–39.85) | 2.04 (1.22–3.15) | 2.04 (1.23–3.39) |
| Low and Moderate Diet Quality (KHEI ≤ 60) (n = 26,078) | High Diet Quality (KHEI > 60) (n = 10,798) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Weighted Event (N) | Weighted Follow-Up (PY) | Model 0: HR (95% CI) | Model 1: HR (95% CI) | Model 2: HR (95% CI) | Weighted Event (N) | Weighted Follow-Up (PY) | Model 0: HR (95% CI) | Model 1: HR (95% CI) | Model 2: HR (95% CI) | |
| All-cause mortality | ||||||||||
| <1.54 | 200,775 | 116,900,000 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 42,827 | 42,058,152 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| ≥1.54 | 294,751 | 21,919,704 | 8.09 (6.84–9.57) | 1.38 (1.15–1.65) | 1.27 (1.06–1.53) | 60,479 | 9,221,865 | 6.83 (4.89–9.53) | 1.05 (0.70–1.56) | 0.96 (0.62–1.48) |
| Cardiovascular mortality | ||||||||||
| <1.54 | 41,405 | 116,900,000 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 9585 | 42,058,152 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| ≥1.54 | 72,379 | 21,919,704 | 9.66 (6.90–13.52) | 1.51 (1.05–2.17) | 1.46 (1.03–2.09) | 10,145 | 9,221,865 | 5.06 (2.52–10.19) | 0.68 (0.31–1.53) | 0.71 (0.32–1.56) |
| All-cause mortality | ||||||||||
| <2.67 | 481,817 | 144,500,000 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 104,080 | 53,041,238 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| ≥2.67 | 62,175 | 1,774,654 | 11.21 (8.84–14.20) | 1.74 (1.34–2.26) | 1.79 (1.38–2.35) | 9817 | 525,633 | 10.25 (6.19–16.98) | 1.68 (0.98–2.89) | 1.33 (0.78–2.25) |
| Cardiovascular mortality | ||||||||||
| <2.67 | 113,797 | 144,500,000 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 18,197 | 53,041,238 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| ≥2.67 | 16,935 | 1,774,654 | 12.95 (8.41–19.93) | 2.03 (1.29–3.19) | 2.00 (1.25–3.20) | 1533 | 525,633 | 9.03 (2.74–29.77) | 0.87 (0.29–2.60) | 0.88 (0.30–2.63) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Jo, G.; Park, D.; Jun, H.J.; Bae, J.H.; Shin, M.-J. The Association between Advanced Liver Fibrosis and Mortality Is Modified by Dietary Quality among Korean Adults: Results from the Korea National Health and Nutrition Examination Survey with Mortality Data. Nutrients 2023, 15, 1501. https://doi.org/10.3390/nu15061501
Lee J, Jo G, Park D, Jun HJ, Bae JH, Shin M-J. The Association between Advanced Liver Fibrosis and Mortality Is Modified by Dietary Quality among Korean Adults: Results from the Korea National Health and Nutrition Examination Survey with Mortality Data. Nutrients. 2023; 15(6):1501. https://doi.org/10.3390/nu15061501
Chicago/Turabian StyleLee, Juhee, Garam Jo, Dahyun Park, Hee Ju Jun, Jae Hyun Bae, and Min-Jeong Shin. 2023. "The Association between Advanced Liver Fibrosis and Mortality Is Modified by Dietary Quality among Korean Adults: Results from the Korea National Health and Nutrition Examination Survey with Mortality Data" Nutrients 15, no. 6: 1501. https://doi.org/10.3390/nu15061501
APA StyleLee, J., Jo, G., Park, D., Jun, H. J., Bae, J. H., & Shin, M.-J. (2023). The Association between Advanced Liver Fibrosis and Mortality Is Modified by Dietary Quality among Korean Adults: Results from the Korea National Health and Nutrition Examination Survey with Mortality Data. Nutrients, 15(6), 1501. https://doi.org/10.3390/nu15061501






