Bifidobacterium as a Potential Biomarker of Sarcopenia in Elderly Women
Abstract
1. Introduction
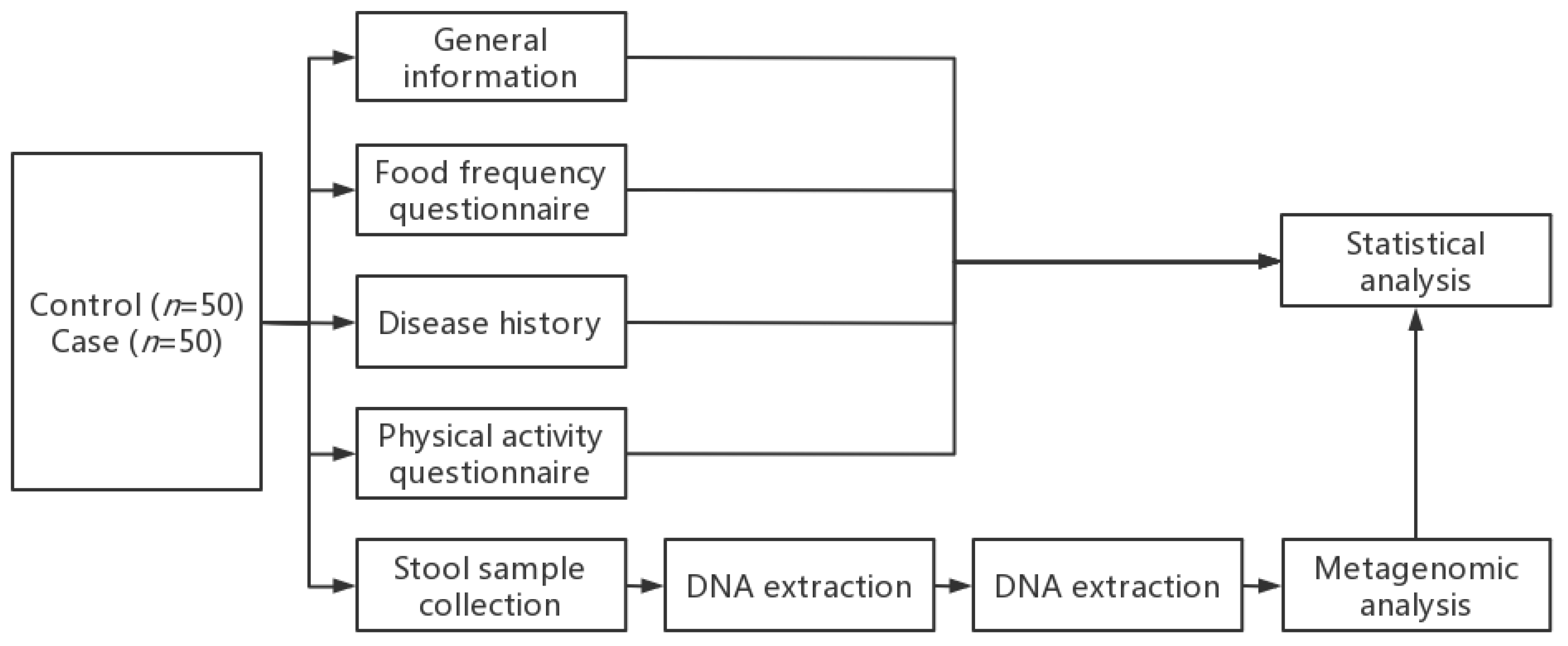
2. Materials and Methods
2.1. Participants
2.2. Screening Criteria
2.3. Data and Biological Sample Collection
2.4. Gut Microbiota Metagenomic Detection
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Dietary Intake
3.3. Body Composition
3.4. Bacterial Composition Analysis
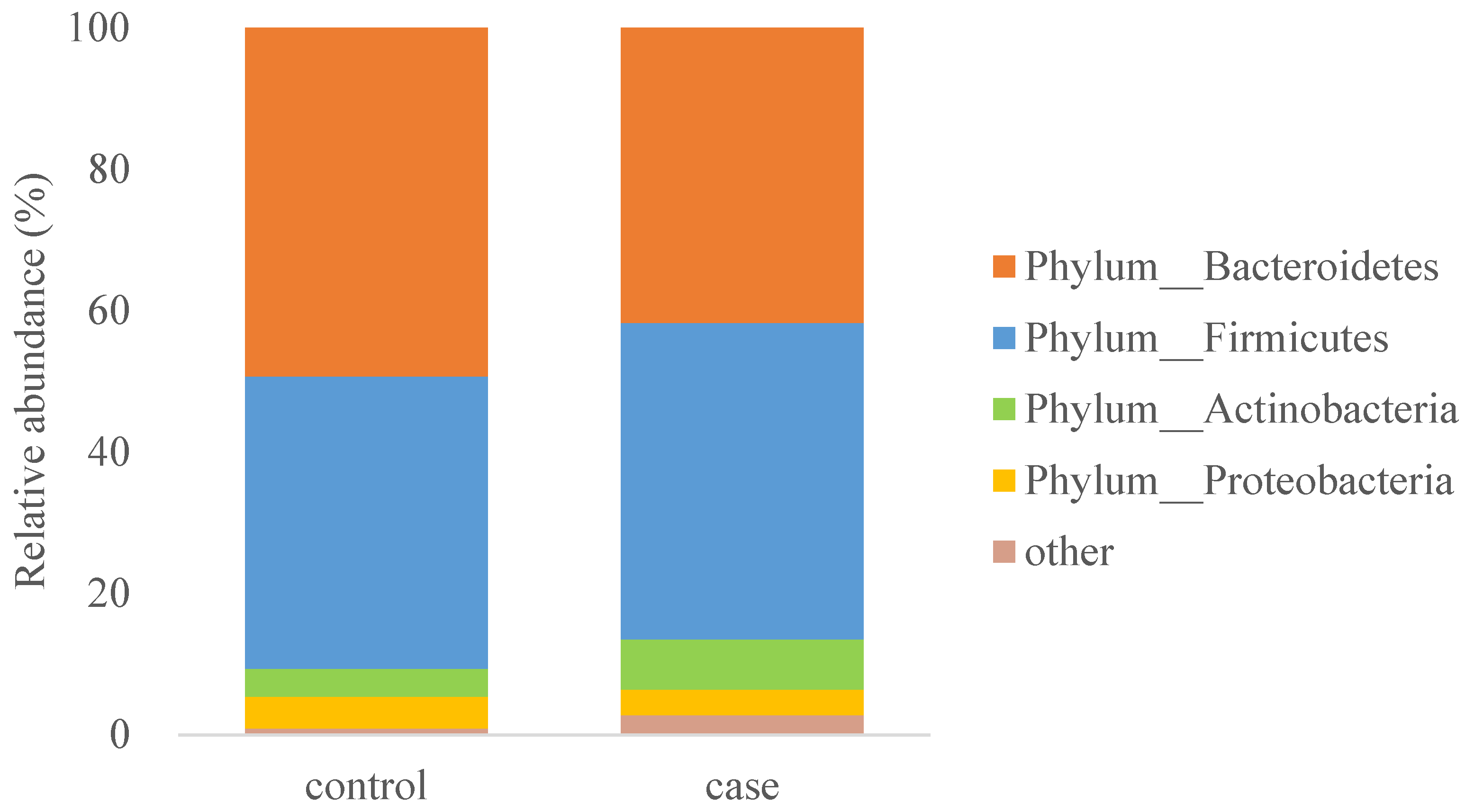
3.5. Linear Discriminant Analysis Effect Size Analysis
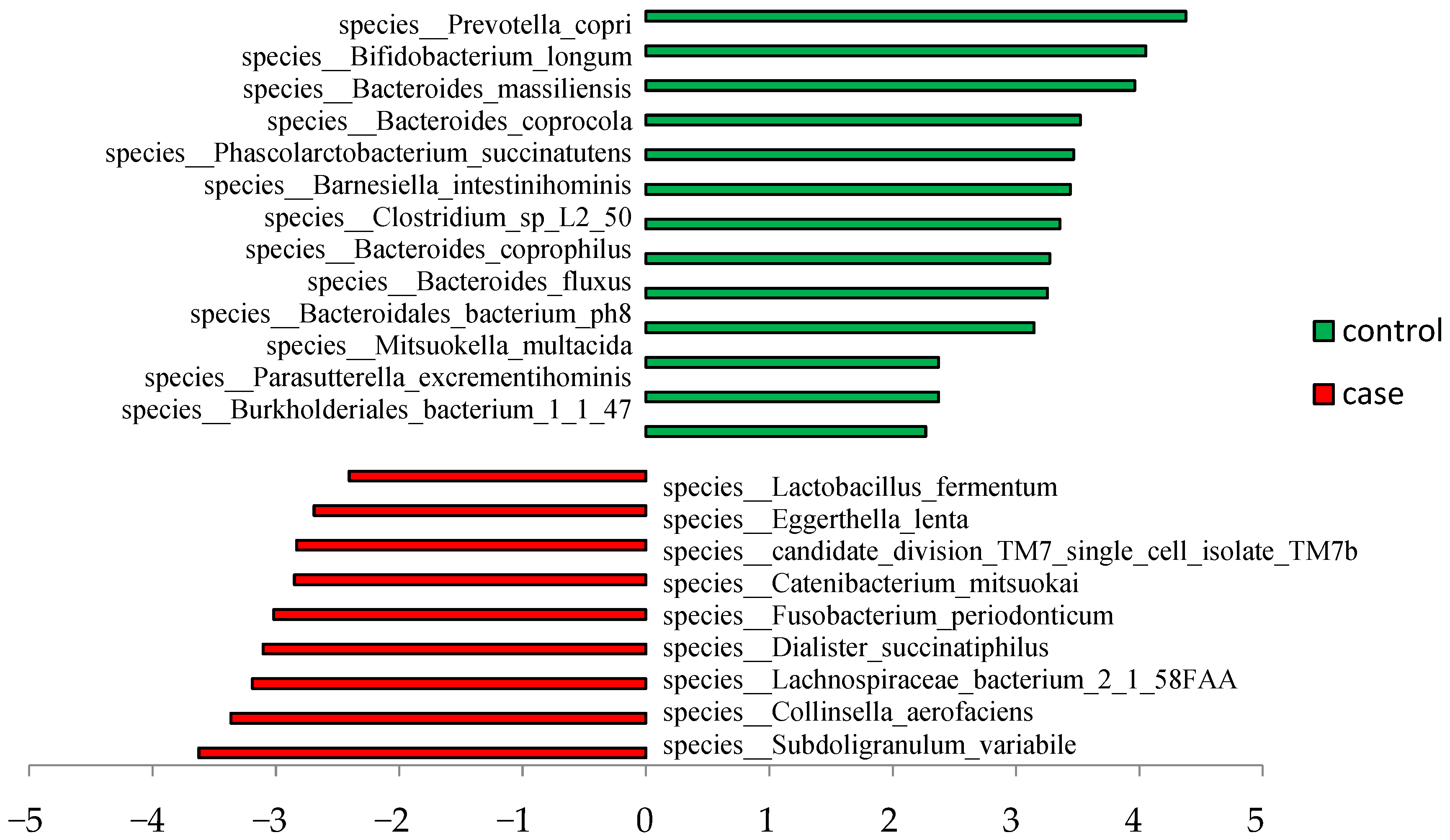
3.6. ROC Analysis
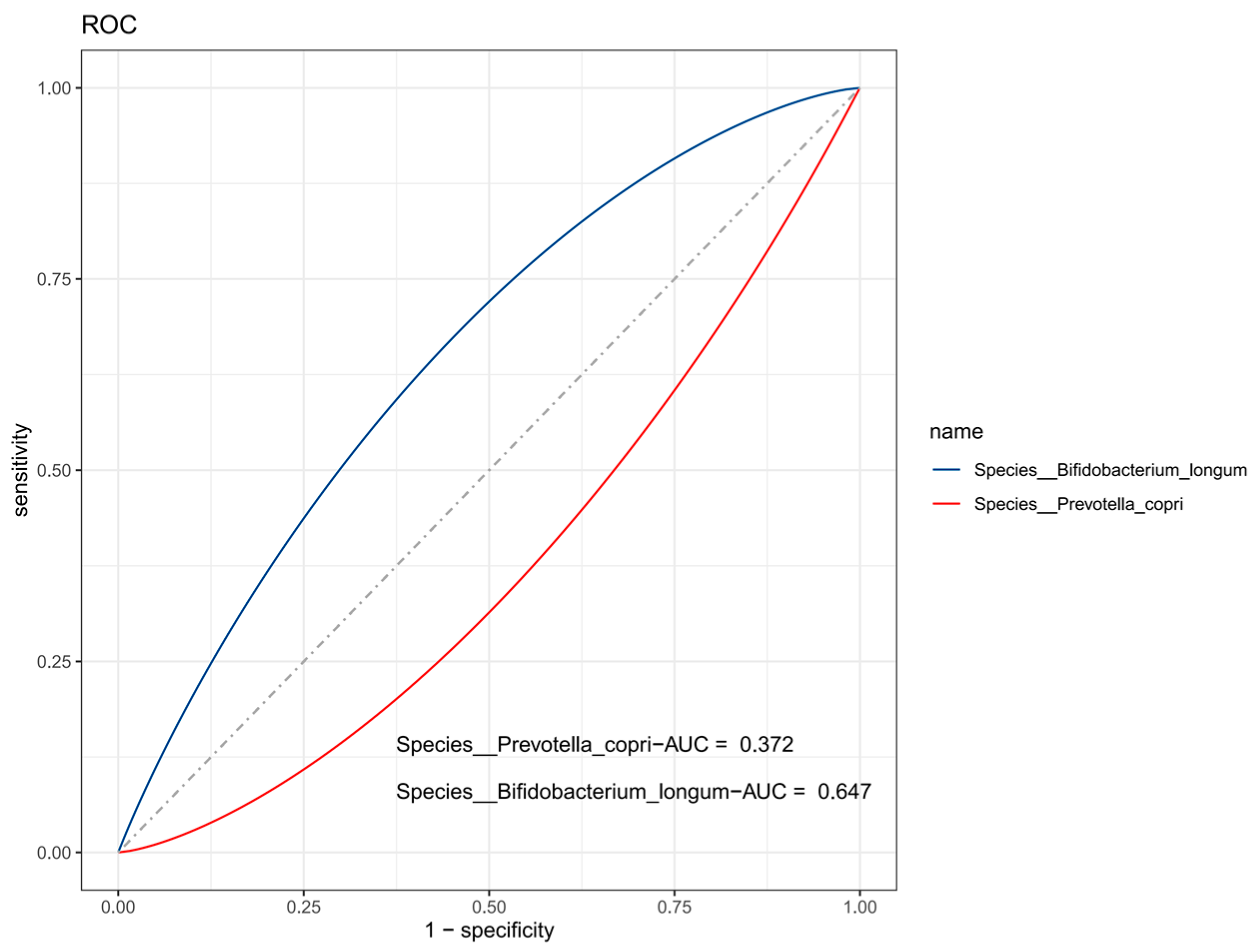
3.7. Spearman Correlation Analysis
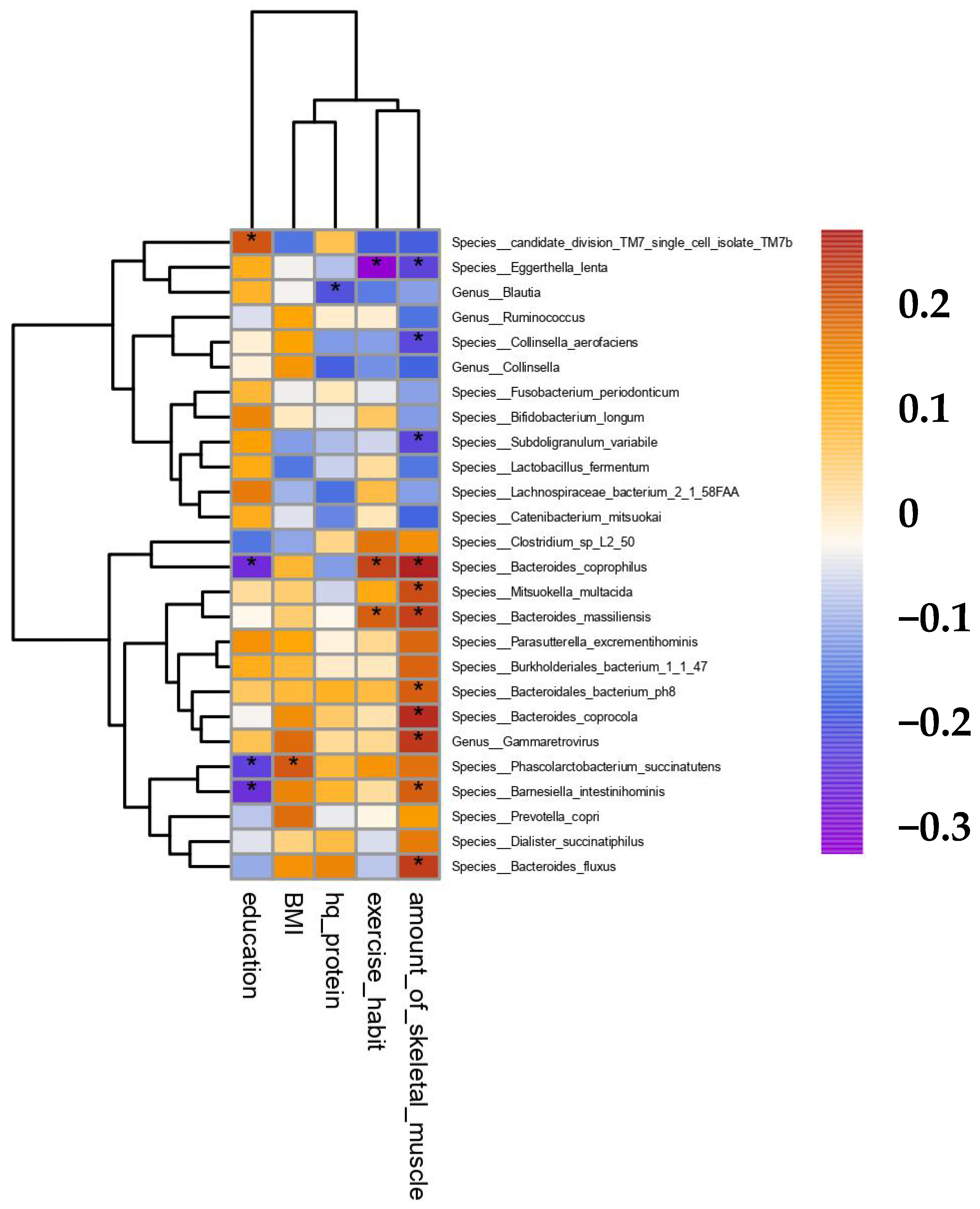
3.8. Multivariate Linear Correlation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Landi, F.; Schneider, S.M.; Zúñiga, C.; Arai, H.; Boirie, Y.; Chen, L.K.; Fielding, R.A.; Martin, F.C.; Michel, J.P.; et al. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 2014, 43, 748–759. [Google Scholar] [CrossRef]
- Chen, Z.; Ho, M.; Chau, P.H. Prevalence, Incidence, and Associated Factors of Possible Sarcopenia in Community-Dwelling Chinese Older Adults: A Pop-ulation-Based Longitudinal Study. Front. Med. 2021, 8, 769708. [Google Scholar] [CrossRef]
- Zhao, W.Y.; Zhang, Y.; Hou, L.S.; Xia, X. The association between systemic inflammatory markers and sarcopenia: Results from the West China Health and Aging Trend Study (WCHAT). Arch. Gerontol. Geriatrics 2021, 92, 104262. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, X.; Hou, L.; Lin, X.; Qin, D.; Wang, H.; Hai, S.; Cao, L.; Dong, B. Prevalence and Risk Factors Governing the Loss of Muscle Function in Elderly Sarcopenia Patients: A longitudinal Study in China with 4 Years of Follow-Up. J. Nutr. Health Aging 2020, 24, 518–524. [Google Scholar] [CrossRef]
- Strasser, B.; Wolters, M.; Weyh, C.; Krüger, K.; Ticinesi, A. The Effects of Lifestyle and Diet on Gut Microbiota Composition, Inflammation and Muscle Performance in Our Aging Society. Nutrients 2021, 13, 2045. [Google Scholar] [CrossRef]
- Liu, C.; Cheung, W.H.; Li, J.; Chow, S.K.H.; Yu, J.; Wong, S.H.; Ip, M.; Sung, J.J.Y.; Wong, R.M.Y. Understanding the gut microbiota and sarcopenia: A systematic review. J. Cachexia Sarcopenia Muscle 2021, 12, 1393–1407. [Google Scholar] [CrossRef]
- Zhang, T.; Cheng, J.K.; Hu, Y.M. Gut microbiota as a promising therapeutic target for age-related sarcopenia. Ageing Res. Rev. 2022, 81, 101739. [Google Scholar] [CrossRef]
- Chen, L.H.; Chang, S.S.; Chang, H.Y.; Wu, C.H.; Pan, C.H.; Chang, C.C.; Chan, C.H.; Huang, H.Y. Probiotic supplementation attenuates age-related sarcopenia via the gut-muscle axis in SAMP8 mice. J. Cachexia Sarcopenia Muscle 2022, 13, 515–531. [Google Scholar] [CrossRef]
- Giron, M.; Thomas, M.; Jarzaguet, M.; Mayeur, C.; Ferrere, G.; Noordine, M.L.; Bornes, S.; Dardevet, D.; Chassard, C.; Auzeloux, I.S. Lacticaseibacillus casei CNCM I-5663 supplementation maintained muscle mass in a model of frail rodents. Front. Nutr. 2022, 9, 928798. [Google Scholar] [CrossRef]
- Deschasaux, M.; Bouter, K.E.; Prodan, A.; Levin, E.; Groen, A.K.; Herrema, H.; Tremaroli, V.; Bakker, G.J.; Attaye, I.; Sietsma, S.J.P.; et al. Depicting the composition of gut microbiota in a population with varied ethnic origins but shared geography. Nat. Med. 2018, 24, 1526–1531. [Google Scholar] [CrossRef]
- Yoon, K.; Kim, N. Roles of Sex Hormones and Gender in the Gut Microbiota. J. Neurogastroenterol. Motil. 2021, 27, 314–325. [Google Scholar] [CrossRef]
- Yang, L.; Smith, L.; Hamer, M. Gender-specific risk factors for incident sarcopenia: 8-year follow-up of the English longitudinal study of ageing. J. Epidemiol. Community Health 2019, 73, 86–88. [Google Scholar] [CrossRef]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307. [Google Scholar] [CrossRef]
- Song, J.; Zang, J.; Tang, H.; Li, W.; Wang, Z.; Zou, S.; Jia, X. Relative validity of food frequency questionnaire for estimating dietary nutrients intake. Wei Sheng Yan Jiu 2016, 45, 743–748. [Google Scholar]
- Segata, N.; Waldron, L.; Ballarini, A.; Narasimhan, V.; Jousson, O.; Huttenhower, C. Metagenomic microbial community profiling using unique clade-specific marker genes. Nat. Methods 2012, 9, 811–814. [Google Scholar] [CrossRef]
- Segata, N.; Izard, J.; Waldron, L.; Gevers, D.; Miropolsky, L.; Garrett, W.S.; Huttenhower, C. Metagenomic biomarker discovery and explanation. Genome Biol. 2011, 12, R60. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Sayer, A.A. Sarcopenia. Lancet 2019, 393, 2636–2646. [Google Scholar] [CrossRef]
- De Sire, R.; Rizzatti, G.; Ingravalle, F.; Pizzoferrato, M.; Petito, V.; Lopetuso, L.; Graziani, C.; Sire, A.; Mentella, M.C.; Mele, M.C.; et al. Skeletal muscle-gut axis: Emerging mechanisms of sarcopenia for intestinal and extra intestinal diseases. Minerva Gastroenterol. Dietol. 2018, 64, 351–362. [Google Scholar] [CrossRef]
- Zhang, X.; Shi, L.; Li, Q.; Song, C.; Han, N.; Yan, T.; Zhang, L.; Ren, D.; Zhao, Y.; Yang, X. Caloric Restriction, Friend or Foe: Effects on Metabolic Status in Association with the Intestinal Microbiome and Metabolome. J. Agric. Food Chem. 2022, 70, 14061–14072. [Google Scholar] [CrossRef]
- Ni, Y.; Yang, X.; Zheng, L.; Wang, Z.; Wu, L.; Jiang, J.; Yang, T.; Ma, L.; Fu, Z. Lactobacillus and Bifidobacterium Improves Physiological Function and Cognitive Ability in Aged Mice by the Regulation of Gut Microbiota. Mol. Nutr. Food Res. 2019, 63, e1900603. [Google Scholar] [CrossRef] [PubMed]
- Tominaga, K.; Tsuchiya, A.; Nakano, O.; Kuroki, Y.; Oka, K.; Minemura, A.; Matsumoto, A.; Takahashi, M.; Kadota, Y.; Tochio, T.; et al. Increase in muscle mass associated with the prebiotic effects of 1-kestose in super-elderly patients with sarcopenia. Biosci. Microbiota Food Health 2021, 40, 150–155. [Google Scholar] [CrossRef]
- Wang, I.K.; Wu, Y.Y.; Yang, Y.F.; Ting, I.W.; Lin, C.C.; Yen, T.H.; Chen, J.H.; Wang, C.H.; Huang, C.C.; Lin, H.C. The effect of probiotics on serum levels of cytokine and endotoxin in peritoneal dialysis patients: A randomised, double-blind, placebo-controlled trial. Benef. Microbes 2015, 6, 423–430. [Google Scholar] [CrossRef]
- Montazeri-Najafabady, N.; Ghasemi, Y.; Dabbaghmanesh, M.H.; Talezadeh, P.; Koohpeyma, F.; Gholami, A. Supportive Role of Probiotic Strains in Protecting Rats from Ovariectomy-Induced Cortical Bone Loss. Probiotics. Probiotics Antimicrob. Proteins 2019, 11, 1145–1154. [Google Scholar] [CrossRef]
- Abdelhamid, A.G.; El-Dougdoug, N.K. Comparative genomics of the gut commensal Bifidobacterium bifidum reveals adaptation to carbohydrate utilization. Biochem. Biophys. Res. Commun. 2021, 547, 155–161. [Google Scholar] [CrossRef]
- Zafar, H.; Saier, M.J. Gut bacteroides species in health and disease. Gut Microbes 2021, 13, 1–20. [Google Scholar] [CrossRef]
- Walther, B.; Karl, J.P.; Booth, S.L.; Boyaval, P. Menaquinones, bacteria, and the food supply: The relevance of dairy and fermented food products to vitamin K requirements. Adv. Nutr. 2013, 4, 463–473. [Google Scholar] [CrossRef]
- Fujita, Y.; Iki, M.; Tamaki, J.; Kouda, K.; Yura, A.; Kadowaki, E.; Sato, Y.; Moon, J.S.; Tomioka, K.; Okamoto, N.; et al. Association between vitamin K intake from fermented soybeans, natto, and bone mineral density in elderly Japanese men: The Fujiwara-kyo Osteoporosis Risk in Men (FORMEN) study. Osteoporos. Int. 2012, 23, 705–714. [Google Scholar] [CrossRef]
- Walker, A.W.; Sanderson, J.D.; Churcher, C.; Parkes, G. High-throughput clone library analysis of the mucosa-associated microbiota reveals dysbiosis and differences between inflamed and non-inflamed regions of the intestine in inflammatory bowel disease. BMC Microbiol. 2011, 11, 7. [Google Scholar] [CrossRef]
- Landi, F.; Calvani, R.; Lorenzi, M.; Martone, A.M.; Tosato, M.; Drey, M.; Angelo, E.D.; Capoluongo, E.; Russo, A.; Bernabei, R.; et al. Serum levels of C-terminal agrin fragment (CAF) are associated with sarcopenia in older multimorbid community-dwellers: Results from the ilSIRENTE study. Exp. Gerontol. 2016, 79, 31–36. [Google Scholar] [CrossRef]
- Bischoff, S.C.; Barbara, G.; Buurman, W.; Ockhuizen, T.; Schulzke, J.D.; Serino, M.; Tilg, H.; Watson, A.; Wells, J.M. Intestinal permeability--a new target for disease prevention and therapy. BMC Gastroenterol. 2014, 14, 189. [Google Scholar] [CrossRef]
- Fielding, R.A.; Reeves, A.R.; Jasuja, R.; Liu, C.; Barrett, B.B.; Lustgarten, M.S. Muscle strength is increased in mice that are colonized with microbiota from high-functioning older adults. Exp. Gerontol. 2019, 127, 110722. [Google Scholar] [CrossRef]
| Variable | Control | Case | F/X2 | p |
|---|---|---|---|---|
| Age, years | 68.7 ± 3.4 | 68.4 ± 3.5 | 0.19 | 0.661 |
| Educational level, n (%) | 7.42 | 0.024 | ||
| High school and above | 25 (50) | 12 (24) | ||
| Junior high school | 22 (44) | 32 (64) | ||
| Primary school and illiterate | 3 (6) | 6 (12) | ||
| Marital status, n (%) | 0.64 | 0.424 | ||
| Married | 43 (86) | 40 (80) | ||
| Divorced or widowed | 7 (14) | 10 (20) | ||
| Pre-retirement occupation, n (%) | 0.19 | 0.656 | ||
| Mental work mainly | 37 (74) | 35 (70) | ||
| Physical labor mainly | 13 (26) | 15 (30) | ||
| Smoking, n(%) | 0.34 | 0.558 | ||
| Smoker | 1 (2) | 2 (4) | ||
| Nonsmoker | 49 (98) | 48 (96) | ||
| Height, cm | 157.8 ± 4.9 | 156.8 ± 5.2 | 1.08 | 0.302 |
| Weight, kg | 60.0 ± 6.3 | 55.5 ± 6.7 | 11.99 | 0.001 |
| BMI, kg/m2 | 24.1 ± 2.4 | 22.5 ± 2.3 | 10.49 | 0.002 |
| BMI group | 3.87 | 0.145 | ||
| Underweight | 1 (2) | 3 (6) | ||
| Normal | 24 (48) | 31 (62) | ||
| Overweight | 25 (50) | 16 (32) | ||
| Grip strength, kg | 20.9 ± 1.2 | 16.3 ± 1.8 | 233.34 | <0.001 |
| Average daily duration of moderate physical activity, median (P25,P75) | 0.0 (0.0, 30.0) | 0.0 (0.0, 5.4) | 2.47 | 0.119 |
| Variable | Control | Case | F/X2 | p |
|---|---|---|---|---|
| Energy, kJ | 8334.3 ± 2732.0 | 7095.5 ± 3234.7 | 4.28 | 0.041 |
| Total protein, g | 88.9 ± 34.6 | 74.3 ± 36.9 | 4.18 | 0.044 |
| High-quality protein, g | 53.1 ± 26.4 | 40 ± 23.5 | 6.81 | 0.010 |
| Fat, g | 57.2 ± 22.5 | 53.3 ± 30.0 | 0.54 | 0.464 |
| Ca, mg | 846.7 ± 502.8 | 691.7 ± 446.2 | 2.66 | 0.106 |
| Vitamin D, IU | 1.1 ± 6.0 | 1.1 ± 3.9 | 0.01 | 0.990 |
| Soybean and its products, g | 9.1 (4.9, 20.9) | 9.3 (5.0, 14.4) | 0.524 | 0.600 |
| Milk and its products, g | 240.0 (113.9, 303.2) | 180.9 (0.0, 5.4) | 0.790 | 0.430 |
| Vegetable, g | 225.9 (123.3, 333.3) | 205.8 (147.0 319.5) | 0.059 | 0.953 |
| Fruit, g | 124.4 (76.7, 226.3) | 96.5 (53.5, 236.9) | 0.900 | 0.368 |
| Poultry and meat, g | 63.8 (41.2, 103.8) | 43.0 (24.1, 82.1) | 1.958 | 0.050 |
| Fish, g | 41.7 (27.1, 64.4) | 37.2 (24.3, 95.9) | 0.407 | 0.684 |
| Variable | Control | Case | F/X2 | p |
|---|---|---|---|---|
| Skeletal muscle mass, kg | 16.9 ± 1.8 | 13.5 ± 1.3 | 120.03 | <0.001 |
| Body fat percentage, % | 35.8 ± 5.6 | 35.3 ± 5.4 | 0.22 | 0.640 |
| Skeletal muscle mass/weight | 0.30; ± 0.02 | 0.24 ± 0.02 | 8.11 | <0.001 |
| Skeletal muscle mass/BMI | 0.71 ± 0.08 | 0.60 ± 0.08 | 44.32 | <0.001 |
| Skeletal muscle mass/body fat percentage | 0.49 ± 0.1 | 0.40 ± 0.08 | 27.26 | <0.001 |
| Variable | AUC | 95% CI | Cutoff | Youden Index | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| Species__Bifidobacterium_longum | 0.647 | 0.539–0.756 | 0.19 | 0.271 | 0.531 | 0.740 |
| Species__Prevotella_copri | 0.372 | 0.261–0.484 | 0.024 | 0.021 | 0.041 | 0.980 |
| Reference Group | Feature | Coefficient | p |
|---|---|---|---|
| Control | Strain__Prevotella_copri_GCF_000157935 | 0.126 | 0.001 |
| Control | Strain__Bifidobacterium_bifidum_unclassified | −0.148 | 0.020 |
| Control | Genus__Atopobium | −0.019 | 0.027 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Z.; Xu, X.; Deji, Y.; Gao, S.; Wu, C.; Song, Q.; Shi, Z.; Xiang, X.; Zang, J.; Su, J. Bifidobacterium as a Potential Biomarker of Sarcopenia in Elderly Women. Nutrients 2023, 15, 1266. https://doi.org/10.3390/nu15051266
Wang Z, Xu X, Deji Y, Gao S, Wu C, Song Q, Shi Z, Xiang X, Zang J, Su J. Bifidobacterium as a Potential Biomarker of Sarcopenia in Elderly Women. Nutrients. 2023; 15(5):1266. https://doi.org/10.3390/nu15051266
Chicago/Turabian StyleWang, Zhengyuan, Xin Xu, Yangzong Deji, Shanxi Gao, Chunxiang Wu, Qi Song, Zehuan Shi, Xuesong Xiang, Jiajie Zang, and Jin Su. 2023. "Bifidobacterium as a Potential Biomarker of Sarcopenia in Elderly Women" Nutrients 15, no. 5: 1266. https://doi.org/10.3390/nu15051266
APA StyleWang, Z., Xu, X., Deji, Y., Gao, S., Wu, C., Song, Q., Shi, Z., Xiang, X., Zang, J., & Su, J. (2023). Bifidobacterium as a Potential Biomarker of Sarcopenia in Elderly Women. Nutrients, 15(5), 1266. https://doi.org/10.3390/nu15051266






