Association of Eicosapentaenoic and Docosahexaenoic Acid Intake with Low Birth Weight in the Second Trimester: The Japan Pregnancy Eating and Activity Cohort Study
Abstract
1. Introduction
2. Materials and Methods
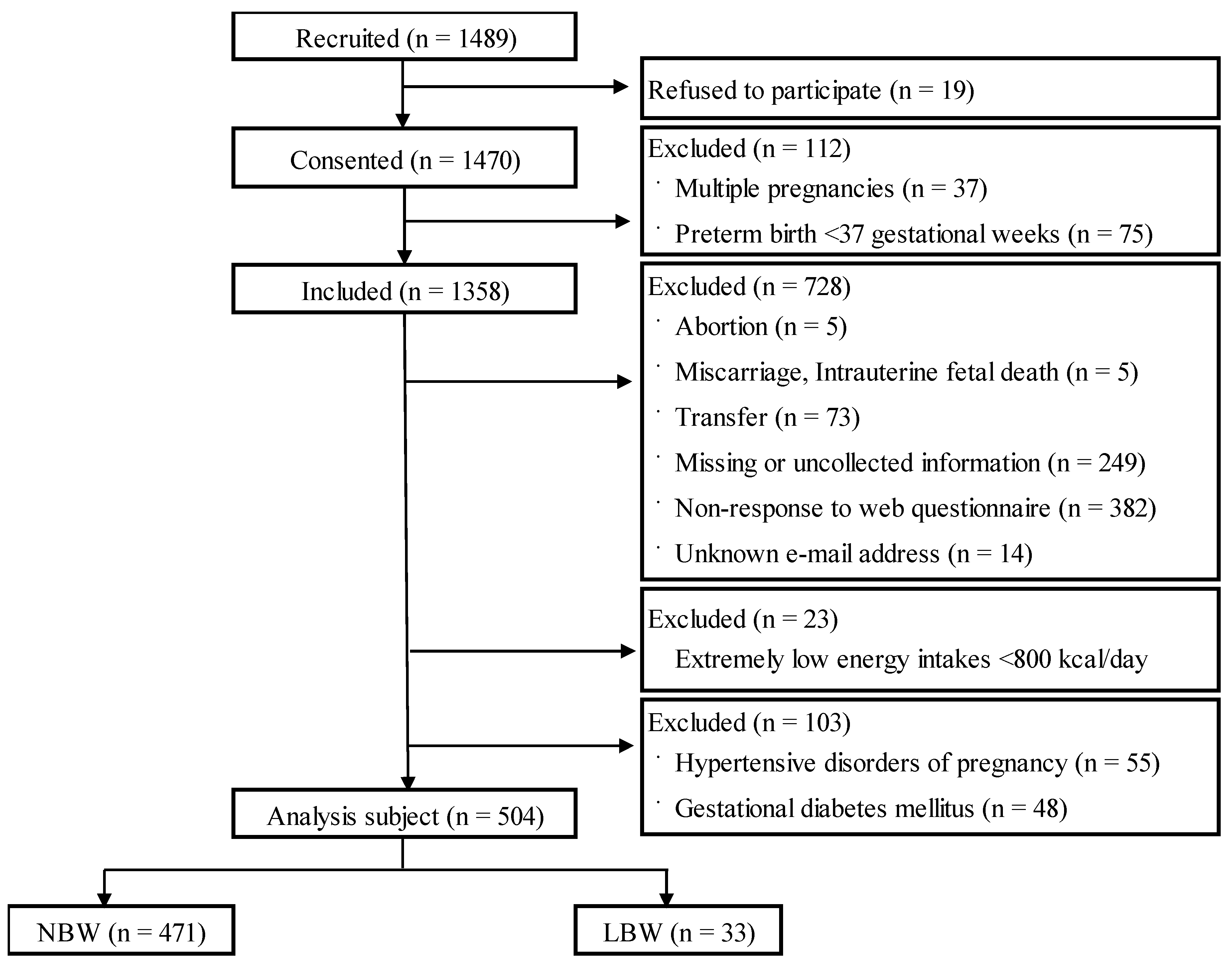
2.1. Study Design and Participants
2.2. Survey Period and Data Collection Methods
2.3. Dietary Intake
2.4. Supplement Use
2.5. Participant Characteristics
2.6. Statistical Analysis
3. Results
3.1. Participants
3.2. Participant Characteristics
3.3. Intake of Nutrients
3.4. Total EPA and DHA Intake and LBW
4. Discussion
4.1. Participants
4.2. Transfer of Fatty Acids to the Fetus during Pregnancy
4.3. Nutrients and EPA and DHA Intake during Pregnancy
4.4. Role of Medical Professionals
4.5. Limitations and Issues
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Ministry of Health and Welfare of Japan. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/tokusyu/syussyo07/dl/02.pdf (accessed on 9 November 2022).
- Japan Committee for UNICEF. Available online: https://www.unicef.or.jp/sowc/data.html (accessed on 9 November 2022).
- Report on Perinatal Maternal and Child Medical Center Network Database Analysis. Available online: https://plaza.umin.ac.jp/nrndata/syukei.htm (accessed on 9 January 2023).
- Fukuoka, H.; Sata, F. Molecular mechanism of developmental origins of health and disease (DOHaD). Jpn. J. Hyg. 2016, 71, 185–187. [Google Scholar] [CrossRef] [PubMed]
- Nishihama, Y.; Nakayama, S.F.; Tabuchi, T. Japan Environment and Children’s Study Group Population attributable fraction of risk factors for low birth weight in the Japan environment and children’s study. Environ. Int. 2022, 170, 107560. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishnan, U. Nutrition and low birth weight: From research to practice. Am. J. Clin. Nutr. 2004, 79, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Rump, P.; Mensink, R.P.; Kester, A.D.; Hornstra, G. Essential fatty acid composition of plasma phospholipids and birth weight: A study in term neonates. Am. J. Clin. Nutr. 2001, 73, 797–806. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Meher, A.; Randhir, K.; Mehendale, S.; Wagh, G.; Joshi, S. Maternal fatty acids and their association with birth outcome: A prospective study. PLoS ONE 2016, 11, e0147359. [Google Scholar] [CrossRef] [PubMed]
- Innis, S.M. Perinatal biochemistry and physiology of long-chain polyunsaturated fatty acids. J. Pediatr. 2003, 143, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Begg, D.P.; Puskás, L.G.; Kitajka, K.; Ménesi, D.; Allen, A.M.; Li, D.; Mathai, M.L.; Shi, J.R.; Sinclair, A.J.; Weisinger, R.S. Hypothalamic gene expression in ω-3 PUFA-deficient male rats before, and following, development of hypertension. Hypertens. Res. 2012, 35, 381–387. [Google Scholar] [CrossRef] [PubMed]
- The Ministry of Health and Welfare of Japan. Available online: https://www.mhlw.go.jp/topics/bukyoku/iyaku/syoku-anzen/suigin/ (accessed on 9 November 2022).
- Muthayya, S.; Dwarkanath, P.; Thomas, T.; Ramprakash, S.; Mehra, R.; Mhaskar, A.; Mhaskar, R.; Thomas, A.; Bhat, S.; Vaz, M.; et al. The effect of fish and ω-3 LCPUFA intake on low birth weight in Indian pregnant women. Eur. J. Clin. Nutr. 2009, 63, 340–346. [Google Scholar] [CrossRef] [PubMed]
- van Eijsden, M.; Hornstra, G.; van der Wal, M.F.; Vrijkotte, T.G.; Bonsel, G.J. Maternal n-3, n-6, and trans fatty acid profile early in pregnancy and term birth weight: A prospective cohort study. Am. J. Clin. Nutr. 2008, 87, 887–895. [Google Scholar] [CrossRef] [PubMed]
- J-PEACH Study: The Japan, Pregnancy, Eating, and Activity, Cohort Study. Available online: https://j-birthcohorts.net/cohorts/jpeach-study/ (accessed on 9 November 2022).
- Kobayashi, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011, 14, 1200–1211. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, M.; Haruna, M.; Matsuzaki, M.; Murayama, R.; Sasaki, S. The biomarker-based validity of a brief-type diet history questionnaire for estimating eicosapentaenoic acid and docosahexaenoic acid intakes in pregnant Japanese women. Asia Pac. J. Clin. Nutr. 2015, 24, 316–322. [Google Scholar] [CrossRef] [PubMed]
- The Ministry of Health and Welfare of Japan National Nutrition and Health Survey. Available online: https://www.mhlw.go.jp/content/000711007.pdf (accessed on 23 June 2023).
- Census of Japan. Type of Last School Graduated. Available online: https://www.e-stat.go.jp/dbview?sid=0003450674 (accessed on 25 June 2023).
- National Survey of Living Standards. Available online: https://www.e-stat.go.jp/dbview?sid=0004003181 (accessed on 25 June 2023).
- Herrera, E.; Amusquivar, E.; López-Soldado, I.; Ortega, H. Maternal lipid metabolism and placental lipid transfer. Horm. Res. 2006, 65 (Suppl. 3), 59–64. [Google Scholar] [CrossRef] [PubMed]
- Okada, T. Developmental lipidology of the fetus and newborn. JOCS 2011, 11, 365–371. [Google Scholar] [CrossRef]
- The Ministry of Health and Welfare of Japan. Available online: https://www.mhlw.go.jp/content/10904750/000586553.pdf (accessed on 9 November 2022).
- Murakami, K.; Sasaki, S.; Takahashi, Y.; Uenishi, K.; Yamasaki, M.; Hayabuchi, H.; Goda, T.; Oka, J.; Baba, K.; Ohki, K.; et al. Misreporting of dietary energy, protein, potassium and sodium in relation to body mass index in young Japanese women. Eur. J. Clin. Nutr. 2008, 62, 111–118. [Google Scholar] [CrossRef]
- The Ministry of Health and Welfare of Japan. Available online: https://www.mhlw.go.jp/content/000788598.pdf (accessed on 13 November 2022).
- Florida Department of Health: WIC Program. Available online: https://www.floridahealth.gov/programs-and-services/wic/_documents/how-wic-works.pdf (accessed on 13 November 2022).
- Hamad, R.; Collin, D.F.; Baer, R.J.; Jelliffe-Pawlowski, L.L. Association of revised WIC food package with perinatal and birth outcomes: A quasi-experimental study. JAMA Pediatr. 2019, 173, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Miura, K.; Takamori, A.; Hamazaki, K.; Tsuchida, A.; Tanaka, T.; Origasa, H.; Inadera, H.; Japan Environment and Children’s Study Group. Dietary patterns during pregnancy and health-related quality of life: The Japan Environment and Children’s Study. PLoS ONE 2020, 15, e0236330. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, T.; Obara, T.; Yonezawa, Y.; Takahashi, I.; Ishikuro, M.; Murakami, K.; Ueno, F.; Noda, A.; Onuma, T.; Iwama, N.; et al. Dietary patterns before and during pregnancy and small for gestational age in Japan: A prospective birth cohort study. Nutr. J. 2022, 21, 57. [Google Scholar] [CrossRef] [PubMed]
- Gete, D.G.; Waller, M.; Mishra, G.D. Effects of maternal diets on preterm birth and low birth weight: A systematic review. Br. J. Nutr. 2020, 123, 446–461. [Google Scholar] [CrossRef] [PubMed]
- Kibret, K.T.; Chojenta, C.; Gresham, E.; Tegegne, T.K.; Loxton, D. Maternal dietary patterns and risk of adverse pregnancy (hypertensive disorders of pregnancy and gestational diabetes mellitus) and birth (preterm birth and low birth weight) outcomes: A systematic review and meta-analysis. Public. Health Nutr. 2018, 22, 506–520. [Google Scholar] [CrossRef] [PubMed]
| Parameters | Mean ± SD | n (%) | |
|---|---|---|---|
| Age at delivery (years) | 34.2±4.5 | ||
| Prepregnancy BMI (kg/m2) | 21.3±3.3 | ||
| Maternal weight gain during pregnancy (kg) | 9.9±3.9 | ||
| Number of gestational weeks (week) | 38.9±1.1 | ||
| Parity | Primipara | 247 (49.0) | |
| Multipara | 257 (51.0) | ||
| Sex of the children | Boys | 237 (47.0) | |
| Girls | 267 (53.0) | ||
| Birth weight (g) | All participants | 3068.6±370.5 | |
| Boys | 3145.8±370.9 | ||
| Girls | 3000.1±356.4 | ||
| LBW (g) | All participants | 2395.3±418.3 | 33 (6.5) |
| Boys | 2412.3±72.4 | 8 (1.6) | |
| Girls | 2389.9±114.0 | 25 (5.0) | |
| Family income (JPY per year) | |||
| <3 million | 18 (3.6) | ||
| 3–<5 million | 105 (20.8) | ||
| 5–<7 million | 107 (21.2) | ||
| 7–<9 million | 89 (17.7) | ||
| ≥9 million | 185 (36.7) | ||
| Education | Junior high or high school | 46 (9.1) | |
| Junior/technical college | 121 (24.0) | ||
| University/graduate school | 337 (66.9) | ||
| Working during the second trimester | Yes | 326 (64.7) | |
| No | 178 (35.3) | ||
| Drink before pregnancy | No drink or <1 time/a week | 380 (75.4) | |
| 2–3 times/a week | 60 (11.9) | ||
| 4–5 times/a week | 30 (6.0) | ||
| ≥6 times/a week | 34 (6.7) | ||
| Smoking | Never | 449 (89.1) | |
| Stopped before this pregnancy | 43 (8.5) | ||
| Stopped during this pregnancy | 10 (2.0) | ||
| Smoked during pregnancy | 2 (0.4) | ||
| Frequency of EPA and DHA supplement intake during the second trimester | |||
| ≥5/a week | 44 (8.7) | ||
| <4/week | 16 (3.2) | ||
| No | 444 (88.1) | ||
| All Participants (n = 504) | Boys (n = 286) | Girls (n = 267) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| NBW (n = 471) | LBW (n = 33) | NBW (n = 229) | LBW (n = 8) | NBW (n = 242) | LBW (n = 25) | ||||
| Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | ||||
| Energy (kcal) | 1545.8 ± 407.4 | 1516.1 ± 524.7 | 0.70 | 1573.6 ± 410.2 | 1408.4 ± 374.2 | 0.26 | 1519.5 ± 403.8 | 1550.6 ± 566.7 | 0.73 |
| Protein (g/1000 kcal) | 57.5 ± 18.4 | 55.6 ± 23.6 | 0.58 | 57.6 ± 18.4 | 49.7 ± 17.2 | 0.23 | 57.4 ± 18.4 | 57.5 ± 25.3 | 0.97 |
| Fat (g/1000 kcal) | 50.1 ± 15.1 | 48.3 ± 17.5 | 0.52 | 51.0 ± 15.2 | 46.1 ± 10.1 | 0.37 | 49.3 ± 14.9 | 49.1 ± 19.4 | 0.95 |
| Carbohydrate (g/1000 kcal) | 212.3 ± 63.1 | 208.2 ± 65.9 | 0.72 | 217.0 ± 65.3 | 196.1 ± 57.0 | 0.37 | 207.9 ± 60.8 | 212.1 ± 69.1 | 0.75 |
| EPA + DHA (mg/1000 kcal) | 297.2 ± 185.4 | 240.7 ± 165.7 | 0.10 | 289.2 ± 192.9 | 216.9 ± 69.1 | 0.29 | 304.7 ± 178.2 | 248.3 ± 187.0 | 0.15 |
| EPA (mg/1000 kcal) | 104.9 ± 74.3 | 83.2 ± 66.52 | 0.10 | 101.5 ± 77.4 | 75.4 ± 29.8 | 0.34 | 108.0 ± 71.4 | 85.6 ± 74.5 | 0.14 |
| DHA (mg/1000 kcal) | 192.2 ± 111.6 | 157.5 ± 100.0 | 0.08 | 187.7 ± 116.0 | 141.4 ± 40.1 | 0.26 | 196.7 ± 107.4 | 162.7 ± 112.9 | 0.14 |
| Classification | All Participants (n = 504) | Boys (n = 237) | Girls (n = 267) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| NBW (n = 471) | LBW (n = 33) | NBW (n = 229) | LBW (n = 8) | NBW (n = 242) | LBW (n = 25) | ||||
| EPA + DHA | n (%) | n (%) | p | n (%) | n (%) | p | n (%) | n (%) | p |
| Low-intake group † | 114 (90.5) | 12 (9.5) | 0.04 * | 58 (95.1) | 3 (4.9) | 0.27 | 56 (86.2) | 9 (13.8) | 0.35 |
| Medium-intake group † | 236 (93.7) | 16 (6.4) | 115 (95.8) | 5 (4.2) | 121 (91.7) | 11 (8.3) | |||
| High-intake group † | 121 (96.0) | 5 (4.0) | 56 (100.0) | 0 (0.0) | 65 (92.9) | 5 (7.1) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshimura, M.; Fujita, M.; Shibata, A.; Ohori, R.; Aoyama, S.; Yonezawa, K.; Sato, Y.; Sasaki, S.; Matsuzaki, M.; Suetsugu, Y.; et al. Association of Eicosapentaenoic and Docosahexaenoic Acid Intake with Low Birth Weight in the Second Trimester: The Japan Pregnancy Eating and Activity Cohort Study. Nutrients 2023, 15, 4831. https://doi.org/10.3390/nu15224831
Yoshimura M, Fujita M, Shibata A, Ohori R, Aoyama S, Yonezawa K, Sato Y, Sasaki S, Matsuzaki M, Suetsugu Y, et al. Association of Eicosapentaenoic and Docosahexaenoic Acid Intake with Low Birth Weight in the Second Trimester: The Japan Pregnancy Eating and Activity Cohort Study. Nutrients. 2023; 15(22):4831. https://doi.org/10.3390/nu15224831
Chicago/Turabian StyleYoshimura, Momoka, Megumi Fujita, Ai Shibata, Riko Ohori, Satoko Aoyama, Kaori Yonezawa, Yoko Sato, Satoshi Sasaki, Masayo Matsuzaki, Yoshiko Suetsugu, and et al. 2023. "Association of Eicosapentaenoic and Docosahexaenoic Acid Intake with Low Birth Weight in the Second Trimester: The Japan Pregnancy Eating and Activity Cohort Study" Nutrients 15, no. 22: 4831. https://doi.org/10.3390/nu15224831
APA StyleYoshimura, M., Fujita, M., Shibata, A., Ohori, R., Aoyama, S., Yonezawa, K., Sato, Y., Sasaki, S., Matsuzaki, M., Suetsugu, Y., & Haruna, M. (2023). Association of Eicosapentaenoic and Docosahexaenoic Acid Intake with Low Birth Weight in the Second Trimester: The Japan Pregnancy Eating and Activity Cohort Study. Nutrients, 15(22), 4831. https://doi.org/10.3390/nu15224831






