Nuts in the Prevention and Management of Type 2 Diabetes
Abstract
1. Introduction
2. Effect of Nut Consumption on Measures of Glucose Metabolism
3. Nuts and Diabetes Prevention
3.1. Epidemiological Evidence
3.2. Clinical Trial Evidence
4. Nuts and Diabetes Management
4.1. Epidemiological Evidence
4.2. Clinical Trial Evidence
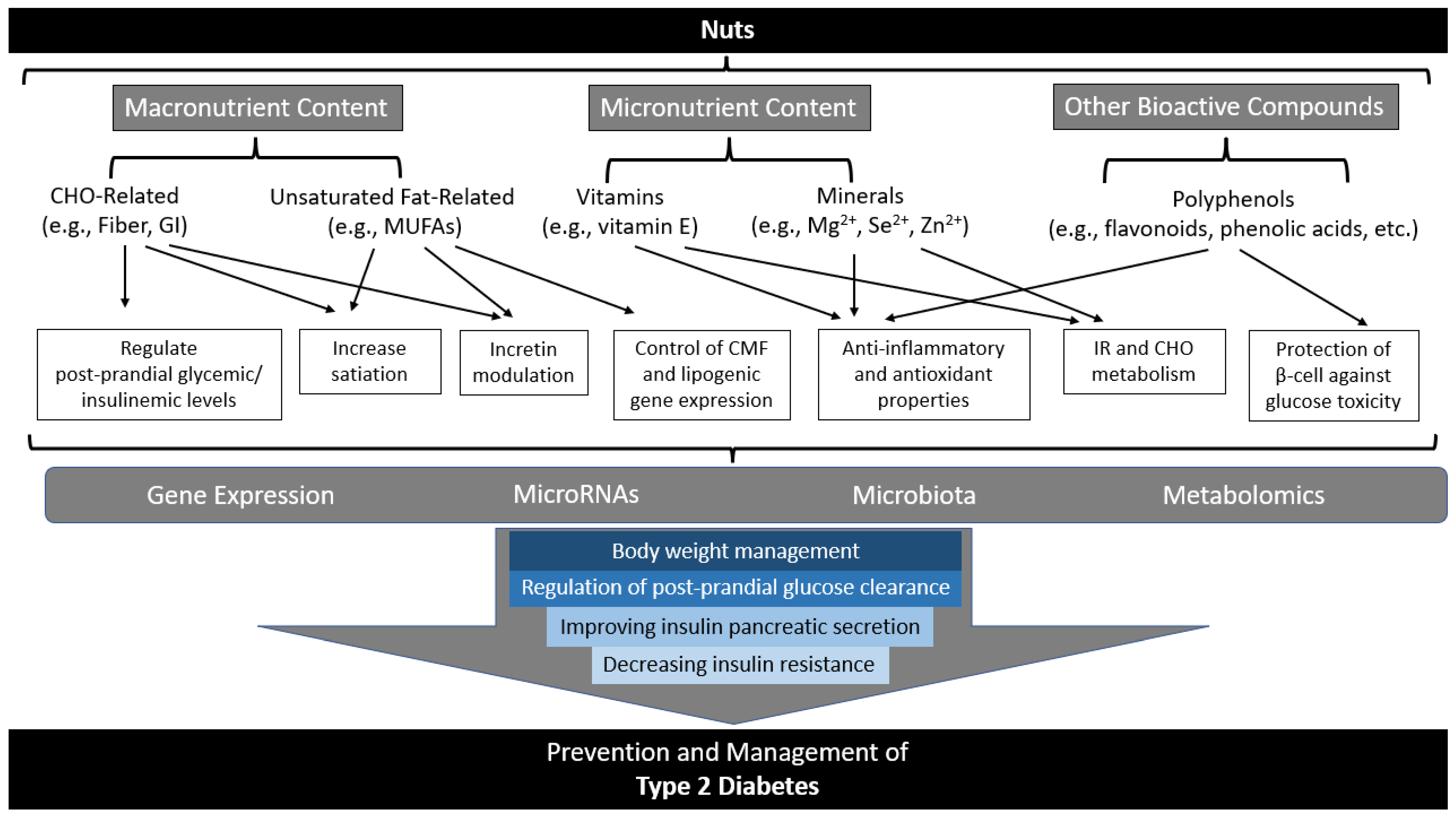
5. Possible Mechanisms of Action of Nuts in Diabetes Prevention and Management
5.1. Related to Macronutrient Composition of Nuts
5.1.1. Low Glycemic Index and Fiber
5.1.2. Fatty Acids: Unsaturated vs. Saturated
5.2. Related to Micronutrients and Other Bioactive Components of Nuts
5.2.1. Vitamins and Minerals
5.2.2. Phenolics and Other Bioactive Compounds
5.3. Related to Body Weight and Adiposity
5.4. Related to Cellular and Molecular Mechanisms of Nuts
5.4.1. Gut Microbiota
5.4.2. Gene Expressions
5.4.3. MicroRNAs
5.4.4. Metabolomics Modulation
6. Current Strengths and Limitations
7. Future Directions
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Federation. Diabetes Is “a Pandemic of Unprecedented Magnitude” Now Affecting One in 10 Adults Worldwide. Diabetes Res. Clin. Pr. 2021, 181, 109133. [Google Scholar] [CrossRef]
- International Diabetes Federation IDF Diabetes Atlas 10th Edition. Available online: www.diabetesatlas.org (accessed on 20 November 2022).
- Mann, J.I.; de Leeuw, I.; Hermansen, K.; Karamanos, B.; Karlström, B.; Katsilambros, N.; Riccardi, G.; Rivellese, A.A.; Rizkalla, S.; Slama, G.; et al. Evidence-Based Nutritional Approaches to the Treatment and Prevention of Diabetes Mellitus. Nutr. Metab. Cardiovasc. Dis. 2004, 14, 373–394. [Google Scholar] [CrossRef] [PubMed]
- Lifestyle Management: Standards of Medical Care in Diabetes. Diabetes Care 2019, 42, S46–S60. [CrossRef] [PubMed]
- Sievenpiper, J.L.; Chan, C.B.; Dworatzek, P.D.; Freeze, C.; Williams, S.L. Nutrition Therapy. Can. J. Diabetes 2018, 42, S64–S79. [Google Scholar] [CrossRef] [PubMed]
- Dyson, P.A.; Twenefour, D.; Breen, C.; Duncan, A.; Elvin, E.; Goff, L.; Hill, A.; Kalsi, P.; Marsland, N.; McArdle, P.; et al. Diabetes UK Evidence-Based Nutrition Guidelines for the Prevention and Management of Diabetes. Diabet. Med. 2018, 35, 541–547. [Google Scholar] [CrossRef]
- Venkatachalan, M.; Sathe, S.K. Chemical Composition of Selected Edible Nut Seeds. J. Agric. Food Chem. 2006, 54, 4705–4714. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada Canadian Nutrient File (CNF). Available online: https://food-nutrition.canada.ca/cnf-fce/index-eng.jsp (accessed on 20 November 2022).
- U.S. Department of Agriculture (USDA), A.R.S. FoodData Central. Available online: https://fdc.nal.usda.gov/ (accessed on 20 November 2022).
- Hosseinpour-Niazi, S.; Hosseini, S.; Mirmiran, P.; Azizi, F. Prospective Study of Nut Consumption and Incidence of Metabolic Syndrome: Tehran Lipid and Glucose Study. Nutrients 2017, 9, 1056. [Google Scholar] [CrossRef] [PubMed]
- Mazidi, M.; Vatanparast, H.; Katsiki, N.; Banach, M. The Impact of Nuts Consumption on Glucose/Insulin Homeostasis and Inflammation Markers Mediated by Adiposity Factors among American Adults. Oncotarget 2018, 9, 31173–31186. [Google Scholar] [CrossRef] [PubMed]
- Park, S.K.; Oh, C.M.; Jung, J.Y. The Association between Insulin Resistance and the Consumption of Nut Including Peanut, Pine Nut and Almonds in Working-Aged Korean Population. Public Health Nutr. 2022, 25, 1904–1911. [Google Scholar] [CrossRef]
- Becerra-Tomás, N.; Paz-Graniel, I.; Hernández-Alonso, P.; Jenkins, D.J.A.; Kendall, C.W.C.; Sievenpiper, J.L.; Salas-Salvadó, J. Nut Consumption and Type 2 Diabetes Risk: A Systematic Review and Meta-Analysis of Observational Studies. Am. J. Clin. Nutr. 2021, 113, 960–971. [Google Scholar] [CrossRef]
- Pan, A.; Sun, Q.; Manson, J.A.E.; Willett, W.C.; Hu, F.B. Walnut Consumption Is Associated with Lower Risk of Type 2 Diabetes in Women. J. Nutr. 2013, 143, 512–518. [Google Scholar] [CrossRef]
- Arab, L.; Dhaliwal, S.K.; Martin, C.J.; Larios, A.D.; Jackson, N.J.; Elashoff, D. Association between Walnut Consumption and Diabetes Risk in NHANES. Diabetes Metab. Res. Rev. 2018, 34, e3031. [Google Scholar] [CrossRef]
- Cubas-Basterrechea, G.; Elío, I.; Sumalla-Cano, S.; Aparicio-Obregón, S.; González-Antón, C.T.; Muñoz-Cacho, P. The Regular Consumption of Nuts Is Associated with a Lower Prevalence of Abdominal Obesity and Metabolic Syndrome in Older People from the North of Spain. Int. J. Environ. Res. Public Health 2022, 19, 1256. [Google Scholar] [CrossRef]
- Micek, A.; Godos, J.; Cernigliaro, A.; Cincione, R.I.; Buscemi, S.; Libra, M.; Galvano, F.; Grosso, G. Total Nut, Tree Nut, and Peanut Consumption and Metabolic Status in Southern Italian Adults. Int. J. Environ. Res. Public Health 2021, 18, 1847. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Guasch-Ferré, M.; Hu, Y.; Li, Y.; Hu, F.B.; Rimm, E.B.; Manson, J.A.E.; Rexrode, K.M.; Sun, Q. Nut Consumption in Relation to Cardiovascular Disease Incidence and Mortality among Patients with Diabetes Mellitus. Circ. Res. 2019, 124, 920–929. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Keum, N.N.; Giovannucci, E.; Fadnes, L.T.; Boffetta, P.; Greenwood, D.C.; Tonstad, S.; Vatten, L.J.; Riboli, E.; Norat, T. Nut Consumption and Risk of Cardiovascular Disease, Total Cancer, All-Cause and Cause-Specific Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. BMC. Med. 2016, 14, 207. [Google Scholar] [CrossRef] [PubMed]
- Mori, A.M.; Considine, R.V.; Mattes, R.D. Acute and Second-Meal Effects of Almond Form in Impaired Glucose Tolerant Adults: A Randomized Crossover Trial. Nutr. Metab. 2011, 8, 6. [Google Scholar] [CrossRef]
- Cohen, A.E.; Johnston, C.S. Almond Ingestion at Mealtime Reduces Postprandial Glycemia and Chronic Ingestion Reduces Hemoglobin A1c in Individuals with Well-Controlled Type 2 Diabetes Mellitus. Metabolism 2011, 60, 1312–1317. [Google Scholar] [CrossRef]
- Kendall, C.W.C.; West, S.G.; Augustin, L.S.; Esfahani, A.; Vidgen, E.; Bashyam, B.; Sauder, K.A.; Campbell, J.; Chiavaroli, L.; Jenkins, A.L.; et al. Acute Effects of Pistachio Consumption on Glucose and Insulin, Satiety Hormones and Endothelial Function in the Metabolic Syndrome. Eur. J. Clin. Nutr. 2014, 68, 370–375. [Google Scholar] [CrossRef]
- Kendall, C.W.C.; Esfahani, A.; Josse, A.R.; Augustin, L.S.A.; Vidgen, E.; Jenkins, D.J.A. The Glycemic Effect of Nut-Enriched Meals in Healthy and Diabetic Subjects. Nutr. Metab. Cardiovasc. Dis. 2011, 21, S34–S39. [Google Scholar] [CrossRef]
- Godwin, N.; Roberts, T.; Hooshmand, S.; Kern, M.; Hong, M.Y. Mixed Nuts May Promote Satiety While Maintaining Stable Blood Glucose and Insulin in Healthy, Obese, and Overweight Adults in a Two-Arm Randomized Controlled Trial. J. Med. Food 2019, 22, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Moreira, A.P.B.; Teixeira, T.F.S.; Alves, R.D.M.; Peluzio, M.C.G.; Costa, N.M.B.; Bressan, J.; Mattes, R.; Alfenas, R.C.G. Effect of a High-Fat Meal Containing Conventional or High-Oleic Peanuts on Post-Prandial Lipopolysaccharide Concentrations in Overweight/Obese Men. J. Hum. Nutr. Diet. 2016, 29, 95–104. [Google Scholar] [CrossRef]
- Jenkins, D.J.A.; Kendall, C.W.C.; Marchie, A.; Josse, A.R.; Nguyen, T.H.; Faulkner, D.A.; Lapsley, K.G.; Blumberg, J.; Mayer, J. Almonds reduce biomarkers of lipid peroxidation in older hyperlipidemic subjects. J. Nutr. 2008, 138, 908–913. [Google Scholar] [CrossRef] [PubMed]
- Josse, A.R.; Kendall, C.W.C.; Augustin, L.S.A.; Ellis, P.R.; Jenkins, D.J.A. Almonds and Postprandial Glycemia-a Dose-Response Study. Metabolism 2007, 56, 400–404. [Google Scholar] [CrossRef]
- Brown, R.; Ware, L.; Gray, A.R.; Chisholm, A.; Tey, S.L. Snacking on Almonds Lowers Glycaemia and Energy Intake Compared to a Popular High-carbohydrate Snack Food: An Acute Randomised Crossover Study. Int. J. Environ. Res. Public Health 2021, 18, 10989. [Google Scholar] [CrossRef]
- Bodnaruc, A.M.; Prud’homme, D.; Giroux, I. Acute Effects of an Isocaloric Macronutrient-Matched Breakfast Meal Containing Almonds on Glycemic, Hormonal and Appetite Responses in Men with Type 2 Diabetes: A Randomized Cross-over Study. Appl. Physiol. Nutr. Metab. 2020, 45, 520–529. [Google Scholar] [CrossRef]
- Muley, A.; Fernandez, R.; Ellwood, L.; Muley, P.; Shah, M. Effect of Tree Nuts on Glycemic Outcomes in Adults with Type 2 Diabetes Mellitus: A Systematic Review. JBI. Evid. Synth. 2021, 19, 966–1002. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Bulló, M.; Babio, N.; Martínez-González, M.Á.; Ibarrola-Jurado, N.; Basora, J.; Estruch, R.; Covas, M.I.; Corella, D.; Arós, F.; et al. Reduction in the Incidence of Type 2 Diabetes with the Mediterranean Diet: Results of the PREDIMED-Reus Nutrition Intervention Randomized Trial. Diabetes Care 2011, 34, 14–19, Erratum in Diabetes Care 2018, 41, 2259–2260. [Google Scholar] [CrossRef] [PubMed]
- Salas-Salvadó, J.; Bulló, M.; Estruch, R.; Ros, E.; Covas, M.-I.; ria Ibarrola-Jurado, N.; Corella, D.; Aró, F.; Gó mez-Gracia, E.; Ruiz-Gutiérrez, V.; et al. Prevention of Diabetes with Mediterranean Diets. A Subgroup Analysis of a Randomized Trial. Ann. Intern. Med. 2014, 160, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Nowrouzi-Sohrabi, P.; Hassanipour, S.; Sisakht, M.; Daryabeygi-Khotbehsara, R.; Savardashtaki, A.; Fathalipour, M. The Effectiveness of Pistachio on Glycemic Control and Insulin Sensitivity in Patients with Type 2 Diabetes, Prediabetes and Metabolic Syndrome: A Systematic Review and Meta-Analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1589–1595. [Google Scholar] [CrossRef] [PubMed]
- Viguiliouk, E.; Kendall, C.W.C.; Mejia, S.B.; Cozma, A.I.; Ha, V.; Mirrahimi, A.; Jayalath, V.H.; Augustin, L.S.A.; Chiavaroli, L.; Leiter, L.A.; et al. Effect of Tree Nuts on Glycemic Control in Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Dietary Trials. PLoS ONE 2014, 9, e103376, Corrected in PLoS ONE 2014, 9, e109224. [Google Scholar] [CrossRef] [PubMed]
- Ojo, O.; Wang, X.H.; Ojo, O.O.; Adegboye, A.R.A. The Effects of Almonds on Gut Microbiota, Glycometabolism, and Inflammatory Markers in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Nutrients 2021, 13, 3377. [Google Scholar] [CrossRef] [PubMed]
- Moosavian, S.P.; Rahimlou, M.; Rezaei Kelishadi, M.; Moradi, S.; Jalili, C. Effects of Almond on Cardiometabolic Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phytother. Res. 2022, 36, 1839–1853. [Google Scholar] [CrossRef] [PubMed]
- Ren, M.; Zhang, H.; Qi, J.; Hu, A.; Jiang, Q.; Hou, Y.; Feng, Q.; Ojo, O.; Wang, X. An Almond-Based Low Carbohydrate Diet Improves Depression and Glycometabolism in Patients with Type 2 Diabetes through Modulating Gut Microbiota and Glp-1: A Randomized Controlled Trial. Nutrients 2020, 12, 3036. [Google Scholar] [CrossRef]
- dos Santos, J.L.; Portal, V.L.; Markoski, M.M.; de Quadros, A.S.; Bersch-Ferreira, Â.; Marcadenti, A. Effect of Pecan Nuts and Extra-Virgin Olive Oil on Glycemic Profile and Nontraditional Anthropometric Indexes in Patients with Coronary Artery Disease: A Randomized Clinical Trial. Eur. J. Clin. Nutr. 2022, 76, 827–834. [Google Scholar] [CrossRef]
- Tindall, A.M.; Johnston, E.A.; Kris-Etherton, P.M.; Petersen, K.S. The Effect of Nuts on Markers of Glycemic Control: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am. J. Clin. Nutr. 2019, 109, 297–314. [Google Scholar] [CrossRef]
- Jenkins, D.J.A.; Kendall, C.W.C.; Josse, A.R.; Salvatore, S.; Brighenti, F.; Augustin, L.S.A.; Ellis, P.R.; Vidgen, E.; Rao, A.V. Almonds Decrease Postprandial Glycemia, Insulinemia, and Oxidative Damage in Healthy Individuals. J. Nutr. 2006, 136, 2987–2992. [Google Scholar] [CrossRef]
- Kendall, C.W.C.; Josse, A.R.; Esfahani, A.; Jenkins, D.J.A. The Impact of Pistachio Intake Alone or in Combination with High-Carbohydrate Foods on Post-Prandial Glycemia. Eur. J. Clin. Nutr. 2011, 65, 696–702. [Google Scholar] [CrossRef]
- Blanco Mejia, S.; Kendall, C.W.C.; Viguiliouk, E.; Augustin, L.S.; Ha, V.; Cozma, A.I.; Mirrahimi, A.; Maroleanu, A.; Chiavaroli, L.; Leiter, L.A.; et al. Effect of Tree Nuts on Metabolic Syndrome Criteria: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. BMJ. Open 2014, 4, 4660. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G.; Iqbal, K.; Schwedhelm, C.; Boeing, H. Food Groups and Intermediate Disease Markers: A Systematic Review and Network Meta-Analysis of Randomized Trials. Am. J. Clin. Nutr. 2018, 108, 576–586. [Google Scholar] [CrossRef] [PubMed]
- Eslami, O.; Khorramrouz, F.; Sohouli, M.; Bagheri, N.; Shidfar, F.; Fernandez, M.L. Effect of Nuts on Components of Metabolic Syndrome in Healthy Adults with Overweight/Obesity: A Systematic Review and Meta-Analysis. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 2459–2469. [Google Scholar] [CrossRef]
- Mateș, L.; Popa, D.S.; Rusu, M.E.; Fizeșan, I.; Leucuța, D. Walnut Intake Interventions Targeting Biomarkers of Metabolic Syndrome and Inflammation in Middle-Aged and Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Antioxidants 2022, 11, 1412. [Google Scholar] [CrossRef] [PubMed]
- Neale, E.P.; Guan, V.; Tapsell, L.C.; Probst, Y.C. Effect of Walnut Consumption on Markers of Blood Glucose Control: A Systematic Review and Meta-Analysis. Br. J. Nutr. 2020, 124, 641–653. [Google Scholar] [CrossRef]
- Jamshidi, S.; Moradi, Y.; Nameni, G.; Mohsenpour, M.A.; Vafa, M. Effects of Cashew Nut Consumption on Body Composition and Glycemic Indices: A Meta-Analysis and Systematic Review of Randomized Controlled Trials. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 605–613. [Google Scholar] [CrossRef]
- Parilli-Moser, I.; Hurtado-Barroso, S.; Guasch-Ferré, M.; Lamuela-Raventós, R.M. Effect of Peanut Consumption on Cardiovascular Risk Factors: A Randomized Clinical Trial and Meta-Analysis. Front. Nutr. 2022, 9. [Google Scholar] [CrossRef] [PubMed]
- Asbaghi, O.; Moodi, V.; Neisi, A.; Shirinbakhshmasoleh, M.; Abedi, S.; Oskouie, F.H.; Eslampour, E.; Ghaedi, E.; Miraghajani, M. The Effect of Almond Intake on Glycemic Control: A Systematic Review and Dose–Response Meta-Analysis of Randomized Controlled Trials. Phytother. Res. 2022, 36, 395–414. [Google Scholar] [CrossRef]
- Lee-Bravatti, M.A.; Wang, J.; Avendano, E.E.; King, L.; Johnson, E.J.; Raman, G. Almond Consumption and Risk Factors for Cardiovascular Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2019, 10, 1076–1088. [Google Scholar] [CrossRef] [PubMed]
- Petersen, K.S.; Murphy, J.; Whitbread, J.; Clifton, P.M.; Keogh, J.B. The Effect of a Peanut-Enriched Weight Loss Diet Compared to a Low-Fat Weight Loss Diet on Body Weight, Blood Pressure, and Glycemic Control: A Randomized Controlled Trial. Nutrients 2022, 14, 2986. [Google Scholar] [CrossRef]
- Caldas, A.P.S.; Rocha, D.M.U.P.; Dionísio, A.P.; Hermsdorff, H.H.M.; Bressan, J. Brazil and Cashew Nuts Intake Improve Body Composition and Endothelial Health in Women at Cardiometabolic Risk (Brazilian Nuts Study): A Randomised Controlled Trial. Br. J. Nutr. 2022, 128, 1747–1757. [Google Scholar] [CrossRef]
- Luo, C.; Zhang, Y.; Ding, Y.; Shan, Z.; Chen, S.; Yu, M.; Hu, F.B.; Liu, L. Nut Consumption and Risk of Type 2 Diabetes, Cardiovascular Disease, and All-Cause Mortality: A Systematic Review and Meta-Analysis. Am. J. Clin. Nutr. 2014, 100, 256–269. [Google Scholar] [CrossRef]
- Guo, K.; Zhou, Z.; Jiang, Y.; Li, W.; Li, Y. Meta-Analysis of Prospective Studies on the Effects of Nut Consumption on Hypertension and Type 2 Diabetes Mellitus. J. Diabetes 2015, 7, 202–212. [Google Scholar] [CrossRef]
- Wu, L.; Wang, Z.; Zhu, J.; Murad, A.L.; Prokop, L.J.; Murad, M.H. Nut Consumption and Risk of Cancer and Type 2 Diabetes: A Systematic Review and Meta-Analysis. Nutr. Rev. 2015, 73, 409–425. [Google Scholar] [CrossRef]
- Zhou, D.; Yu, H.; He, F.; Reilly, K.H.; Zhang, J.; Li, S.; Zhang, T.; Wang, B.; Ding, Y.; Xi, B. Nut Consumption in Relation to Cardiovascular Disease Risk and Type 2 Diabetes: A Systematic Review and Meta-Analysis of Prospective Studies. Am. J. Clin. Nutr. 2014, 100, 270–277. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G.; Lampousi, A.M.; Knüppel, S.; Iqbal, K.; Schwedhelm, C.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food Groups and Risk of Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Prospective Studies. Eur. J. Epidemiol. 2017, 32, 363–375. [Google Scholar] [CrossRef]
- Afshin, A.; Micha, R.; Khatibzadeh, S.; Mozaffarian, D. Consumption of Nuts and Legumes and Risk of Incident Ischemic Heart Disease, Stroke, and Diabetes: A Systematic Review and Meta-Analysis. Am. J. Clin. Nutr. 2014, 100, 278–288. [Google Scholar] [CrossRef]
- Hernández-Alonso, P.; Camacho-Barcia, L.; Bulló, M.; Salas-Salvadó, J. Nuts and Dried Fruits: An Update of Their Beneficial Effects on Type 2 Diabetes. Nutrients 2017, 9, 673. [Google Scholar] [CrossRef]
- Jenkins, D.J.A.; Hu, F.B.; Tapsell, L.C.; Josse, A.R.; Kendall, C.W.C. Possible Benefit of Nuts in Type 2 Diabetes. J. Nutr. 2008, 138, 1752S–1756S. [Google Scholar] [CrossRef]
- Kendall, C.W.C.; Josse, A.R.; Esfahani, A.; Jenkins, D.J.A. Nuts, Metabolic Syndrome and Diabetes. Br. J. Nutr. 2010, 104, 465–473. [Google Scholar] [CrossRef]
- Calbet, J.A.; MacLean, D.A. Role of Caloric Content on Gastric Emptying in Humans. J. Physiol. 1997, 498, 553–559. [Google Scholar] [CrossRef]
- Hunt, J.N.; Stubbs, D.F. The Volume and Energy Content of Meals as Determinants of Gastric Emptying. J. Physiol. 1975, 245, 209–225. [Google Scholar] [CrossRef]
- Peracchi, M.; Gebbia, C.; Ogliari, C.; Fraquelli, M.; Vigano, R.; Baldassarri, A.; Bianchi, P.A.; Conte, D. Influence of Caloric Intake on Gastric Emptying of Solids Assessed by 13C-Octanoic Acid Breath Test. Scand. J. Gastroenterol. 2000, 35, 814–818. [Google Scholar] [CrossRef]
- Dikeman, C.L.; Fahey, G.C. Viscosity as Related to Dietary Fiber: A Review. Crit. Rev. Food Sci. Nutr. 2006, 46, 649–663. [Google Scholar] [CrossRef]
- Tolhurst, G.; Heffron, H.; Lam, Y.S.; Parker, H.E.; Habib, A.M.; Diakogiannaki, E.; Cameron, J.; Grosse, J.; Reimann, F.; Gribble, F.M. Short-Chain Fatty Acids Stimulate Glucagon-like Peptide-1 Secretion via the G-Protein-Coupled Receptor FFAR2. Diabetes 2012, 61, 364–371. [Google Scholar] [CrossRef]
- Russell, W.R.; Baka, A.; Björck, I.; Delzenne, N.; Gao, D.; Griffiths, H.R.; Hadjilucas, E.; Juvonen, K.; Lahtinen, S.; Lansink, M.; et al. Impact of Diet Composition on Blood Glucose Regulation. Crit. Rev. Food Sci. Nutr. 2016, 56, 541–590. [Google Scholar] [CrossRef]
- Heppner, K.M.; Perez-Tilve, D. GLP-1 Based Therapeutics: Simultaneously Combating T2DM and Obesity. Front. Neurosci. 2015, 9, 92. [Google Scholar] [CrossRef]
- Kim, Y.; Keogh, J.B.; Clifton, P.M. Benefits of Nut Consumption on Insulin Resistance and Cardiovascular Risk Factors: Multiple Potential Mechanisms of Actions. Nutrients 2017, 9, 1271. [Google Scholar] [CrossRef]
- Imamura, F.; Micha, R.; Wu, J.H.Y.; de Oliveira Otto, M.C.; Otite, F.O.; Abioye, A.I.; Mozaffarian, D. Effects of Saturated Fat, Polyunsaturated Fat, Monounsaturated Fat, and Carbohydrate on Glucose-Insulin Homeostasis: A Systematic Review and Meta-Analysis of Randomised Controlled Feeding Trials. PLoS Med. 2016, 13, e1002087. [Google Scholar] [CrossRef]
- Risérus, U.; Willett, W.C.; Hu, F.B. Dietary Fats and Prevention of Type 2 Diabetes. Prog. Lipid Res. 2009, 48, 44–51. [Google Scholar] [CrossRef]
- Storlien A’, L.H.; Pan, D.A.; Kriketos, A.D.; O’connor, J.; Caterson, I.D.; Cooney, G.J.; Jenkins, A.B.; Baur, L.A. Skeletal Muscle Membrane Lipids and Insulin Resistance. Lipids 1996, 31, S261–S265. [Google Scholar] [CrossRef]
- Ginsberg, B.H.; Brown, T.J.; Simon, I.; Spector, A.A. Effect of the Membrane Lipid Environment on the Properties of Insulin Receptors. Diabetes 1981, 30, 773–780. [Google Scholar] [CrossRef]
- Kien, C.L. Dietary Interventions for Metabolic Syndrome: Role of Modifying Dietary Fats. Curr. Diab. Rep. 2009, 9, 43–50. [Google Scholar] [CrossRef]
- Clarke, S.D.; Williams, L. The Multi-Dimensional Regulation of Gene Expression by Fatty Acids: Polyunsaturated Fats as Nutrient Sensors. Curr. Opin. Lipidol. 2004, 15, 13–18. [Google Scholar] [CrossRef]
- Khalili, L.; Valdes-Ramos, R.; Harbige, L.S. Effect of N-3 (Omega-3) Polyunsaturated Fatty Acid Supplementation on Metabolic and Inflammatory Biomarkers and Body Weight in Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of RCTs. Metabolites 2021, 11, 742. [Google Scholar] [CrossRef]
- Hernández-Alonso, P.; Giardina, S.; Salas-Salvadó, J.; Arcelin, P.; Bulló, M. Chronic Pistachio Intake Modulates Circulating MicroRNAs Related to Glucose Metabolism and Insulin Resistance in Prediabetic Subjects. Eur. J. Nutr. 2017, 56, 2181–2191. [Google Scholar] [CrossRef]
- Rajaram, S.; Sabaté, J. Nuts, Body Weight and Insulin Resistance. Br. J. Nutr. 2006, 96, S79–S86. [Google Scholar] [CrossRef]
- Vinceti, M.; Filippini, T.; Rothman, K.J. Selenium Exposure and the Risk of Type 2 Diabetes: A Systematic Review and Meta-Analysis. Eur. J. Epidemiol. 2018, 33, 789–810. [Google Scholar] [CrossRef]
- Zhao, J.V.; Schooling, C.M.; Zhao, J.X. The Effects of Folate Supplementation on Glucose Metabolism and Risk of Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ann. Epidemiol. 2018, 28, 249–257.e1. [Google Scholar] [CrossRef]
- Feng, J.; Wang, H.; Jing, Z.; Wang, Y.; Cheng, Y.; Wang, W.; Sun, W. Role of Magnesium in Type 2 Diabetes Mellitus. Biol. Trace. Elem. Res. 2020, 196, 74–85. [Google Scholar] [CrossRef]
- Ebrahimi Mousavi, S.; Ghoreishy, S.M.; Hemmati, A.; Mohammadi, H. Association between Magnesium Concentrations and Prediabetes: A Systematic Review and Meta-Analysis. Sci. Rep. 2021, 11, 24388. [Google Scholar] [CrossRef]
- Larsson, S.C.; Wolk, A. Magnesium Intake and Risk of Type 2 Diabetes: A Meta-Analysis. J. Intern. Med. 2007, 262, 208–214. [Google Scholar] [CrossRef]
- Kazemi, A.; Ryul Shim, S.; Jamali, N.; Hassanzadeh-Rostami, Z.; Soltani, S.; Sasani, N.; Mohsenpour, M.A.; Firoozi, D.; Basirat, R.; Hosseini, R.; et al. Comparison of Nutritional Supplements for Glycemic Control in Type 2 Diabetes: A Systematic Review and Network Meta-Analysis of Randomized Trials. Diabetes Res. Clin. Pr. 2022, 191, 110037. [Google Scholar] [CrossRef]
- Elderawi, W.A.; Naser, I.A.; Taleb, M.H.; Abutair, A.S. The Effects of Oral Magnesium Supplementation on Glycemic Response among Type 2 Diabetes Patients. Nutrients 2019, 11, 44. [Google Scholar] [CrossRef]
- Vitale, M.; Masulli, M.; Rivellese, A.A.; Bonora, E.; Cappellini, F.; Nicolucci, A.; Squatrito, S.; Antenucci, D.; Barrea, A.; Bianchi, C.; et al. Dietary Intake and Major Food Sources of Polyphenols in People with Type 2 Diabetes: The TOSCA.IT Study. Eur. J. Nutr. 2018, 57, 679–688. [Google Scholar] [CrossRef]
- Godos, J.; Marventano, S.; Mistretta, A.; Galvano, F.; Grosso, G. Dietary Sources of Polyphenols in the Mediterranean Healthy Eating, Aging and Lifestyle (MEAL) Study Cohort. Int. J. Food. Sci. Nutr. 2017, 68, 750–756. [Google Scholar] [CrossRef]
- Tresserra-Rimbau, A.; Medina-Remón, A.; Pérez-Jiménez, J.; Martínez-González, M.A.; Covas, M.I.; Corella, D.; Salas-Salvadó, J.; Gómez-Gracia, E.; Lapetra, J.; Arós, F.; et al. Dietary Intake and Major Food Sources of Polyphenols in a Spanish Population at High Cardiovascular Risk: The PREDIMED Study. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 953–959. [Google Scholar] [CrossRef]
- Xiao, J.B.; Hogger, P. Dietary Polyphenols and Type 2 Diabetes: Current Insights and Future Perspectives. Curr. Med. Chem. 2014, 22, 23–38. [Google Scholar] [CrossRef]
- Rienks, J.; Barbaresko, J.; Oluwagbemigun, K.; Schmid, M.; Nöthlings, U. Polyphenol Exposure and Risk of Type 2 Diabetes: Dose-Response Meta-Analyses and Systematic Review of Prospective Cohort Studies. Am. J. Clin. Nutr. 2018, 108, 49–61. [Google Scholar] [CrossRef]
- INC International Nut & Dried Fruit Council. Nuts & Dried Fruits Statistical Yearbook 2019/2020; Reus, Spain, 2021. Available online: https://inc.nutfruit.org/technical-projects/ (accessed on 20 November 2022).
- Wharton, S.; Pedersen, S.D.; Lau, D.C.W.; Sharma, A.M. Weight Management in Diabetes. Can. J. Diabetes 2018, 42, S124–S129. [Google Scholar] [CrossRef]
- Anderson, J.W.; Kendall, C.W.C.; Jenkins, D.J.A. Importance of Weight Management in Type 2 Diabetes: Review with Meta-Analysis of Clinical Studies. J. Am. Coll. Nutr. 2003, 22, 331–339. [Google Scholar] [CrossRef]
- Nishi, S.K.; Viguiliouk, E.; Blanco Mejia, S.; Kendall, C.W.C.; Bazinet, R.P.; Hanley, A.J.; Comelli, E.M.; Salas Salvadó, J.; Jenkins, D.J.A.; Sievenpiper, J.L. Are Fatty Nuts a Weighty Concern? A Systematic Review and Meta-Analysis and Dose–Response Meta-Regression of Prospective Cohorts and Randomized Controlled Trials. Obes. Rev. 2021, 22, e13330. [Google Scholar] [CrossRef]
- Muralidharan, J.; Galiè, S.; Hernández-Alonso, P.; Bulló, M.; Salas-Salvadó, J. Plant-Based Fat, Dietary Patterns Rich in Vegetable Fat and Gut Microbiota Modulation. Front. Nutr. 2019, 6, 157. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, E.; Lambert, K.; Stanford, J.; Neale, E.P. The Effect of Nut Consumption (Tree Nuts and Peanuts) on the Gut Microbiota of Humans: A Systematic Review. Br. J. Nutr. 2021, 125, 508–520. [Google Scholar] [CrossRef]
- Portincasa, P.; Bonfrate, L.; Vacca, M.; de Angelis, M.; Farella, I.; Lanza, E.; Khalil, M.; Wang, D.Q.H.; Sperandio, M.; di Ciaula, A. Gut Microbiota and Short Chain Fatty Acids: Implications in Glucose Homeostasis. Int. J. Mol. Sci. 2022, 23, 1105. [Google Scholar] [CrossRef]
- Khan, S.; Jena, G. The Role of Butyrate, a Histone Deacetylase Inhibitor in Diabetes Mellitus: Experimental Evidence for Therapeutic Intervention. Epigenomics 2015, 7, 669–680. [Google Scholar] [CrossRef]
- Cao, H.; Ou, J.; Chen, L.; Zhang, Y.; Szkudelski, T.; Delmas, D.; Daglia, M.; Xiao, J. Dietary Polyphenols and Type 2 Diabetes: Human Study and Clinical Trial. Crit. Rev. Food Sci. Nutr. 2019, 59, 3371–3379. [Google Scholar] [CrossRef]
- Kim, Y.A.; Keogh, J.B.; Clifton, P.M. Polyphenols and Glycemic Control. Nutrients 2016, 8, 17. [Google Scholar] [CrossRef]
- García-Mantrana, I.; Calatayud, M.; Romo-Vaquero, M.; Espín, J.C.; Selma, M.V.; Collado, M.C. Urolithin Metabotypes Can Determine the Modulation of Gut Microbiota in Healthy Individuals by Tracking Walnuts Consumption over Three Days. Nutrients 2019, 11, 2483. [Google Scholar] [CrossRef]
- Rivière, A.; Selak, M.; Lantin, D.; Leroy, F.; de Vuyst, L. Bifidobacteria and Butyrate-Producing Colon Bacteria: Importance and Strategies for Their Stimulation in the Human Gut. Front. Microbiol. 2016, 7, 979. [Google Scholar] [CrossRef]
- Bernat-Karpińska, M.; Piątkiewicz, P.; Czech, A.; Wierzbicki, P. The Expression of Particular Glucose Transporters and Insulin Resistance Indicators in the Risk Groups of Type 2 Diabetes--a Two-Year Follow-Up. Endokrynol. Pol. 2012, 63, 212–219. [Google Scholar]
- di Renzo, L.; Cioccoloni, G.; Bernardini, S.; Abenavoli, L.; Aiello, V.; Marchetti, M.; Cammarano, A.; Alipourfard, I.; Ceravolo, I.; Gratteri, S. A Hazelnut-Enriched Diet Modulates Oxidative Stress and Inflammation Gene Expression without Weight Gain. Oxid. Med. Cell. Longev. 2019, 2019, 4683723. [Google Scholar] [CrossRef]
- Ortega, F.J.; Cardona-Alvarado, M.I.; Mercader, J.M.; Moreno-Navarrete, J.M.; Moreno, M.; Sabater, M.; Fuentes-Batllevell, N.; Ramírez-Chávez, E.; Ricart, W.; Molina-Torres, J.; et al. Circulating Profiling Reveals the Effect of a Polyunsaturated Fatty Acid-Enriched Diet on Common MicroRNAs. J. Nutr. Biochem. 2015, 26, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferre, M.; Bhupathiraju, S.N.; Hu, F.B. Use of Metabolomics in Improving Assessment of Dietary Intake. Clin. Chem. 2018, 64, 82–98. [Google Scholar] [CrossRef]
- Garcia-Aloy, M.; Hulshof, P.J.M.; Estruel-Amades, S.; Osté, M.C.J.; Lankinen, M.; Geleijnse, J.M.; de Goede, J.; Ulaszewska, M.; Mattivi, F.; Bakker, S.J.L.; et al. Biomarkers of Food Intake for Nuts and Vegetable Oils: An Extensive Literature Search. Genes Nutr. 2019, 14, 7. [Google Scholar] [CrossRef]
- Guasch-Ferré, M.; Hernández-Alonso, P.; Drouin-Chartier, J.P.; Ruiz-Canela, M.; Razquin, C.; Toledo, E.; Li, J.; Dennis, C.; Wittenbecher, C.; Corella, D.; et al. Walnut Consumption, Plasma Metabolomics, and Risk of Type 2 Diabetes and Cardiovascular Disease. J. Nutr. 2021, 151, 303–311. [Google Scholar] [CrossRef]
- Willett, W. Nutritional. Epidemiology, 3rd ed.; Oxford University Press: New York, NY, USA, 2012; ISBN 9780199754038. [Google Scholar]
- Bergman, R.N. Origins and History of the Minimal Model of Glucose Regulation. Front. Endocrinol. 2021, 11, 583016. [Google Scholar] [CrossRef]
- Neale, E.P.; Tran, G.; Brown, R.C. Barriers and Facilitators to Nut Consumption: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 9127. [Google Scholar] [CrossRef]
| Variables | Finding 1 | Level of Evidence 2 | Reference |
|---|---|---|---|
| Epidemiological Evidence | |||
| Fasting blood glucose | ↓ | + | [11] |
| Plasma insulin | ↓ | + | |
| HOMA-IR | ↓ | + | [11,12] |
| HOMA-B | ↓ | + | [11] |
| HbA1c | ↓ | + | |
| OGTT | ↓ | + | |
| Diabetes incidence | ↓/↔ | + | [13,14] |
| Diabetes prevalence | ↓/↔ | + | [13,15,16,17] |
| CVD incidence in participants with T2D | ↓ | + | [18] |
| Diabetes mortality | ↓ | ++ | [19] |
| Clinical Trial Evidence | |||
| Acute Trial Evidence | |||
| In participants free of T2D: | |||
| Postprandial glycemia | ↓ | ++ | [20,21,22,23,24,25,26] |
| Postprandial insulinemia | ↓/↔ | + | [21,27,28] |
| In participants with T2D: | |||
| Postprandial glycemia | ↓ | + | [21,23,29,30] |
| Postprandial insulinemia | ↓/↔ | + | [21,29] |
| Glucose metabolic clearance rate | ↑ | + | [29] |
| Longer-term Trial Evidence | |||
| In participants free of T2D at baseline: | |||
| Diabetes incidence | ↓/↔ | + | [31,32,33] |
| In participants with T2D at baseline: | |||
| Fasting glucose | ↓ | + | [30,34,35,36,37,38,39] |
| Fasting insulin | ↔ | + | |
| HbA1c | ↓ | + | |
| HOMA-IR | ↔ | + | |
| In participants with/without T2D at baseline: | |||
| Fasting glucose | ↔ | + | [40] |
| Fasting insulin | ↓ | + | |
| HbA1c | ↔ | + | |
| HOMA-IR | ↓ | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishi, S.K.; Viguiliouk, E.; Kendall, C.W.C.; Jenkins, D.J.A.; Hu, F.B.; Sievenpiper, J.L.; Atzeni, A.; Misra, A.; Salas-Salvadó, J. Nuts in the Prevention and Management of Type 2 Diabetes. Nutrients 2023, 15, 878. https://doi.org/10.3390/nu15040878
Nishi SK, Viguiliouk E, Kendall CWC, Jenkins DJA, Hu FB, Sievenpiper JL, Atzeni A, Misra A, Salas-Salvadó J. Nuts in the Prevention and Management of Type 2 Diabetes. Nutrients. 2023; 15(4):878. https://doi.org/10.3390/nu15040878
Chicago/Turabian StyleNishi, Stephanie K., Effie Viguiliouk, Cyril W. C. Kendall, David J. A. Jenkins, Frank B. Hu, John L. Sievenpiper, Alessandro Atzeni, Anoop Misra, and Jordi Salas-Salvadó. 2023. "Nuts in the Prevention and Management of Type 2 Diabetes" Nutrients 15, no. 4: 878. https://doi.org/10.3390/nu15040878
APA StyleNishi, S. K., Viguiliouk, E., Kendall, C. W. C., Jenkins, D. J. A., Hu, F. B., Sievenpiper, J. L., Atzeni, A., Misra, A., & Salas-Salvadó, J. (2023). Nuts in the Prevention and Management of Type 2 Diabetes. Nutrients, 15(4), 878. https://doi.org/10.3390/nu15040878








