Breastfeeding Duration Is Associated with the Risk of Tooth Loss, Chewing Difficulty, and Undernutrition among Older Korean Women: Results of the Korea National Health and Nutrition Examination Survey (KNHANES) 2013–2015
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Anthropometry, Lifestyle, Health Status, and Reproductive Factors
2.3. Number of Teeth and Chewing Ability
2.4. Dietary Intake
2.5. Statistical Analyses
3. Results
3.1. Characteristics of Study Participants
3.2. Number of Teeth and Chewing Ability According to Breastfeeding Duration
3.3. Dietary Intake According to Breastfeeding Duration
3.4. Risk of Tooth Loss, Chewing Difficulty, and Undernutrition According to Breastfeeding Duration
3.5. Risk of Undernutrition According to Tooth Loss/Chewing Difficulty, Stratified by Breastfeeding Duration
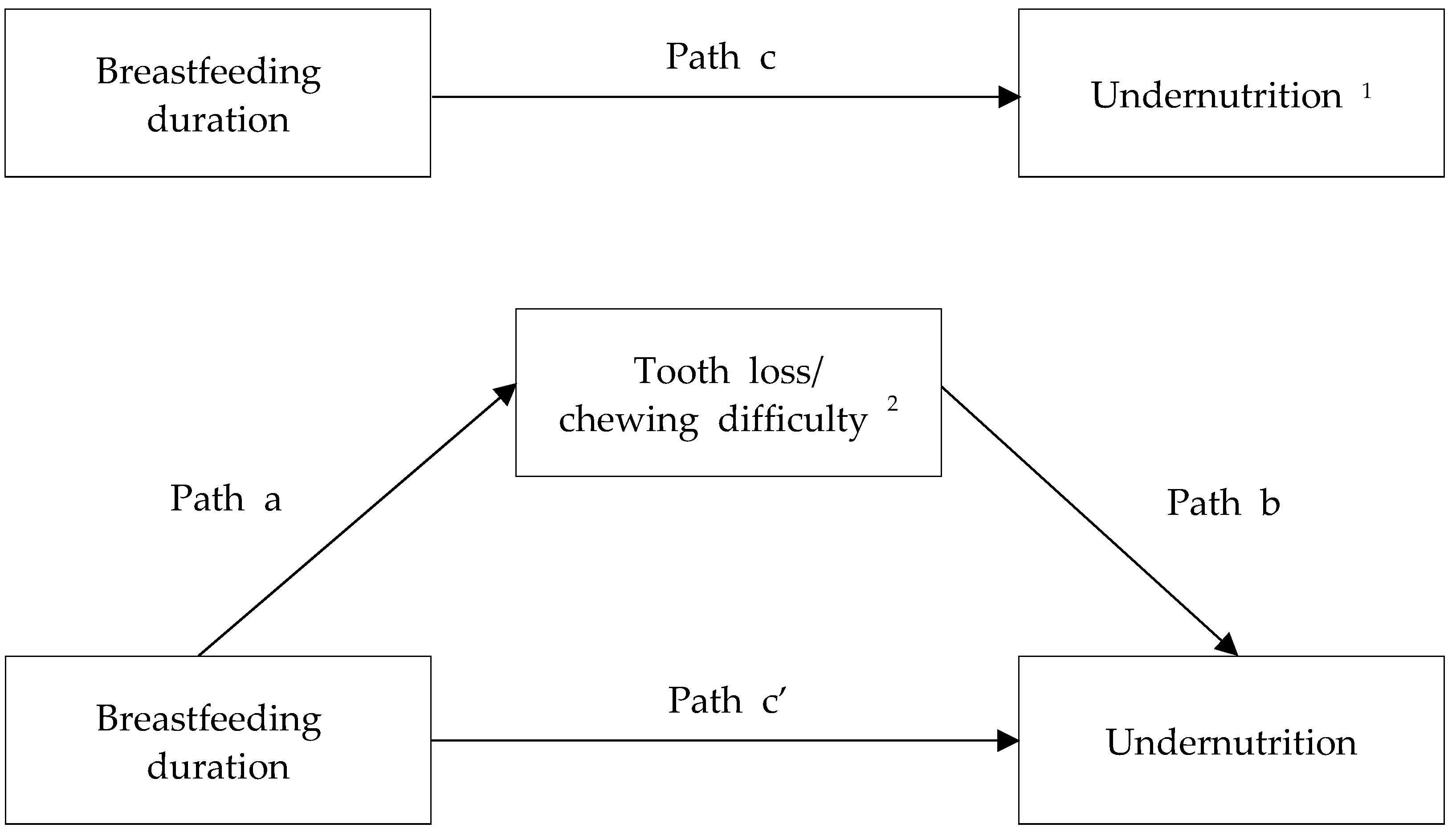
3.6. Mediating Effect of Tooth Loss/Chewing Difficulty on the Association between Breastfeeding Duration and Undernutrition Risk
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Westerfield, K.L.; Koenig, K.; Oh, R. Breastfeeding: Common questions and answers. Am. Fam. Physician 2018, 98, 368–373. [Google Scholar] [PubMed]
- Kovacs, C.S. Calcium and bone metabolism during pregnancy and lactation. J. Mammary Gland. Biol. Neoplasia 2005, 10, 105–118. [Google Scholar] [CrossRef] [PubMed]
- More, C.; Bettembuk, P.; Bhattoa, H.P.; Balogh, A. The effects of pregnancy and lactation on bone mineral density. Osteoporos. Int. 2001, 12, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Sowers, M.; Eyre, D.; Hollis, B.W.; Randolph, J.F.; Shapiro, B.; Jannausch, M.L.; Crutchfield, M. Biochemical markers of bone turnover in lactating and nonlactating postpartum women. J. Clin. Endocrinol. Metab. 1995, 80, 2210–2216. [Google Scholar] [CrossRef]
- Affinito, P.; Tommaselli, G.A.; di Carlo, C.; Guida, F.; Nappi, C. Changes in bone mineral density and calcium metabolism in breastfeeding women: A one year follow-up study. J. Clin. Endocrinol. Metab. 1996, 81, 2314–2318. [Google Scholar] [CrossRef]
- Athonvarangkul, D.; Wysolmerski, J.J. Crosstalk within a brain-breast-bone axis regulates mineral and skeletal metabolism during lactation. Front. Physiol. 2023, 14, 1121579. [Google Scholar] [CrossRef]
- Kovacs, C.S. Maternal mineral and bone metabolism during pregnancy, lactation, and post-weaning recovery. Physiol. Rev. 2016, 96, 449–547. [Google Scholar] [CrossRef]
- Martin, T.J. Osteoblast-derived PTHrP is a physiological regulator of bone formation. J. Clin. Investig. 2005, 115, 2322–2324. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, N.K.; Lee, S.Y. Current understanding of RANK signaling in osteoclast differentiation and maturation. Mol. Cells 2017, 40, 706–713. [Google Scholar] [CrossRef]
- López, J.M.; González, G.; Reyes, V.; Campino, C.; Díaz, S. Bone turnover and density in healthy women during breastfeeding and after weaning. Osteoporos. Int. 1996, 6, 153–159. [Google Scholar] [CrossRef]
- Ardeshirpour, L.; Dann, P.; Adams, D.J.; Nelson, T.; VanHouten, J.; Horowitz, M.C.; Wysolmerski, J.J. Weaning triggers a decrease in receptor activator of nuclear factor-kappaB ligand expression, widespread osteoclast apoptosis, and rapid recovery of bone mass after lactation in mice. Endocrinology 2007, 148, 3875–3886. [Google Scholar] [CrossRef] [PubMed]
- Grizzo, F.M.F.; Alarcão, A.C.J.; Dell’ Agnolo, C.M.; Pedroso, R.B.; Santos, T.S.; Vissoci, J.R.N.; Pinheiro, M.M.; Carvalho, M.D.B.; Pelloso, S.M. How does women’s bone health recover after lactation? A systematic review and meta-analysis. Osteoporos. Int. 2020, 31, 413–427. [Google Scholar] [CrossRef] [PubMed]
- Hughes, F.J. Periodontium and periodontal disease. In Stem Cell Biology and Tissue Engineering in Dental Sciences; Academic Press: Cambridge, MA, USA, 2015; pp. 433–444. [Google Scholar] [CrossRef]
- Gorrel, C.; Andersson, S.; Verhaert, L. Anatomy of the teeth and periodontium. In Veterinary Dentistry for the General Practitioner, 2nd ed.; Saunders Ltd.: London, UK, 2013; pp. 37–41. [Google Scholar] [CrossRef]
- Shoji, K.; Ohtsuka-Isoya, M.; Horiuchi, H.; Shinoda, H. Bone mineral density of alveolar bone in rats during pregnancy and lactation. J. Periodontol. 2000, 71, 1073–1078. [Google Scholar] [CrossRef]
- Shoji, K.; Ohtsuka-Isoya, M.; Shimauchi, H.; Shinoda, H. Effects of lactation on alveolar bone loss in experimental periodontitis. J. Periodontol. 2007, 78, 152–156. [Google Scholar] [CrossRef]
- Omi, M.; Mishina, Y. Role of osteoclasts in oral homeostasis and jawbone diseases. Oral Sci. Int. 2020, 18, 14–27. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Ko, Y.; Park, Y.G.; Park, J.B. Associations between the number of natural teeth in postmenopausal women and duration of lactation: The 2010–2012 Korea National Health and Nutrition Examination Survey. Maturitas 2016, 85, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Hatch, J.P.; Shinkai, R.S.; Sakai, S.; Rugh, J.D.; Paunovich, E.D. Determinants of masticatory performance in dentate adults. Arch. Oral Biol. 2001, 46, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Ojima, T.; Nagahata, T.; Kondo, I.; Ninomiya, T.; Yoshita, K.; Arai, Y.; Ohkubo, T.; Murakami, K.; Nishi, N.; et al. Having few remaining teeth is associated with a low nutrient intake and low serum albumin levels in middle-aged and older Japanese individuals: Findings from the NIPPON DATA2010. Environ. Health Prev. Med. 2019, 24, 1. [Google Scholar] [CrossRef]
- Motokawa, K.; Mikami, Y.; Shirobe, M.; Edahiro, A.; Ohara, Y.; Iwasaki, M.; Watanabe, Y.; Kawai, H.; Kera, T.; Obuchi, S.; et al. Relationship between chewing ability and nutritional status in Japanese older adults: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 1216. [Google Scholar] [CrossRef]
- World Health Organization. Breastfeeding. Available online: https://www.who.int/health-topics/breastfeeding#tab=tab_2 (accessed on 6 November 2023).
- Taylor, J. North American Culture: Undermining Breastfeeding. Available online: https://www.contemporaryobgyn.net/view/north-american-culture-undermining-breastfeeding (accessed on 6 November 2023).
- Martinez, G.A.; Dodd, D.A. 1981 milk feeding patterns in the United States during the first 12 months of life. Pediatrics 1983, 71, 166–170. [Google Scholar] [CrossRef]
- Windsor, J.E. Korean women & breastfeeding. AWHONN Lifelines 2003, 7, 61–64. [Google Scholar] [CrossRef]
- Sung, Y.A.; Ahn, J.Y.; Lee, H.Y.; Kim, J.Y.; Ahn, D.H.; Hong, Y.J. A survey of breast-feeding. J. Korean Pediatr. Soc. 1998, 41, 444–450. [Google Scholar]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Korea Disease Control and Prevention Agency. Available online: https://knhanes.kdca.go.kr/knhanes/eng/index.do (accessed on 6 November 2023).
- Kim, H.S. Metabolic syndrome related health inequalities in Korean elderly: Korean National Health and Nutrition Examination Survey (KNHAES). Int. J. Equity Health 2014, 13, 463. [Google Scholar] [CrossRef][Green Version]
- Kim, J.Y.; Kim, D.H.; Kim, Y.H.; Shin, H.Y. Associations of breastfeeding duration and reproductive factors with sarcopenia in elderly Korean women: A cross-sectional study from the Korea National Health and Nutrition Examination Survey 2010–2011. Korean J. Fam. Med. 2019, 40, 165–170. [Google Scholar] [CrossRef]
- Seo, Y.H.; Shin, H.Y. Relationship between hs-CRP and HbA1c in diabetes mellitus patients: 2015–2017 Korean National Health and Nutrition Examination Survey. Chonnam Med. J. 2021, 57, 62–67. [Google Scholar] [CrossRef]
- Yang, H.J.; Park, S.; Yoon, T.Y.; Ryoo, J.H.; Park, S.K.; Jung, J.Y.; Lee, J.H.; Oh, C.M. Nationwide changes in physical activity, nutrient intake, and obesity in South Korea during the COVID-19 pandemic era. Front. Endocrinol. 2022, 13, 965842. [Google Scholar] [CrossRef]
- Lee, S.K.; Hwang, S.Y. Oral health in adults with coronary artery disease and its risk factors: A comparative study using the Korea National Health and Nutrition Examination Survey data. BMC Cardiovasc. Disord. 2021, 21, 71. [Google Scholar] [CrossRef]
- da Silveira, D.L.; da Rosa Carlos Monteiro, L.E.; da Silva Christofoli, C.; Schaan, B.D.; Telo, G.H. Number of teeth lost on diet quality and glycemic control in patients with type 2 diabetes mellitus. Arch. Endocrinol. Metab. 2022, 66, 40–49. [Google Scholar] [CrossRef]
- Yamato, M.; Matsuyama, S.; Murakami, Y.; Aida, J.; Lu, Y.; Sugawara, Y.; Tsuji, I. Association between the number of remaining teeth and disability-free life expectancy, and the impact of oral self-care in older Japanese adults: A prospective cohort study. BMC Geriatr. 2022, 22, 820. [Google Scholar] [CrossRef]
- Hashimoto, H.; Hashimoto, S.; Shimazaki, Y. Relationship between tooth loss and the medications used for the treatment of rheumatoid arthritis in Japanese patients with rheumatoid arthritis: A cross-sectional study. J. Clin. Med. 2021, 10, 876. [Google Scholar] [CrossRef]
- Lawrence, H.P.; Garcia, R.I.; Essick, G.K.; Hawkins, R.; Krall, E.A.; Spiro, A., 3rd; Vokonas, P.S.; Kong, L.; King, T.; Koch, G.G. A longitudinal study of the association between tooth loss and age-related hearing loss. Spec. Care Dent. 2001, 21, 129–140. [Google Scholar] [CrossRef]
- Kim, M.J. Food consumption frequency of Korean adults based on whether or not having chewing difficulty using 2013–2016 KNHANES by sex-stratified comparative analysis. Nutr. Res. Pract. 2020, 14, 637–653. [Google Scholar] [CrossRef]
- The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2020; Ministry of Health and Welfare: Sejong, Republic of Korea; The Korean Nutrition Society: Seoul, Republic of Korea, 2020. [Google Scholar]
- Sorenson, A.W.; Wyse, B.W.; Wittwer, A.J.; Hansen, R.G. An index of nutritional quality for a balanced diet. New help for an old problem. J. Am. Diet. Assoc. 1976, 68, 236–242. [Google Scholar] [CrossRef]
- Won, M.S.; Kim, S.; Yang, Y.J. Comparison of health status and nutrient intake between depressed women and non-depressed women: Based on the 2013 Korea National Health and Nutrition Examination Survey. Clin. Nutr. Res. 2016, 5, 112–125. [Google Scholar] [CrossRef]
- Seo, E.-H. Survey on body image perception, dietary habits and nutrient intakes according to interest level in health of female university students in Gyeongnam area. Korean J. Food Nutr. 2015, 28, 281–294. [Google Scholar] [CrossRef]
- Kwon, Y.J.; Lee, J.W.; Kang, H.T. Secular trends in lipid profiles in Korean adults based on the 2005–2015 KNHANES. Int. J. Environ. Res. Public Health 2019, 16, 2555. [Google Scholar] [CrossRef]
- Huh, Y.; Kim, Y.N.; Kim, Y.S. Trends and determinants in breastfeeding among Korean women: A nationwide population-based study. Int. J. Environ. Res. Public Health 2021, 18, 13279. [Google Scholar] [CrossRef]
- Baek, J.Y.; Lee, E.; Jung, H.W.; Jang, I.Y. Geriatrics fact sheet in Korea 2021. Ann. Geriatr. Med. Res. 2021, 25, 65–71. [Google Scholar] [CrossRef]
- Bomfim, R.A.; Cascaes, A.M.; de Oliveira, C. Multimorbidity and tooth loss: The Brazilian National Health Survey, 2019. BMC Public Health 2021, 21, 2311. [Google Scholar] [CrossRef]
- Hag Mohamed, S.; Sabbah, W. Is tooth loss associated with multiple chronic conditions? Acta Odontol. Scand. 2023, 81, 443–448. [Google Scholar] [CrossRef]
- Oh, N.-G.; Seo, J.-S. Health and nutrition status of elderly people with multimorbidity: A Korea National Health and Nutrition Examination Survey (2013~2015). Korean J. Community Nutr. 2020, 25, 502–511. [Google Scholar] [CrossRef]
- Ley, S.H.; Chavarro, J.E.; Li, M.; Bao, W.; Hinkle, S.N.; Wander, P.L.; Rich-Edwards, J.; Olsen, S.; Vaag, A.; Damm, P.; et al. Lactation duration and long-term risk for incident type 2 diabetes in women with a history of gestational diabetes mellitus. Diabetes Care 2020, 43, 793–798. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Diez-Fernandez, A.; Sanchez-Lopez, M.; Mora-Rodriguez, R.; Notario-Pacheco, B.; Torrijos-Nino, C.; Martinez-Vizcaino, V. Obesity as a mediator of the influence of cardiorespiratory fitness on cardiometabolic risk: A mediation analysis. Diabetes Care 2014, 37, 855–862. [Google Scholar] [CrossRef]
- Gunzler, D.; Chen, T.; Wu, P.; Zhang, H. Introduction to mediation analysis with structural equation modeling. Shanghai Arch. Psychiatry 2013, 25, 390–394. [Google Scholar] [CrossRef]
- Williams, E.D.; Tapp, R.J.; Magliano, D.J.; Shaw, J.E.; Zimmet, P.Z.; Oldenburg, B.F. Health behaviours, socioeconomic status and diabetes incidence: The Australian Diabetes Obesity and Lifestyle Study (AusDiab). Diabetologia 2010, 53, 2538–2545. [Google Scholar] [CrossRef]
- Tiwari, T.; Scarbro, S.; Bryant, L.L.; Puma, J. Factors associated with tooth loss in older adults in rural Colorado. J. Community Health 2016, 41, 476–481. [Google Scholar] [CrossRef]
- Ferreira, R.O.; Correa, M.G.; Magno, M.B.; Almeida, A.; Fagundes, N.C.F.; Rosing, C.K.; Maia, L.C.; Lima, R.R. Physical activity reduces the prevalence of periodontal disease: Systematic review and meta-analysis. Front. Physiol. 2019, 10, 234. [Google Scholar] [CrossRef]
- Michaud, D.S.; Fu, Z.; Shi, J.; Chung, M. Periodontal disease, tooth loss, and cancer risk. Epidemiol. Rev. 2017, 39, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, R.A.; Ritti-Dias, R.M.; Balagopal, P.B.; Conceicao, R.D.O.; Santos, R.D.; Cucato, G.G.; Bittencourt, M.S. Self-initiated physical activity is associated with high sensitivity C-reactive protein: A longitudinal study in 5030 adults. Atherosclerosis 2018, 273, 131–135. [Google Scholar] [CrossRef]
- Gabiec, K.; Baginska, J.; Laguna, W.; Rodakowska, E.; Kaminska, I.; Stachurska, Z.; Dubatowka, M.; Kondraciuk, M.; Kaminski, K.A. Factors associated with tooth loss in general population of Bialystok, Poland. Int. J. Environ. Res. Public Health 2022, 19, 2369. [Google Scholar] [CrossRef]
- Consumer Guide to Dentistry. Causes and Consequences of Tooth Loss. Available online: https://www.yourdentistryguide.com/tooth-loss/ (accessed on 6 November 2023).
- Paunica, I.; Giurgiu, M.; Dumitriu, A.S.; Paunica, S.; Pantea Stoian, A.M.; Martu, M.A.; Serafinceanu, C. The bidirectional relationship between periodontal disease and diabetes mellitus—A review. Diagnostics 2023, 13, 681. [Google Scholar] [CrossRef] [PubMed]
- Mishellany, A.; Woda, A.; Labas, R.; Peyron, M.A. The challenge of mastication: Preparing a bolus suitable for deglutition. Dysphagia 2006, 21, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Pereira, L.J.; van der Bilt, A. The influence of oral processing, food perception and social aspects on food consumption: A review. J. Oral Rehabil. 2016, 43, 630–648. [Google Scholar] [CrossRef] [PubMed]
- Jeong, G.; Park, S.W.; Lee, Y.K.; Ko, S.Y.; Shin, S.M. Maternal food restrictions during breastfeeding. Korean J. Pediatr. 2017, 60, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Kwon, Y. Development of a database of capsaicinoid contents in foods commonly consumed in Korea. Food Sci. Nutr. 2020, 8, 4611–4624. [Google Scholar] [CrossRef] [PubMed]
- Tada, A.; Miura, H. The relationship between vitamin C and periodontal diseases: A systematic review. Int. J. Environ. Res. Public Health 2019, 16, 2472. [Google Scholar] [CrossRef]
- Kuzmanova, D.; Jansen, I.D.; Schoenmaker, T.; Nazmi, K.; Teeuw, W.J.; Bizzarro, S.; Loos, B.G.; van der Velden, U. Vitamin C in plasma and leucocytes in relation to periodontitis. J. Clin. Periodontol. 2012, 39, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Staudte, H.; Kranz, S.; Völpel, A.; Schütze, J.; Sigusch, B.W. Comparison of nutrient intake between patients with periodontitis and healthy subjects. Quintessence Int. 2012, 43, 907–916. [Google Scholar]
- Iwasaki, M.; Moynihan, P.; Manz, M.C.; Taylor, G.W.; Yoshihara, A.; Muramatsu, K.; Watanabe, R.; Miyazaki, H. Dietary antioxidants and periodontal disease in community-based older Japanese: A 2-year follow-up study. Public Health Nutr. 2013, 16, 330–338. [Google Scholar] [CrossRef]
- Iwasaki, M.; Manz, M.C.; Taylor, G.W.; Yoshihara, A.; Miyazaki, H. Relations of serum ascorbic acid and α-tocopherol to periodontal disease. J. Dent. Res. 2012, 91, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Gokhale, N.H.; Acharya, A.B.; Patil, V.S.; Trivedi, D.J.; Thakur, S.L. A short-term evaluation of the relationship between plasma ascorbic acid levels and periodontal disease in systemically healthy and type 2 diabetes mellitus subjects. J. Diet. Suppl. 2013, 10, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Abou Sulaiman, A.E.; Shehadeh, R.M. Assessment of total antioxidant capacity and the use of vitamin C in the treatment of non-smokers with chronic periodontitis. J. Periodontol. 2010, 81, 1547–1554. [Google Scholar] [CrossRef] [PubMed]


| Breastfeeding Duration (Months) | p | ||||
|---|---|---|---|---|---|
| 1–18 | 19–36 | 37–72 | ≥73 | ||
| Unweighted n | 161 | 411 | 559 | 535 | |
| Age (years) | 70.1 ± 0.4 c | 70.1 ± 0.3 c | 72.5 ± 0.2 b | 75.2 ± 0.2 a | <0.001 |
| Height (cm) | 151.8 ± 0.5 ab | 152.8 ± 0.3 a | 151.3 ± 0.3 b | 149.9 ± 0.3 c | <0.001 |
| Weight (kg) | 55.4 ± 0.7 bc | 57.2 ± 0.5 a | 56.3 ± 0.4 ab | 54.7 ± 0.5 c | 0.001 |
| BMI (kg/m2) | 24.0 ± 0.3 | 24.4 ± 0.2 | 24.6 ± 0.1 | 24.3 ± 0.2 | 0.199 |
| Smoking (yes) | 3.5 (1.7) | 1.7 (0.7) | 2.6 (0.8) | 2.6 (0.7) | 0.694 |
| Drinking (yes) | 23.3 (3.7) | 19.2 (2.4) | 20.6 (1.9) | 15.2 (1.7) | 0.098 |
| Regular walking (yes) | 38.7 (4.3) | 37.5 (2.8) | 34.7 (2.5) | 23.1 (2.1) | <0.001 |
| Daily frequency of tooth brushing | |||||
| ≤1 | 15.9 (3.3) | 12.7 (2.0) | 19.3 (2.1) | 20.1 (1.9) | 0.010 |
| 2 | 38.0 (4.4) | 52.1 (2.8) | 49.7 (2.5) | 47.1 (2.2) | |
| ≥3 | 46.0 (4.5) | 35.2 (2.6) | 31.0 (2.4) | 32.8 (2.3) | |
| Hypertension (yes) | 48.8 (4.3) | 54.6 (2.9) | 56.0 (2.3) | 60.9 (2.6) | 0.079 |
| Diabetes (yes) | 13.5 (2.5) | 16.6 (2.0) | 24.0 (2.1) | 22.9 (2.3) | 0.006 |
| Dyslipidemia (yes) | 39.2 (4.1) | 38.3 (2.6) | 30.0 (2.3) | 28.9 (2.3) | 0.009 |
| Stroke/myocardial infarction/ angina pectoris (yes) | 15.1 (3.4) | 8.3 (1.5) | 12.6 (1.6) | 15.2 (2.0) | 0.045 |
| Cancer (yes) | 10.4 (2.6) | 7.7 (1.5) | 8.1 (1.4) | 6.4 (1.3) | 0.538 |
| Number of chronic diseases 1 | |||||
| 0 | 27.7 (4.0) | 27.8 (2.4) | 26.1 (2.1) | 23.4 (2.1) | 0.847 |
| 1 | 35.0 (4.2) | 35.7 (2.7) | 35.2 (2.4) | 35.7 (2.5) | |
| ≥2 | 37.3 (4.0) | 36.5 (2.6) | 38.7 (2.3) | 40.9 (2.7) | |
| Number of pregnancies | 4.1 ± 0.2 d | 5.0 ± 0.1 c | 5.6 ± 0.1 b | 6.6 ± 0.1 a | <0.001 |
| Time since last birth (years) | 40.6 ± 0.7 ab | 41.0 ± 0.3 b | 42.0 ± 0.3 a | 41.6 ± 0.3 ab | 0.031 |
| Breastfeeding duration (months) | 10.6 ± 0.4 d | 30.6 ± 0.3 c | 58.0 ± 0.5 b | 123.9 ± 2.2 a | <0.001 |
| Breastfeeding Duration (Months) | p | ||||
|---|---|---|---|---|---|
| 1–18 | 19–36 | 37–72 | ≥73 | ||
| Number of teeth | |||||
| 0–9 | 14.5 (3.2) | 12.8 (1.9) | 24.5 (2.1) | 33.8 (2.3) | <0.001 |
| 10–20 | 22.2 (3.6) | 24.9 (2.4) | 28.1 (2.2) | 30.8 (2.2) | |
| 21–26 | 41.1 (4.5) | 40.0 (2.5) | 34.2 (2.3) | 27.3 (2.3) | |
| ≥27 | 22.2 (3.5) | 22.2 (2.2) | 13.2 (1.6) | 8.1 (1.2) | |
| Chewing ability | |||||
| Very uncomfortable | 7.1 (2.0) | 12.6 (1.9) | 16.2 (1.9) | 22.1 (2.1) | 0.001 |
| Uncomfortable | 28.5 (4.0) | 29.7 (2.6) | 31.9 (2.3) | 31.5 (2.3) | |
| Moderate | 17.7 (3.2) | 20.5 (2.2) | 18.3 (1.9) | 14.6 (1.7) | |
| Not uncomfortable | 17.9 (3.7) | 16.5 (2.2) | 12.5 (1.5) | 10.8 (1.4) | |
| Not uncomfortable at all | 28.9 (4.0) | 20.7 (2.0) | 21.1 (1.9) | 21.0 (2.0) | |
| Breastfeeding Duration (Months) | p | p for Trend | ||||
|---|---|---|---|---|---|---|
| 1–18 | 19–36 | 37–72 | ≥73 | |||
| Nutrient | ||||||
| Energy (kcal) | 1592.1 ± 61.8 | 1536.3 ± 43.7 | 1508.0 ± 31.9 | 1550.3 ± 39.0 | 0.526 | 0.985 |
| Carbohydrates (g) | 286.4 ± 12.4 | 273.9 ± 8.6 | 272.7 ± 6.2 | 289.4 ± 7.9 | 0.202 | 0.236 |
| Proteins (g) | 51.5 ± 2.2 | 50.7 ± 1.6 | 48.3 ± 1.5 | 47.3 ± 1.4 | 0.165 | 0.040 |
| Fats (g) | 24.8 ± 1.6 a | 24.3 ± 1.2 a | 22.0 ± 1.0 a | 19.0 ± 1.0 b | <0.001 | <0.001 |
| Dietary fibers (g) | 23.7 ± 1.3 | 22.4 ± 0.9 | 21.6 ± 0.8 | 21.4 ± 0.8 | 0.304 | 0.109 |
| Vitamin A (µg RAE) | 520.0 ± 62.2 | 578.6 ± 50.6 | 583.5 ± 52.5 | 543.7 ± 52.3 | 0.804 | 0.803 |
| Thiamin (mg) | 1.67 ± 0.07 | 1.54 ± 0.05 | 1.51 ± 0.04 | 1.55 ± 0.04 | 0.246 | 0.549 |
| Riboflavin (mg) | 1.01 ± 0.05 ab | 1.05 ± 0.05 a | 0.92 ± 0.04 bc | 0.84 ± 0.03 c | <0.001 | <0.001 |
| Niacin (mg) | 12.3 ± 0.6 ab | 12.6 ± 0.6 a | 11.3 ± 0.4 bc | 11.1 ± 0.4 c | 0.023 | 0.006 |
| Vitamin C (mg) | 120.3 ± 11.3 | 107.9 ± 12.6 | 96.2 ± 6.9 | 92.1 ± 7.0 | 0.105 | 0.039 |
| Calcium (mg) | 411.6 ± 24.9 | 400.1 ± 17.9 | 387.7 ± 17.9 | 368.8 ± 16.5 | 0.273 | 0.049 |
| Phosphorus (mg) | 872.6 ± 38.2 a | 832.3 ± 25.8 ab | 786.9 ± 23.0 bc | 767.6 ± 21.5 c | 0.015 | 0.003 |
| Iron (mg) | 13.9 ± 1.0 | 15.2 ± 0.9 | 14.3 ± 0.8 | 14.8 ± 1.2 | 0.721 | 0.916 |
| Sodium (mg) | 2814.0 ± 163.4 | 2991.7 ± 122.8 | 2809.2 ± 108.2 | 2850.1 ± 112.6 | 0.611 | 0.681 |
| Potassium (mg) | 2980.9 ± 182.1 a | 2581.3 ± 97.7 b | 2509.0 ± 76.4 b | 2412.8 ± 82.0 b | 0.012 | 0.002 |
| Carbohydrates (%) | 73.0 ± 0.9 b | 73.1 ± 0.7 b | 74.2 ± 0.6 b | 76.3 ± 0.6 a | <0.001 | <0.001 |
| Proteins (%) | 12.9 ± 0.3 | 13.2 ± 0.2 | 12.9 ± 0.2 | 12.5 ± 0.2 | 0.052 | 0.009 |
| Fats (%) | 14.0 ± 0.7 a | 13.7 ± 0.5 a | 12.9 ± 0.5 a | 11.2 ± 0.5 b | <0.001 | <0.001 |
| Food group | ||||||
| Grains (g) | 261.2 ± 13.8 ab | 260.8 ± 11.4 b | 260.4 ± 8.3 b | 294.2 ± 10.1 a | 0.026 | 0.010 |
| Potatoes (g) | 79.4 ± 24.2 a | 40.5 ± 9.0 ab | 41.4 ± 6.8 ab | 30.9 ± 6.4 b | 0.020 | 0.005 |
| Legumes (g) | 46.3 ± 9.2 | 36.4 ± 4.0 | 35.6 ± 3.4 | 31.5 ± 3.8 | 0.407 | 0.094 |
| Nuts and seeds (g) | 8.1 ± 2.1 | 6.9 ± 1.3 | 5.5 ± 1.1 | 4.4 ± 0.9 | 0.206 | 0.033 |
| Vegetables (g) | 342.7 ± 23.1 | 308.0 ± 14.4 | 299.7 ± 13.3 | 305.5 ± 13.4 | 0.377 | 0.384 |
| Mushrooms (g) | 5.6 ± 1.8 | 3.5 ± 1.0 | 4.6 ± 1.5 | 3.6 ± 1.0 | 0.645 | 0.437 |
| Seaweeds (g) | 31.0 ± 10.1 | 40.4 ± 7.2 | 28.4 ± 6.2 | 21.1 ± 5.6 | 0.151 | 0.037 |
| Fruits (g) | 227.2 ± 28.8 | 207.6 ± 24.9 | 187.9 ± 15.4 | 177.0 ± 14.6 | 0.301 | 0.065 |
| Meats (g) | 51.2 ± 10.7 | 77.7 ± 12.1 | 76.1 ± 16.9 | 50.8 ± 10.4 | 0.116 | 0.144 |
| Fish and shellfish (g) | 98.2 ± 22.8 | 97.9 ± 10.5 | 96.1 ± 12.0 | 80.6 ± 9.7 | 0.475 | 0.142 |
| Eggs (g) | 15.9 ± 2.5 a | 15.6 ± 1.9 a | 14.0 ± 1.9 a | 9.2 ± 1.5 b | 0.007 | 0.001 |
| Milk and dairy products (g) | 84.2 ± 11.0 | 72.5 ± 9.7 | 63.8 ± 6.8 | 54.2 ± 6.3 | 0.050 | 0.007 |
| Beverages (g) | 125.3 ± 54.0 | 57.3 ± 15.8 | 39.6 ± 7.5 | 30.8 ± 7.6 | 0.307 | 0.069 |
| Alcohol (g) | 23.4 ± 7.9 | 16.0 ± 3.9 | 17.3 ± 4.6 | 19.0 ± 4.3 | 0.715 | 0.952 |
| Oils (g) | 4.2 ± 0.4 | 4.4 ± 0.4 | 4.3 ± 0.4 | 3.8 ± 0.4 | 0.581 | 0.213 |
| Sugars (g) | 7.1 ± 1.1 | 7.9 ± 1.0 | 8.2 ± 0.9 | 6.0 ± 0.7 | 0.156 | 0.045 |
| Seasonings (g) | 31.4 ± 3.7 | 39.5 ± 2.8 | 35.9 ± 2.4 | 37.3 ± 2.4 | 0.225 | 0.695 |
| Total (g) | 1344.8 ± 65.6 a | 1232.3 ± 47.8 ab | 1153.3 ± 34.1 bc | 1119.9 ± 34.0 c | 0.002 | <0.001 |
| Tooth Loss/ Chewing Difficulty | Breastfeeding Duration (Months) | p for Interaction | |||
|---|---|---|---|---|---|
| 1–36 | ≥37 | ||||
| OR | 95% CI | OR | 95% CI | ||
| No | 1 | 1 | 0.712 | ||
| Yes | 1.74 | 0.79–3.84 | 1.92 | 1.21–3.02 | |
| Beta | SE | OR | 95% CI | p | Sobel Test | ||
|---|---|---|---|---|---|---|---|
| Z (p) | |||||||
| Path c | Breastfeeding duration → Undernutrition | 0.490 | 0.209 | 1.63 | 1.09–2.46 | 0.019 | 2.167 (0.030) |
| Path a | Breastfeeding duration → Tooth loss/chewing difficulty | 0.390 | 0.134 | 1.48 | 1.14–1.92 | 0.004 | |
| Path c’ | Breastfeeding duration → Undernutrition | 0.448 | 0.211 | 1.57 | 1.04–2.37 | 0.033 | |
| Path b | Tooth loss/chewing difficulty → Undernutrition | 0.636 | 0.196 | 1.89 | 1.29–2.77 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jo, Y.R.; Park, Y.K.; Lim, H.-S. Breastfeeding Duration Is Associated with the Risk of Tooth Loss, Chewing Difficulty, and Undernutrition among Older Korean Women: Results of the Korea National Health and Nutrition Examination Survey (KNHANES) 2013–2015. Nutrients 2023, 15, 5024. https://doi.org/10.3390/nu15245024
Jo YR, Park YK, Lim H-S. Breastfeeding Duration Is Associated with the Risk of Tooth Loss, Chewing Difficulty, and Undernutrition among Older Korean Women: Results of the Korea National Health and Nutrition Examination Survey (KNHANES) 2013–2015. Nutrients. 2023; 15(24):5024. https://doi.org/10.3390/nu15245024
Chicago/Turabian StyleJo, Ye Rang, Yoo Kyoung Park, and Hee-Sook Lim. 2023. "Breastfeeding Duration Is Associated with the Risk of Tooth Loss, Chewing Difficulty, and Undernutrition among Older Korean Women: Results of the Korea National Health and Nutrition Examination Survey (KNHANES) 2013–2015" Nutrients 15, no. 24: 5024. https://doi.org/10.3390/nu15245024
APA StyleJo, Y. R., Park, Y. K., & Lim, H.-S. (2023). Breastfeeding Duration Is Associated with the Risk of Tooth Loss, Chewing Difficulty, and Undernutrition among Older Korean Women: Results of the Korea National Health and Nutrition Examination Survey (KNHANES) 2013–2015. Nutrients, 15(24), 5024. https://doi.org/10.3390/nu15245024







