The Development of Text Messages to Support People at Risk of Diabetes in Low-Resourced Communities: The South African Diabetes Prevention Programme
Abstract
:1. Introduction
2. Methods and Processes
2.1. Brief Description of the South African Diabetes Prevention Program Intervention
2.2. South African Diabetes Prevention Program Curriculum Development
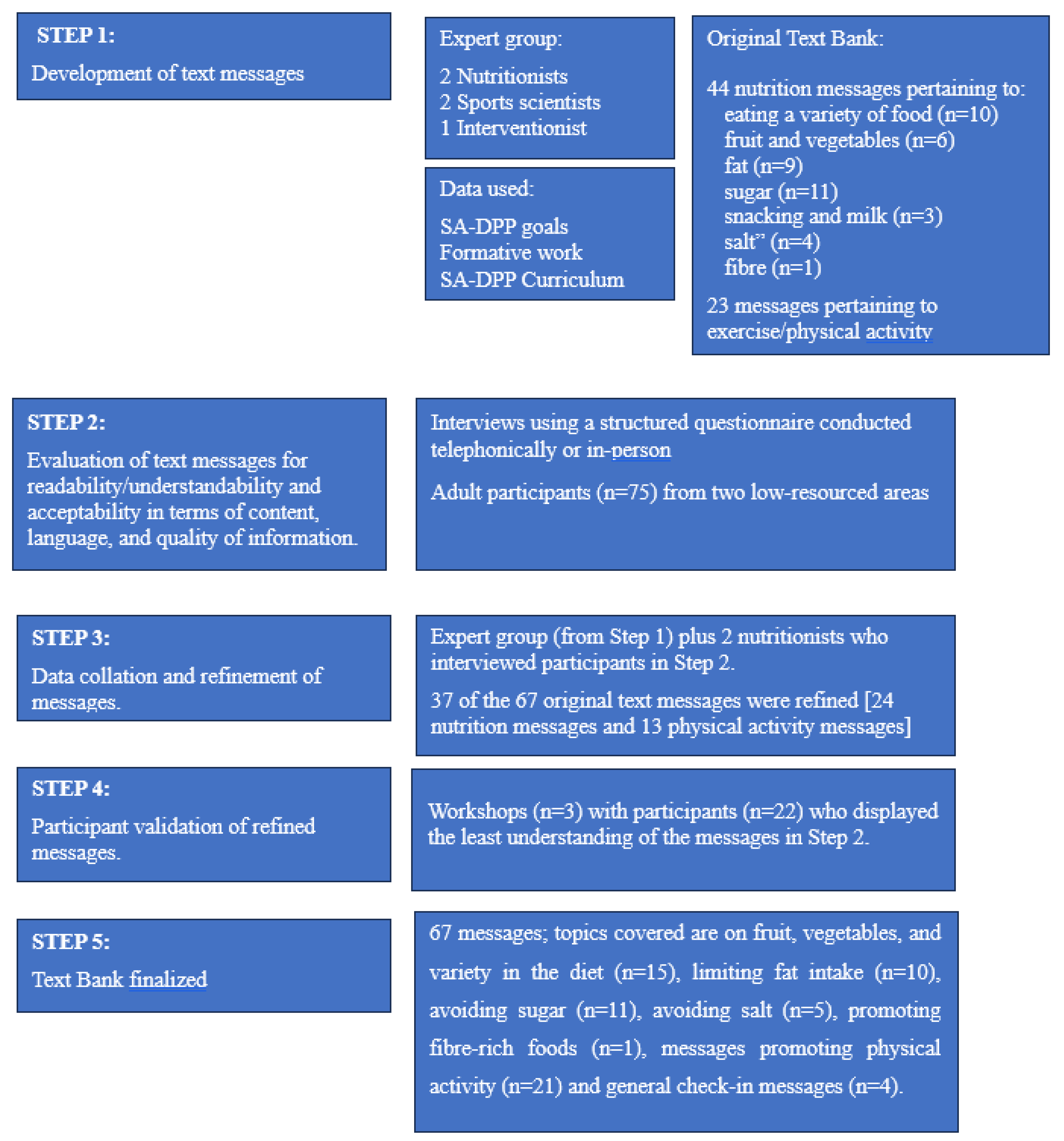
2.3. Text Messaging Development Protocol
2.3.1. Step 1: Text Message Development
2.3.2. Step 2: Text Message Evaluation
2.3.3. Steps 3–5: Message Refinement
3. Results
3.1. Evaluation of Text Messages for Readability/Understandability and Acceptability in Terms of Content, Language, and Quality of Information
3.2. Data Collation and Refinement of Messages
3.3. Participant Validation of Refined Messages
3.4. Text Bank Finalized
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). The Top 10 Causes of Death; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- International Diabetes Federation (IDF). IDF Diabetes Atlas, 10th ed.; International Diabetes Federation (IDF): Brussels, Belgium, 2021. [Google Scholar]
- Pillay-van Wyk, V.; Msemburi, W.; Laubscher, R.; Dorrington, R.E.; Groenewald, P.; Glass, T.; Nojilana, B.; Joubert, J.D.; Matzopoulos, R.; Prinsloo, M.; et al. Mortality trends and differentials in South Africa from 1997 to 2012: Second National Burden of Disease Study. Lancet Glob. Health 2016, 4, e642–e653. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M.; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009, 374, 1677–1686. [Google Scholar] [CrossRef] [PubMed]
- Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: The Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 2015, 3, 866–875. [Google Scholar] [CrossRef]
- Thomson, H.; Oliver, N.; Godsland, I.F.; Darzi, A.; Srivanichakorn, W.; Majeed, A.; Johnston, D.G.; Nanditha, A.; Snehalatha, C.; Raghavan, A.; et al. Protocol for a clinical trial of text messaging in addition to standard care versus standard care alone in prevention of type 2 diabetes through lifestyle modification in India and the UK. BMC Endocr. Disord. 2018, 18, 63. [Google Scholar] [CrossRef] [PubMed]
- Free, C.; Phillips, G.; Galli, L.; Watson, L.; Felix, L.; Edwards, P.; Patel, V.; Haines, A. The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review. PLOS Med. 2013, 10, e1001362. [Google Scholar] [CrossRef]
- Head, K.J.; Noar, S.M.; Iannarino, N.T.; Harrington, N.G. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc. Sci. Med. 2013, 97, 41–48. [Google Scholar] [CrossRef]
- Whittaker, R.; Merry, S.; Dorey, E.; Maddison, R. A Development and Evaluation Process for mHealth Interventions: Examples from New Zealand. J. Health Commun. 2012, 17, 11–21. [Google Scholar] [CrossRef]
- Douglas, N.; Free, C. ‘Someone batting in my corner’: Experiences of smoking-cessation support via text message. Br. J. Gen. Pr. 2013, 63, e768–e776. [Google Scholar] [CrossRef] [PubMed]
- Pfammatter, A.; Spring, B.; Saligram, N.; Davé, R.; Gowda, A.; Blais, L.; Arora, M.; Ranjani, H.; Ganda, O.; Hedeker, D.; et al. mHealth Intervention to Improve Diabetes Risk Behaviors in India: A Prospective, Parallel Group Cohort Study. J. Med. Internet Res. 2016, 18, e207. [Google Scholar] [CrossRef]
- Willoughby, J.F.; Furberg, R. Underdeveloped or Underreported? Coverage of Pretesting Practices and Recommendations for Design of Text Message–Based Health Behavior Change Interventions. J. Health Commun. 2015, 20, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Abroms, L.C.; Whittaker, R.; Free, C.; Van Alstyne, J.M.; Schindler-Ruwisch, J.M. Developing and Pretesting a Text Messaging Program for Health Behavior Change: Recommended Steps. JMIR mHealth uHealth 2015, 3, e107. [Google Scholar] [CrossRef] [PubMed]
- Parra, S.; Ortega, A.; Kanter, R.; Kain, J. Process of developing text messages on healthy eating and physical activity for Chilean mothers with overweight or obese preschool children to be delivered via WhatsApp. Cogent Soc. Sci. 2018, 4, 1521057. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Velicer, W.F. The Transtheoretical Model of Health Behavior Change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Rappaport, J. Terms of empowerment/exemplars of prevention: Toward a theory for community psychology. Am. J. Community Psychol. 1987, 15, 121–148. [Google Scholar] [CrossRef]
- Perkins, D.D. Speaking truth to power: Empowerment ideology as social intervention and policy. Am. J. Community Psychol. 1995, 23, 765–794. [Google Scholar] [CrossRef]
- Tuomilehto, J.; Lindström, J.; Eriksson, J.G.; Valle, T.T.; Hämäläinen, H.; Ilanne-Parikka, P.; Keinänen-Kiukaanniemi, S.; Laakso, M.; Louheranta, A.; Rastas, M.; et al. Prevention of Type 2 Diabetes Mellitus by Changes in Lifestyle among Subjects with Impaired Glucose Tolerance. N. Engl. J. Med. 2001, 344, 1343–1350. [Google Scholar] [CrossRef]
- Hill, J.; Faber, M.; Peer, N.; George, C.; Oldenburg, B.; Kengne, A.P. Adapting and Developing A Diabetes Prevention Intervention Programme for South Africa: Curriculum and Tools. Int. J. Environ. Res. Public Health 2023, 20, 4463. [Google Scholar] [CrossRef]
- Ackermann, R.T.; Marrero, D.G. Adapting the Diabetes Prevention Program Lifestyle Intervention for Delivery in the Community. Diabetes Educ. 2007, 33, 69–78. [Google Scholar] [CrossRef]
- Mathews, E.; Thomas, E.; Absetz, P.; D’esposito, F.; Aziz, Z.; Balachandran, S.; Daivadanam, M.; Thankappan, K.R.; Oldenburg, B. Cultural adaptation of a peer-led lifestyle intervention program for diabetes prevention in India: The Kerala diabetes prevention program (K-DPP). BMC Public Health 2017, 17, 974. [Google Scholar] [CrossRef]
- Vorster, H.H.; Badham, J.B.; Venter, C.S. An introduction to the revised food-based dietary guidelines for South Africa. South Afr. J. Clin. Nutr. 2013, 26, S5–S12. [Google Scholar]
- de Castro, M.S.; Pilger, D.; Fuchs, F.D.; Ferreira, M.B.C. Development and validity of a method for the evaluation of printed education material. Pharm. Pr. (Internet) 2007, 5, 89–94. [Google Scholar] [CrossRef]
- Love, P.; Maunder, E.; Green, J. Are South African women willing and able to apply the new food-based dietary guidelines? Lessons for nutrition educators. South Afr. J. Clin. Nutr. 2008, 21, 17–24. [Google Scholar] [CrossRef]
- Love, P.; Maunder, E.M.W.; Green, M.; Ross, F.; Smale-Lovely, J.; Charlton, K.E. South African food-based dietary guidelines: Testing of the preliminary guidelines among women in KwaZulu-Natal and the Western Cape. South Afr. J. Clin. Nutr. 2001, 14, 9–19. [Google Scholar]
- du Plessis, L.; Daniels, L.; Koornhof, H.; Samuels, S.; Möller, I.; Röhrs, S. Overview of field-testing of the revised, draft South African Paediatric Food-Based Dietary Guidelines amongst mothers/caregivers of children aged 0–5 years in the Western Cape and Mpumalanga, South Africa. South Afr. J. Clin. Nutr. 2021, 34, 123–131. [Google Scholar] [CrossRef]
- Röhrs, S.; du Plessis, L. Field-testing of the revised, draft South African Paediatric Food-Based Dietary Guidelines among moth-ers/caregivers of children between the ages of 3 and 5 years in the Northern Metropole, City of Cape Town, Western Cape province, South Africa. South Afr. J. Clin. Nutr. 2021, 34, 151–156. [Google Scholar] [CrossRef]
- Cole-Lewis, H.; Kershaw, T. Text Messaging as a Tool for Behavior Change in Disease Prevention and Management. Epidemiologic Rev. 2010, 32, 56–69. [Google Scholar] [CrossRef] [PubMed]
- Sekhon, M.; Cartwright, M.; Francis, J.J. Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Serv. Res. 2017, 17, 88. [Google Scholar] [CrossRef]
- Hill, J.; Yako, Y.; George, C.; Musarurwa, H.; Jordaan, E.; Kengne, A.P. A study protocol for a cluster randomized controlled trial to test the applicability of the South African diabetes prevention program in the Eastern Cape Province of South Africa. BMC Public Health 2023, 23, 214. [Google Scholar] [CrossRef] [PubMed]
| Original Message | Comments Received (Survey as Recorded by Interviewers) | Refined Message |
|---|---|---|
| Eat vegetables of different colors, e.g., dark green leafy, yellow, orange, and purple vegetables. | Beetroot is not a purple veg. See it as red. | Eat vegetables of different colors, e.g., dark green leafy (spinach), yellow, orange (butternut/carrots), red (tomato), and purple vegetables (beetroot). |
| Eat different types of food daily to ensure variety in your diet. | “Different types of food” was understood as different vegetables. Diet was understood to mean eating a “certain way”. | Eat foods from different groups every day, i.e., meat, dairy, vegetables, and fruit. |
| Limit or avoid processed foods such as polony and sausage. Healthier options are eggs, peanut butter, canned tuna, and pilchards. | Processed foods were not commonly understood. | Limit ready-to-eat meat products such as polony, Vienna sausages, and Russian sausages. Healthier options are eggs, peanut butter, canned tuna, and pilchards. |
| Do not throw away stale vegetables, use them in soups and stews. | 54.5% of participants did not understand the term “stale” | Do not throw away wilted vegetables, use them in soups and stews. |
| Eat a fresh salad with your cooked meal to add variety and increase your vegetable intake. | Do not usually eat salad with cooked food. | Eat a salad with your meal to increase your vegetable intake. |
| Every hour of TV you watch may shorten your life by 22 min. Why not exercise instead? It can lengthen your life! | Did not understand. | Sitting and watching too much TV is not good for your health. Why not exercise instead? |
| Refined Message | Comments Received from Participants |
|---|---|
| Wilted not clear to all. “Wilted sounds very up-pity”. In Afrikaans, the group understands/or sees it as “oorryp” [over ripe] [Notes from Workshop 1] Wilted” not clear to most participants. [Notes from Workshop 2] “Wilted” not understood by most participants. [Notes from Workshop 3] |
| Spices are seen as chicken spice and barbeque spice, which already contain salt. Herbs are rarely used/only in specific dishes. [Notes from Workshop 1] Herbs were understood correctly. Spices were understood to be “Aromat” or “Braai spice”. Rather say “natural spice” and give examples. [Notes from Workshop 2] Herbs were understood as “plants”. Spices were understood to be Robertson’s “steak & chop spice” or “chicken spice”. [Notes from Workshop 3] |
| Problem with eating cereal with no sugar. Suggestion that we say less sugar to no sugar as was done with a message with reference to tea and coffee. [Notes from Workshop 1] Not all understood “roughage/fiber” There was much resistance to “without sugar for breakfast”. They cannot have Weetbix without sugar. [Notes from Workshop 2] Most did not understand “roughage/fiber”. They have an Xhosa name for it, perhaps that could be used? Participants indicated that Weetbix does need a bit of sugar. [Notes from Workshop 3] |
| Replied that they cannot avoid it, only limit it. [Notes from Workshop 2] Replied that they cannot completely avoid it. [Notes from Workshop 3] |
| Replied that they cannot completely avoid it, but they can limit it. [Notes from Workshop 2] Replied that they cannot completely avoid it. [Notes from Workshop 3] |
| Refined Message | Final Message/s |
|---|---|
| Do not throw away unused or leftover vegetables, use them in soups and stews. |
| Slowly reduce salt when preparing food: use herbs, salt-free spices, and seasonings instead to make food tasty. |
| Avoid salty snacks such as Niknaks and chips (Simba) to lower your salt intake. |
| Avoid sweets and chocolates as they increase your blood sugar too much and too quickly. |
| Every new week brings new opportunities to start or restart healthy habits. Every day brings new opportunities to live healthily. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hill, J.; Faber, M.; George, C.; Peer, N.; Mulabisano, T.; Mostert, S.; Sobngwi, E.; Kengne, A.P. The Development of Text Messages to Support People at Risk of Diabetes in Low-Resourced Communities: The South African Diabetes Prevention Programme. Nutrients 2023, 15, 4692. https://doi.org/10.3390/nu15214692
Hill J, Faber M, George C, Peer N, Mulabisano T, Mostert S, Sobngwi E, Kengne AP. The Development of Text Messages to Support People at Risk of Diabetes in Low-Resourced Communities: The South African Diabetes Prevention Programme. Nutrients. 2023; 15(21):4692. https://doi.org/10.3390/nu15214692
Chicago/Turabian StyleHill, Jillian, Mieke Faber, Cindy George, Nasheeta Peer, Tshavhuyo Mulabisano, Sonja Mostert, Eugene Sobngwi, and Andre P. Kengne. 2023. "The Development of Text Messages to Support People at Risk of Diabetes in Low-Resourced Communities: The South African Diabetes Prevention Programme" Nutrients 15, no. 21: 4692. https://doi.org/10.3390/nu15214692
APA StyleHill, J., Faber, M., George, C., Peer, N., Mulabisano, T., Mostert, S., Sobngwi, E., & Kengne, A. P. (2023). The Development of Text Messages to Support People at Risk of Diabetes in Low-Resourced Communities: The South African Diabetes Prevention Programme. Nutrients, 15(21), 4692. https://doi.org/10.3390/nu15214692






