The Association of Loneliness with Diabetes Is Mediated by Physical Activity and BMI but Not Diet Quality
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Predictor Variable: Loneliness
2.3. Behavioral Lifestyle Factors
2.3.1. Diet
2.3.2. Physical Activity
- Do you play sports or are you physically active in your leisure time or time awake? (yes/no)
- What sport or physical activity do you do most frequently? (low intensity e.g., walking, moderate intensity, e.g., biking, high intensity, e.g., basketball)
- How many hours a week do you play or do your most frequent activity? (<1 h, 1–2 h, 2–3 h, 3–4 h, >4 h)
- What sport or physical activity do you do next most frequently? (low intensity e.g., walking, moderate intensity, e.g., biking, high intensity, e.g., basketball)
- During leisure time, I watch television (five-point Likert scale from never, seldom, sometimes, often, to very often)
- During leisure time, I walk (five-point Likert scale from never, seldom, sometimes, often, to very often)
- During leisure time, I cycle (five-point Likert scale from never, seldom, sometimes, often, to very often)
- How many minutes per day do you walk or cycle to and from work or shopping? (<5 min, 5–15 min, 15–30 min, 30–45 min, >45 min)
- For sport activities: <1 h ~ 30 min; 1–2 h ~90 min; 2–3 h ~150 minutes.; 3–4 h ~210 min; >4 h ~270 min.
- For non-sports leisure activities: (<5 min ~2.5 min; 5–15 min ~10 minutes; 15–30 min ~22.5 min; 30–45 min ~37.5 min; >45 min ~52.5 min.
2.3.3. Body Mass Index
2.4. Covariates
2.5. Outcome Variable: Diabetes
2.6. Statistical Analysis
3. Results
3.1. Sample Characteristics
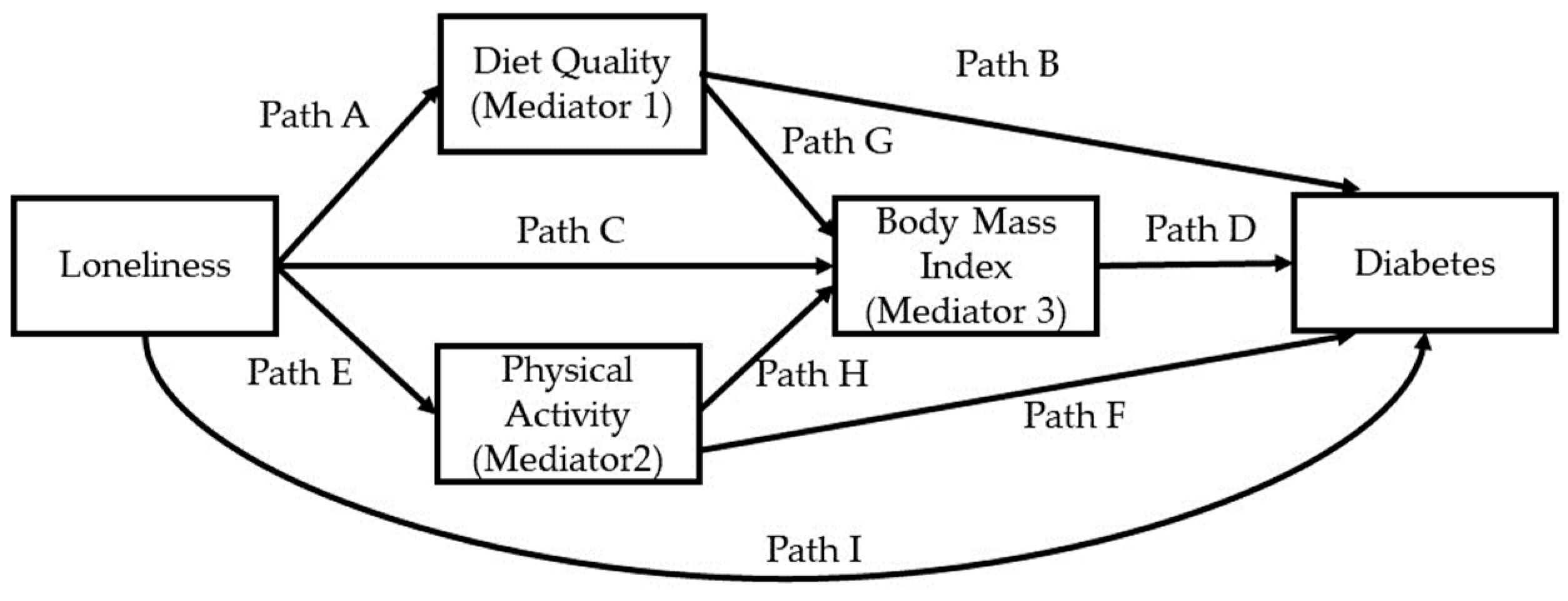
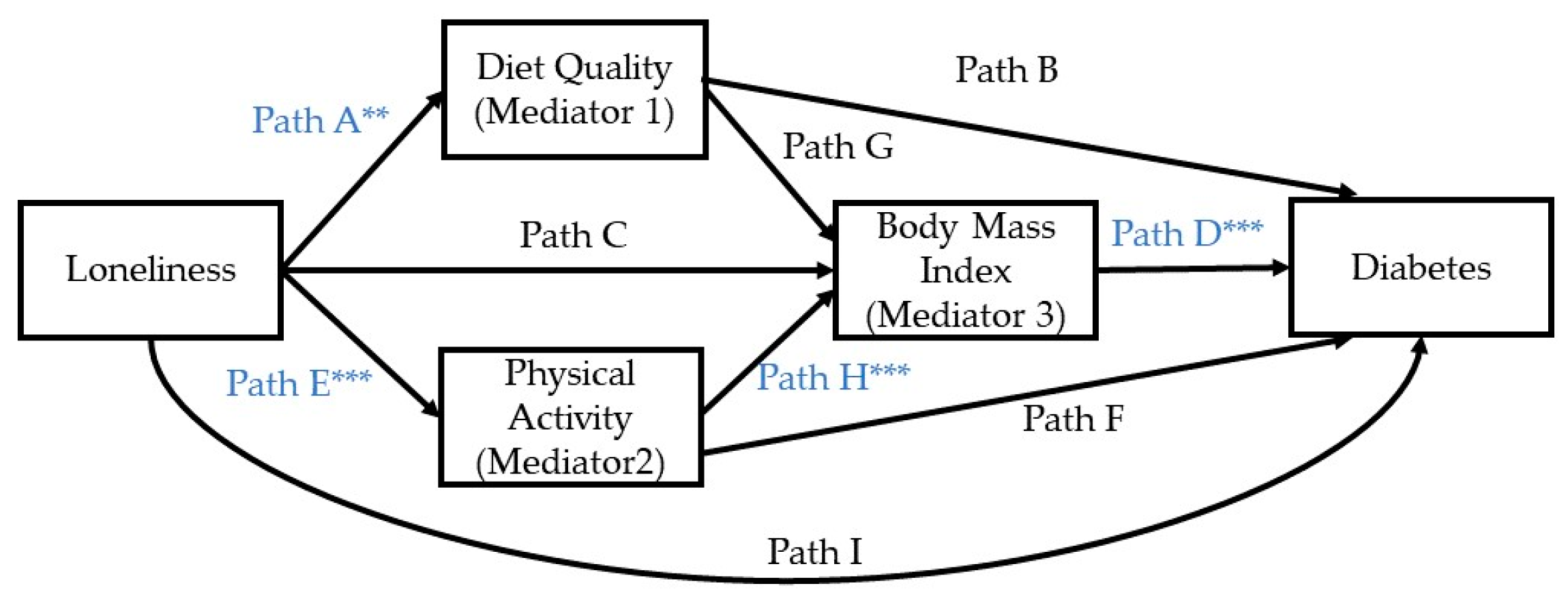
3.2. Summary of Model #80 of PROCESS Macro
3.3. Model 1. Path A: Diet Quality
3.4. Model 2: Path E: Physical Activity
3.5. Model 3: Paths C, G, H: Diet Quality, Physical Activity, BMI
3.6. Model 4: Paths B, D, F, I, and Indirect Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Christiansen, J.; Lund, R.; Qualter, P.; Andersen, C.M.; Pedersen, S.S.; Lasgaard, M. Loneliness, Social Isolation, and Chronic Disease Outcomes. Ann. Behav. Med. 2020, 55, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Hackett, R.A.; Hudson, J.L.; Chilcot, J. Loneliness and type 2 diabetes incidence: Findings from the English Longitudinal Study of Ageing. Diabetologia 2020, 63, 2329–2338. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, R.E.; Nilsen, R.M.; Strandberg, R.B. Loneliness increases the risk of type 2 diabetes: A 20 year follow-up—results from the HUNT study. Diabetologia 2023, 66, 82–92. [Google Scholar] [CrossRef]
- Wang, X.; Ma, H.; Li, X.; Heianza, Y.; Fonseca, V.; Qi, L. Joint association of loneliness and traditional risk factor control and incident cardiovascular disease in diabetes patients. Eur. Heart J. 2023, 44, 2583–2591. [Google Scholar] [CrossRef]
- Cacioppo, S.; Capitanio, J.P.; Cacioppo, J.T. Toward a neurology of loneliness. Psychol. Bull. 2014, 140, 1464–1504. [Google Scholar] [CrossRef] [PubMed]
- Hawkley, L.C. Loneliness and health. Nat. Rev. Dis. Primers 2022, 8, 22. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Cheskin, L.J.; Frankenfeld, C.L.; Rana, Z.H.; de Jonge, L. Loneliness is associated with unhealthful dietary behaviors and physical inactivity among US college students. J. Am. Coll. Health 2022, 1–6. [Google Scholar] [CrossRef]
- Richard, A.; Rohrmann, S.; Vandeleur, C.L.; Schmid, M.; Barth, J.; Eichholzer, M. Loneliness is adversely associated with physical and mental health and lifestyle factors: Results from a Swiss national survey. PLoS ONE 2017, 12, e0181442. [Google Scholar] [CrossRef]
- Ferrer-Cascales, R.; Albaladejo-Blázquez, N.; Ruiz-Robledillo, N.; Rubio-Aparicio, M.; Laguna-Pérez, A.; Zaragoza-Martí, A. Low Adherence to the Mediterranean Diet in Isolated Adolescents: The Mediation Effects of Stress. Nutrients 2018, 10, 1894. [Google Scholar] [CrossRef]
- Sirois, F.M.; Biskas, M. Loneliness and preferences for palatable foods: The role of coping. Curr. Res. Behav. Sci. 2023, 5, 100119. [Google Scholar] [CrossRef]
- Mason, T.B. Loneliness, eating, and body mass index in parent–adolescent dyads from the Family Life, Activity, Sun, Health, and Eating study. Pers. Relatsh. 2020, 27, 420–432. [Google Scholar] [CrossRef]
- Kobayashi, L.C.; Steptoe, A. Social Isolation, Loneliness, and Health Behaviors at Older Ages: Longitudinal Cohort Study. Ann. Behav. Med. 2018, 52, 582–593. [Google Scholar] [CrossRef]
- Yanguas, J.; Pinazo-Henandis, S.; Tarazona-Santabalbina, F.J. The complexity of loneliness. Acta Biomed. 2018, 89, 302–314. [Google Scholar] [CrossRef]
- Smith, K.J.; Gavey, S.; NE, R.I.; Kontari, P.; Victor, C. The association between loneliness, social isolation and inflammation: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2020, 112, 519–541. [Google Scholar] [CrossRef] [PubMed]
- Van Bogart, K.; Engeland, C.G.; Sliwinski, M.J.; Harrington, K.D.; Knight, E.L.; Zhaoyang, R.; Scott, S.B.; Graham-Engeland, J.E. The Association Between Loneliness and Inflammation: Findings From an Older Adult Sample. Front. Behav. Neurosci. 2021, 15, 801746. [Google Scholar] [CrossRef] [PubMed]
- Koyama, Y.; Nawa, N.; Yamaoka, Y.; Nishimura, H.; Sonoda, S.; Kuramochi, J.; Miyazaki, Y.; Fujiwara, T. Interplay between social isolation and loneliness and chronic systemic inflammation during the COVID-19 pandemic in Japan: Results from U-CORONA study. Brain Behav. Immun. 2021, 94, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Jaremka, L.M.; Fagundes, C.P.; Peng, J.; Bennett, J.M.; Glaser, R.; Malarkey, W.B.; Kiecolt-Glaser, J.K. Loneliness promotes inflammation during acute stress. Psychol. Sci. 2013, 24, 1089–1097. [Google Scholar] [CrossRef]
- Christiansen, J.; Larsen, F.B.; Lasgaard, M. Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people? Soc. Sci. Med. 2016, 152, 80–86. [Google Scholar] [CrossRef]
- Hackett, R.A.; Poole, L.; Hunt, E.; Panagi, L.; Steptoe, A. Loneliness and biological responses to acute stress in people with Type 2 diabetes. Psychophysiology 2019, 56, e13341. [Google Scholar] [CrossRef]
- Kusaslan Avci, D. Evaluation of the relationship between loneliness and medication adherence in patients with diabetes mellitus: A cross-sectional study. J. Int. Med. Res. 2018, 46, 3149–3161. [Google Scholar] [CrossRef]
- He, D.; Qiao, Y.; Xiong, S.; Liu, S.; Ke, C.; Shen, Y. Association between Dietary Quality and Prediabetes based on the Diet Balance Index. Sci. Rep. 2020, 10, 3190. [Google Scholar] [CrossRef] [PubMed]
- Sanjeevi, N.; Freeland-Graves, J.H. Low diet quality is associated with adverse levels of metabolic health markers and clustering of risk factors in adults with type 2 diabetes. J. Hum. Nutr. Diet. 2023, 36, 31–39. [Google Scholar] [CrossRef]
- Whitelock, E.; Ensaff, H. On Your Own: Older Adults’ Food Choice and Dietary Habits. Nutrients 2018, 10, 413. [Google Scholar] [CrossRef] [PubMed]
- Walker, D.; Beauchene, R.E. The relationship of loneliness, social isolation, and physical health to dietary adequacy of independently living elderly. J. Am. Diet. Assoc. 1991, 91, 300–304. [Google Scholar] [CrossRef]
- Delerue Matos, A.; Barbosa, F.; Cunha, C.; Voss, G.; Correia, F. Social isolation, physical inactivity and inadequate diet among European middle-aged and older adults. BMC Public Health 2021, 21, 924. [Google Scholar] [CrossRef]
- Schnurr, T.M.; Jakupović, H.; Carrasquilla, G.D.; Ängquist, L.; Grarup, N.; Sørensen, T.I.A.; Tjønneland, A.; Overvad, K.; Pedersen, O.; Hansen, T.; et al. Obesity, unfavourable lifestyle and genetic risk of type 2 diabetes: A case-cohort study. Diabetologia 2020, 63, 1324–1332. [Google Scholar] [CrossRef]
- Wild, S.H.; Byrne, C.D. ABC of obesity. Risk factors for diabetes and coronary heart disease. BMJ 2006, 333, 1009–1011. [Google Scholar] [CrossRef] [PubMed]
- Hajek, A.; König, H.H. Obesity and loneliness. Findings from a longitudinal population-based study in the second half of life in Germany. Psychogeriatrics 2019, 19, 135–140. [Google Scholar] [CrossRef]
- Jung, F.U.; Luck-Sikorski, C. Overweight and Lonely? A Representative Study on Loneliness in Obese People and Its Determinants. Obes. Facts 2019, 12, 440–447. [Google Scholar] [CrossRef]
- Oser, T.K.; Roy, S.; Parascando, J.; Mullen, R.; Radico, J.; Reedy-Cooper, A.; Moss, J. Loneliness in Primary Care Patients: Relationships With Body Mass Index and Health Care Utilization. J. Patient Cent. Res. Rev. 2021, 8, 239–247. [Google Scholar] [CrossRef]
- Beltrán-Carrillo, V.J.; Megías, Á.; González-Cutre, D.; Jiménez-Loaisa, A. Elements behind sedentary lifestyles and unhealthy eating habits in individuals with severe obesity. Int. J. Qual Stud. Health Well-Being 2022, 17, 2056967. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.K.; Lepkowski, J.M.; Powe, N.R.; LaVeist, T.; Kuczmarski, M.F.; Zonderman, A.B. Healthy aging in neighborhoods of diversity across the life span (HANDLS): Overcoming barriers to implementing a longitudinal, epidemiologic, urban study of health, race, and socioeconomic status. Ethn. Dis. 2010, 20, 267–275. [Google Scholar] [PubMed]
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res. Aging 2004, 26, 655–672. [Google Scholar] [CrossRef] [PubMed]
- Steinfeldt, L.; Anand, J.; Murayi, T. Food reporting patterns in the USDA Automated Multiple-Pass Method. Procedia Food Sci. 2013, 2, 145–156. [Google Scholar] [CrossRef]
- Guenther, P.M.; Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Buckman, D.W.; Dodd, K.W.; Casavale, K.O.; Carroll, R.J. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J. Nutr. 2014, 144, 399–407. [Google Scholar] [CrossRef]
- National Institute on Aging, Intramural Research Program. Healthy Eating Index 2010 Calculation. Available online: https://handls.nih.gov/06Coll-w01HEI.htm (accessed on 24 August 2023).
- National Cancer Institute, National Institutes of Health. Healthy Eating Index; Overview of the Methods & Calculations. Available online: https://epi.grants.cancer.gov/hei/hei-methods-and-calculations.html (accessed on 24 August 2023).
- Baecke, J.A.; Burema, J.; Frijters, J.E. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am. J. Clin. Nutr. 1982, 36, 936–942. [Google Scholar] [CrossRef]
- Tebar, W.R.; Ritti-Dias, R.M.; Fernandes, R.A.; Damato, T.M.M.; Barros, M.V.G.; Mota, J.; Andersen, L.B.; Christofaro, D.G.D. Validity and reliability of the Baecke questionnaire against accelerometer-measured physical activity in community dwelling adults according to educational level. PLoS ONE 2022, 17, e0270265. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. The 2004 HHS Poverty Guidelines. Available online: https://aspe.hhs.gov/2004-hhs-poverty-guidelines (accessed on 24 August 2023).
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; Guilford Press: New York, NY, USA, 2022. [Google Scholar]
- Bland, J.M.; Altman, D.G. Statistics notes. The odds ratio. BMJ 2000, 320, 1468. [Google Scholar] [CrossRef]
- Pels, F.; Kleinert, J. Loneliness and physical activity: A systematic review. Int. Rev. Sport Exerc. Psychol. 2016, 9, 231–260. [Google Scholar] [CrossRef]
- Abe, M.; Fujii, H.; Funakoshi, S.; Satoh, A.; Kawazoe, M.; Maeda, T.; Tada, K.; Yokota, S.; Yamanokuchi, T.; Yoshimura, C.; et al. Comparison of Body Mass Index and Waist Circumference in the Prediction of Diabetes: A Retrospective Longitudinal Study. Diabetes Ther. 2021, 12, 2663–2676. [Google Scholar] [CrossRef]
- Haghighatdoost, F.; Amini, M.; Feizi, A.; Iraj, B. Are body mass index and waist circumference significant predictors of diabetes and prediabetes risk: Results from a population based cohort study. World J. Diabetes 2017, 8, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Andreyeva, T. Diet Quality and Health in Older Americans. Nutrients 2022, 14, 1198. [Google Scholar] [CrossRef] [PubMed]
- Zaman, R.; Hankir, A.; Jemni, M. Lifestyle Factors and Mental Health. Psychiatr. Danub. 2019, 31, 217–220. [Google Scholar] [PubMed]
- Walsh, R. Lifestyle and Mental Health. Am. Psychol. 2011, 66, 579–592. [Google Scholar] [CrossRef] [PubMed]
- Oftedal, S.; Kolt, G.S.; Holliday, E.G.; Stamatakis, E.; Vandelanotte, C.; Brown, W.J.; Duncan, M.J. Associations of health-behavior patterns, mental health and self-rated health. Prev. Med. 2019, 118, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, M.F.; Cremer Sees, A.; Hotchkiss, L.; Cotugna, N.; Evans, M.K.; Zonderman, A.B. Higher Healthy Eating Index-2005 scores associated with reduced symptoms of depression in an urban population: Findings from the Healthy Aging in Neighborhoods of Diversity Across the Life Span (HANDLS) study. J. Am. Diet. Assoc. 2010, 110, 383–389. [Google Scholar] [CrossRef]
- Kuczmarski, M.F.; Orsega-Smith, E.; Mode, N.A.; Rawal, R.; Evans, M.K.; Zonderman, A.B. Healthy Behaviors Associated with Changes in Mental and Physical Strength in Urban African American and White Adults. Nutrients 2021, 13, 1824. [Google Scholar] [CrossRef]
- Carroll, S.J.; Dale, M.J.; Niyonsenga, T.; Taylor, A.W.; Daniel, M. Associations between area socioeconomic status, individual mental health, physical activity, diet and change in cardiometabolic risk amongst a cohort of Australian adults: A longitudinal path analysis. PLoS ONE 2020, 15, e0233793. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Prochaska, J.O. A Review of Multiple Health Behavior Change Interventions for Primary Prevention. Am. J. Lifestyle Med. 2011, 5, 1883. [Google Scholar] [CrossRef]
- Barbu, E.; Popescu, M.R.; Popescu, A.C.; Balanescu, S.M. Inflammation as A Precursor of Atherothrombosis, Diabetes and Early Vascular Aging. Int. J. Mol. Sci. 2022, 23, 963. [Google Scholar] [CrossRef]
| Characteristic | Overall Sample n = 1713 | African American n = 1044 | White n = 669 | p |
|---|---|---|---|---|
| Age, y X ± SE | 56.6 ± 0.2 | 56.7 ± 0.3 | 56.4 ± 0.3 | 0.416 |
| Male, % | 41.0 | 41.7 | 40.1 | 0.510 |
| African American, % | 60.9 | - | - | - |
| Income, % <125% poverty | 37.7 | 41.1 | 32.4 | <0.001 |
| Education, y X ± SE | 12.3 ± 0.1 | 12.2 ± 0.1 | 12.4 ± 0.1 | 0.042 |
| Alcohol intake, g X ± SE | 7.5 ± 0.6 | 7.7 ± 0.7 | 7.4 ± 0.9 | 0.763 |
| Body Mass Index, kg/m2 X ± SE | 31.0 ± 7.9 | 31.0 ± 0.2 | 30.9 ± 0.3 | 0.753 |
| Diabetes | 0.008 | |||
| Diabetic, % | 24.0 | 26.1 | 20.8 | |
| Pre-diabetic, % | 15.9 | 14.2 | 18.5 | |
| Healthy Eating Index-2012, X ± SE | 49.05 ± 0.29 | 48.91 ± 0.35 | 49.26 ± 0.51 | 0.563 |
| Physical activity, mins/week X ± SE | 187 ± 6 | 190 ± 7 | 182 ± 9 | 0.501 |
| Loneliness: | ||||
| Total score, X ± SE | 4.73 ± 0.04 | 4.68 ± 0.05 | 4.81 ± 0.07 | 0.124 |
| You feel that you lack companionship | 0.394 | |||
| Often, % | 14.4 | 14.1 | 14.9 | |
| Some of the time, % | 41.0 | 42.3 | 39.0 | |
| You feel left out | 0.033 | |||
| Often, % | 7.5 | 6.2 | 9.4 | |
| Some of the time, % | 39.1 | 38.8 | 39.6 | |
| You feel isolated from others | 0.067 | |||
| Often, % | 7.8 | 7.2 | 8.8 | |
| Some of the time, % | 33.3 | 31.8 | 35.7 |
| Paths | Direct Effect b | p | Odds Ratio | Confidence Interval | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| A: Loneliness -> Diet quality | −0.485 ± 0.166 | 0.004 | 0.33 | 0.15 | 0.69 |
| B: Diet Quality -> Diabetes | 0.006 ± 0.005 | 0.214 | 1.01 | 0.99 | 1.03 |
| C: Loneliness -> Body mass index | −0.021 ± 0.112 | 0.852 | 0.95 | 0.58 | 1.58 |
| D: BMI -> Diabetes | 0.065 ± 0.007 | <0.001 | 1.16 | 1.12 | 1.20 |
| E: Loneliness -> Physical activity | −16.702 ± 3.305 | <0.001 | 1.98 × 10−17 | 6.54 × 10−24 | 6.04 × 10−11 |
| F: Physical activity -> Diabetes | −0.0002 ± 0.0002 | 0.382 | 1.00 | 1.00 | 1.00 |
| G: Diet quality -> BMI | 0.030 ± 0.016 | 0.068 | 1.07 | 0.99 | 1.15 |
| H: Physical activity -> BMI | −0.006 ± 0.001 | <0.001 | 0.99 | 0.98 | 0.99 |
| I: Loneliness -> Diabetes | 0.061 ± 0.032 | 0.056 | 1.15 | 1.00 | 1.33 |
| Relationship | Indirect Effect a | Bootstrap Confidence Interval | |
|---|---|---|---|
| Lower Bound | Upper Bound | ||
| Loneliness -> Diet quality -> Diabetes | −0.0028 ± 0.0025 | −0.0086 | 0.0013 |
| Loneliness -> Physical activity -> Diabetes | 0.0035 ± 0.0041 | −0.0042 | 0.0123 |
| Loneliness -> Body mass index -> Diabetes | −0.0014 ± 0.0080 | −0.0172 | 0.0139 |
| Loneliness -> Diet quality -> BMI ->Diabetes | −0.0009 ± 0.0006 | −0.0024 | 0.0000 |
| Loneliness -> Physical activity -> BMI -> Diabetes | 0.0061 ± 0.0015 * | 0.0036 | 0.0094 |
| Outcome: Heathy Eating Index | Coefficient Loge (OR) | Standard Error | t | p | Confidence Intervals | |
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Constant | 36.2309 | 2.9483 | 12.2888 | 0.0000 | 30.4483 | 42.0136 |
| Loneliness | −0.4845 | 0.1663 | −2.9131 | 0.0036 | −0.8107 | −0.1583 |
| Age | 0.1244 | 0.0309 | 4.0265 | 0.0001 | 0.0638 | 0.1850 |
| Race | 0.0372 | 0.5691 | 0.0653 | 0.9479 | −1.0791 | 1.1534 |
| Sex | −3.0711 | 0.5651 | −5.4342 | 0.0000 | −4.1796 | −1.9627 |
| Poverty | −1.6233 | 0.5910 | −2.7467 | 0.0061 | −2.7825 | −0.4642 |
| Alcohol intake | 0.0271 | 0.0121 | 2.2459 | 0.0248 | 0.0034 | 0.0508 |
| Education | 1.1700 | 0.1127 | 10.3835 | 0.0000 | 0.9490 | 1.3910 |
| Outcome: Physical Activity | Coefficient Loge (OR) | Standard Error | t | p | Confidence Intervals | |
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Constant | 315.5284 | 58.5894 | 5.3854 | 0.0000 | 200.6138 | 430.4430 |
| Loneliness | −16.7017 | 3.3051 | −5.0533 | 0.0000 | −23.1842 | 10.2192 |
| Age | −3.8177 | 0.6140 | −6.2183 | 0.0000 | −5.0219 | −2.6135 |
| Race | 9.1480 | 11.3098 | 0.8089 | 0.4187 | −13.0345 | 31.3305 |
| Sex | 44.0386 | 11.2308 | 3.9212 | 0.0001 | 22.0109 | 66.0662 |
| Poverty | −8.5966 | 11.7445 | −0.7320 | 0.4643 | −31.6318 | 14.4386 |
| Alcohol intake | 0.1375 | 0.2398 | 0.5734 | 0.5664 | −0.3328 | 0.6078 |
| Education | 8.1480 | 2.2393 | 3.6387 | 0.0003 | 3.7560 | 12.5399 |
| Outcome: BMI | Coefficient Loge (OR) | Standard Error | t | p | Confidence Intervals | |
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Constant | 41.0491 | 2.0533 | 19.9922 | 0.0000 | 37.0219 | 45.0762 |
| Loneliness | −0.0208 | 0.1116 | −0.1866 | 0.8520 | −0.2396 | 0.1980 |
| HEI | 0.0296 | 0.0162 | 1.8248 | 0.0682 | −0.0022 | 0.0614 |
| Physical activity | −0.0056 | 0.0008 | −6.8672 | 0.0000 | −0.0072 | −0.0040 |
| Age | −0.0747 | 0.0209 | −3.5704 | 0.0004 | −0.1157 | −0.0336 |
| Race | 0.3106 | 0.3784 | 0.8208 | 0.4119 | −0.4316 | 1.0529 |
| Sex | −2.8089 | 0.3813 | −7.3665 | 0.0000 | −3.3568 | −2.0610 |
| Poverty | −1.0160 | 0.3938 | −2.5799 | 0.0100 | −1.7883 | −0.2436 |
| Alcohol intake | −0.0384 | 0.0080 | −4.7818 | 0.0000 | −0.0542 | −0.0227 |
| Education | −0.0799 | 0.0774 | −1.0329 | 0.3018 | −0.2316 | 0.0718 |
| Outcome: Diabetes | Coefficient Loge (OR) | Standard Error | t | p | Confidence Intervals | |
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Constant | −5.1235 | 0.6699 | −7.6477 | 0.0000 | −6.4365 | −3.8104 |
| Loneliness | 0.0605 | 0.0316 | 1.9136 | 0.0557 | −0.0015 | 0.1225 |
| HEI | 0.0057 | 0.0046 | 1.2426 | 0.2104 | −0.0033 | 0.0147 |
| Physical activity | −0.0002 | 0.0002 | −0.8747 | 0.3817 | −0.0007 | 0.0003 |
| BMI | 0.0651 | 0.0072 | 8.9850 | 0.0000 | 0.0509 | 0.0793 |
| Age | 0.0450 | 0.0061 | 7.3665 | 0.0000 | 0.0330 | 0.0569 |
| Race | 0.0246 | 0.1074 | 0.2288 | 0.8190 | −0.1859 | 0.2351 |
| Sex | 0.4198 | 0.1104 | 3.8034 | 0.0001 | 0.2035 | 0.6361 |
| Poverty | −0.0974 | 0.1122 | −0.8685 | 0.3851 | −0.3173 | 0.1224 |
| Alcohol intake | −0.0057 | 0.0028 | −2.0452 | 0.0408 | −0.0112 | −0.0002 |
| Education | −0.0712 | 0.0221 | −3.2216 | 0.0013 | −0.1146 | −0.0279 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuczmarski, M.F.; Orsega-Smith, E.; Evans, M.K.; Zonderman, A.B. The Association of Loneliness with Diabetes Is Mediated by Physical Activity and BMI but Not Diet Quality. Nutrients 2023, 15, 4923. https://doi.org/10.3390/nu15234923
Kuczmarski MF, Orsega-Smith E, Evans MK, Zonderman AB. The Association of Loneliness with Diabetes Is Mediated by Physical Activity and BMI but Not Diet Quality. Nutrients. 2023; 15(23):4923. https://doi.org/10.3390/nu15234923
Chicago/Turabian StyleKuczmarski, Marie Fanelli, Elizabeth Orsega-Smith, Michele K. Evans, and Alan B. Zonderman. 2023. "The Association of Loneliness with Diabetes Is Mediated by Physical Activity and BMI but Not Diet Quality" Nutrients 15, no. 23: 4923. https://doi.org/10.3390/nu15234923
APA StyleKuczmarski, M. F., Orsega-Smith, E., Evans, M. K., & Zonderman, A. B. (2023). The Association of Loneliness with Diabetes Is Mediated by Physical Activity and BMI but Not Diet Quality. Nutrients, 15(23), 4923. https://doi.org/10.3390/nu15234923





