Diet-Related Disease Prevention in a Rural Australian Setting: Understanding Barriers, Enablers, and the Role of Rural Health Services in Supporting Changes in Local Rural Food Environments
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Design
2.3. Theoretical Framework
2.4. Participants and Recruitment
2.5. Data Collection
2.5.1. Group Model Building
2.5.2. Semi-Structured Interviews with Food Outlet Participants
2.6. Data Analysis
3. Results
3.1. Participants
3.2. Summary of Overall Themes
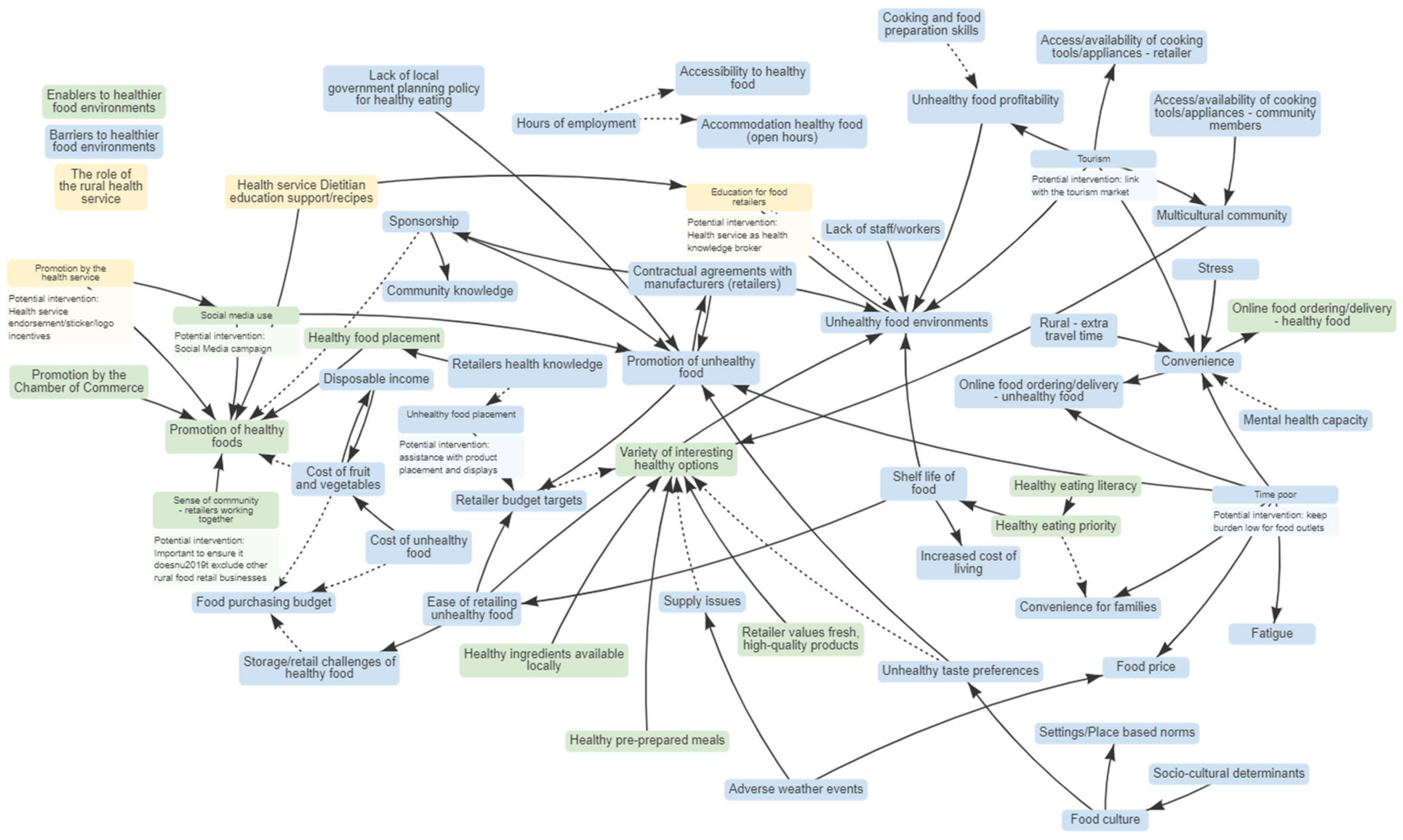
3.3. Local Government and Health Service Causal Loop Diagram
3.3.1. Enablers to Healthier Food Environments
‘I haven’t actually found anything that has stopped us from doing what we wanna do. We’ve been able to source local produce of numerous suppliers, which are all homemade or locally made. And then we also make them ourselves. So produce has been quite easy to find’Interview participant #12 (Food outlet)
‘…what people are offered is what they’re gonna get. So, that’s why here, we try to make it a—only fresh produce, healthy produce…..I think that’s what [Local Government Area] wants and needs. And there are a couple of places around town now that offer it. So, if we can keep going with that, I think we’re on the right track’Interview participant #12 (Food outlet)
‘Well, I think obviously, as a business, you lose business if you’re not gonna meet demands and meet needs, but in terms of affecting business, like you lose business, like after a swim or a gym or something like that, they don’t necessarily want a chocolate or anything like that. So, if you don’t have anything healthy on offer, they’re not gonna buy from you’Interview participant #11 (Food outlet)
3.3.2. Barriers to Healthier Food Environments
‘…when we were doing the choose water campaign <health service name> were looking at putting water in all their vending machines, but the contract was with <drink name> would say that they needed to have certain products for those machines. Because that was part of the deal, of having the machine’GMB1 Participant #7 (Local Government)
‘To my knowledge, there’s nothing in the planning scheme that would prevent, say, a fast-food outlet from establishing itself anywhere in the Shire as long as the zoning is correct. Same with, say, their signage or their marketing. A healthy outlet has to abide by the same rules as an unhealthy outlet. So there’s nothing in the planning scheme that local government can enact to change that’GMB2 Participant #3 (Local Government)
‘Maccas [McDonalds] and KFC [Kentucky Fried Chicken] do home deliveries now’GMB1 Participant #7 (Local Government)
‘And in terms of shelf life, we tend to throw a lot of our fresh products. Cost would be a massive thing. We currently sell sandwiches and they’re seven dollars a pop. We’re throwing them out every two days ‘cause it’s just not what people wanna spend that amount of money on’Interview participant #11 (Food outlet)
‘…we do have things like—we do vegan options which I guess ultimately vegan is quite healthy and we have cold options there. So just confirming what are the healthy options in our business. I mean, we obviously think that vegan’s healthy. We’ve got cheese and salad rolls that are healthy, so we do a vegan sandwich’Interview participant #10 (Food outlet)
3.3.3. Rural Health Services Are a Leading Broker of Knowledge for Healthy Food Environments
‘There was a lot of like (we) promote like vegan and gluten free… Without understanding that that was promoting a healthy option when really that’s just catering to different dietary requirements’GMB1 Participant #1 (Health Service)
‘Yeah, that [having a dietitian], would be beneficial like them to sort of have a look at the menu and go, “Well, yes, this is fully healthy,” or, “This is like half healthy. But if we did this, it would be fully healthy.’Interview participant #13 (Food outlet)
‘…some sort of sticker to stick on my label saying this is a healthy choice option’Interview participant #10 (Food outlet)
‘Even if we still had the menus and that put into (the health service) that they can pass on to their clients and things like that’Interview participant #1 (Food outlet)
‘Maybe not here, but elsewhere like in the doctor’s office or something. I know it sounds a bit weird, but you know advertising for sandwich for us there, but—Yeah, outside the business’Interview participant #3 (Food outlet)
3.3.4. Characteristics of Desirable Healthy Food Environment Interventions
‘I have a big following on social media—Facebook and Instagram. I can’t believe it. The minute I post something, I get busy’Interview participant #1 (Food outlet)
‘…we probably wouldn’t wanna go anything too overly taxing for us or the staff, I mean, we’ve got enough to do at the moment as it is, but if it’s just putting a sticker on a label saying this is a healthy option, then it’s a no brainer’Interview participant #10 (Food outlet)
‘…(the intervention outlets) Could be included in tourism marketing so that when people come here they can look for healthy options’Interview participant #2 (Food outlet)
‘I think there’s ways that we can incentivise good practice that maybe looks like providing healthy food options, you might get a discount on your rent……I think it would be us (local government) acting alone when an entire industry is built on unhealthy sponsorship of sports.’GMB2 Participant #3 (Local Government)
‘I call it small town syndrome, but it is working together, networking’Interview participant #1 (Food outlet)
‘It’d have to be pretty careful to not alienate the ones that don’t do it. Yeah. So, that’s probably—I think you got to take that into consideration’Interview participant #9 (Food outlet)
‘I think small businesses should help promote other small businesses. My whole thing is to be unique. And I think if we’re talking amongst each other, as much as we could get ideas and gauge support from them, it doesn’t necessarily mean we’re going to run—all of us are not gonna have beef stroganoff on the same day, but we can bounce ideas around and just help promote each other’Interview participant #4 (Food outlet)
4. Discussion
4.1. Strengths
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Semi-Structured Interview Guide for Food Outlet Participants
Appendix A.1. Moderator Verbal Introduction
Appendix A.2. Semi-Structured Interview Guide Discussion Points
- What affects the food retail environment in <town>? (suppliers, seasons)
- How will these change as time goes on?
- If we don’t make any changes, how will this impact the health of <town> residents?
- How can we promote healthy food options already present in stores?
- Are there any factors that are connected to each other, or affect each other in some way?
- What can we (<health service> staff) do to help you as a retailer to improve/advertise the healthy food options?
- Are there any areas of this map that you think needs attention? (does anything look wrong or need clarification?)
- Are there large, important issues missing from the map that should be included?
- If we were to run an intervention to trial some of these changes, what are some challenges stopping you from being involved? For example, customers wants/needs, staffing.
- If you could be involved in making some of these suggested changes within your business, how long would you like to trial this for? (4 weeks, 12 weeks?)
- To improve the food environment in <town>, what would be your top priority?
References
- Australian Institute of Health and Welfare. Rural and Remote Health; Australian Institute of Health and Welfare: Bruce, Australia, 2023. [Google Scholar]
- Alston, L.; Jacobs, J.; Allender, S.; Nichols, M. A comparison of the modelled impacts on CVD mortality if attainment of public health recommendations was achieved in metropolitan and rural Australia. Public Health Nutr. 2020, 23, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Alston, L.; Versace, V.; Brown, E.; Nichols, M.; Whelan, J.; Bolton, K.A.; Sacks, G.; Needham, C.; Orellana, L.; Allender, S. Understanding the healthfulness of outlets providing lunch and dinner meals: A census of a rural food retail environment using two measurement tools, in Victoria, Australia. Aust. N. Z. J. Public Health 2020, 45, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Whelan, J.; Millar, L.; Bell, C.; Russell, C.; Grainger, F.; Allender, S.; Love, P. You Can’t Find Healthy Food in the Bush: Poor Accessibility, Availability and Adequacy of Food in Rural Australia. Int. J. Environ. Res. Public Health 2018, 15, 2316. [Google Scholar] [CrossRef] [PubMed]
- Alston, L.; Raeside, R.; Jia, S.S.; Partridge, S.R. Underinvestment in nutrition research for at-risk populations: An analysis of research funding awarded in Australia from 2014 to 2021. Nutr. Diet. 2022, 79, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Australian Department of Health. Modified Monash Model. Canberra (AUST): Government of Australia. 2019. Available online: https://www.rdaa.com.au/documents/item/740 (accessed on 30 October 2023).
- Farmer, J.; Prior, M.; Taylor, J. A theory of how rural health services contribute to community sustainability. Soc. Sci. Med. 2012, 75, 1903–1911. [Google Scholar] [CrossRef]
- Farmer, J.; Davis, H.; Blackberry, I.; de Cotta, T. Assessing the value of rural community health services. Aust. J. Prim. Health 2018, 24, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Prior, M.; Farmer, J.; Godden, D.J.; Taylor, J. More than health: The added value of health services in remote Scotland and Australia. Health Place 2010, 16, 1136–1144. [Google Scholar] [CrossRef]
- Pearce, C.; Rychetnik, L.; Wutzke, S.; Wilson, A. Obesity prevention and the role of hospital and community-based health services: A scoping review. BMC Health Serv. Res. 2019, 19, 453. [Google Scholar] [CrossRef]
- Deloitte. Design, service and infrastructure plan for Victoria’s rural and regional health system. In Discussion Paper; Deloittes: Melbourne, Australia, 2016. [Google Scholar]
- Department of Health. Community Health—Health Promotion Program 2021–2025: Victorian State Government. 2023. Available online: https://www.health.vic.gov.au/publications/community-health-health-promotion-2021-25 (accessed on 30 October 2023).
- Victorian Legislation. Food Act 1984. Victorian Government. 1984. Available online: https://www.legislation.vic.gov.au/in-force/acts/food-act-1984/110 (accessed on 30 October 2023).
- Victorian Agency for Health. Legislative Requirements of Municipal Public Health and Wellbeing Plans. 2023. Available online: https://www.health.vic.gov.au/population-health-systems/requirements-of-municipal-public-health-and-wellbeing-planning (accessed on 30 October 2023).
- Boelsen-Robinson, T.; Peeters, A.; Thow, A.-M.; Hawkes, C. Barriers and facilitators to implementing a healthier food outlet initiative: Perspectives from local governments. Public Health Nutr. 2021, 24, 2758–2770. [Google Scholar] [CrossRef]
- Middel, C.N.H.; Schuitmaker-Warnaar, T.J.; Mackenbach, J.D.; Broerse, J.E.W. Systematic review: A systems innovation perspective on barriers and facilitators for the implementation of healthy food-store interventions. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 108. [Google Scholar] [CrossRef]
- Hasdell, R.; Poland, B.; Cole, D.; Sheppard, F.; Burton, L.; Mah, C.L. Retail Food Environment Intervention Planning: Interviews With Owners and Managers of Small- and Medium-Sized Rural Food Stores. Health Promot. Pract. 2021, 22, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Colac Otway. 2021. Available online: https://www.abs.gov.au/census/find-census-data/quickstats/2021/LGA21750 (accessed on 30 October 2023).
- Victorian Agency for Health Information. Victorian Population Health Survey 2020—Dashboard. 2020. Available online: https://vahi.vic.gov.au/reports/population-health/victorian-population-health-survey-2020-dashboards (accessed on 30 October 2023).
- Felmingham, T.; Backholer, K.; Hoban, E.; Brown, A.D.D.; Nagorcka-Smith, P.; Allender, S. Success of community-based system dynamics in prevention interventions: A systematic review of the literature. Front. Public Health 2023, 11, 1103834. [Google Scholar] [CrossRef]
- Hovmand, P.S. Community Based System Dynamics; Springer: New York, NY, USA, 2014. [Google Scholar]
- Bolton, K.A.; Fraser, P.; Lowe, J.; Moodie, M.; Bell, C.; Strugnell, C.; Hayward, J.; McGlashan, J.; Millar, L.; Whelan, J.; et al. Generating change through collective impact and systems science for childhood obesity prevention: The GenR8 Change case study. PLoS ONE 2022, 17, e0266654. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.; Moore, T.H.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 7, CD001871. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Population-Based Approaches to Childhood Obesity Prevention Geneva, Switzerland. 2012. Available online: https://apps.who.int/iris/bitstream/handle/10665/80149/9789241504782_eng.pdf (accessed on 30 October 2023).
- McGlashan, J.; Hayward, J.; Brown, A.; Owen, B.; Millar, L.; Johnstone, M.; Creighton, D.; Allender, S. complex perspectives on obesity drivers: Action-driven communities and evidence-oriented experts. Obes. Sci. Pract. 2018, 4, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Ryom, K.; Aaby, A.; Maindal, H.T.; Kirkegaard, H.; Østergaard, J.N.; Allender, S.; et Breddam, C. Participatory System Dynamics Approach Targeting Childhood Health in a Small Danish Community (Children’s Cooperation Denmark): Protocol for a Feasibility Study Design. JMIR Res. Protoc. 2023, 12, e43949. [Google Scholar] [CrossRef] [PubMed]
- Savona, N.; Brown, A.; Macauley, T.; Aguiar, A.; Hayward, J.; Ayuandini, S.; Habron, J.; Grewal, N.K.; Luszczynska, A.; Mendes, S.; et al. System mapping with adolescents: Using group model building to map the complexity of obesity. Obes. Rev. 2023, 24 (Suppl. S1), e13506. [Google Scholar] [CrossRef]
- Allender, S.; Munira, S.L.; Bourke, S.; Lancsar, E. Participatory systems science for enhancing health and wellbeing in the Indian Ocean territories. Front. Public Health 2023, 11, 1013869. [Google Scholar] [CrossRef]
- Crotty, M. Foundations of Social Research: Meaning and Perspective in the Research Process, 1st ed.; Routledge: London, UK, 1998. [Google Scholar]
- Sterman, J.D. Business Dynamics: Systems Thinking and Modeling for a Complex World; Irwin/McGrawHill: Boston, UK, 2000. [Google Scholar]
- Hayward, J.; Morton, S.; Johnstone, M.; Creighton, D.; Allender, S. Tools and analytic techniques to synthesise community knowledge in CBPR using computer-mediated participatory system modelling. NPJ Digit. Med. 2020, 3, 22. [Google Scholar] [CrossRef]
- Ritchie, J.; Spencer, L. The Qualitative Researcher’s Companion; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2002; Available online: https://methods.sagepub.com/book/the-qualitative-researchers-companion (accessed on 1 February 2023).
- Whelan, J.; Brown, A.D.; Coller, L.; Strugnell, C.; Allender, S.; Alston, L.; Hayward, J.; Brimblecombe, J.; Bell, C. The Impact of COVID-19 on Rural Food Supply and Demand in Australia: Utilising Group Model Building to Identify Retailer and Customer Perspectives. Nutrients 2021, 13, 417. [Google Scholar] [CrossRef]
- Vargas, C.; Whelan, J.; Brimblecombe, J.; Brock, J.; Christian, M.; Allender, S. Co-creation of healthier food retail environments: A systematic review to explore the type of stakeholders and their motivations and stage of engagement. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2022, 23, e13482. [Google Scholar] [CrossRef] [PubMed]
- Whelan, J.; Love, P.; Aitken, J.; Millar, L.; Morley, C.; Melgren, N.; Allender, S.; Bell, C. A mixed-methods evaluation of a health-promoting café located in a small health service in rural Victoria, Australia. Aust. J. Rural Health 2023, 31, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Riesenberg, D.; Blake, M.R.; Boelsen-Robinson, T.; Peeters, A.; Cameron, A.J. Local government policies on healthy food promotion and obesity prevention: Results from a national Australian survey. Aust. N Z J. Public Health 2022, 46, 696–703. [Google Scholar] [CrossRef] [PubMed]
- Victorian State Government. Using Victoria’s Planning System. Department of Environment LWaP. 2022. Available online: https://www.planning.vic.gov.au/guide-home/using-victorias-planning-system (accessed on 30 October 2023).
- Murphy, M.; Badland, H.; Jordan, H.; Koohsari, M.J.; Giles-Corti, B. Local Food Environments, Suburban Development, and BMI: A Mixed Methods Study. Int. J. Environ. Res. Public Health 2018, 15, 1392. [Google Scholar] [CrossRef] [PubMed]
- Swinburn, B.; Vandevijvere, S.; Kraak, V.; Sacks, G.; Snowdon, W.; Hawkes, C.; Barquera, S.; Friel, S.; Kelly, B.; Kumanyika, S.; et al. Monitoring and benchmarking government policies and actions to improve the healthiness of food environments: A proposed Government Healthy Food Environment Policy Index. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2013, 14 (Suppl. S1), 24–37. [Google Scholar] [PubMed]
- Sacks, G.R.E. For the Food-EPI Australia Project Team. Policies for Tackling Obesity and Creating Healthier food Environments: 2019 Progress Update, Australian Governments; Deakin University: Melbourne, Australia, 2019. [Google Scholar]
- Osborne, S.R.; Alston, L.V.; Bolton, K.A.; Whelan, J.; Reeve, E.; Wong Shee, A.; Browne, J.; Walker, T.; Versace, V.L.; Allender, S.; et al. Beyond the black stump: Rapid reviews of health research issues affecting regional, rural and remote Australia. Med. J. Aust. 2020, 213 (Suppl. S11), S3. [Google Scholar] [CrossRef] [PubMed]
- Rosewarne, E.; Chislett, W.-K.; McKenzie, B.; Reimers, J.; Jolly, K.-A.; Corben, K.; Trieu, K.; Webster, J. Stakeholder perspectives on the effectiveness of the Victorian Salt Reduction Partnership: A qualitative study. BMC Nutr. 2021, 7, 12. [Google Scholar] [CrossRef]
- Versace, V.L.; Skinner, T.C.; Bourke, L.; Harvey, P.; Barnett, T. National analysis of the Modified Monash Model, population distribution and a socio-economic index to inform rural health workforce planning. Aust. J. Rural Health 2021, 29, 801–810. [Google Scholar] [CrossRef]
| Theme | Subtheme |
|---|---|
| Enablers to healthier food environments | Access to local and appealing healthy food options Promotion of healthier options in stores and on menus Importance of community and social conscience Consumer demand for healthy options and foods that meet dietary requirements |
| Barriers to healthier food environments | Consumer demand for less healthy options and preference for convenience Contractual agreements with manufacturers that promote unhealthy food supply Local Government Planning policy that does not inhibit the number of unhealthy food outlets Community mental health stressors Poor access to high quality healthy food Lack of knowledge and skills among retailers for understanding healthy food options |
| Rural health services are a leading broker of knowledge for healthy food environments | Utilising community perception that the health service is the ‘health leader’ in the town Health knowledge brokerage for helping retailers to decipher between dietary requirements and healthy options Advertisement/social media on health service channels to promote businesses who are making efforts to promote healthier food environments Health service endorsement of healthy food businesses Support from dietitians and health promotion officers |
| Characteristics of desirable healthy food environment interventions | Important to ensure the intervention doesn’t exclude other rural food retail businesses Incentives for businesses who are promoting healthier food environments Assistance with Social media/advertisement of healthy options available Health-service endorsed sticker/logo to identify healthier options Keep the implementation burden low for food outlets Link the outlets who are promoting healthy environments to tourism promotion, to increase business |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wheaton, N.; Alston, E.; Versace, V.L.; Field, M.; Wong Shee, A.; Jacobs, J.; Backholer, K.; Allender, S.; Nichols, M.; Needham, C.; et al. Diet-Related Disease Prevention in a Rural Australian Setting: Understanding Barriers, Enablers, and the Role of Rural Health Services in Supporting Changes in Local Rural Food Environments. Nutrients 2023, 15, 4979. https://doi.org/10.3390/nu15234979
Wheaton N, Alston E, Versace VL, Field M, Wong Shee A, Jacobs J, Backholer K, Allender S, Nichols M, Needham C, et al. Diet-Related Disease Prevention in a Rural Australian Setting: Understanding Barriers, Enablers, and the Role of Rural Health Services in Supporting Changes in Local Rural Food Environments. Nutrients. 2023; 15(23):4979. https://doi.org/10.3390/nu15234979
Chicago/Turabian StyleWheaton, Nikita, Emily Alston, Vincent L. Versace, Michael Field, Anna Wong Shee, Jane Jacobs, Kathryn Backholer, Steven Allender, Melanie Nichols, Cindy Needham, and et al. 2023. "Diet-Related Disease Prevention in a Rural Australian Setting: Understanding Barriers, Enablers, and the Role of Rural Health Services in Supporting Changes in Local Rural Food Environments" Nutrients 15, no. 23: 4979. https://doi.org/10.3390/nu15234979
APA StyleWheaton, N., Alston, E., Versace, V. L., Field, M., Wong Shee, A., Jacobs, J., Backholer, K., Allender, S., Nichols, M., Needham, C., Bolton, K. A., Blake, M. R., Stewart, F., Close, E., & Alston, L. (2023). Diet-Related Disease Prevention in a Rural Australian Setting: Understanding Barriers, Enablers, and the Role of Rural Health Services in Supporting Changes in Local Rural Food Environments. Nutrients, 15(23), 4979. https://doi.org/10.3390/nu15234979






