The Association of Physical Activity Level with Micronutrient and Health Status of Austrian Bank Employees
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample Recruitment
2.2. Research Procedure and Measures
2.3. Physical Activity and Sedentary Behavior
2.4. Blood Sample Analysis
2.5. Statistical Analysis
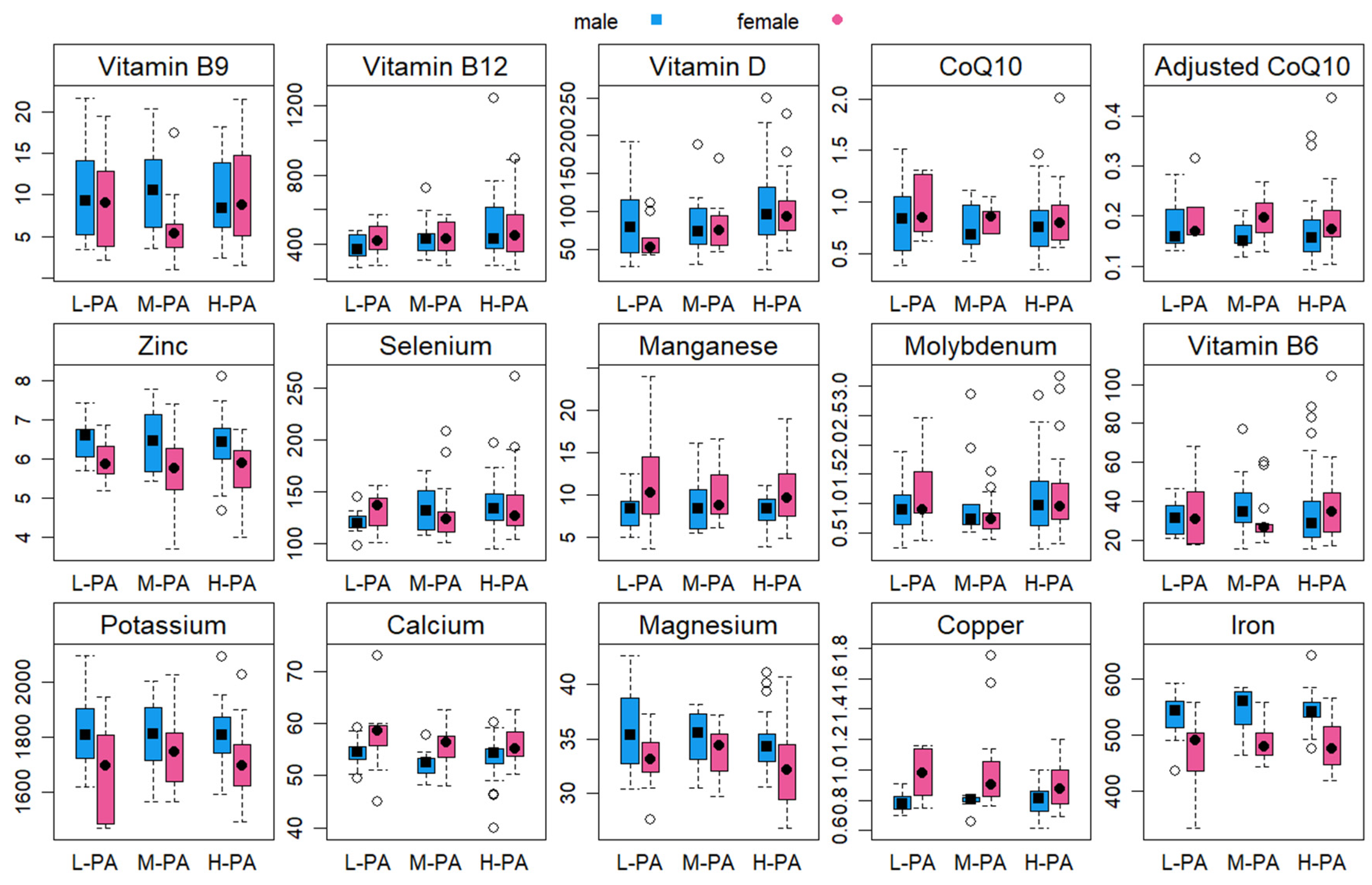
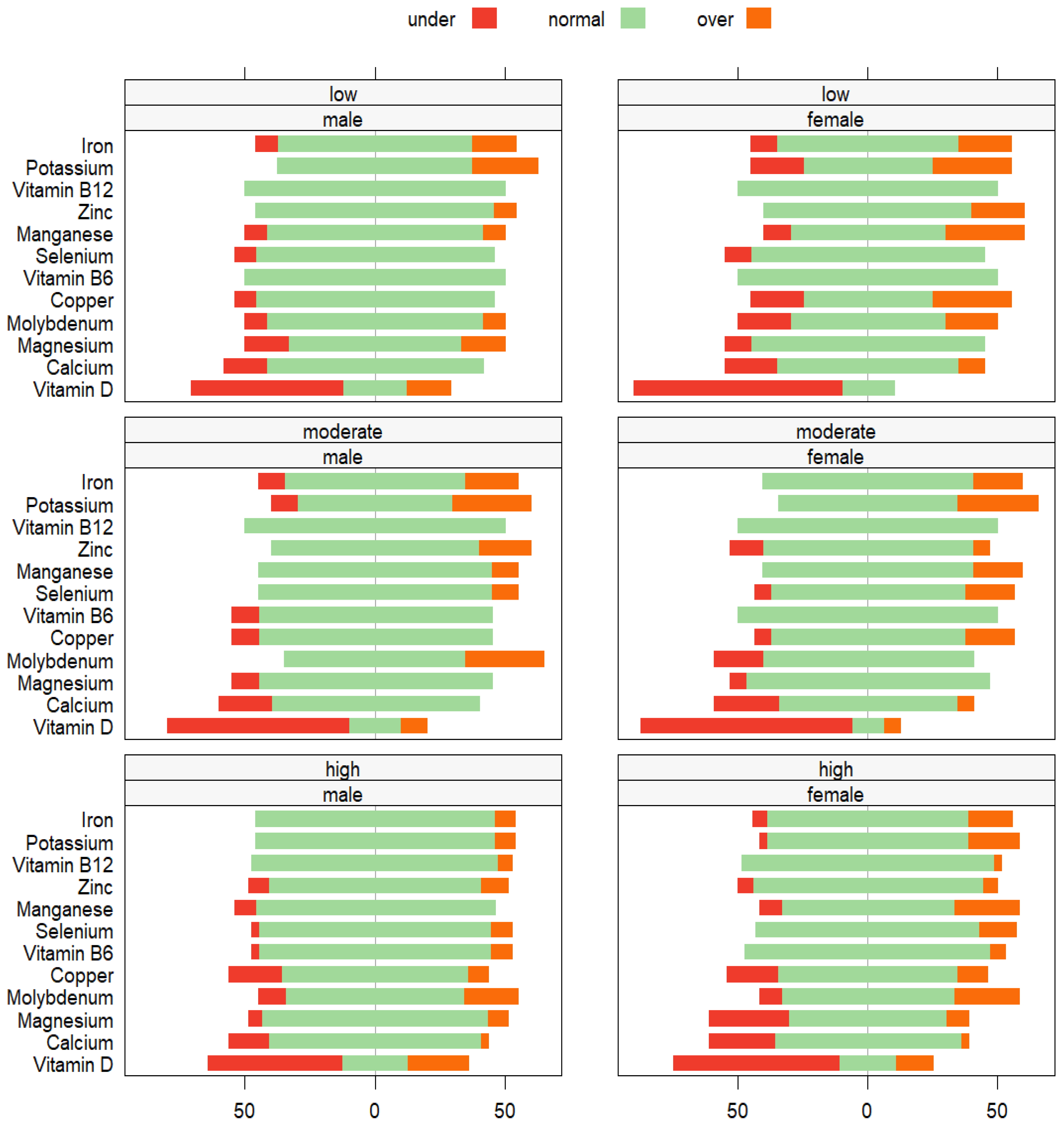
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American College of Lifestyle Medicine—JAMA Physician Competencies for Prescribing Lifestyle Medicine. Available online: https://lifestylemedicine.org/overview/ (accessed on 20 October 2022).
- Mikkelsen, B.; Williams, J.; Rakovac, I.; Wickramasinghe, K.; Hennis, A.; Shin, H.R.; Farmer, M.; Weber, M.; Berdzuli, N.; Borges, C.; et al. A Life Course Approach to Prevention and Control of Non-Communicable Diseases. BMJ 2019, 364, L257. [Google Scholar] [CrossRef] [PubMed]
- Hellénius, M.; Sundberg, C.J. Physical Activity as Medicine: Time to Translate Evidence into Clinical Practice. Br. J. Sports Med. 2011, 45, 158. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 26 March 2023).
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide Trends in Insufficient Physical Activity from 2001 to 2016: A Pooled Analysis of 358 Population-Based Surveys with 1.9 Million Participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Global Status Report on Physical Activity. 2022. Available online: https://www.who.int/teams/health-promotion/physical-activity/global-status-report-on-physical-activity-2022 (accessed on 26 March 2023).
- Lamers, Y. Approaches to Improving Micronutrient Status Assessment at the Population Level. Proc. Nutr. Soc. 2019, 78, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Ashton, K.; Harvey, L.J.; Decsi, T.; Fairweather-Tait, S.J. Assessing Potential Biomarkers of Micronutrient Status by Using a Systematic Review Methodology: Methods. Am. J. Clin. Nutr. 2009, 89, 1953S–1959S. [Google Scholar] [CrossRef] [PubMed]
- McClung, H.L.; Ptomey, L.T.; Shook, R.P.; Aggarwal, A.; Gorczyca, A.M.; Sazonov, E.S.; Becofsky, K.; Weiss, R.; Das, S.K. Dietary Intake and Physical Activity Assessment: Current Tools, Techniques, and Technologies for Use in Adult Populations. Am. J. Prev. Med. 2018, 55, e93–e104. [Google Scholar] [CrossRef] [PubMed]
- Westerterp, K.R. Assessment of Physical Activity: A Critical Appraisal. Eur. J. Appl. Physiol. 2009, 105, 823–828. [Google Scholar] [CrossRef]
- Schulte, P.A.; Wagner, G.R.; Ostry, A.; Blanciforti, L.A.; Cutlip, R.G.; Krajnak, K.M.; Luster, M.; Munson, A.E.; O’Callaghan, J.P.; Parks, C.G.; et al. Work, Obesity, and Occupational Safety and Health. Am. J. Public. Health 2007, 97, 428–436. [Google Scholar] [CrossRef]
- Harrison, J.; Dawson, L. Occupational Health: Meeting the Challenges of the Next 20 Years. Saf. Health Work. 2016, 7, 143–149. [Google Scholar] [CrossRef]
- Statistics Austria. Österreichische Gesundheitsbefragung 2019—Hauptergebnisse; Statistics Austria: Vienna, Austria, 2019; Available online: https://www.statistik.at/fileadmin/publications/Oesterreichische-Gesundheitsbefragung2019_Hauptergebnisse.pdf (accessed on 26 March 2023).
- Thivel, D.; Tremblay, A.; Genin, P.M.; Panahi, S.; Rivière, D.; Duclos, M. Physical Activity, Inactivity, and Sedentary Behaviors: Definitions and Implications in Occupational Health. Front. Public Health 2018, 6, 288. [Google Scholar] [CrossRef]
- van Uffelen, J.G.; Wong, J.; Chau, J.Y.; van der Ploeg, H.P.; Riphagen, I.; Gilson, N.D.; Burton, N.W.; Healy, G.N.; Thorp, A.A.; Clark, B.K.; et al. Occupational Sitting and Health Risks: A Systematic Review. Am. J. Prev. Med. 2010, 39, 379–388. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.C.; Chey, T.; Stamatakis, E.; Brown, W.J.; Matthews, C.E.; Bauman, A.E.; van der Ploeg, H.P. Daily Sitting Time and All-Cause Mortality: A Meta-Analysis. PLoS ONE 2013, 8, e80000. [Google Scholar] [CrossRef] [PubMed]
- Ganesh Kumar, S.; Deivanai Sundaram, N. Prevalence and Risk Factors of Hypertension among Bank Employees in Urban Puducherry, India. Int. J. Occup. Environ. Med. 2014, 5, 94–100. [Google Scholar] [PubMed]
- Shenkin, A. Micronutrients in Health and Disease. Postgrad. Med. J. 2006, 82, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E. Global Distribution and Disease Burden Related to Micronutrient Deficiencies; Nestlé Nutrition Institute Workshop Series. 2014; pp. 21–28. Available online: https://www.nestlenutrition-institute.org/videos/global-distribution-and-disease-burden-related-micronutrient-deficiencies (accessed on 20 October 2023).
- Elmadfa, I. Österreichischer Ernährungsbericht 2012. Available online: https://ernaehrungsbericht.univie.ac.at/fileadmin/user_upload/dep_ernaehrung/forschung/ernaehrungsberichte/oesterr_ernaehrungsbericht_2012.pdf (accessed on 26 March 2023).
- Elmadfa, I. Österreichischer Ernährungsbericht 2017. Available online: https://ernaehrungsbericht.univie.ac.at/fileadmin/user_upload/dep_ernaehrung/forschung/ernaehrungsberichte/erna_hrungsbericht2017_web_20171018.pdf (accessed on 26 March 2023).
- Wimalawansa, S.J. Associations of Vitamin D with Insulin Resistance, Obesity, Type 2 Diabetes, and Metabolic Syndrome. J. Steroid Biochem. Mol. Biol. 2018, 175, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Strange, R.C.; Shipman, K.E.; Ramachandran, S. Metabolic Syndrome: A Review of the Role of Vitamin D in Mediating Susceptibility and Outcome. World J. Diabetes 2015, 6, 896–911. [Google Scholar] [CrossRef] [PubMed]
- Houston, M.C.; Harper, K.J. Potassium, Magnesium, and Calcium: Their Role in Both the Cause and Treatment of Hypertension. J. Clin. Hypertens. 2008, 10, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Palfrey, H.A.; Pathak, R.; Kadowitz, P.J.; Gettys, T.W.; Murthy, S.N. The Metabolism and Significance of Homocysteine in Nutrition and Health. Nutr. Metab. 2017, 14, 78. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.; Man, C.; Xu, J.; Fan, Y. Elevated Homocysteine Levels and Risk of Cardiovascular and All-Cause Mortality: A Meta-Analysis of Prospective Studies. J. Zhejiang Univ. Sci. B 2015, 16, 78–86. [Google Scholar] [CrossRef]
- Saini, R. Coenzyme Q10: The Essential Nutrient. J. Pharm. Bioallied Sci. 2011, 3, 466–467. [Google Scholar] [CrossRef]
- Mantle, D.; Lopez-Lluch, G.; Hargreaves, I.P. Coenzyme Q10 Metabolism: A Review of Unresolved Issues. Int. J. Mol. Sci. 2023, 24, 2585. [Google Scholar] [CrossRef] [PubMed]
- GoInvo. Determinant of Health. Available online: https://www.goinvo.com/vision/determinants-of-health/ (accessed on 26 March 2023).
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health Benefits of Physical Activity: The Evidence. CMAJ 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Fogelholm, M. Micronutrients: Interaction between Physical Activity, Intakes, and Requirements. Public Health Nutr. 1999, 2, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Maughan, R.J. Role of Micronutrients in Sport and Physical Activity. Br. Med. Bull. 1999, 55, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Yesildemir, O.; Gencer Bingol, F.; Icer, M.A.; Koksal, E. Association of Physical Activity Status with Dietary Energy Density and Nutritional Adequacy. Food Sci. Technol. 2022, 42, e50021. [Google Scholar] [CrossRef]
- Hughes, R.L.; Holscher, H.D. Fueling Gut Microbes: A Review of the Interaction between Diet, Exercise, and the Gut Microbiota in Athletes. Adv. Nutr. 2021, 12, 2190–2215. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Liu, Y.; Sun, Y.; Zhang, X. Combined Physical Exercise and Diet: Regulation of Gut Microbiota to Prevent and Treat Metabolic Disease: A Review. Nutrients 2022, 14, 4774. [Google Scholar] [CrossRef] [PubMed]
- Monda, V.; Villano, I.; Messina, A.; Valenzano, A.; Esposito, T.; Moscatelli, F.; Viggiano, A.; Cibelli, G.; Chieffi, S.; Monda, M.; et al. Exercise Modifies the Gut Microbiota with Positive Health Effects. Oxid. Med. Cell. Longev. 2017, 2017, 3831972. [Google Scholar] [CrossRef]
- Beck, K.L.; von Hurst, P.R.; O’Brien, W.J.; Badenhorst, C.E. Micronutrients and Athletic Performance: A Review. Food Chem. Toxicol. 2021, 158, 112618. [Google Scholar] [CrossRef]
- Tardy, A.L.; Pouteau, E.; Marquez, D.; Yilmaz, C.; Scholey, A. Vitamins and Minerals for Energy, Fatigue, and Cognition: A Narrative Review of the Biochemical and Clinical Evidence. Nutrients 2020, 12, 228. [Google Scholar] [CrossRef]
- Martin, M. (Ed.) Das Standardlabor in der Naturheilkundlichen Praxis [The Standard Laboratory in Naturopathic Practice]; Urban & Fischer in Elsevier: Amsterdam, The Netherlands, 2016; ISBN 978-3-437-56303-4. [Google Scholar]
- World Health Organization (WHO). Body Mass Index. Available online: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index (accessed on 26 March 2023).
- Melina, V.; Craig, W.; Levin, S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. J. Acad. Nutr. Diet. 2016, 116, 1970–1980. [Google Scholar] [CrossRef] [PubMed]
- Wirnitzer, K.; Motevalli, M.; Tanous, D.; Wirnitzer, G.; Leitzmann, C.; Wagner, K.-H.; Rosemann, T.; Knechtle, B. Training and Racing Behaviors of Omnivorous, Vegetarian, and Vegan Endurance Runners—Results from the NURMI Study (Step 1). Nutrients 2021, 13, 3521. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Global Physical Activity Questionnaire (GPAQ). Available online: https://www.who.int/publications/m/item/global-physical-activity-questionnaire (accessed on 26 March 2023).
- World Health Organization (WHO). WHO Guidelines on Physical Activity and Sedentary Behaviour. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 26 March 2023).
- Schulz-Ruhtenberg, N. Mikronährstoffe und Aminosäuren—Einsatz in der Sporternährung. Available online: https://sportaerztezeitung.com/rubriken/ernaehrung/2474/mikronaehrstoffe-und-aminosaeuren/ (accessed on 20 October 2023).
- Mikronährstoffdefizite. 2019. Available online: https://www.sportaerztezeitung.de/sportkardiologie-abo/articles/mikronaehrstoffdefizite (accessed on 26 March 2023).
- Gaffney-Stomberg, E. The Impact of Trace Minerals on Bone Metabolism. Biol. Trace Elem. Res. 2019, 188, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Refsum, H.; Smith, A.D.; Ueland, P.M.; Nexo, E.; Clarke, R.; McPartlin, J.; Ebbing, M. Facts and Recommendations About Total Homocysteine Determinations: An Expert Opinion. Clin. Chem. 2004, 50, 3–32. [Google Scholar] [CrossRef] [PubMed]
- Niklowitz, P.; Onur, S.; Fischer, A.; Laudes, M.; Palussen, M.; Menke, T.; Döring, F. Coenzyme Q10 Serum Concentration and Redox Status in European Adults: Influence of Age, Sex, and Lipoprotein Concentration. J. Clin. Biochem. Nutr. 2016, 58, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Caspersen, C.J. Sedentary Behaviour and Cardiovascular Disease: A Review of Prospective Studies. Int. J. Epidemiol. 2012, 41, 1338–1353. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U. Infographic: Physical Activity, Sitting Time, and Mortality. Br. J. Sports Med. 2018, 52, 1164–1165. [Google Scholar] [CrossRef]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary Time and Its Association with Risk for Disease Incidence, Mortality, and Hospitalization in Adults: A Systematic Review and Meta-Analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef]
- World Health Organization (WHO). 2021 Physical Activity Factsheets. Available online: https://sport.ec.europa.eu/sites/default/files/2021-11/PA%20European%20Report%202021%20Web_v1_1.pdf (accessed on 26 March 2023).
- Krug, S.J.S.; Mensink, G.B.M.; Müters, S.; Finger, J.D.; Lampert, T. English Version of “Ko¨rperliche Aktivita¨t. Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1)”. Bundesgesundheitsblatt 2013, 56, 765–771. [Google Scholar] [CrossRef]
- Cattafesta, M.; Bissoli, N.S.; Salaroli, L.B. Metabolic Syndrome and C-reactive Protein in Bank Employees. Diabetes Metab. Syndr. Obes. 2016, 9, 137–144. [Google Scholar]
- Statistics Austria. Overweight and Obesity. Available online: https://www.statistik.at/en/statistics/population-and-society/health/health-determinants/overweight-and-obesity (accessed on 26 March 2023).
- Sanchi, G.R.; Borges, L.R. Lifestyle and Nutritional Status of Employees of a Chain of Banks in Pelotas, Rio Grande do Sul, Brazil. Rev. Bras. Med. Trab. 2020, 17, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Cattafesta, M.; Salaroli, L.B. Diets High in Vegetables, Fruits, Cereals, and Tubers as a Protective Factor for Metabolic Syndrome in Bank Employees. Diabetes Metab. Syndr. Obes. 2018, 11, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Addo, P.N.; Nyarko, K.M.; Sackey, S.O.; Akweongo, P.; Sarfo, B. Prevalence of Obesity and Overweight and Associated Factors among Financial Institution Workers in Accra Metropolis, Ghana: A Cross-Sectional Study. BMC Res. Notes 2015, 8, 599. [Google Scholar] [CrossRef] [PubMed]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef] [PubMed]
- Motevalli, M.; Wagner, K.-H.; Leitzmann, C.; Tanous, D.; Wirnitzer, G.; Knechtle, B.; Wirnitzer, K. Female Endurance Runners Have a Healthier Diet than Males—Results from the NURMI Study (Step 2). Nutrients 2022, 14, 2590. [Google Scholar] [CrossRef] [PubMed]
- Rennie, K.L.; Johnson, L.; Jebb, S.A. Behavioural Determinants of Obesity. Best Pract. Res. Clin. Endocrinol. Metab. 2005, 19, 343–358. [Google Scholar] [CrossRef] [PubMed]
- Sherar, L.B.; Esliger, D.W.; Baxter-Jones, A.D.; Tremblay, M.S. Age and Gender Differences in Youth Physical Activity: Does Physical Maturity Matter? Med. Sci. Sports Exerc. 2007, 39, 830–835. [Google Scholar] [CrossRef]
- Kleinke, F.; Penndorf, P.; Ulbricht, S.; Dörr, M.; Hoffmann, W.; van den Berg, N. Levels of and Determinants for Physical Activity and Physical Inactivity in a Group of Healthy Elderly People in Germany: Baseline Results of the MOVING-Study. PLoS ONE 2020, 15, e0237495. [Google Scholar] [CrossRef]
- Wirnitzer, K.C.; Drenowatz, C.; Cocca, A.; Tanous, D.R.; Motevalli, M.; Wirnitzer, G.; Schätzer, M.; Ruedl, G.; Kirschner, W. Health Behaviors of Austrian Secondary Level Pupils at a Glance: First Results of the From Science 2 School Study Focusing on Sports Linked to Mixed, Vegetarian, and Vegan Diets. Int. J. Environ. Res. Public Health 2021, 23, 12782. [Google Scholar] [CrossRef]
- Wirnitzer, K.C.; Drenowatz, C.; Cocca, A.; Tanous, D.R.; Motevalli, M.; Wirnitzer, G.; Schätzer, M.; Ruedl, G.; Kirschner, W. Health Behaviors of Austrian Secondary School Teachers and Principals at a Glance: First Results of the From Science 2 School Study Focusing on Sports Linked to Mixed, Vegetarian, and Vegan Diets. Nutrients 2022, 14, 1065. [Google Scholar] [CrossRef]
- Wirnitzer, K.C.; Motevalli, M.; Cocca, A.; Tanous, D.R.; Motevalli, M.; Wirnitzer, G.; Schätzer, M.; Ruedl, G.; Kirschner, W. Health Behavior of Austrian Tertiary Students Focusing on Diet Type Linked to Sports and Exercise—First Glimpse of Results from the “Sustainably Healthy—From Science 2 High School and University” Study. Front. Public Health 2023, 11, 1129004. [Google Scholar] [CrossRef]
- Wirnitzer, K.C.; Motevalli, M.; Tanous, D.R.; Wirnitzer, G.; Wagner, K.H.; Schätzer, M.; Drenowatz, C.; Cocca, A.; Ruedl, G.; Kirschner, W. A Glimpse of Academic Staff Health Behavior on Diet Type and Physical Activity at Austrian Universities: First Findings from the “Sustainably Healthy—From Science 2 High School & University” Study. Front. Public Health 2023, 11, 1194602. [Google Scholar] [PubMed]
- Luzak, A.; Heier, M.; Thorand, B.; Laxy, M.; Nowak, D.; Peters, A.; Schulz, H. Physical Activity Levels, Duration Pattern and Adherence to WHO Recommendations in German Adults. PLoS ONE 2017, 12, e0172503. [Google Scholar] [CrossRef] [PubMed]
- Aderibigbe, S.A.; Sule, G.O.; Olatona, F.A.; Goodman, O.O.; Sekoni, O.O. Knowledge and Practice of Sedentary Lifestyle Among Bankers in Abuja, North-Central Nigeria. Res. J. Health Sci. 2017, 5, 167. [Google Scholar]
- Nketiah, G.B.; Odoi-Agyarko, K.; Ndanu, T.A.; Hayford, F.E.A.; Amoh, G.; Lawson, H. Physical Inactivity Among Corporate Bank Workers in Accra, Ghana: Implications for Health Promotion. PLoS ONE 2023, 18, e0277994. [Google Scholar] [CrossRef] [PubMed]
- Kelly, S.; Martin, S.; Kuhn, I.; Cowan, A.; Brayne, C.; Lafortune, L. Barriers and Facilitators to the Uptake and Maintenance of Healthy Behaviors by People at Mid-Life: A Rapid Systematic Review. PLoS ONE 2016, 11, e0145074. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.-M.; The Lancet Sedentary Behaviour Working Group. Does Physical Activity Attenuate, or Even Eliminate, the Detrimental Association of Sitting Time with Mortality? A Harmonized Meta-Analysis of Data from More Than 1 Million Men and Women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- DGE Nutrition Report. Available online: https://www.dge.de/english/nutrition-reports/ (accessed on 26 March 2023).
- Wirnitzer, K.; Motevalli, M.; Tanous, D.; Wirnitzer, G.; Leitzmann, C.; Pichler, R.; Rosemann, T.; Knechtle, B. Who Is Running in the D-A-CH Countries? An Epidemiological Approach of 2455 Omnivorous, Vegetarian, and Vegan Recreational Runners—Results from the NURMI Study (Step 1). Nutrients 2022, 14, 677. [Google Scholar] [CrossRef]
- Elmadfa, I.; Meyer, A.L.; Wottawa, D.; Wagner, K.; Hasenegger, V. Vitamin D Intake and Status in Austria and Its Effects on Some Health Indicators. Austin J. Nutr. Metab. 2017, 4, 1050. [Google Scholar]
- Cui, A.; Zhang, T.; Xiao, P.; Fan, Z.; Wang, H.; Zhuang, Y. Global and Regional Prevalence of Vitamin D Deficiency in Population-Based Studies from 2000 to 2022: A Pooled Analysis of 7.9 Million Participants. Front. Nutr. 2023, 10, 1070808. [Google Scholar] [CrossRef]
- Lips, P. Vitamin D Status and Nutrition in Europe and Asia. J. Steroid Biochem. Mol. Biol. 2007, 103, 620–625. [Google Scholar] [CrossRef]
- Palacios, C.; Gonzalez, L. Is Vitamin D Deficiency a Major Global Public Health Problem? J. Steroid Biochem. Mol. Biol. 2014, 144, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Brett, A.S. Standard Definition of Vitamin D Deficiency Is Challenged. Available online: https://www.jwatch.org/na44769/2017/08/15/standard-definition-vitamin-d-deficiency-challenged (accessed on 26 March 2023).
- Murphy, R.; Ciappio, E.; McBurney, M. Risk of Deficiency in Multiple Concurrent Micronutrients in Children and Adults in the United States. Nutrients 2017, 9, 655. [Google Scholar]
- Jordan, S.L.; Albracht-Schulte, K.; Robert-McComb, J.J. Micronutrient Deficiency in Athletes and Inefficiency of Supplementation: Is Low Energy Availability a Culprit? PharmaNutrition 2020, 14, 100229. [Google Scholar] [CrossRef]
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and Athletic Performance. J. Acad. Nutr. Diet. 2016, 116, 501–528. [Google Scholar] [CrossRef] [PubMed]
- Potgieter, S. Sport Nutrition: A Review of the Latest Guidelines for Exercise and Sport Nutrition from the American College of Sport Nutrition, the International Olympic Committee and the International Society for Sports Nutrition. S. Afr. J. Clin. Nutr. 2013, 26, 6–16. [Google Scholar] [CrossRef]
- Wardenaar, F.; Brinkmans, N.; Ceelen, I.; Van Rooij, B.; Mensink, M.; Witkamp, R.; De Vries, J. Micronutrient Intakes in 553 Dutch Elite and Sub-Elite Athletes: Prevalence of Low and High Intakes in Users and Non-Users of Nutritional Supplements. Nutrients 2017, 9, 142. [Google Scholar] [CrossRef]
- Al Mutairi, F. Hyperhomocysteinemia: Clinical Insights. J. Cent. Nerv. Syst. Dis. 2020, 12, 1179573520962230. [Google Scholar] [CrossRef]
- Rauh, M.; Verwied, S.; Knerr, I.; Dörr, H.G.; Sönnichsen, A.; Koletzko, B. Homocysteine Concentrations in a German Cohort of 500 Individuals: Reference Ranges and Determinants of Plasma Levels in Healthy Children and Their Parents. Amino Acids 2001, 20, 409–418. [Google Scholar] [CrossRef]
- Unt, E.; Zilmer, K.; Mägi, A.; Kullisaar, T.; Kairane, C.; Zilmer, M. Homocysteine Status in Former Top-Level Male Athletes: Possible Effect of Physical Activity and Physical Fitness. Scand. J. Med. Sci. Sports 2008, 18, 360–366. [Google Scholar] [CrossRef]
- Dankner, R.; Chetrit, A.; Dror, G.K.; Sela, B.A. Physical Activity Is Inversely Associated with Total Homocysteine Levels, Independent of C677T MTHFR Genotype and Plasma B Vitamins. Age 2007, 29, 219–227. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Hurtig-Wennlöf, A.; Ortega, F.B.; Patterson, E.; Nilsson, T.K.; Castillo, M.J.; Sjöström, M. Homocysteine Levels in Children and Adolescents Are Associated with the Methylenetetrahydrofolate Reductase 677C>T Genotype, but Not with Physical Activity, Fitness, or Fatness: The European Youth Heart Study. Br. J. Nutr. 2007, 97, 255–262. [Google Scholar] [CrossRef]
- Del Pozo-Cruz, J.; Rodríguez-Bies, E.; Ballesteros-Simarro, M.; Navas-Enamorado, I.; Tung, B.T.; Navas, P.; López-Lluch, G. Physical Activity Affects Plasma Coenzyme Q10 Levels Differently in Young and Old Humans. Biogerontology 2014, 15, 199–211. [Google Scholar] [CrossRef]
- Łopuszańska-Dawid, M.; Szklarska, A.; Kołodziej, H.; Lipowicz, A.; Jankowska, E.A. The relationship between: Occupational status, biological condition and androgen hormone level among Polish adult men: The Wroclaw Male Study. Aging Male 2016, 19, 231–238. [Google Scholar] [CrossRef]
- Kozieł, S.; Lopuszańska, M.; Szklarska, A.; Lipowicz, A. The Negative Health Consequences of Unemployment: The case of Poland. Econ. Hum. Biol. 2010, 8, 255–260. [Google Scholar] [CrossRef]
| Total (n = 123) | Low PA (n = 22) | Moderate PA (n = 26) | High PA (n = 75) | Statistics and p-Values | ||
|---|---|---|---|---|---|---|
| Sex | male (n = 61) | 50% | 55% | 38% | 52% | χ2(2) = 1.68, p = 0.432 |
| female (n = 62) | 50% | 45% | 62% | 48% | ||
| Age (y) | 43 (20–65) | 52 (23–62) | 45 (20–65) | 41 (20–65) | F(2, 120) = 1.68, p = 0.191 | |
| Body Weight (kg) | 71 (43–114) | 76 (53–95) | 75 (45–114) | 69 (43–114) | F(2, 120) = 4.16, p = 0.018 | |
| Height (cm) | 173 (154–190) | 172 (163–190) | 170 (157–186) | 175 (154–190) | F(2, 120) = 0.80, p = 0.452 | |
| BMI (kg/m2) | 23.6 (16.9–40.4) | 25.1 (19.6–34.1) | 24.9 (18.0–40.4) | 22.7 (16.9–36.0) | F(2, 120) = 7.63, p = 0.001 | |
| BMI Levels | <18.5 | 6% | - | 4% | 8% | χ2(6) = 12.89, p = 0.045 |
| 18.5–24.9 | 61% | 50% | 46% | 69% | ||
| 25.0–29.9 | 28% | 41% | 38% | 21% | ||
| ≥30.0 | 5% | 9% | 12% | 1% | ||
| Diet Type | mixed | 93% | 100% | 92% | 91% | χ2(2) = 2.19, p = 0.334 |
| vegetarian/vegan | 7% | - | 8% | 9% | ||
| Sedentary Time (h/week) | 42.5 ± 23.3 | 53.4 ± 25.9 | 42.4 ± 20.3 | 39.3 ± 22.8 | F(2, 120) = 3.15, p = 0.047 | |
| Homocysteine (µmol/L) | 10.57 ± 4.30 | 11.05 ± 2.84 | 11.80 ± 6.46 | 10.01 ± 3.63 | F(2, 120) = 2.59, p = 0.079 | |
| Homocysteine Levels | <10 | 52% | 36% | 46% | 59% | χ2(4) = 5.21, p = 0.266 |
| 10–15 | 39% | 55% | 38% | 35% | ||
| >15 | 9% | 9% | 15% | 7% | ||
| CoQ10 * (mg/L) | 0.82 ± 0.28 | 0.89 ± 0.34 | 0.79 ± 0.20 | 0.81 ± 0.29 | F(2, 79) = 0.35, p = 0.703 | |
| Adjusted CoQ10 * (µmol/mmol Chol) | 0.18 ± 0.06 | 0.19 ± 0.06 | 0.17 ± 0.04 | 0.18 ± 0.06 | F(2, 79) = 0.44, p = 0.644 | |
| Females (n = 62) | Statistics and p-Values | ||||
|---|---|---|---|---|---|
| Total | Low PA | Moderate PA | High PA | ||
| Potassium (mg/L) | 1687 ± 234 | 1684 ± 180 | 1751 ± 134 | 1660 ± 277 | F(2, 59) = 0.85, p = 0.433 |
| Calcium (mg/L) | 56.3 ± 4.1 | 57.7 ± 7.2 | 55.8 ± 3.4 | 56.1 ± 3.2 | F(2, 59) = 0.71, p = 0.497 |
| Magnesium (mg/L) | 32.8 ± 3.0 | 33.0 ± 2.7 | 33.8 ± 2.4 | 32.3 ± 3.3 | F(2, 59) = 1.89, p = 0.161 |
| Copper (mg/L) | 0.93 ± 0.20 | 0.97 ± 0.16 | 1.01 ± 0.28 | 0.89 ± 0.15 | F(2, 59) = 1.24, p = 0.297 |
| Iron (mg/L) | 482 ± 43 | 473 ± 63 | 488 ± 37 | 481 ± 41 | F(2, 59) = 0.16, p = 0.855 |
| Zinc (mg/L) | 5.80 ± 0.69 | 5.97 ± 0.56 | 5.72 ± 0.91 | 5.78 ± 0.63 | F(2, 59) = 0.25, p = 0.778 |
| Selenium (µg/L) | 138 ± 42 | 131 ± 19 | 145 ± 66 | 137 ± 32 | F(2, 59) = 0.21, p = 0.813 |
| Manganese (µg/L) | 10.33 ± 3.70 | 11.39 ± 5.61 | 9.98 ± 3.12 | 10.19 ± 3.34 | F(2, 59) = 0.22, p = 0.806 |
| Molybdenum (µg/L) | 1.12 ± 0.83 | 1.15 ± 0.69 | 0.79 ± 0.31 | 1.25 ± 0.98 | F(2, 59) = 2.93, p = 0.061 |
| Vitamin B6 (µg/L) | 38.2 ± 30.8 | 33.4 ± 16.5 | 29.9 ± 12.1 | 43.3 ± 38.1 | F(2, 59) = 1.55, p = 0.221 |
| Vitamin B9 (ng/mL) | 8.88 ± 5.70 | 8.74 ± 5.66 | 5.83 ± 3.87 | 10.23 ± 5.98 | F(2, 57) = 2.98, p = 0.059 |
| Vitamin B12 (pg/mL) | 579 ± 877 | 438 ± 90 | 436 ± 97 | 684 ± 1150 | F(2, 58) = 0.45, p = 0.641 |
| Vitamin D (nmol/L) | 89.9 ± 37.2 | 63.1 ± 24.3 | 79.9 ± 30.9 | 101.9 ± 38.1 | F(2, 59) = 7.95, p = 0.001 |
| Males (n = 61) | Statistics and p-Values | ||||
|---|---|---|---|---|---|
| Total | Low PA | Moderate PA | High PA | ||
| Potassium (mg/L) | 1811 ± 113 | 1827 ± 144 | 1811 ± 136 | 1806 ± 98 | F(2, 58) = 0.01, p = 0.994 |
| Calcium (mg/L) | 53.5 ± 3.4 | 54.5 ± 2.9 | 52.3 ± 2.8 | 53.4 ± 3.7 | F(2, 58) = 1.97, p = 0.148 |
| Magnesium (mg/L) | 34.9 ± 2.8 | 35.8 ± 3.9 | 35.2 ± 2.5 | 34.5 ± 2.4 | F(2, 58) = 0.68, p = 0.511 |
| Copper (mg/L) | 0.79 ± 0.09 | 0.78 ± 0.06 | 0.79 ± 0.05 | 0.79 ± 0.10 | F(2, 58) = 0.13, p = 0.880 |
| Iron (mg/L) | 543 ± 34 | 536 ± 44 | 546 ± 41 | 544 ± 28 | F(2, 58) = 0.38, p = 0.685 |
| Zinc (mg/L) | 6.43 ± 0.68 | 6.52 ± 0.52 | 6.45 ± 0.81 | 6.41 ± 0.70 | F(2, 58) = 0.11, p = 0.894 |
| Selenium (µg/L) | 136 ± 35 | 121 ± 12 | 134 ± 23 | 142 ± 41 | F(2, 58) = 3.39, p = 0.040 |
| Manganese (µg/L) | 8.29 ± 2.13 | 8.14 ± 2.10 | 8.83 ± 3.27 | 8.20 ± 1.81 | F(2, 58) = 0.07, p = 0.933 |
| Molybdenum (µg/L) | 1.60 ± 4.23 | 0.93 ± 0.42 | 4.36 ± 10.36 | 1.10 ± 0.61 | F(2, 58) = 0.12, p = 0.886 |
| Vitamin B6 (µg/L) | 36.5 ± 22.3 | 31.4 ± 8.8 | 38.5 ± 17.9 | 37.6 ± 26.1 | F(2, 58) = 0.38, p = 0.684 |
| Vitamin B9 (ng/mL) | 10.02 ± 4.92 | 10.22 ± 6.03 | 10.90 ± 5.05 | 9.73 ± 4.62 | F(2, 58) = 0.16, p = 0.851 |
| Vitamin B12 (pg/mL) | 491 ± 247 | 381 ± 74 | 452 ± 127 | 535 ± 292 | F(2, 58) = 3.20, p = 0.048 |
| Vitamin D (nmol/L) | 99.8 ± 49.9 | 89.7 ± 51.2 | 84.1 ± 44.4 | 107.0 ± 50.5 | F(2, 58) = 1.27, p = 0.290 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schauer, M.; Motevalli, M.; Tanous, D.; Mair, S.; Burtscher, M.; Wirnitzer, K. The Association of Physical Activity Level with Micronutrient and Health Status of Austrian Bank Employees. Nutrients 2023, 15, 4884. https://doi.org/10.3390/nu15234884
Schauer M, Motevalli M, Tanous D, Mair S, Burtscher M, Wirnitzer K. The Association of Physical Activity Level with Micronutrient and Health Status of Austrian Bank Employees. Nutrients. 2023; 15(23):4884. https://doi.org/10.3390/nu15234884
Chicago/Turabian StyleSchauer, Markus, Mohamad Motevalli, Derrick Tanous, Susanne Mair, Martin Burtscher, and Katharina Wirnitzer. 2023. "The Association of Physical Activity Level with Micronutrient and Health Status of Austrian Bank Employees" Nutrients 15, no. 23: 4884. https://doi.org/10.3390/nu15234884
APA StyleSchauer, M., Motevalli, M., Tanous, D., Mair, S., Burtscher, M., & Wirnitzer, K. (2023). The Association of Physical Activity Level with Micronutrient and Health Status of Austrian Bank Employees. Nutrients, 15(23), 4884. https://doi.org/10.3390/nu15234884







