A Comparative Evaluation of the Caloric Intake and Economic Efficiency of Two Types of Homogenized Diets in a Hospital Setting
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Objectives of the Study
2.3. Inclusion and Exclusion Criteria
2.4. Data Collection
- (1)
- Hospital admission: age, sex, body mass index (BMI), plasma albumin level, underlying disease, comorbidities (Type I-II diabetes mellitus, cardiopathy, chronic kidney disease stage I–IV, chronic obstructive pulmonary disease, cancer).
- (2)
- Within 72 h of hospitalization or of the first prescription of the homogenized diet: evaluation of fluid and food intake. This survey was carried out by the health workers of the wards and recorded in the electronic medical record; The daily millilitres of liquids consumed, the daily kilocalories, and the percentage of food consumed were considered. This assessment is carried out as a standard hospital procedure in order to identify possible alterations in patients’ water or food intake. For the purposes of this study, three days of evaluation were considered in order to make the collected data homogeneous in consideration of the different periods of hospitalization, which differed in the sample considered.
- (3)
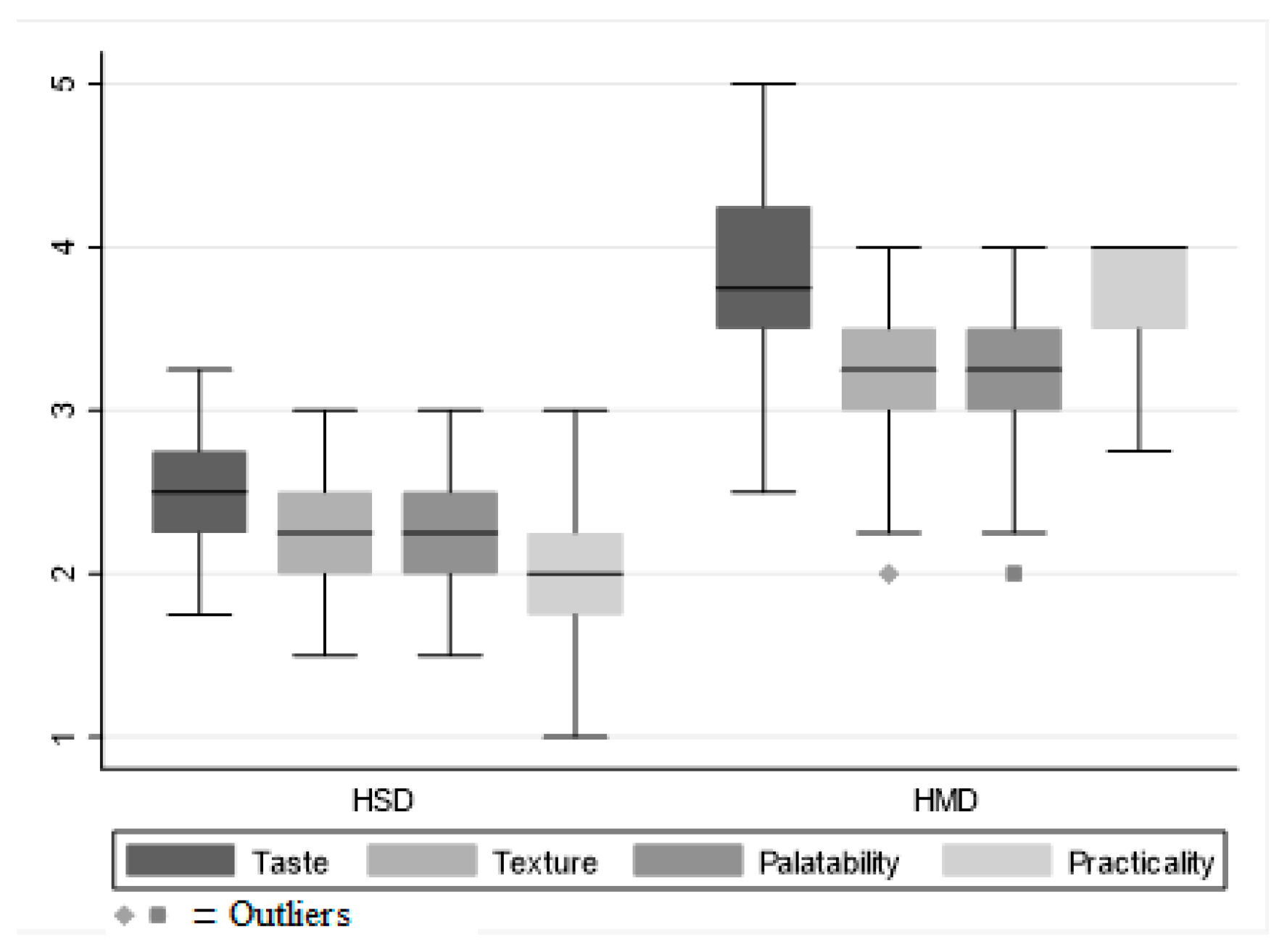
- After measuring water and food intake, two external evaluators (academic staff) carried out an evaluation of the rheological characteristics of the foods consumed and the palatability of the homogenized diet taken using an evaluation scale that considered variables such as taste, texture, palatability, practicality, and ease of use. Each variable was assigned a score according to a 5-point Likert scale (1 = insufficient, 2 = sufficient, 3 = good, 4 = excellent, 5 = exceptional). Both evaluators were unaware of the diet administered by the hospital catering service and had previously followed specific training conducted by a dietitian and a nutritionist in order to interview patients in a standardized way. Additionally, each assessment form was supported by a dedicated legend to interpret patient feedback and assign an assessment score. Data collection for this study was performed retrospectively and managed by an independent data manager, receiving data that was anonymized and devoid of any identifying information about either the patient or diet. This approach further ensured the integrity and accuracy of the collected data. The data obtained was then used to address the primary and secondary objectives. As this study is purely observational and retrospective, follow-up periods were not included.
2.5. Study Procedures
2.6. Statistical Analysis
2.7. Acronyms
3. Results
3.1. Demographic and Clinical Characteristics of the Sample
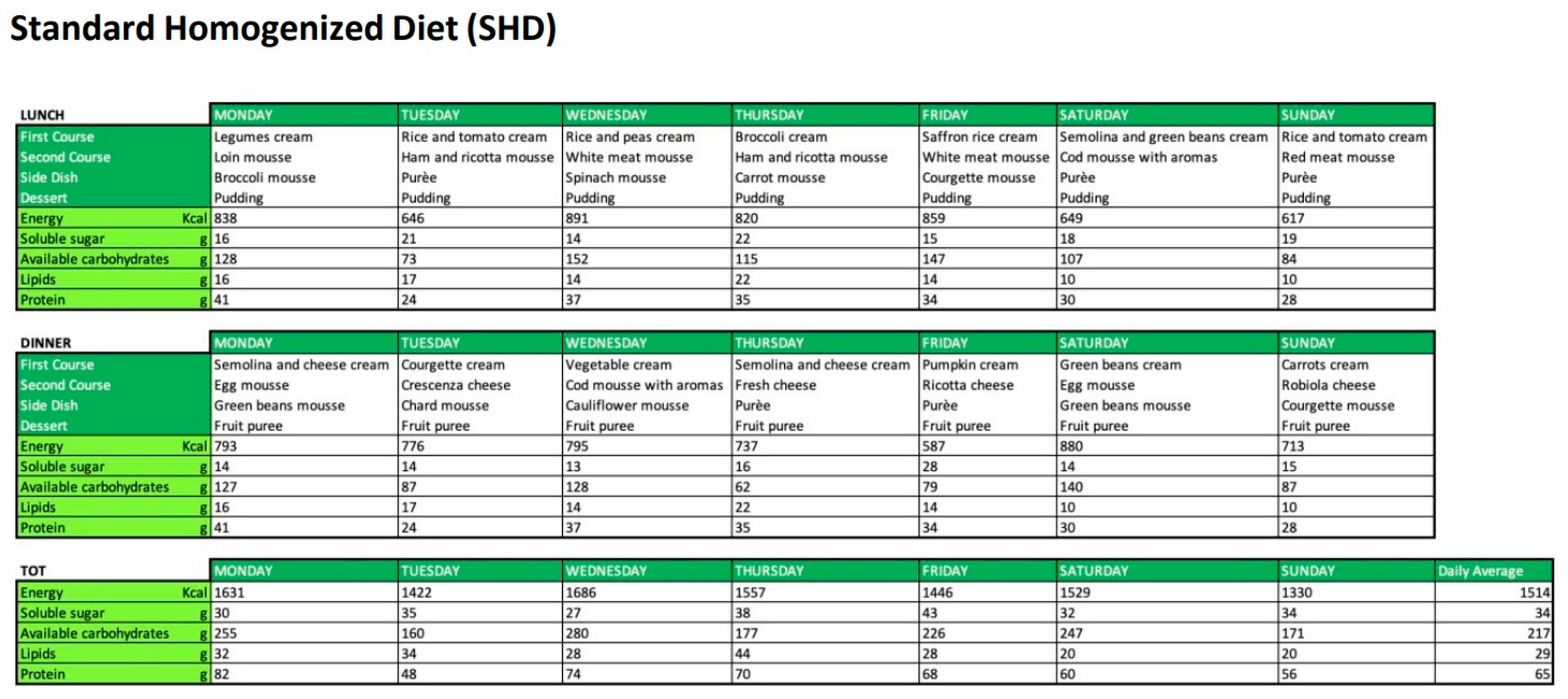
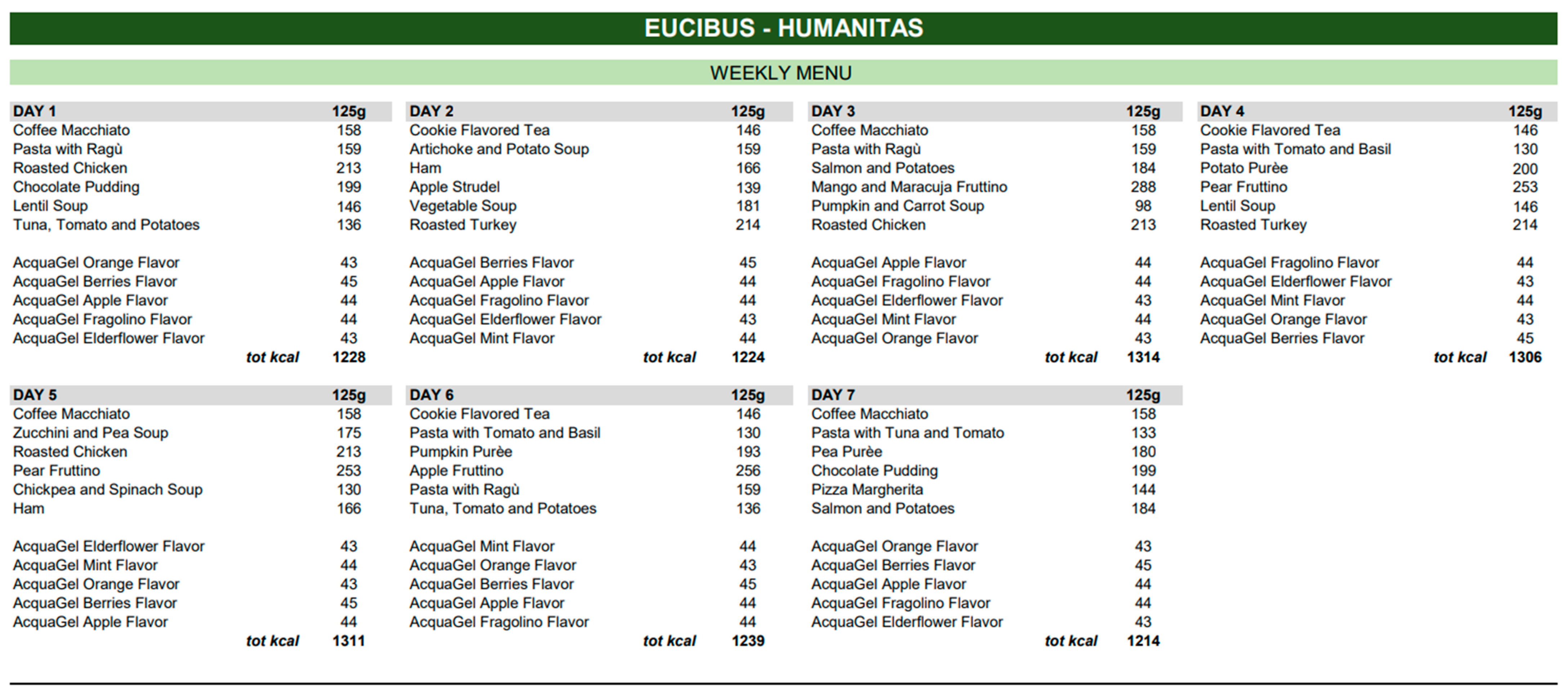
3.2. Dietary Intake of the Homogenized Diets
3.3. Food Intake and Clinical Variables
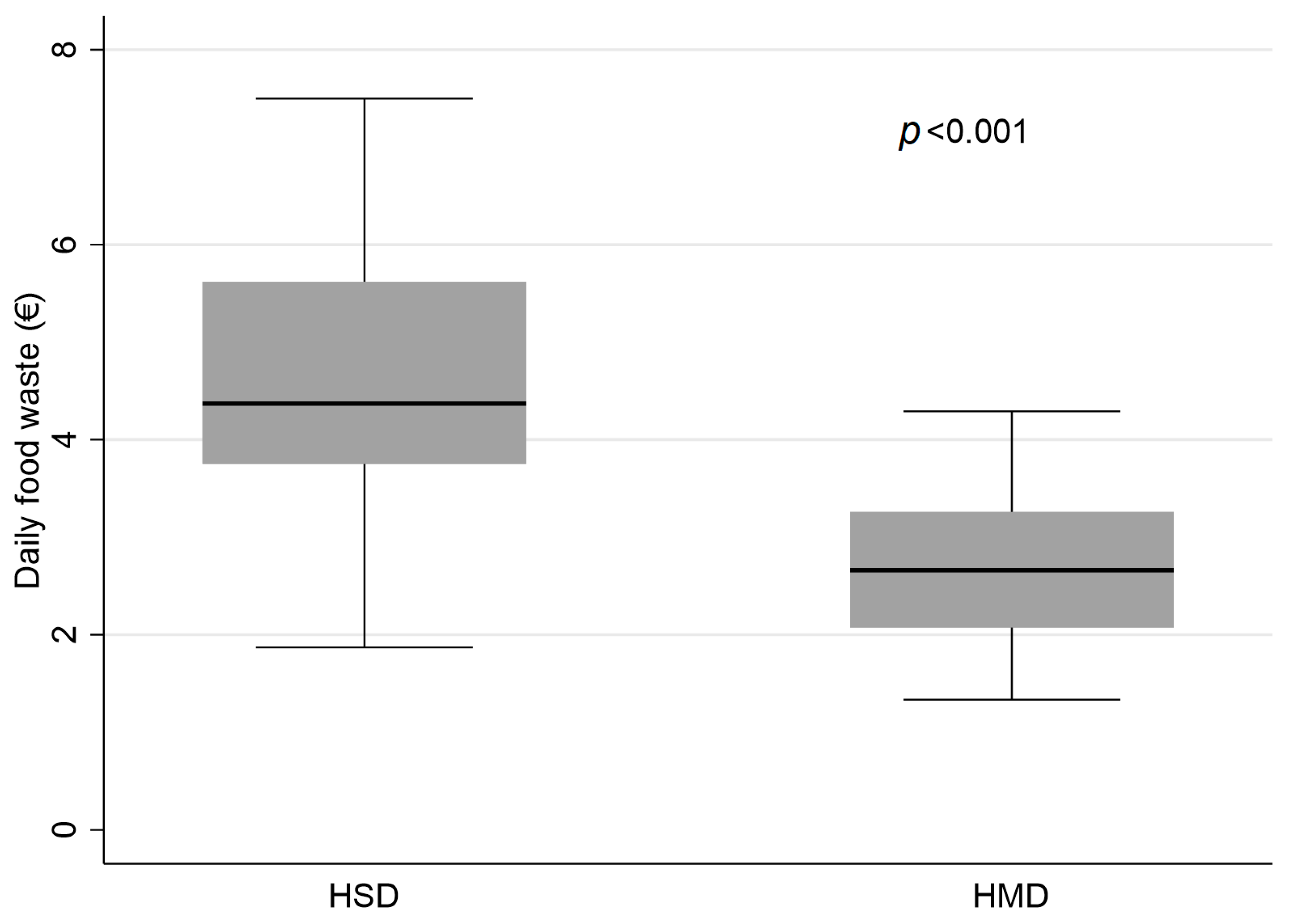
3.4. Economic Impact of Diets
4. Discussion
4.1. Study Limitations
4.2. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Sire, A.; Ferrillo, M.; Lippi, L.; Agostini, F.; de Sire, R.; Ferrara, P.E.; Raguso, G.; Riso, S.; Roccuzzo, A.; Ronconi, G.; et al. Sarcopenic Dysphagia, Malnutrition, and Oral Frailty in Elderly: A Comprehensive Review. Nutrients 2022, 14, 982. [Google Scholar] [CrossRef]
- Fleurke, M.; Voskuil, D.W.; Beneken Genaamd Kolmer, D.M. The role of the dietitian in the management of malnutrition in the elderly: A systematic review of current practices. Nutr. Diet. 2020, 77, 60–75. [Google Scholar] [CrossRef]
- Stefano, M.; Andrea, B.; Daniela, C.; Emanuela, M.; Lorena, P.; Daniela, D.; Sökeland, F.; Azzolini, E.; Mazzoleni, B. Malnutrition risk as a negative prognostic factor in COVID-19 patients. Clin. Nutr. ESPEN 2021, 45, 369–373. [Google Scholar] [CrossRef]
- Norman, K.; Haß, U.; Pirlich, M. Malnutrition in Older Adults-Recent Advances and Remaining Challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef]
- Serón-Arbeloa, C.; Labarta-Monzón, L.; Puzo-Foncillas, J.; Mallor-Bonet, T.; Lafita-López, A.; Bueno-Vidales, N.; Montoro-Huguet, M. Malnutrition Screening and Assessment. Nutrients 2022, 14, 2392. [Google Scholar] [CrossRef]
- Bomze, L.; Dehom, S.; Lao, W.P.; Thompson, J.; Lee, N.; Cragoe, A.; Luceno, C.; Crawley, B. Comorbid Dysphagia and Malnutrition in Elderly Hospitalized Patients. Laryngoscope 2021, 131, 2441–2447. [Google Scholar] [CrossRef] [PubMed]
- Cochet, C.; Belloni, G.; Buondonno, I.; Chiara, F.; D’Amelio, P. The Role of Nutrition in the Treatment of Sarcopenia in Old Patients: From Restoration of Mitochondrial Activity to Improvement of Muscle Performance, a Systematic Review. Nutrients 2023, 15, 3703. [Google Scholar] [CrossRef] [PubMed]
- Dziewas, R.; Beck, A.M.; Clavé, P.; Hamdy, S.; Heppner, H.J.; Langmore, S.; Leischker, A.H.; Martino, R.; Pluschinski, P.; Rösler, A.; et al. Oropharyngeal dysphagia in older people: From pathophysiology to appropriate intervention: A review and synthesis of an international expert meeting. Aging Interv. Clin. 2016, 11, 189–208. [Google Scholar] [CrossRef]
- Mancin, S.; Sguanci, M.; Reggiani, F.; Morenghi, E.; Piredda, M.; De Marinis, M.G. Dysphagia screening post-stroke: Systematic review. BMJ Support Palliat Care 2023, spcare-2022-004144. [Google Scholar] [CrossRef] [PubMed]
- Thiyagalingam, S.; Kulinski, A.E.; Thorsteinsdottir, B.; Shindelar, K.L.; Takahashi, P.Y. Dysphagia in Older Adults. Mayo Clin. Proc. 2021, 96, 488–497. [Google Scholar] [CrossRef]
- Feng, H.Y.; Zhang, P.P.; Wang, X.W. Presbyphagia: Dysphagia in the elderly. World J. Clin. Cases 2023, 11, 2363–2373. [Google Scholar] [CrossRef]
- Bellanti, F.; Lo Buglio, A.; Quiete, S.; Vendemiale, G. Malnutrition in Hospitalized Old Patients: Screening and Diagnosis, Clinical Outcomes, and Management. Nutrients 2022, 14, 910. [Google Scholar] [CrossRef]
- Garand, K.L.; Beall, J.; Hill, E.G.; Davidson, K.; Blair, J.; Pearson, W., Jr.; Martin-Harris, B. Effects of Presbyphagia on Oropharyngeal Swallowing Observed during Modified Barium Swallow Studies. J. Nutr. Health Aging 2022, 26, 973–980. [Google Scholar] [CrossRef]
- Sieber, C.C. Malnutrition and sarcopenia. Aging Clin. Exp. Res. 2019, 31, 793–798. [Google Scholar] [CrossRef]
- Zelig, R.; Goldstein, S.; Touger-Decker, R.; Firestone, E.; Golden, A.; Johnson, Z.; Kaseta, A.; Sackey, J.; Tomesko, J.; Parrott, J.S. Tooth Loss and Nutritional Status in Older Adults: A Systematic Review and Meta-analysis. JDR Clin. Trans. Res. 2022, 7, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Yin, J.; Wang, J.; Xu, X. Food for the elderly based on sensory perception: A review. Curr. Res. Food Sci. 2022, 5, 1550–1558. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.S.; Miles, A.; Braakhuis, A. Nutritional Intake and Meal Composition of Patients Consuming Texture Modified Diets and Thickened Fluids: A Systematic Review and Meta-Analysis. Healthcare 2020, 8, 579. [Google Scholar] [CrossRef]
- Wu, X.S.; Miles, A.; Braakhuis, A.J. Texture-Modified Diets, Nutritional Status and Mealtime Satisfaction: A Systematic Review. Healthcare 2021, 9, 624. [Google Scholar] [CrossRef]
- Thibault, R.; Abbasoglu, O.; Ioannou, E.; Meija, L.; Ottens-Oussoren, K.; Pichard, C.; Rothenberg, E.; Rubin, D.; Siljamäki-Ojansuu, U.; Vaillant, M.F.; et al. ESPEN guideline on hospital nutrition. Clin. Nutr. 2021, 40, 5684–5709. [Google Scholar] [CrossRef]
- Mancin, S.; Sguanci, M.; Cattani, D.; Soekeland, F.; Axiak, G.; Mazzoleni, B.; De Marinis, M.G.; Piredda, M. Nutritional knowledge of nursing students: A systematic literature review. Nurse Educ. Today 2023, 126, 105826. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [PubMed]
- Ministero della Salute. Linee di Indirizzo Nazionale per la Ristorazione Ospedaliera, Assistenziale e Scolastica. 2021. Available online: https://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?lingua=italiano&id=3141 (accessed on 3 July 2023).
| Characteristics | HSD (n = 55) | HMD (n = 31) | p Value |
|---|---|---|---|
| Age (Years) | 82.2 ± 9.8 | 81.5 ± 11.6 | 0.991 |
| Sex (M) | 28 (50.91%) | 12 (41.38%) | 0.406 |
| BMI (Kg/m2) | 22.2 ± 3.5 | 23.4 ± 5.4 | 0.406 |
| MUST | 0.91 ± 1.27 | 0.94 ± 1.01 | 0.621 |
| Albumin (g/L) | 29.9 ± 6.2 | 29.0 ± 4.2 | 0.571 |
| Disease | |||
| Cancer | 8 (14.55%) | 1 (3.33%) | 0.108 |
| UTI | 5 (9.09%) | 3 (10.00%) | 0.891 |
| Pneumonia | 15 (27.27%) | 8 (26.67%) | 0.952 |
| Sepsis | 13 (23.64%) | 9 (30.00%) | 0.522 |
| Neurodegenerative pathologies | 21 (38.18%) | 10 (33.33%) | 0.657 |
| Comorbidity | 34 (61.82%) | 20 (66.67%) | 0.657 |
| COPD | 6 (17.65%) | 4 (20.00%) | |
| Cardiopathy | 14 (41.18%) | 8 (40.00%) | |
| Diabetes | 10 (29.41%) | 7 (35.00%) | |
| CKD (stages I–IV) | 9 (26.47%) | 7 (35.00%) | |
| Comorbidity (n) | 1 (1–3) | 1 (1–3) | 0.714 |
| Dysphagia | 26 (47.27%) | 10 (37.04%) | 0.479 |
| Characteristics | HSD (n = 55) | HMD (n = 31) | p |
|---|---|---|---|
| Water intake (mL) | 500 (0–2000) | 375 (187.5–500) | 0.357 |
| Daily calorie intake (kcal) | 634 ± 204 | 862 ± 89 | <0.001 |
| Portion (% consumed) | 53.4 ± 12.7 | 71.9 ± 8.5 | <0.001 |
| Assessment | |||
| Taste | 2.5 ± 0.4 | 3.7 ± 0.6 | <0.001 |
| Textures | 2.3 ± 0.4 | 3.2 ± 0.5 | <0.001 |
| Palatability | 2.3 ± 0.4 | 3.2 ± 0.5 | <0.001 |
| Practicality | 2.0 ± 0.4 | 3.7 ± 0.4 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crippa, C.; Matteucci, S.; Pastore, M.; Morenghi, E.; Starace, E.; De Pasquale, G.; Pieri, G.; Soekeland, F.; Gibbi, S.M.; Lo Cricchio, G.; et al. A Comparative Evaluation of the Caloric Intake and Economic Efficiency of Two Types of Homogenized Diets in a Hospital Setting. Nutrients 2023, 15, 4731. https://doi.org/10.3390/nu15224731
Crippa C, Matteucci S, Pastore M, Morenghi E, Starace E, De Pasquale G, Pieri G, Soekeland F, Gibbi SM, Lo Cricchio G, et al. A Comparative Evaluation of the Caloric Intake and Economic Efficiency of Two Types of Homogenized Diets in a Hospital Setting. Nutrients. 2023; 15(22):4731. https://doi.org/10.3390/nu15224731
Chicago/Turabian StyleCrippa, Camilla, Sofia Matteucci, Manuela Pastore, Emanuela Morenghi, Erica Starace, Giulia De Pasquale, Gabriella Pieri, Fanny Soekeland, Stefano Maria Gibbi, Giuliana Lo Cricchio, and et al. 2023. "A Comparative Evaluation of the Caloric Intake and Economic Efficiency of Two Types of Homogenized Diets in a Hospital Setting" Nutrients 15, no. 22: 4731. https://doi.org/10.3390/nu15224731
APA StyleCrippa, C., Matteucci, S., Pastore, M., Morenghi, E., Starace, E., De Pasquale, G., Pieri, G., Soekeland, F., Gibbi, S. M., Lo Cricchio, G., Zorloni, A., Mazzoleni, B., & Mancin, S. (2023). A Comparative Evaluation of the Caloric Intake and Economic Efficiency of Two Types of Homogenized Diets in a Hospital Setting. Nutrients, 15(22), 4731. https://doi.org/10.3390/nu15224731







