1. Introduction
Dementia was the seventh leading cause of death worldwide in 2022, with 10 million new cases reported each year [
1]. As of 2019, it is estimated that there are approximately 50–60 million people with dementia worldwide, with a predicted increase to approximately 150 million by 2050 [
2]. The global societal cost of dementia in 2019 was estimated at USD 1.3 trillion, and the growing number of people with dementia has enormous social and economic consequences [
3]. Alzheimer’s disease (AD), the most common cause of dementia, has no treatment to halt or reverse its progression, although some treatments temporarily improve symptoms [
4]. AD generally develops after a stage called mild cognitive impairment (MCI), in which there is cognitive impairment beyond the normal cognitive decline associated with aging, but not to an extent that interferes with daily life [
5]. According to the Alzheimer’s Disease Neuroimaging Initiative, the transition rate from MCI to AD is estimated to be 16.5% per year [
6]. Approximately 24% of people return to normal cognition from MCI. Therefore, it is important to take appropriate measures at the MCI stage at the latest to reduce progression to AD [
7].
Currently, no drugs are approved by the United States Food and Drug Administration for the treatment of MCI, and pharmacotherapies targeting the non-dementia stage have not yet been established. Therefore, the focus of treatment is to improve lifestyle risk factors, such as diet and exercise [
8]. Diet is considered a modifiable risk factor for the development of dementia. Many nutrients, such as unsaturated fatty acids, polyphenols, tea leaf extracts, caffeine, imidazole dipeptides, and some probiotics, have beneficial effects on the course of cognitive decline in older adults [
9,
10,
11,
12,
13].
In recent decades, research on the effects of diet on cognitive decline has shifted to dietary patterns that consider nutrient interactions and synergies, rather than the function of individual nutrients [
14]. A number of studies examining the relationship between dietary patterns and cognitive function suggest that specific food combinations may have a greater effect than individual nutrients alone [
15]. Therefore, establishing a high-quality dietary habit rich in food diversity, rather than a dietary pattern high in a single food such as staple grains, is attracting attention as a dietary strategy for disease prevention [
16]. In particular, the Mediterranean diet, Dietary Approaches to Stop Hypertension (DASH) diet, and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet, which combine these elements to reduce cognitive decline, have been actively studied and associated with lower cognitive decline and risk of AD [
17]. These dietary patterns emphasize a balanced intake of a variety of foods, including vegetables, fruits, legumes, fish, and poultry [
17].
Although nutritional intervention by changing dietary patterns is a promising approach to suppressing cognitive decline, it is difficult to apply the MIND diet and the Mediterranean Sea diet, which were developed with reference to Western dietary habits, directly to an Eastern country like Japan, because dietary habits vary greatly depending on the dietary culture of each country.
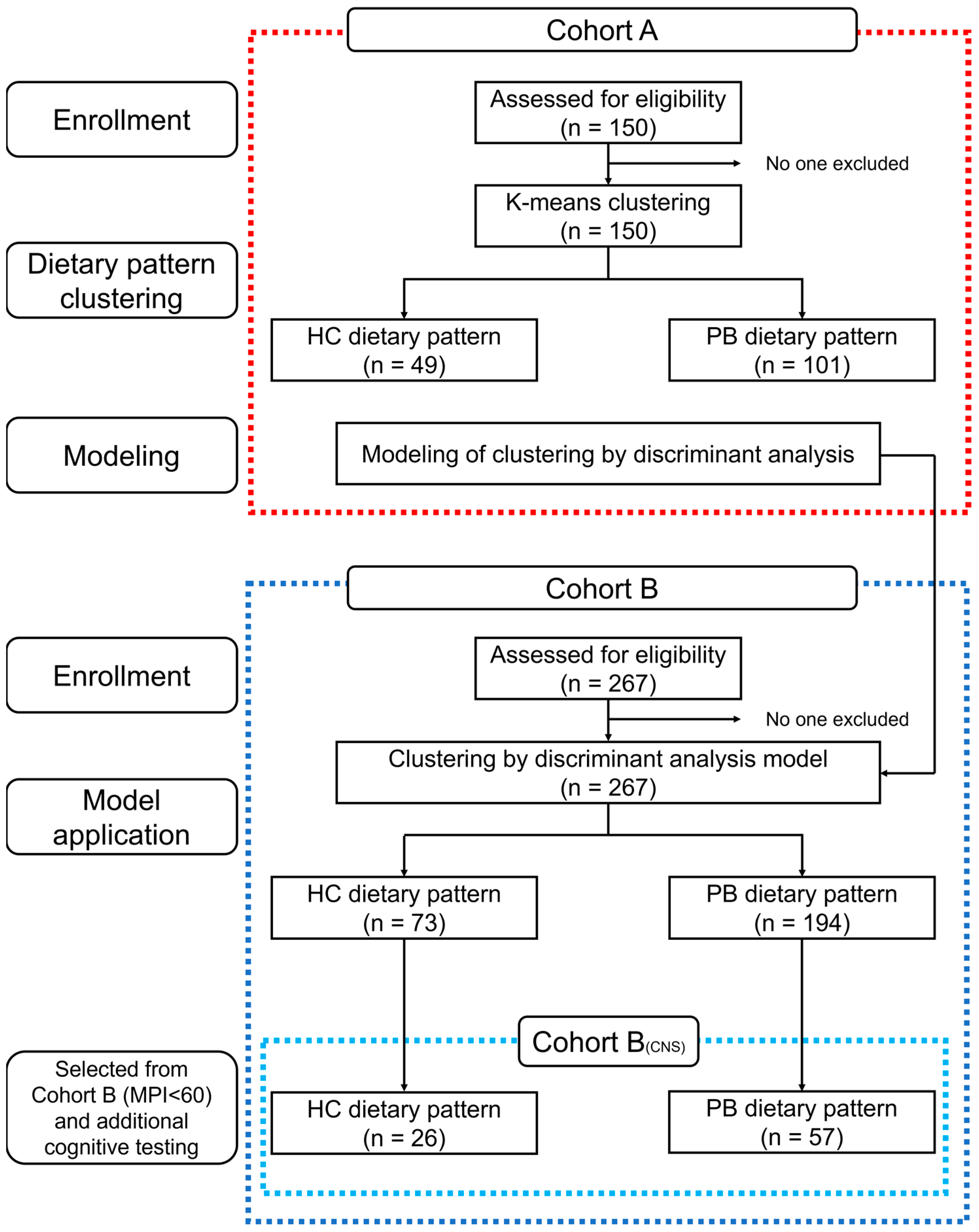
The purpose of this study was to identify dietary patterns that suppress cognitive decline that are easily applicable to elderly East Asian people, like the Japanese, by classifying dietary patterns based on the actual dietary intake of elderly Japanese through cluster analysis and examining differences in cognitive function among dietary patterns. Furthermore, to make the dietary patterns found by cluster analysis classifiable for new data, the classification was modeled by discriminant analysis and applied to a new cohort to confirm the differences in cognitive function among dietary patterns.
4. Discussion
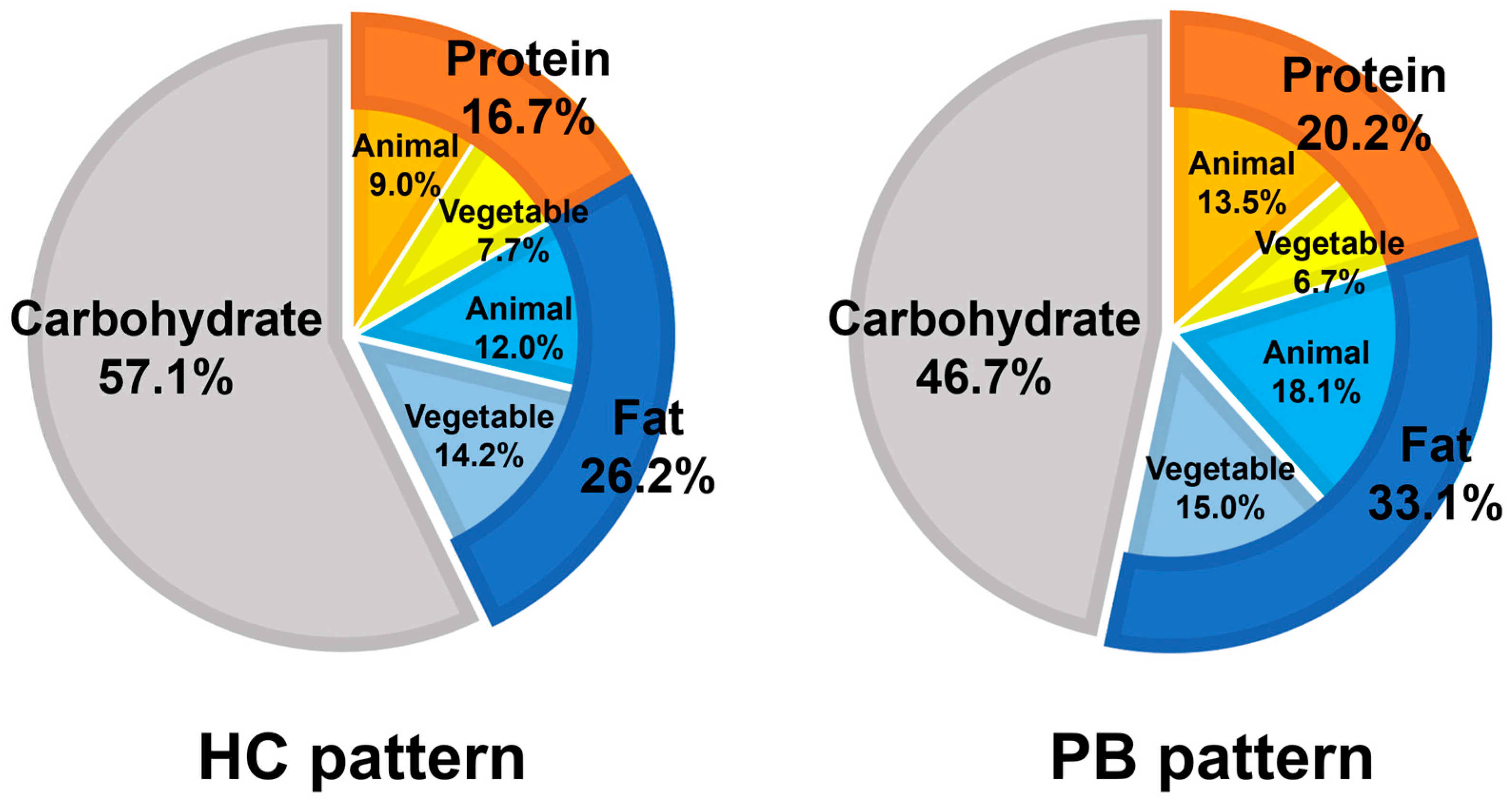
Nutritional adjustment by changing daily dietary patterns is attracting attention as a promising approach to delay the progression to AD. However, it is difficult to directly apply dietary patterns that are expected to protect cognitive functions, such as the Mediterranean, DASH, and MIND diets, to the Japanese, whose dietary culture is very different from that of Western countries. Therefore, in this study, we conducted a cluster analysis based on the food group intake of elderly Japanese to compare cognitive functions among dietary patterns with the aim of finding dietary patterns that are suitable for elderly Japanese and help maintain cognitive functions. Cluster analysis revealed patterns of a high cereal diet and a high legume, vegetable, seafood, meat, and egg diet. The HC pattern was associated with significantly lower cognitive function than the PB pattern. A classification model was then created based on the food groups with significant differences between dietary patterns and applied to the new cohort. The results showed that cognitive function was significantly lower in the HC pattern as well as in the cohort from which the model was created.
Legumes, green vegetables, other vegetables, and fish, which have a high intake in the PB pattern dietary habits, are recommended foods in the MIND diet [
28]. The Mediterranean and DASH diets slow cognitive decline [
29,
30]. The MIND diet was created by combining these two diets for neurodegenerative delay. This diet slows cognitive decline with aging, and has been suggested to reduce the risk of AD [
31]. In the BDHQ used in this study, all foods classified as legumes could be categorized as soy products. Several studies have shown that cognitive function improves with a higher intake of soy products [
32,
33]. Research on the neuroprotective effects of soy foods has primarily focused on soy isoflavones. The findings suggest that soy isoflavones may improve general cognitive function [
34,
35]. Consumption of vegetables, especially green leafy vegetables, is associated with less cognitive decline [
36,
37]. Green leafy vegetables are rich in carotenoids, flavonoids, and vitamin E, which are considered to reduce the risk of cognitive decline [
38]. Fish are rich in long-chain omega-3 fatty acids. Eating fish at least once a week reportedly reduces the risk of dementia [
39]. The results of this study are consistent with the findings of previous studies.
The PB pattern is rich in proteins and has a relatively low carbohydrate content. Carbohydrates have a much greater effect on insulin secretion than proteins or fats, and low carbohydrate diets are effective in reducing weight loss, reducing risk factors for cardiovascular disease, and improving type 2 diabetes [
40,
41,
42,
43]. Hyperinsulinemia and diabetes are significant risk factors for AD [
44]. In a clinical study on MCI, a 6-week low carbohydrate diet intervention significantly reduced fasting blood glucose, fasting insulin, and body weight, and improved verbal memory function [
45]. Hyperinsulinemia promotes central nervous system inflammation and neurodegeneration; very low carbohydrate diets were reported to reduce inflammatory factors associated with neurodegeneration [
46]. Based on these findings, Krikorian et al. [
45] suggested that, in addition to improving energy metabolism, the reduction in neuroinflammation may contribute to improved neurocognitive function in MCI. As for grains, only whole grains are recommended in the MIND diet, but foods classified as grains in the BDHQ are not intended to be whole grains. Refined grains cause blood glucose levels to rise more rapidly and produce more insulin than whole grains [
47]. In the HC pattern, a high intake of refined grains may stimulate insulin secretion and associated cognitive decline.
In addition to low carbohydrate intake, high protein intake may protect cognitive function. An increased risk of MCI or dementia has been reported in individuals with low energy intake from protein [
48]. It has also been reported that the higher the long-term protein intake, the lower the probability of developing subjective cognitive decline [
49]. In particular, animal proteins, including meat, are an excellent source of protein because of their high protein absorption rate, and a high protein diet with a high proportion of meat has been reported to significantly improve cognitive reaction time in randomized intervention trials [
50]. In particular, imidazole dipeptide, a histidine-containing dipeptide found in meats such as pork, poultry, and fish, has attracted attention as an animal peptide with cognitive function protective effects [
51]. In fact, our RCT studies in humans have shown that mixed consumption of anserine and carnosine [
52,
53,
54,
55], as well as anserine alone [
13], is beneficial for cognitive decline in older adults. Although the mechanism by which protein intake affects cognitive function is not conclusively known, dietary protein intake provides a source of amino acids necessary for neurotransmitter synthesis. For example, serotonin is synthesized from the essential amino acid phenylalanine, and lower serotonin levels are associated with worse cognitive function [
56]. Protein intake may also have indirect effects on cognitive function. Japan is the most aged country in the world, and the prevalence of frailty is known to be higher among adults over the age of 80 years than in other countries [
57]. Frailty is described as a vulnerable state in which homeostasis is poorly resolved as a result of the cumulative impairments associated with aging, and is associated with a variety of health problems, including dementia [
57,
58]. Many studies have reported an inverse association between protein intake and prevalence of frailty [
59]. A diet high in protein may be linked to the prevention of frailty and, in turn, to a reduced risk of cognitive decline.
Besides, the PB pattern has a higher intake of fats, especially animal fats, than the HC pattern. Previous studies have shown a positive correlation between cognitive function scores and fat intake, particularly oleic acid intake, in elderly Japanese [
10]. Oleic acid is a fatty acid found in animal fats as well as in olive oil. For example, lard, the fat of pork, and het, the fat of beef, contain nearly 50% oleic acid in total fat [
60]. Olive oil is a recommended food in the Mediterranean and MIND diets [
28], and about 70% of the fat in olive oil is oleic acid [
61]. Since olive oil is not as common in Japanese food culture as it is in the West, it is possible that animal fats are replacing the role of olive oil as a source of oleic acid.
It is possible that not only the single effects of these specific foods and nutrients on cognitive function, but also the synergistic effects of multiple nutrients through well-balanced intake of various foods may contribute to the improvement of cognitive function. Dietary diversity, also known as food variety, is a concept related to nutritional intake that has received much attention in terms of disease prevention in recent years and may have a unique impact on health beyond being an indicator of nutritional sufficiency [
16]. Previous studies examining the relationship between cognitive function and dietary diversity in elderly subjects have shown that cognitive decline is suppressed as dietary diversity scores increase [
62], and that higher scores for recommended food intake are associated with less cognitive decline [
63]. Because the nutritional intake capacity of the elderly is poorer than that of younger adults and is more susceptible to the effects of a monotonous diet, it is considered important to ensure that dietary diversity is not compromised to maintain brain function, especially in the elderly [
64]. Although the mechanisms related to the effects of dietary diversity on cognitive function are often unclear, it has been suggested that dietary diversity may help maintain health by increasing the diversity of the gut microbiota [
65] and ensuring a balance of various bioactive substances [
66]. To summarize our discussion thus far, the results of this study may have resulted from a diverse diet that included a variety of recommended foods, in addition to the single effects of specific foods and nutrients that have been scientifically supported to slow cognitive decline through research on diets as treatments.
Nevertheless, our study has some limitations. First, the total number of participants in this observational study was 417, which is a small sample size. However, reliability is ensured by the fact that dietary pattern classifications found in one population were applied to another population, and the same dietary patterns were confirmed to be associated with cognitive decline. Second, this was a cross-sectional study and did not show a causal relationship between dietary patterns and cognitive decline. Therefore, although we excluded people diagnosed with dementia from the participant recruitment, we cannot completely dismiss the possibility of reverse causation, that is, that dietary patterns are altered by symptoms of dementia. In addition, although the same results were obtained after adjusting for covariates in the dietary pattern classification applying the discriminant analysis model, it cannot be ruled out that other unknown confounding factors may be influencing changes in dietary patterns and cognitive function. Third, it remains unclear which nutrients in the two dietary patterns affect cognitive function and their mechanism of action. In particular, foods that differ from the recommended and discouraged foods in the well-studied dietary patterns, such as the Mediterranean, DASH, and MIND diets, should be examined in detail to determine whether they are unique to the elderly Japanese population. Finally, detailed cognitive assessment during the application phase of the classification model was performed only for participants with suspected cognitive decline. Needless to say, it would be more desirable to perform additional, detailed cognitive testing on all subjects. However, since the cognitive function of all subjects in Cohort B was already measured by MPI scores, we considered that limited resources should be spent on subjects who were already exhibiting symptoms of cognitive decline.
Despite these limitations, we believe that this study has made a significant contribution to the goal of establishing a diet that reduces cognitive decline suitable for the elderly Japanese by demonstrating dietary patterns associated with cognitive function in the elderly Japanese. Another important implication of our study is that we created a model that classifies dietary patterns according to the intake of seven food groups, and observed differences in cognitive function between dietary patterns, suggesting that simply examining the intake of certain foods may be used to predict cognitive decline in older adults.
We are currently planning an intervention study to shift older adults with HC patterns to PB patterns to prove the causal relationship between dietary patterns and cognitive function found in this study. Validation with larger sample sizes and additional research on the role of individual nutrients is needed to establish a standard diet therapy for dementia in elderly Japanese individuals.