Effects of Lacticaseibacillus paracasei Strain Shirota on Daytime Performance in Healthy Office Workers: A Double-Blind, Randomized, Crossover, Placebo-Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Test Beverages
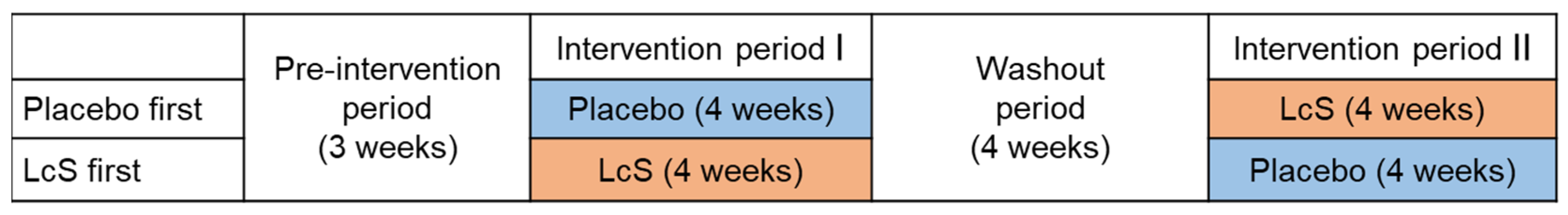
2.2. Study Design and Participants
2.3. Questionnaires
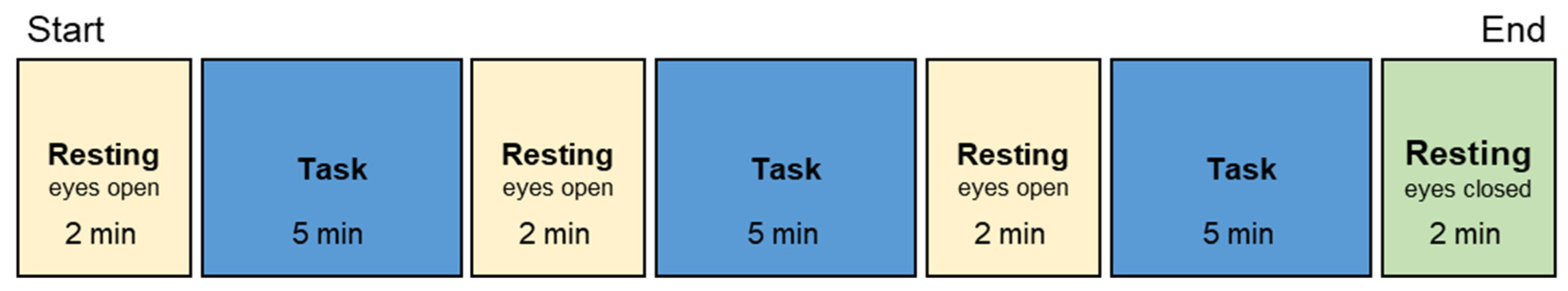
2.4. Daytime EEG and HRV Measurement
2.5. Analysis of EEG and HRV
2.6. Statistical Analysis
3. Results
3.1. Characteristics of Participants
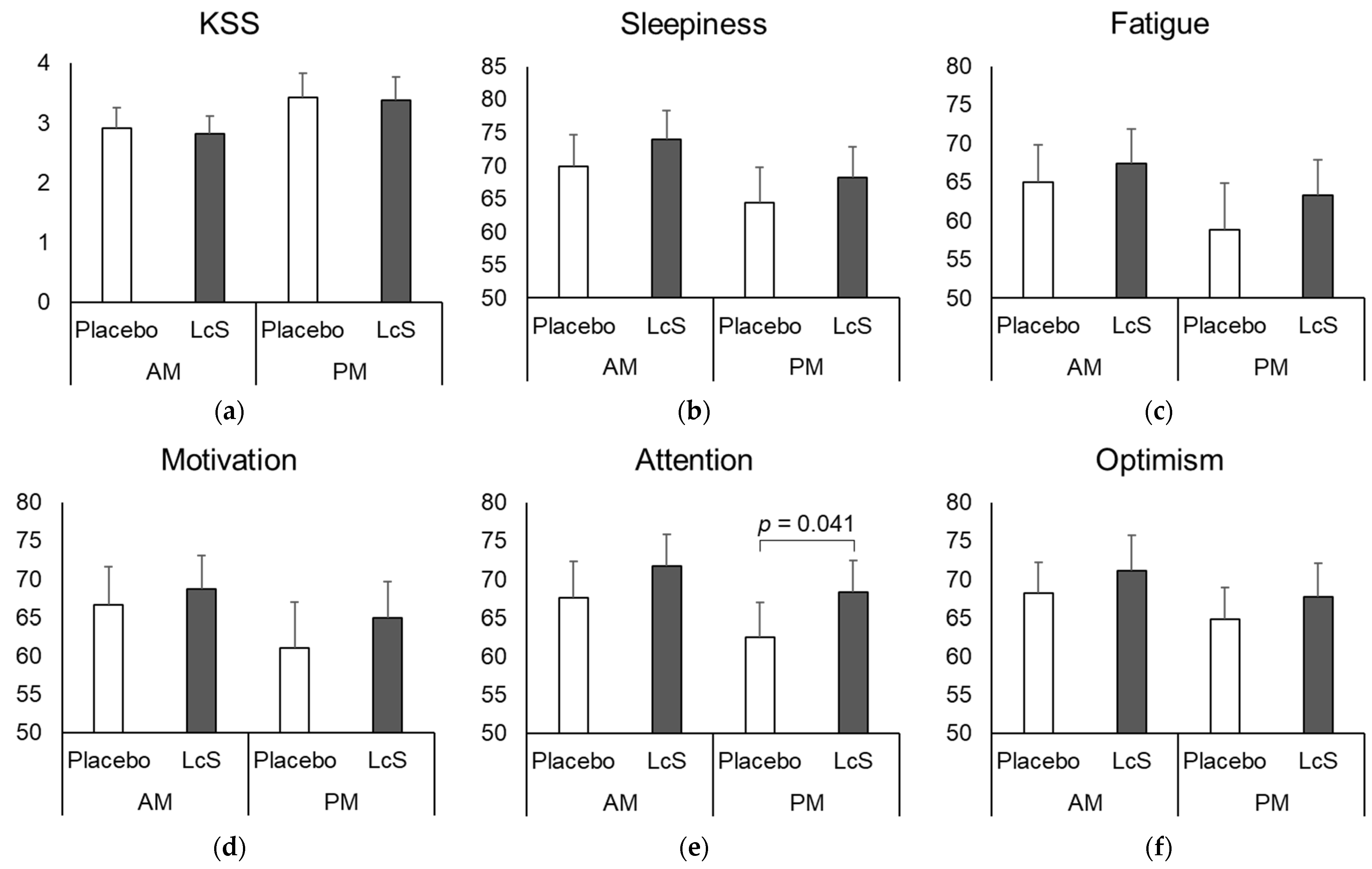
3.2. Perceived Mood
3.3. EEG
3.4. HRV
3.5. Relationship between the Perceived Mood and Physiological Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Selye, H. The general adaptation syndrome and the diseases of adaptation. J. Clin. Endocrinol. Metab. 1946, 6, 117–230. [Google Scholar] [CrossRef]
- Charmandari, E.; Tsigos, C.; Chrousos, G. Endocrinology of the stress response. Annu. Rev. Physiol. 2005, 67, 259–284. [Google Scholar] [CrossRef] [PubMed]
- Chu, B.; Marwaha, K.; Sanvictores, T.; Ayers, D. Physiology, Stress Reaction. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Furuichi, W.; Shimura, A.; Miyama, H.; Seki, T.; Ono, K.; Masuya, J.; Inoue, T. Effects of job stressors, stress response, and sleep disturbance on presenteeism in office workers. Neuropsychiatr. Dis. Treat. 2020, 16, 1827–1833. [Google Scholar] [CrossRef] [PubMed]
- Rosekind, M.R.; Gregory, K.B.; Mallis, M.M.; Brandt, S.L.; Seal, B.; Lerner, D. The cost of poor sleep: Workplace productivity loss and associated costs. J. Occup. Environ. Med. 2010, 52, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Economy. Trade and Industry of Japan Corporate Health Management Guidebook: Recommendation for Health Promotion through Cooperation and Cooperation. Revised 1st Edition. Available online: https://www.meti.go.jp/policy/mono_info_service/healthcare/kenkokeiei-guidebook2804.pdf (accessed on 24 February 2023).
- Lo, J.C.; Groeger, J.A.; Santhi, N.; Arbon, E.L.; Lazar, A.S.; Hasan, S.; von Schantz, M.; Archer, S.N.; Dijk, D.-J. Effects of partial and acute total sleep deprivation on performance across cognitive domains, individuals and circadian phase. PLoS ONE 2012, 7, e45987. [Google Scholar] [CrossRef]
- Abe, T.; Komada, Y.; Nishida, Y.; Hayashida, K.; Inoue, Y. Short sleep duration and long spells of driving are associated with the occurrence of Japanese drivers’ rear-end collisions and single-car accidents. J. Sleep Res. 2010, 19, 310–316. [Google Scholar] [CrossRef]
- Kaida, K.; Takahashi, M.; Akerstedt, T.; Nakata, A.; Otsuka, Y.; Haratani, T.; Fukasawa, K. Validation of the Karolinska sleepiness scale against performance and EEG variables. Clin. Neurophysiol. 2006, 117, 1574–1581. [Google Scholar] [CrossRef] [PubMed]
- Wutzl, B.; Golaszewski, S.M.; Leibnitz, K.; Langthaler, P.B.; Kunz, A.B.; Leis, S.; Schwenker, K.; Thomschewski, A.; Bergmann, J.; Trinka, E. Narrative Review: Quantitative EEG in disorders of consciousness. Brain Sci. 2021, 11, 697. [Google Scholar] [CrossRef]
- Von Rosenberg, W.; Chanwimalueang, T.; Adjei, T.; Jaffer, U.; Goverdovsky, V.; Mandic, D.P. Resolving ambiguities in the LF/HF ratio: LF-HF scatter plots for the categorization of mental and physical stress from HRV. Front. Physiol. 2017, 8, 360. [Google Scholar] [CrossRef]
- Sawada, Y.; Ohtomo, N.; Tanaka, Y.; Tanaka, G.; Yamakoshi, K.; Terachi, S.; Shimamoto, K.; Nakagawa, M.; Satoh, S.; Kuroda, S.; et al. New technique for time series analysis combining the maximum entropy method and non-linear least squares method: Its value in heart rate variability analysis. Med. Biol. Eng. Comput. 1997, 35, 318–322. [Google Scholar] [CrossRef]
- Al Omran, Y.; Aziz, Q. The brain-gut axis in health and disease. Adv. Exp. Med. Biol. 2014, 817, 135–153. [Google Scholar] [CrossRef]
- Holdeman, L.V.; Good, I.J.; Moore, W.E. Human fecal flora: Variation in bacterial composition within individuals and a possible effect of emotional stress. Appl. Environ. Microbiol. 1976, 31, 359–375. [Google Scholar] [CrossRef] [PubMed]
- Bailey, M.T.; Coe, C.L. Maternal separation disrupts the integrity of the intestinal microflora in infant rhesus monkeys. Dev. Psychobiol. 1999, 35, 146–155. [Google Scholar] [CrossRef]
- Sudo, N.; Chida, Y.; Aiba, Y.; Sonoda, J.; Oyama, N.; Yu, X.-N.; Kubo, C.; Koga, Y. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J. Physiol. 2004, 558, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Son, J.S.; Zheng, L.J.; Rowehl, L.M.; Tian, X.; Zhang, Y.; Zhu, W.; Litcher-Kelly, L.; Gadow, K.D.; Gathungu, G.; Robertson, C.E.; et al. Comparison of fecal microbiota in children with autism spectrum disorders and neurotypical siblings in the simons simplex collection. PLoS ONE 2015, 10, e0137725. [Google Scholar] [CrossRef]
- Aizawa, E.; Tsuji, H.; Asahara, T.; Takahashi, T.; Teraishi, T.; Yoshida, S.; Ota, M.; Koga, N.; Hattori, K.; Kunugi, H. Possible association of Bifidobacterium and Lactobacillus in the gut microbiota of patients with major depressive disorder. J. Affect. Disord. 2016, 202, 254–257. [Google Scholar] [CrossRef]
- Zheng, P.; Zeng, B.; Zhou, C.; Liu, M.; Fang, Z.; Xu, X.; Zeng, L.; Chen, J.; Fan, S.; Du, X.; et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol. Psychiatry 2016, 21, 786–796. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Wang, K.; Hu, J. Effect of probiotics on depression: A systematic review and meta-analysis of randomized controlled trials. Nutrients 2016, 8, 483. [Google Scholar] [CrossRef]
- Martínez-González, A.E.; Andreo-Martínez, P. Prebiotics, probiotics and fecal microbiota transplantation in autism: A systematic review. Rev. Psiquiatr. Salud Ment. 2020, 13, 150–164. [Google Scholar] [CrossRef]
- Li, W.; Guo, J.; Shen, Y.; Huang, L.; Leng, B.; Fan, D.; Shui, L.; Chen, C. Probiotics, prebiotics, and synbiotics for the treatment of dementia: Protocol for a systematic review. Medicine 2020, 99, e18608. [Google Scholar] [CrossRef]
- Otaka, M.; Kikuchi-Hayakawa, H.; Ogura, J.; Ishikawa, H.; Yomogida, Y.; Ota, M.; Hidese, S.; Ishida, I.; Aida, M.; Matsuda, K.; et al. Effect of Lacticaseibacillus paracasei Strain Shirota on Improvement in Depressive Symptoms, and Its Association with Abundance of Actinobacteria in Gut Microbiota. Microorganisms 2021, 9, 1026. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Wittouck, S.; Salvetti, E.; Franz, C.M.A.P.; Harris, H.M.B.; Mattarelli, P.; O’Toole, P.W.; Pot, B.; Vandamme, P.; Walter, J.; et al. A taxonomic note on the genus Lactobacillus: Description of 23 novel genera, emended description of the genus Lactobacillus Beijerinck 1901, and union of Lactobacillaceae and Leuconostocaceae. Int. J. Syst. Evol. Microbiol. 2020, 70, 2782–2858. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration. Agency Response Letter GRAS Notice No. GRN 000429. Available online: https://www.fda.gov/downloads/Food/IngredientsPackagingLabeling/GRAS/NoticeInventory/UCM309143.pdf (accessed on 30 October 2023).
- Matsumoto, K.; Takada, T.; Shimizu, K.; Moriyama, K.; Kawakami, K.; Hirano, K.; Kajimoto, O.; Nomoto, K. Effects of a probiotic fermented milk beverage containing Lactobacillus casei strain Shirota on defecation frequency, intestinal microbiota, and the intestinal environment of healthy individuals with soft stools. J. Biosci. Bioeng. 2010, 110, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Nagata, S.; Asahara, T.; Wang, C.; Suyama, Y.; Chonan, O.; Takano, K.; Daibou, M.; Takahashi, T.; Nomoto, K.; Yamashiro, Y. The effectiveness of Lactobacillus beverages in controlling infections among the residents of an aged care facility: A randomized placebo-controlled double-blind trial. Ann. Nutr. Metab. 2016, 68, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Shida, K.; Sato, T.; Iizuka, R.; Hoshi, R.; Watanabe, O.; Igarashi, T.; Miyazaki, K.; Nanno, M.; Ishikawa, F. Daily intake of fermented milk with Lactobacillus casei strain Shirota reduces the incidence and duration of upper respiratory tract infections in healthy middle-aged office workers. Eur. J. Nutr. 2017, 56, 45–53. [Google Scholar] [CrossRef]
- Nagao, F.; Nakayama, M.; Muto, T.; Okumura, K. Effects of a fermented milk drink containing Lactobacillus casei strain Shirota on the immune system in healthy human subjects. Biosci. Biotechnol. Biochem. 2000, 64, 2706–2708. [Google Scholar] [CrossRef]
- Kato-Kataoka, A.; Nishida, K.; Takada, M.; Suda, K.; Kawai, M.; Shimizu, K.; Kushiro, A.; Hoshi, R.; Watanabe, O.; Igarashi, T.; et al. Fermented milk containing Lactobacillus casei strain Shirota prevents the onset of physical symptoms in medical students under academic examination stress. Benef. Microbes 2016, 7, 153–156. [Google Scholar] [CrossRef]
- Kato-Kataoka, A.; Nishida, K.; Takada, M.; Kawai, M.; Kikuchi-Hayakawa, H.; Suda, K.; Ishikawa, H.; Gondo, Y.; Shimizu, K.; Matsuki, T.; et al. Fermented milk containing Lactobacillus casei strain Shirota preserves the diversity of the gut microbiota and relieves abdominal dysfunction in healthy medical students exposed to academic stress. Appl. Environ. Microbiol. 2016, 82, 3649–3658. [Google Scholar] [CrossRef]
- Takada, M.; Nishida, K.; Kataoka-Kato, A.; Gondo, Y.; Ishikawa, H.; Suda, K.; Kawai, M.; Hoshi, R.; Watanabe, O.; Igarashi, T.; et al. Probiotic Lactobacillus casei strain Shirota relieves stress-associated symptoms by modulating the gut–brain interaction in human and animal models. Neurogastroenterol. Motil. 2016, 28, 1027–1036. [Google Scholar] [CrossRef]
- Takada, M.; Nishida, K.; Gondo, Y.; Kikuchi-Hayakawa, H.; Ishikawa, H.; Suda, K.; Kawai, M.; Hoshi, R.; Kuwano, Y.; Miyazaki, K.; et al. Beneficial effects of Lactobacillus casei strain Shirota on academic stress-induced sleep disturbance in healthy adults: A double-blind, randomised, placebo-controlled trial. Benef. Microbes 2017, 8, 153–162. [Google Scholar] [CrossRef]
- Van Dinteren, R.; Arns, M.; Jongsma, M.L.A.; Kessels, R.P.C. P300 development across the lifespan: A systematic review and meta-analysis. PLoS ONE 2014, 9, e87347. [Google Scholar] [CrossRef] [PubMed]
- Kropotov, J.; Ponomarev, V.; Tereshchenko, E.P.; Müller, A.; Jäncke, L. Effect of aging on ERP components of cognitive control. Front. Aging Neurosci. 2016, 8, 69. [Google Scholar] [CrossRef]
- Hellerstedt, R.; Moccia, A.; Brunskill, C.M.; Bowman, H.; Bergström, Z.M. Aging reduces EEG markers of recognition despite intact performance: Implications for forensic memory detection. Cortex 2021, 140, 80–97. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, S.; Magee, M.; Stone, J.E.; Mulhall, M.D.; Collins, A.; Howard, M.E.; Lockley, S.W.; Rajaratnam, S.M.W.; Sletten, T.L. The impact of shift work on sleep, alertness and performance in healthcare workers. Sci. Rep. 2019, 9, 4635. [Google Scholar] [CrossRef] [PubMed]
- Lima, N.C.; Kirov, R.; de Almondes, K.M. Impairment of executive functions due to sleep alterations: An integrative review on the use of P300. Front. Neurosci. 2022, 16, 906492. [Google Scholar] [CrossRef] [PubMed]
- Akerstedt, T.; Gillberg, M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 1990, 52, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Iwahashi, S.; Tanaka, Y.; Fukudo, S.; Hongo, M. The development of the Japanese version of the perceived stress scale. Jpn. Soc. Psycosom. Med. 2002, 42, 459–466. [Google Scholar] [CrossRef]
- Shimokouch, M.; Kuroiw, Y.; Tobimatsu, S.; Ichikawa, G.; Yoshikawa, H.; Yamakawa, T.; Kakimoto, R.; Shibazaki, H.; Ozaki, I.; Sonoo, M.; et al. Guidelines for evoked potentials. Jpn. J. Electroencephalogr. Electromyogr. 1998, 26, 185–200. [Google Scholar]
- Ono, Y. Frequency analysis of spontaneous brain waves. In Introduction to Biological Processing with MATLAB; Corona Publishing Co., Ltd.: Tokyo, Japan, 2018; pp. 24–43. ISBN 978-4-339-07245-7. [Google Scholar]
- Takahashi, T.; Murata, T.; Hamada, T.; Omori, M.; Kosaka, H.; Kikuchi, M.; Yoshida, H.; Wada, Y. Changes in EEG and autonomic nervous activity during meditation and their association with personality traits. Int. J. Psychophysiol. 2005, 55, 199–207. [Google Scholar] [CrossRef]
- Vandoolaeghe, E.; van Hunsel, F.; Nuyten, D.; Maes, M. Auditory event related potentials in major depression: Prolonged P300 latency and increased P200 amplitude. J. Affect. Disord. 1998, 48, 105–113. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Tsuchiya, H.; Yamagata, S.; Toyoda, G.; Kobayashi, S. Event-related brain potentials in response to novel sounds in dementia. Clin. Neurophysiol. 2000, 111, 195–203. [Google Scholar] [CrossRef]
- Tokuda, H.; Sueyasu, T.; Kontani, M.; Kawashima, H.; Shibata, H.; Koga, Y. Low doses of long-chain polyunsaturated fatty acids affect cognitive function in elderly Japanese men: A randomized controlled trial. J. Oleo Sci. 2015, 64, 633–644. [Google Scholar] [CrossRef]
- Pan, J.; Takeshita, T.; Morimoto, K. Acute caffeine effect on repeatedly measured P300. Environ. Health Prev. Med. 2000, 5, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.M.; So, Y.; Lee, K.A.; Lash, A.A.; Becker, C.E. The P300 event-related potential. The effects of sleep deprivation. J. Occup. Med. 1992, 34, 1143–1152. [Google Scholar] [PubMed]
- Nakajima, K.; Hata, Y.; Osono, Y.; Hamura, M.; Kobayashi, S.; Watanuki, M. Antihypertensive Effect of Extracts of Lactobacillus casei in Patients with Hypertension. J. Clin. Biochem. Nutr. 1995, 18, 181–187. [Google Scholar] [CrossRef][Green Version]
- Tanida, M.; Imanishi, K.; Akashi, H.; Kurata, Y.; Chonan, O.; Naito, E.; Kunihiro, S.; Kawai, M.; Kato-Kataoka, A.; Shibamoto, T. Injection of Lactobacillus casei strain Shirota affects autonomic nerve activities in a tissue-specific manner, and regulates glucose and lipid metabolism in rats. J. Diabetes Investig. 2014, 5, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Tanida, M.; Takada, M.; Kato-Kataoka, A.; Kawai, M.; Miyazaki, K.; Shibamoto, T. Intragastric injection of Lactobacillus casei strain Shirota suppressed spleen sympathetic activation by central corticotrophin-releasing factor or peripheral 2-deoxy-d-glucose in anesthetized rats. Neurosci. Lett. 2016, 619, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Bravo, J.A.; Forsythe, P.; Chew, M.V.; Escaravage, E.; Savignac, H.M.; Dinan, T.G.; Bienenstock, J.; Cryan, J.F. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc. Natl. Acad. Sci. USA 2011, 108, 16050–16055. [Google Scholar] [CrossRef] [PubMed]
- Bercik, P.; Park, A.J.; Sinclair, D.; Khoshdel, A.; Lu, J.; Huang, X.; Deng, Y.; Blennerhassett, P.A.; Fahnestock, M.; Moine, D.; et al. The anxiolytic effect of Bifidobacterium longum NCC3001 involves vagal pathways for gut-brain communication. Neurogastroenterol. Motil. 2011, 23, 1132–1139. [Google Scholar] [CrossRef]
- Ishibashi, Y.; Shimura, A. Association between work productivity and sleep health: A cross-sectional study in Japan. Sleep Health 2020, 6, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare of Japan Comprehensive Survey of Living Conditions. 2019. Available online: https://www.mhlw.go.jp/toukei/list/20-21.html (accessed on 24 February 2023).
- Dwan, K.; Li, T.; Altman, D.G.; Elbourne, D. CONSORT 2010 statement: Extension to randomised crossover trials. BMJ 2019, 366, l4378. [Google Scholar] [CrossRef] [PubMed]


| Placebo First | LcS First | Total | |
|---|---|---|---|
| Number | 2 males, 4 females | 3 males, 3 females | 5 males, 7 females |
| Age (years) | 47.2 ± 7.8 | 45.5 ± 5.9 | 46.3 ± 6.6 |
| Height (cm) | 161.75 ± 7.04 | 166.50 ± 9.89 | 164.13 ± 8.55 |
| Body weight (kg) | 54.66 ± 12.08 | 58.16 ± 13.22 | 56.42 ± 12.21 |
| Body mass index | 20.71 ± 3.16 | 20.80 ± 2.89 | 20.76 ± 2.88 |
| JPSS | 18.2 ± 7.5 | 25.5 ± 11.2 | 21.8 ± 9.8 |
| PSQI | 6.7 ± 1.6 | 7.3 ± 1.8 | 7.0 ± 1.7 |
| Complaints about sleep | |||
| Sleep latency | 1/6 | 0/6 | 1/12 |
| Wake after sleep onset | 5/6 | 4/6 | 9/12 |
| Waking up too early | 3/6 | 3/6 | 6/12 |
| Sleep quality | 1/6 | 2/6 | 3/12 |
| Sleepiness on rising | 2/6 | 2/6 | 4/12 |
| Daytime sleepiness | 3/6 | 4/6 | 7/12 |
| Sleep duration | 2/6 | 2/6 | 4/12 |
| Time | Treatment | HR (bpm) | LF/HF | HF (ms2) | |||
|---|---|---|---|---|---|---|---|
| Resting (Eyes closed) | AM | Placebo | 67.8 ± 3.1 | 4.13 ± 1.20 | 321.1 ± 105.9 | ||
| LcS | 64.7 ± 3.0 | * | 3.60 ± 1.12 | 200.4 ± 37.1 | |||
| PM | Placebo | 68.0 ± 3.0 | 3.52 ± 1.45 | 390.2 ± 215.1 | |||
| LcS | 66.9 ± 4.0 | 5.28 ± 3.16 | 279.3 ± 103.7 | ||||
| Resting (Eyes open) | AM | Placebo | 67.5 ± 2.5 | 6.69 ± 1.86 | 307.9 ± 129.4 | ||
| LcS | 66.5 ± 2.8 | 4.73 ± 1.07 | 295.5 ± 90.8 | ||||
| PM | Placebo | 68.5 ± 2.7 | 5.67 ± 1.50 | 348.0 ± 142.2 | |||
| LcS | 67.0 ± 3.4 | 6.59 ± 2.50 | 352.5 ± 96.4 | ||||
| Task | AM | Placebo | 67.4 ± 2.6 | 4.55 ± 1.33 | 296.5 ± 63.7 | ||
| LcS | 65.9 ± 2.9 | 3.32 ± 1.00 | 430.2 ± 198.4 | ||||
| PM | Placebo | 68.0 ± 3.1 | 4.64 ± 1.32 | 420.9 ± 203.2 | |||
| LcS | 66.4 ± 3.4 | 3.24 ± 0.87 | * | 289.8 ± 70.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kikuchi-Hayakawa, H.; Ishikawa, H.; Suda, K.; Gondo, Y.; Hirasawa, G.; Nakamura, H.; Takada, M.; Kawai, M.; Matsuda, K. Effects of Lacticaseibacillus paracasei Strain Shirota on Daytime Performance in Healthy Office Workers: A Double-Blind, Randomized, Crossover, Placebo-Controlled Trial. Nutrients 2023, 15, 5119. https://doi.org/10.3390/nu15245119
Kikuchi-Hayakawa H, Ishikawa H, Suda K, Gondo Y, Hirasawa G, Nakamura H, Takada M, Kawai M, Matsuda K. Effects of Lacticaseibacillus paracasei Strain Shirota on Daytime Performance in Healthy Office Workers: A Double-Blind, Randomized, Crossover, Placebo-Controlled Trial. Nutrients. 2023; 15(24):5119. https://doi.org/10.3390/nu15245119
Chicago/Turabian StyleKikuchi-Hayakawa, Hiroko, Hiroshi Ishikawa, Kazunori Suda, Yusuke Gondo, Genki Hirasawa, Hayato Nakamura, Mai Takada, Mitsuhisa Kawai, and Kazunori Matsuda. 2023. "Effects of Lacticaseibacillus paracasei Strain Shirota on Daytime Performance in Healthy Office Workers: A Double-Blind, Randomized, Crossover, Placebo-Controlled Trial" Nutrients 15, no. 24: 5119. https://doi.org/10.3390/nu15245119
APA StyleKikuchi-Hayakawa, H., Ishikawa, H., Suda, K., Gondo, Y., Hirasawa, G., Nakamura, H., Takada, M., Kawai, M., & Matsuda, K. (2023). Effects of Lacticaseibacillus paracasei Strain Shirota on Daytime Performance in Healthy Office Workers: A Double-Blind, Randomized, Crossover, Placebo-Controlled Trial. Nutrients, 15(24), 5119. https://doi.org/10.3390/nu15245119





