The Impact of Interventional Weight Loss on Bone Marrow Adipose Tissue in People Living with Obesity and Its Connection to Bone Metabolism
Abstract
:1. Introduction
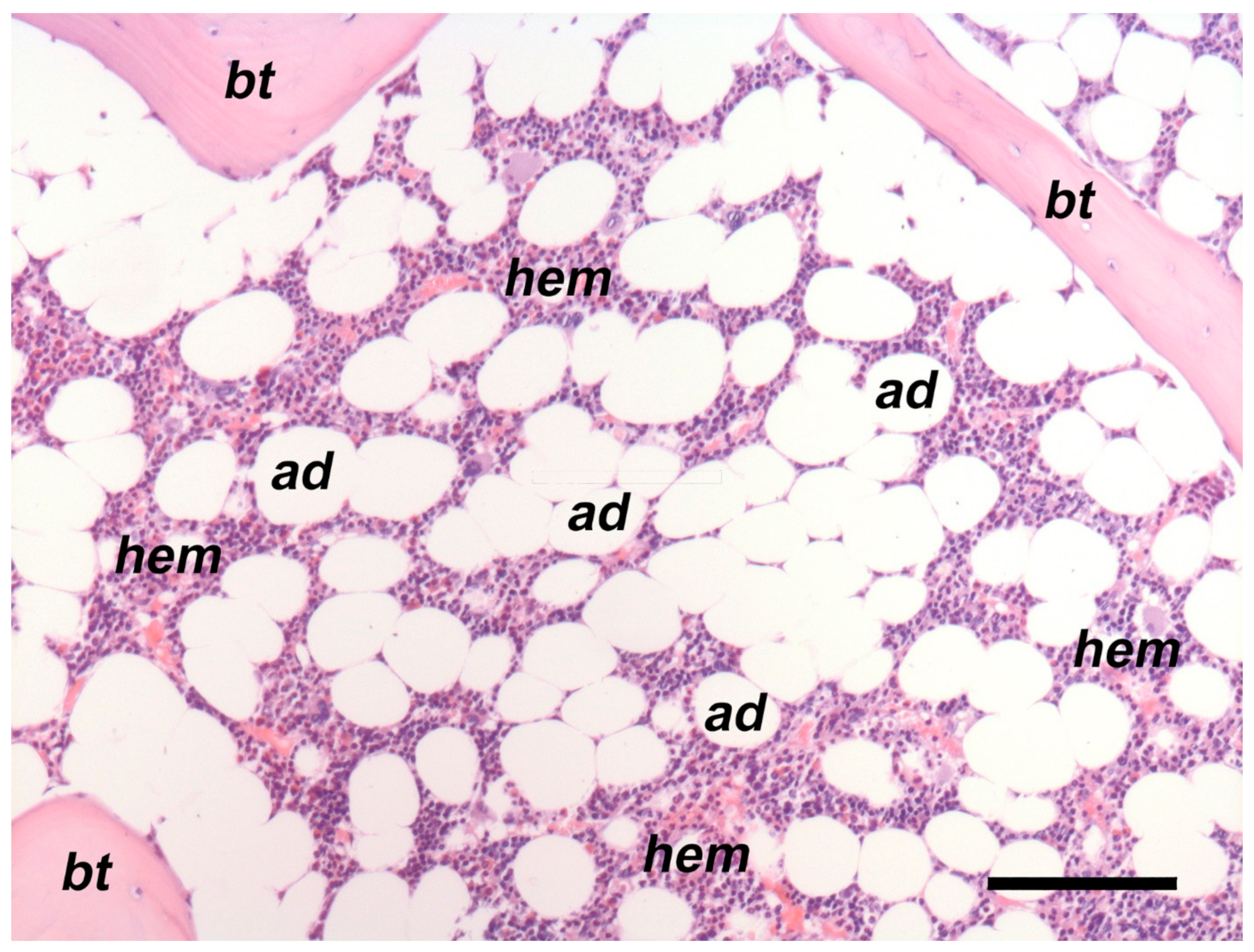
2. Human BMAT Is a Unique Fat Depot
3. Non-Invasive Measurement of BMAT in Humans
4. Obesity and BMAT
5. Dietary-Induced Weight Loss and BMAT
6. Surgical Weight Loss and BMAT
6.1. Roux-en-Y Gastric Bypass
6.2. Sleeve Gastrectomy
6.3. Roux-en-Y Gastric Bypass versus Sleeve Gastrectomy
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Gadde, K.M.; Martin, C.K.; Berthoud, H.R.; Heymsfield, S.B. Obesity: Pathophysiology and Management. J. Am. Coll. Cardiol. 2018, 71, 69–84. [Google Scholar] [CrossRef] [PubMed]
- Pasquali, R.; Casanueva, F.; Haluzik, M.; van Hulsteijn, L.; Ledoux, S.; Monteiro, M.P.; Salvador, J.; Santini, F.; Toplak, H.; Dekkers, O.M. European Society of Endocrinology Clinical Practice Guideline: Endocrine work-up in obesity. Eur. J. Endocrinol. 2020, 182, G1–G32. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.H.; Stoll, C.R.; Song, J.; Varela, J.E.; Eagon, C.J.; Colditz, G.A. The effectiveness and risks of bariatric surgery: An updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014, 149, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Sjöström, L.; Peltonen, M.; Jacobson, P.; Ahlin, S.; Andersson-Assarsson, J.; Anveden, Å.; Bouchard, C.; Carlsson, B.; Karason, K.; Lönroth, H.; et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascu-lar and macrovascular complications. JAMA 2014, 311, 2297–2304. [Google Scholar] [CrossRef]
- Kadowaki, T.; Isendahl, J.K.; Khalid, U.; Lee, S.W.; Nishida, T.; Ogawa, W.; Tobe, K.; Yamauchi, T.; Lim, S. Semaglutide once a week in adults with overweight or obesity, with or without type 2 diabetes in an east Asian population (STEP 6): A randomised, double-blind, double-dummy, placebo-controlled, phase 3a trial. Lancet Diabetes Endocrinol. 2022, 10, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Rubino, D.M.; Grenway, F.L.; Khalid, O.; O’Neil, P.M.; Rosenstock, J.; Sørrig, R.; Wadden, T.A.; Wizert, A.; Garvey, W.T.; STEP 8 Investigators. Effect of weekly subcutaneous Semaglutide vs daily Liraglutide on body weight in adults with overweight or obesity without diabetes. The Step 8 Randomized Clinical Study. JAMA 2022, 327, 138–150. [Google Scholar] [CrossRef] [PubMed]
- Lespessailles, E.; Paccou, J.; Javier, R.M.; Thomas, T.; Cortet, B.; GRIO Scientific Committee. GRIO Scientific Committee. Obesity, Bariatric Surgery, and Fractures. J. Clin. Endocrinol. Metab. 2019, 104, 4756–4768. [Google Scholar] [CrossRef]
- Paccou, J.; Caiazzo, R.; Lespessailles, E.; Cortet, B. Bariatric Surgery and Osteoporosis. Calcif. Tissue Int. 2022, 110, 576–591. [Google Scholar] [CrossRef]
- Papageorgiou, M.; Kerschan-Schindl, K.; Sathyapalan, T.; Pietschmann, P. Is Weight Loss Harmful for Skeletal Health in Obese Older Adults? Gerontology 2020, 66, 2–14. [Google Scholar] [CrossRef]
- Shanbhogue, V.V.; Støving, R.K.; Frederiksen, K.H.; Hanson, S.; Brixen, K.; Gram, J.; Jørgensen, N.R.; Hansen, S. Bone structural changes after gastric bypass surgery evaluated by HR-pQCT: A two-year longitudinal study. Eur. J. Endocrinol. 2017, 176, 685–693. [Google Scholar] [CrossRef]
- Paccou, J.; Martignène, N.; Lespessailles, E.; Babykina, E.; Pattou, F.; Cortet, B.; Ficheur, G. Gastric bypass but not sleeve gastrectomy increases risk of major osteoporotic fracture: French population-based cohort study. J. Bone Miner Res. 2020, 35, 1415–1423. [Google Scholar] [CrossRef] [PubMed]
- Khalid, S.I.; Omotosho, P.A.; Spagnoli, A.; Torquati, A. Association of Bariatric Surgery with Risk of Fracture in Patients with Severe Obesity. JAMA Netw. Open 2020, 3, e207419. [Google Scholar] [CrossRef] [PubMed]
- Paccou, J.; Tsourdi, E.; Meier, C.; Palermo, A.; Pepe, J.; Body, J.-J.; Zillikens, M.C. Bariatric surgery and skeletal health: A narrative review and position statement for management by the European Calcified Tissue Society (ECTS). Bone 2021, 154, 116236. [Google Scholar] [CrossRef] [PubMed]
- Villareal, D.T.; Shah, K.; Banks, M.R.; Sinacore, D.R.; Klein, S. Effect of weight loss and exercise therapy on bone metabolism and mass in obese older adults: A one-year randomized controlled trial. J. Clin. Endocrinol. Metab. 2008, 93, 2181–2187. [Google Scholar] [CrossRef] [PubMed]
- Paccou, J.; Penel, G.; Chauveau, C.; Cortet, B.; Hardouin, P. Marrow adiposity and bone: Review of clinical implications. Bone 2019, 118, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Veldhuis-Vlug, A.G.; Rosen, C.J. Clinical implications of bone marrow adiposity. J. Intern. Med. 2018, 283, 121–139. [Google Scholar] [CrossRef] [PubMed]
- Beekman, K.M.; Duque, G.; Corsi, A.; Tencerova, M.; Bisschop, P.H.; Paccou, J. Osteoporosis and Bone Marrow Adipose Tissue. Curr. Osteoporos. Rep. 2023, 21, 45–55. [Google Scholar] [CrossRef]
- Li, Z.; Rosen, C.J. The Multifaceted Roles of Bone Marrow Adipocytes in Bone and Hematopoietic Homeostasis. J. Clin. Endocrinol. Metab. 2023, dgad355. [Google Scholar] [CrossRef]
- Paccou, J.; Hardouin, P.; Cotten, A.; Penel, G.; Cortet, B. The Role of Bone Marrow Fat in Skeletal Health: Usefulness and Perspectives for Clinicians. J. Clin. Endocrinol. Metab. 2015, 100, 3613–3621. [Google Scholar] [CrossRef]
- Cawthorn, W.P.; Scheller, E.L.; Learman, B.S.; Parlee, S.D.; Simon, B.R.; Mori, H.; Ning, X.; Bree, A.J.; Schell, B.; Broome, D.T.; et al. Bone Marrow Adipose Tissue Is an Endocrine Organ that Contributes to Increased Circulating Adiponectin during Caloric Restriction. Cell Metab. 2014, 20, 368–375. [Google Scholar] [CrossRef]
- Paccou, J.; Badr, S.; Lombardo, D.; Khizindar, H.; Deken, V.; Ruschke, S.; Karampinos, D.C.; Cotten, A.; Cortet, B. Bone Marrow Adiposity and Fragility Fractures in Postmenopausal Women: The ADIMOS Case-Control Study. J. Clin. Endocrinol. Metab. 2023, 108, 2526–2536. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, A.V. Marrow fat and bone: Review of clinical findings. Front. Endocrinol. 2015, 6, 40. [Google Scholar] [CrossRef] [PubMed]
- Woods, G.N.; Ewing, S.K.; Schafer, A.L.; Gudnason, V.; Sigurdsson, S.; Lang, T.; Hue, T.F.; Kado, D.M.; Vittinghoff, E.; Rosen, C.; et al. Saturated and Unsaturated Bone Marrow Lipids Have Distinct Effects on Bone Density and Fracture Risk in Older Adults. J. Bone Miner. Res. 2022, 37, 700–710. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Bowers, E.; Zhu, J.; Yu, H.; Hardij, J.; Bagchi, D.P.; Mori, H.; Lewis, K.T.; Granger, K.; Schill, R.L.; et al. Lipolysis of bone marrow adipocytes is required to fuel bone and the marrow niche during energy deficits. eLife 2022, 11, e78496. [Google Scholar] [CrossRef] [PubMed]
- Fazeli, P.K.; Bredella, M.A.; Pachon-Peña, G.; Zhao, W.; Zhang, X.; Faje, A.T.; Resulaj, M.; Polineni, S.P.; Holmes, T.M.; Lee, H.; et al. The dynamics of human bone marrow adipose tissue in response to feeding and fasting. J. Clin. Investig. 2021, 6, 138636. [Google Scholar] [CrossRef] [PubMed]
- Craft, C.S.; Li, Z.; MacDougald, O.A.; Scheller, E.L. Molecular differences between subtypes of bone marrow adipocytes. Curr. Mol. Biol. Rep. 2018, 4, 16–23. [Google Scholar] [CrossRef]
- Sollmann, N.; Löffler, M.T.; Kronthaler, S.; Böhm, C.; Dieckmeyer, M.; Ruschke, S.; Kirschke, J.S.; Carballido-Gamio, J.; Karampinos, D.C.; Krug, R.; et al. MRI-Based Quantitative Osteoporosis Imaging at the Spine and Femur. J. Magn. Reson. Imaging 2021, 54, 12–35. [Google Scholar] [CrossRef] [PubMed]
- Beekman, K.M.; Regenboog, M.; Nederveen, A.J.; Bravenboer, N.; Heijer, M.D.; Bisschop, P.H.; Hollak, C.E.; Akkerman, E.M.; Maas, M. Gender- and Age-Associated Differences in Bone Marrow Adipose Tissue and Bone Marrow Fat Unsaturation Throughout the Skeleton, Quantified Using Chemical Shift Encoding-Based Water–Fat MRI. Front. Endocrinol. 2022, 13, 815835. [Google Scholar] [CrossRef]
- Tratwal, J.; Labella, R.; Bravenboer, N.; Kerckhofs, G.; Douni, E.; Scheller, E.L.; Badr, S.; Karampinos, D.C.; Beck-Cormier, S.; Palmisano, B.; et al. Reporting Guidelines, Review of Methodological Standards, and Challenges Toward Harmonization in Bone Marrow Adiposity Research. Report of the Methodologies Working Group of the International Bone Marrow Adiposity Society. Front. Endocrinol. 2020, 11, 65. [Google Scholar] [CrossRef]
- Lecka-Czernik, B.; Stechschulte, L.A.; Czernik, P.J.; Dowling, A.R. High bone mass in adult mice with diet-induced obesity results from a combination of initial increase in bone mass followed by attenuation in bone formation; implications for high bone mass and decreased bone quality in obesity. Mol. Cell Endocrinol. 2015, 410, 35–41. [Google Scholar] [CrossRef]
- Doucette, C.R.; Horowitz, M.C.; Berry, R.; MacDougald, O.A.; Anunciado-Koza, R.; Koza, R.A.; Rosen, C.J. A High Fat Diet Increases Bone Marrow Adipose Tissue (MAT) But Does Not Alter Trabecular or Cortical Bone Mass in C57BL/6J Mice. J. Cell Physiol. 2015, 230, 2032–2037. [Google Scholar] [CrossRef]
- Scheller, E.L.; Khoury, B.; Moller, K.L.; Wee, N.K.Y.; Khandaker, S.; Kozloff, K.M.; Abrishami, S.H.; Zamarron, B.F.; Singer, K. Changes in Skeletal Integrity and Marrow Adiposity during High-Fat Diet and after Weight Loss. Front. Endocrinol. 2016, 7, 102. [Google Scholar] [CrossRef] [PubMed]
- Devlin, M.J.; Robbins, A.; Cosman, M.N.; Moursi, C.A.; Cloutier, A.M.; Louis, L.; Van Vliet, M.; Conlon, C.; Bouxsein, M.L. Differential effects of high fat diet and diet-induced obesity on skeletal acquisition in female C57BL/6J vs. FVB/NJ Mice. Bone Rep. 2018, 8, 204–214. [Google Scholar] [CrossRef]
- Charles, A.; Mugisha, A.; Iconaru, L.; Baleanu, F.; Benoit, F.; Surquin, M.; Bergmann, P.; Body, J.J. Distribution of Fracture Sites in Postmenopausal Overweight and Obese Women: The FRISBEE Study. Calcif. Tissue Int. 2022, 111, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Piotrowska, K.; Tarnowski, M. Bone Marrow Adipocytes—Role in Physiology and Various Nutritional Conditions in Human and Animal Models. Nutrients 2021, 13, 1412. [Google Scholar] [CrossRef]
- Li, Z.; MacDougald, O.A. Preclinical models for investigating how bone marrow adipocytes influence bone and hematopoietic cellularity. Best Pract. Res. Clin. Endocrinol. Metab. 2021, 35, 101547. [Google Scholar] [CrossRef]
- Gkastaris, K.; Goulis, D.G.; Potoupnis, M.; Anastasilakis, A.D.; Kapetanos, G. Obesity, osteoporosis and bone metabolism. J. Musculoskelet. Neuronal. Interact. 2020, 20, 372–381. [Google Scholar] [PubMed]
- Compston, J.E.; Watts, N.B.; Chapurlat, R.; Cooper, C.; Boonen, S.; Greenspan, S.; Pfeilschifter, J.; Silverman, S.; Díez-Pérez, A.; Lindsay, R.; et al. Obesity is not protective against fracture in postmenopausal women: GLOW. Am. J. Med. 2011, 124, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Johansson, H.; Kanis, J.A.; Odén, A.; McCloskey, E.; Chapurlat, R.D.; Christiansen, C.; Cummings, S.R.; Diez-Perez, A.; Eisman, J.A.; Fujiwara, S.; et al. A meta-analysis of the association of fracture risk and body mass index in women. J. Bone Miner. Res. 2014, 29, 223–233. [Google Scholar] [CrossRef]
- Cohen, A.; Dempster, D.W.; Recker, R.R.; Lappe, J.M.; Zhou, H.; Zwahlen, A.; Müller, R.; Zhao, B.; Lang, T.; Saeed, I.; et al. Abdominal fat is associated with lower bone formation and inferior bone quality in healthy premenopausal women: A transiliac bone biopsy study. J. Clin. Endocrinol. Metab. 2013, 98, 2562–2572. [Google Scholar] [CrossRef]
- Bredella, M.A.; Torriani, M.; Ghomi, R.H.; Thomas, B.J.; Brick, D.J.; Gerweck, A.V.; Rosen, C.J.; Klibanski, A.; Miller, K.K. Vertebral bone marrow fat is positively associated with visceral fat and inversely associated with IGF-1 in obese women. Obesity 2011, 19, 49–53. [Google Scholar] [CrossRef]
- Bredella, M.; Gill, C.; Gerweck, A.; Landa, M.G.; Kumar, V.; Daley, S.M.; Torriani, M.; Miller, K.K. Ectopic and Serum Lipid Levels Are Positively Associated with Bone Marrow Fat in Obesity. Radiology 2013, 269, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Singhal, V.; Bose, A.; Liang, Y.; Srivastava, G.; Goode, S.; Stanford, F.C.; Misra, M.; Bredella, M.A. Marrow adipose tissue in adolescent girls with obesity. Bone 2019, 129, 115103. [Google Scholar] [CrossRef] [PubMed]
- Singhal, V.; Flores, L.P.T.; Stanford, F.C.; Toth, A.T.; Carmine, B.; Misra, M.; Bredella, M.A. Differential associations between appendicular and axial marrow adipose tissue with bone microarchitecture in adolescents and young adults with obesity. Bone 2018, 116, 203–206. [Google Scholar] [CrossRef] [PubMed]
- CDC: Centers for Disease Control and Prevention. Losing Weight; What Is Healthy Weight Loss? Available online: http://www.cdc.gov/healthyweight/losing_weight/index.html (accessed on 15 May 2023).
- NICE: National Institute for Health and Care Excellence CG43. Obesity: Guidance on the Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children; NICE: London, UK, 2006. [Google Scholar]
- Verheijden, M.W.; Bakx, J.C.; Van Weel, C.; Koelen, M.A.; Van Staveren, W.A. Role of social support in lifestyle-focussed weight management interventions. Euro. J. Clin. Nutr. 2005, 59 (Suppl. S1), 179–186. [Google Scholar] [CrossRef] [PubMed]
- Cordes, C.; Dieckmeyer, M.; Ott, B.; Shen, J.; Ruschke, S.; Settles, M.; Eichhorn, C.; Bauer, J.S.; Kooijman, H.; Rummeny, E.J.; et al. MR-detected changes in liver, abdominal, and vertebral bone marrow fat after a four-week calorie restriction in obese women. J. Magn. Reson. Imaging JMRI 2015, 42, 272–1280. [Google Scholar] [CrossRef]
- Vogt, L.J.; Steveling, A.; Meffert, P.J.; Kromrey, M.L.; Kessler, R.; Hosten, N.; Krüger, J.; Gärtner, S.; Aghdassi, A.A.; Mayerle, J.; et al. Magnetic resonance imaging of changes in abdominal compartments in obese diabetics during a low-calorie weight-loss program. PLoS ONE 2016, 11, e0153595. [Google Scholar] [CrossRef] [PubMed]
- Spurny, M.; Jiang, Y.; Sowah, S.A.; Schübel, R.; Nonnenmacher, T.; Bertheau, R.; Kirsten, R.; Johnson, T.; Hillengass, J.; Schlett, C.L.; et al. Changes in Bone Marrow Fat upon Dietary-Induced Weight Loss. Nutrients 2020, 12, 1509. [Google Scholar] [CrossRef] [PubMed]
- Ofir, N.; Mizrakli, Y.; Greenshpan, Y.; Gepner, Y.; Sharabi, O.; Tsaban, G.; Zelicha, H.; Meir, A.Y.; Ceglarek, U.; Stumvoll, M.; et al. Vertebrae but not femur marrow fat transiently decreases in response to body weight loss in an 18-month randomized control trial. Bone 2023, 171, 116727. [Google Scholar] [CrossRef]
- Kim, T.Y.; Schwartz, A.V.; Li, X.; Xu, K.; Black, D.M.; Petrenko, D.M.; Stewart, L.; Rogers, S.J.; Posselt, A.M.; Carter, J.T.; et al. Bone Marrow Fat Changes After Gastric Bypass Surgery Are Associated with Loss of Bone Mass. J. Bone Miner. Res. 2017, 32, 2239–2247. [Google Scholar] [CrossRef]
- Kim, T.Y.; Schwartz, A.V.; Li, X.; Xu, K.; Kazakia, G.J.; Grunfeld, C.; Nissenson, R.A.; Shoback, D.M.; Schafer, A.L. Bone marrow adipose tissue composition and glycemic improvements after gastric bypass surgery. Bone Rep. 2022, 17, 101596. [Google Scholar] [CrossRef] [PubMed]
- Beekman, K.M.; Akkerman, E.M.; Streekstra, G.J.; Veldhuis-Vlug, A.G.; Acherman, Y.; Gerdes, V.E.; den Heijer, M.; Maas, M.; Bravenboer, N.; Bisschop, P.H. The Effect of Roux-en-Y Gastric Bypass on Bone Marrow Adipose Tissue and Bone Mineral Density in Postmenopausal, Nondiabetic Women. Obesity 2021, 29, 1120–1127. [Google Scholar] [CrossRef] [PubMed]
- Blom-Høgestøl, I.K.; Mala, T.; Kristinsson, J.A.; Hauge, E.; Brunborg, C.; Gulseth, H.L.; Eriksen, E.F. Changes in Bone Marrow Adipose Tissue One Year After Roux-en-Y Gastric Bypass: A Prospective Cohort Study. J. Bone Miner. Res. 2019, 34, 1815–1823. [Google Scholar] [CrossRef] [PubMed]
- Bredella, M.A.; Singhal, V.; Hazhir Karzar, N.; Animashaun, A.; Bose, A.; Stanford, F.C.; Carmine, B.; Misra, M. Effects of Sleeve Gastrectomy on Bone Mar-row Adipose Tissue in Adolescents and Young Adults with Obesity. J. Clin. Endocrinol. Metab. 2020, 105, e3961–e3970. [Google Scholar] [CrossRef] [PubMed]
- Huber, F.A.; Singhal, V.; Tuli, S.; Becetti, I.; López López, A.P.; Bouxsein, M.L.; Misra, M.; Bredella, M.A. Two-year Skeletal Effects of Sleeve Gastrectomy in Ado-lescents with Obesity Assessed with Quantitative CT and MR Spectroscopy. Radiology 2023, 307, e223256. [Google Scholar] [CrossRef] [PubMed]
- Bredella, M.A.; Greenblatt, L.B.; Eajazi, A.; Torriani, M.; Yu, E.W. Effects of Roux-en-Y gastric bypass and sleeve gastrectomy on bone mineral density and marrow adipose tissue. Bone 2017, 95, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Ivaska, K.K.; Huovinen, V.; Soinio, M.; Hannukainen, J.C.; Saunavaara, V.; Salminen, P.; Helmiö, M.; Parkkola, R.; Nuutila, P.; Kiviranta, R. Changes in bone metabolism after bariatric surgery by gastric bypass or sleeve gastrectomy. Bone 2017, 95, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Rao, R.S.; Rao, V.; Kini, S. Animal models in bariatric surgery—A review of the surgical techniques and postsurgical physiology. Obes. Surg. 2010, 20, 1293–1305. [Google Scholar] [CrossRef]
- Lutz, T.A.; Bueter, M. The Use of Rat and Mouse Models in Bariatric Surgery Experiments. Front. Nutr. 2016, 3, 25. [Google Scholar] [CrossRef]
- Scheller, E.L.; Doucette, C.R.; Learman, B.S.; Cawthorn, W.P.; Khandaker, S.; Schell, B.; Wu, B.; Ding, S.-Y.; Bredella, M.A.; Fazeli, P.K.; et al. Region-specific variation in the properties of skeletal adipocytes reveals regulated and constitutive marrow adipose tissues. Nat. Commun. 2015, 6, 7808. [Google Scholar] [CrossRef]
- Li, Z.; Hardij, J.; Bagchi, D.P.; Scheller, E.L.; MacDougald, O.A. Development, regulation, metabolism and function of bone marrow adipose tissues. Bone 2018, 110, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Suchacki, K.J.; Cawthorn, W.P. Molecular Interaction of Bone Marrow Adipose Tissue with Energy Metabolism. Curr. Mol. Biol. Rep. 2018, 4, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Scheller, E.L.; Khandaker, S.; Learman, B.S.; Cawthorn, W.P.; Anderson, L.M.; Pham, H.; Robles, H.; Wang, Z.; Li, Z.; Parlee, S.D.; et al. Bone marrow adipocytes resist lipolysis and remodeling in response to β-adrenergic stimulation. Bone 2019, 118, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Styner, M.; Thompson, W.R.; Galior, K.; Uzer, G.; Wu, X.; Kadari, S.; Case, N.; Xie, Z.; Sen, B.; Romaine, A.; et al. Bone marrow fat accumulation accelerated by high fat diet is suppressed by exercise. Bone 2014, 64, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Hardij, J.; Evers, S.S.; Hutch, C.R.; Choi, S.M.; Shao, Y.; Learman, B.S.; Lewis, K.T.; Schill, R.L.; Mori, H.; et al. G-CSF partially mediates effects of sleeve gastrectomy on the bone marrow niche. J. Clin. Investig. 2019, 129, 2404–2416. [Google Scholar] [CrossRef] [PubMed]
- Bozadjieva-Kramer, N.; Shin, J.H.; Shao, Y.; Gutierrez-Aguilar, R.; Li, Z.; Heppner, K.M.; Chiang, S.; Vargo, S.G.; Granger, K.; Sandoval, D.A.; et al. Intestinal-derived FGF15 protects against deleterious effects of vertical sleeve gastrectomy in mice. Nat. Commun. 2021, 12, 4768. [Google Scholar] [CrossRef]
- Fazeli, P.K.; Horowitz, M.C.; MacDougald, O.A.; Scheller, E.L.; Rodeheffer, M.S.; Rosen, C.J.; Klibanski, A. Marrow fat and bone—New perspectives. J. Clin. Endocrinol. Metab. 2013, 98, 935–945. [Google Scholar] [CrossRef]
- Botolin, S.; McCabe, L.R. Bone loss and increased bone adiposity in spontaneous and pharmacologically induced diabetic mice. Endocrinology 2007, 148, 198–205. [Google Scholar] [CrossRef]
- Sulston, R.J.; Learman, B.S.; Zhang, B.; Scheller, E.L.; Parlee, S.D.; Simon, B.R.; Mori, H.; Bree, A.J.; Wallace, R.J.; Krishnan, V.; et al. Increased Circulating Adiponectin in Response to Thiazolidinediones: Investigating the Role of Bone Marrow Adipose Tissue. Front. Endocrinol. 2016, 7, 128. [Google Scholar] [CrossRef]
- Tencerova, M.; Figeac, F.; Ditzel, N.; Taipaleenmäki, H.; Nielsen, T.K.; Kassem, M. High-Fat Diet-Induced Obesity Promotes Expansion of Bone Marrow Adipose Tissue and Impairs Skeletal Stem Cell Functions in Mice. J. Bone Miner. Res. 2018, 33, 1154–1165. [Google Scholar] [CrossRef]
- Devlin, M.J.; Cloutier, A.M.; Thomas, N.A.; Panus, D.A.; Lotinun, S.; Pinz, I.; Baron, R.; Rosen, C.J.; Bouxsein, M.L. Caloric restriction leads to high marrow adiposity and low bone mass in growing mice. J. Bone Miner. Res. 2010, 25, 2078–2088. [Google Scholar] [CrossRef] [PubMed]
- Cawthorn, W.P.; Scheller, E.L.; Parlee, S.D.; Pham, H.A.; Learman, B.S.; Redshaw, C.M.H.; Sulston, R.J.; Burr, A.A.; Das, A.K.; Simon, B.R.; et al. Expansion of Bone Marrow Adipose Tissue During Caloric Restriction Is Associated With Increased Circulating Glucocorticoids and Not With Hypoleptinemia. Endocrinology 2016, 157, 508–521. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Bagchi, D.P.; Zhu, J.; Bowers, E.; Yu, H.; Hardij, J.; Mori, H.; Granger, K.; Skjaerlund, J.D.; Mandair, G.S.; et al. Constitutive bone marrow adipocytes suppress local bone formation. J. Clin. Investig. 2022, 7, e160915. [Google Scholar] [CrossRef] [PubMed]
- Baum, T.; Yap, S.P.; Karampinos, D.C.; Nardo, L.; Kuo, D.; Burghardt, A.J.; Masharani, U.B.; Schwartz, A.V.; Li, X.; Link, T.M. Does vertebral bone marrow fat content correlate with abdominal adipose tissue, lumbar spine bone mineral density, and blood biomarkers in women with type 2 diabetes mellitus? J. Magn. Reason. Imaging 2012, 35, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Sheu, Y.; Amati, F.; Schwartz, A.V.; Danielson, M.E.; Li, X.; Boudreau, R.; Cauley, J.A.; Osteoporotic Fractures in Men (MrOS) Research Group. Vertebral bone marrow fat, bone mineral density and diabetes: The Osteoporotic Fractures in Men (MrOS) study. Bone 2017, 97, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Yu, E.W.; Greenblatt, L.; Eajazi, A.; Torriani, M.; Bredella, M.A. Marrow adipose tissue composition in adults with morbid obesity. Bone 2017, 97, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Woods, G.N.; Ewing, S.K.; Sigurdsson, S.; Kado, D.M.; Ix, J.H.; Hue, T.F.; Eiriksdottir, G.; Xu, K.; Gudnason, V.; Lang, T.F.; et al. Chronic Kidney Disease Is Associated with Greater Bone Marrow Adiposity. J. Bone Miner. Res. 2018, 33, 2158–2164. [Google Scholar] [CrossRef] [PubMed]
- Moorthi, R.N.; Fadel, W.; Eckert, G.J.; Ponsler-Sipes, K.; Moe, S.M.; Lin, C. Bone marrow fat is increased in chronic kidney disease by magnetic resonance spectroscopy. Osteoporos. Int. 2015, 26, 1801–1807. [Google Scholar] [CrossRef]
- Badr, S.; Cotten, A.; Mentaverri, R.; Lombardo, D.; Labreuche, J.; Martin, C.; Hénaut, L.; Cortet, B.; Paccou, J. Relationship between Bone Marrow Adipose Tissue and kidney function in postmenopausal women. Bone Rep. 2023, 19, 101713. [Google Scholar] [CrossRef]
- Kuiper, J.W.; van Kuijk, C.; Grashuis, J.L.; Ederveen, A.G.H.; Schütte, H.E. Accuracy and the Influence of Marrow Fat on Quantitative CT and Dual-Energy X-ray Absorp-tiometry Measurements of the Femoral Neck in Vitro. Osteoporos. Int. 1996, 6, 25–30. [Google Scholar] [CrossRef]
- Sfeir, J.G.; Drake, M.T.; Atkinson, E.J.; Achenbach, S.J.; Camp, J.J.; Tweed, A.J.; McCready, L.K.; Yu, L.; Adkins, M.C.; Amin, S.; et al. Evaluation of Cross-Sectional and Longitudinal Changes in Volumetric Bone Mineral Density in Postmenopausal Women Using Single-versus Dual-Energy Quantitative Computed Tomography. Bone 2018, 112, 145–152. [Google Scholar] [CrossRef]
- Yu, E.W.; Thomas, B.J.; Brown, J.K.; Finkelstein, J.S. Simulated Increases in Body Fat and Errors in Bone Mineral Density Measurements by DXA and QCT. J. Bone Miner. Res. 2012, 27, 119–124. [Google Scholar] [CrossRef]

| Study | Population | Obesity Classification Study | Imaging Method | Results |
|---|---|---|---|---|
| Bredella et al., Obesity 2011 [41] | n = 47 Age: 32.8 ± 7.1 years BMI (range: 18–41 kg/m2) Mean 30 ± 7 kg/m2 Female 100% Premenopausal: yes T2D: no | Cross-sectional BMI (range: 18–41 kg/m2) Cohort divided into low (n = 23) and high visceral fat (VAT) content (n = 24) | BMAT: (1H MRS; 3.0T MR imaging system) and QCT for vBMD BMAT in L4 Trabecular vBMD in L4 | L4 BMAT as lipid/water ratio Higher in high VAT group vs. low VAT group (p = 0.05) Trabecular vBMD (mg/cm3) Low VAT group vs. high VAT group (NS) |
| Bredella et al., Radiology, 2013 [42] | n = 106 (46 men and 60 women) Age: 33.7 ± 6.8 years BMI (range 18.1–48.8 kg/m2) Mean 33.1 kg/m2 ± 7.1 Female: 65% Premenopausal: yes T2D: no | Cross-sectional BMI (range 18.1–48.8 kg/m2) | BMAT: (1H MRS; 3.0T MR imaging system) and QCT for vBMD | Positive correlations between BMAT L4 and ectopic fat content independent of BMI Positive correlations between BMAT L4 and HDL cholesterol levels |
| Cohen et al., JCEM, 2013 [40] | n = 40 Age: 37.3 ± 8.2 years BMI: 25.8 ± 4.7 kg/m2 Female: 100% Premenopausal: yes T2D: no | Cross-sectional BMI ranged from 20.1 to 39.2 kg/m2 | BMAT: transiliac bone biopsy, scanned by μCT; evaluation by OsteoMeasure (OsteoMeasure, version 4.00C; OsteoMetrics, Inc., Atlanta, GA, USA) software aBMD (DXA): Femoral neck, total hip, lumbar spine | Increased BMAT in obese and overweight vs. lean controls Negative correlation between BMAT and several bone parameters |
| Singhal et al., Bone, 2019 [43] | n = 60 adolescent girls Age: 14–21 years 18 ± 2 years Female: 100% Premenopausal: yes T2D: no | Cross-sectional BMI above the 95th percentile for age and gender | BMAT: 1H MRS (vertebra): L4 vBMD: QCT L4 | BMAT was lower in obese at the femoral diaphysis (p ≤ 0.0001) and the lumbar spine (p = 0.0039) For the whole group, BMAT at the lumbar spine and femoral diaphysis was inversely associated with BMI, total fat mass, lean mass, and VAT |
| Study | Population | Intervention | Imaging Method | Results |
|---|---|---|---|---|
| Kim et al. JBMR, 2017 [52] | n = 25 Age: 48 ± 12 years Female 100%, Postmenopausal: 37% T2D: 52% Other: Premenopausal women on OAC and postmenopausal women on HRT | RYGB Preoperative and 6 months postoperative | BMAT (1H MRS): L3–4 vBMD (QCT): L3–4 | ΔBMAT: Decrease in BMAT in T2D+ group Total: −2.5 ± 10%; p = 0.20 T2D+: −6.5 ± 11%; p = 0.05 T2D−: +1.8 ± 5.6%; p = 0.29 ΔvBMD: Decrease in vBMD of the lumbar spine Total: −6.4 ± 5.9%, p < 0.05 T2D+: −4.2 ± 6.5%; p < 0.05 T2D−: −8.7 ± 4.2%; p < 0.05 Other: In T2D−: negative association between ΔBMAT and Δbody weight Negative correlation between ΔBMAT and ΔBMD (r = −0.58, p < 0.01) Greater decrease in HbA1c was associated with decrease in BMAT |
| Kim et al. Bone Reports 2022 [53] | n = 25 Age: 48.2 ± 11.7 years Female 100%, Postmenopausal: 37% T2D: 52% Other: Premenopausal women on OAC and postmenopausal women on HRT | RYGB Preoperative and 6 months postoperative | BMAT: (1H MRS) BMAT and unsaturated lipid index (UI) L3–4 and BMAT in the distal tibia in subset of n = 15 vBMD: QCT L3–4 | Spine ΔBMAT: No change Total: 66 ± 14% → 65 ± 14; −1.5%, p = 0.54 T2D+: 66 ± 13% → 62 ± 14; −6.5%, p = 0.09 T2D−: 65 ± 15% → 68 ± 14; +4%, p = 0.13 Spine ΔUI: Increased in T2D+ Total: 5.1 ± 1.7% → 5.1 ± 1.6%; 0%, p = 0.90 T2D+: 4.5 ± 0.8% → 5.6 ± 1.5%; +24.4%, p = 0.02 T2D−: 5.7 ± 2.2% → 4.6 ± 1.5%; −19.3%, p = 0.06 Tibia (n = 15; T2D+ n = 9) ΔBMAT: No change Total: 98 ± 1% → 98 ± 1%; −0.3%, p = 0.32 T2D+: 97 ± 1% → 97 ± 1%; −0.4%, p = 0.34 T2D−: 98 ± 1% → 98 ± 1%; −0.1%, p = 0.86 Tibia (n = 15; T2D+ n = 9) ΔUI: Decreased in total group Total: 4.2 ± 1.2% → 3.9 ± 1.2%; −7.1%, p = 0.04 T2D+: 4.1 ± 1.0% → 3.8 ± 1.2%; −7.3%, p = 0.24 T2D−: 4.5 ± 1.5% → 3.9 ± 1.3%; −13.3%, p = 0.11 vBMD L3–L4: Decreased in all groups Total: −6.4 ± 5.9%, p < 0.05 T2D+: −4.2 ± 6.5%, p < 0.05 T2D−: 8.7 ± 4.2%, p < 0.05 Other: At the spine, a significant interaction between T2D status and ΔBMAT (p = 0.02) and ΔUI (p < 0.01) ΔUI was inversely correlated with ΔHbA1c (r = −0.47, p = 0.02) |
| Beekman et al. Obesity, 2021 [54] | n = 14 Age: 58 ± 4 years Female: 100% Postmenopausal: 100% T2D: 0% | RYGB Preoperative, postoperative (3 and 12 months) | BMAT (CSE-WFI) L3–5 vBMD (QCT) L3–4 | ΔBMAT: Decreased 12 months after surgery Baseline: 51 ± 8% 3 months: 50 ± 8% 12 months: 46 ± 7%; −9.3%, p = 0.004 ΔvBMD: Decreased 3 and 12 months after surgery Baseline: 101 ± 26 mg/cm3 3 months: 94 ± 28 mg/cm3; −7.6%, p = 0.003 12 months: 94 ± 28 mg/cm3; −6.4%, p = 0.035 Other: No correlation between changes in BMAT and changes in vBMD Positive correlation between changes in BMAT and changes in body weight |
| Blom-Høgestøl et al. JBMR 2019 [55] | n = 30 Age: 46.3 ± 9.6 years Female: 60% Postmenopausal: n = 8; 44% of the females T2D: 37% | RYGB Preoperative and 1-year postoperative | BMAT: Iliac crest biopsy (grid-based point counting) aBMD: lumbar spine and femoral neck | ΔBMAT: BMAT decreased after RYGB in female subjects Total: 40.4 ± 1.7% → 35.6 ± 12.8%; −10,7%, p = 0.04 Female: 39.4 ± 9.9% → 30.1 ± 9.0%; −22.4% p < 0.001 Male: 41.9 ± 8.4% → 43.7 ± 13.8%; +6.8%, ns ΔBMAT: BMAT decreased similar in pre- and postmenopausal women Postmenopausal: −18.8 ± 18% Pre-menopausal: −25.3 ± 21.3% ΔBMAT: BMAT decreased in T2D+ and T2D− groups T2D+: 43.3 ± 10.9% → 40.3 ± 15.3%; −6.9% T2D−: 38.7 ± 8.1% → 32.8 ± 10.7%; −15.2% (n = 11, after RYGB: remission in 10/11) ΔaBMD: decreased after RYGB Lumbar spine: −4.3 ± 5.9% Femoral neck: −8.2 ± 4.85% Total hip: −11.8 ± 4.9% Other: Changes in serum estradiol in males was negatively associated with changes in BMAT after RYGB (Serum testosterone increased, p < 0.001, estradiol decreased, p = 0.035) ΔBMAT was positively associated with ΔBMI and Δbody fat |
| Bredella et al. JCEM, 2020 [56] | n = 26 Age: 18.0 ± 2.1 years Female: 73% Postmenopausal: 0% T2D: unknown | Sleeve gastrectomy (SG) Preoperative and 1-year postoperative | BMAT: (1H MRS) BMAT and unsaturated and saturated BMAT (lipid to water ratio): L1–L2, femoral mid-diaphysis, distal tibia metaphysis vBMD (QCT): L1–L2 | Lumbar spine L1–L2: Decrease in BMAT and increase in saturated lipids ΔBMAT: 0.37 ± 0.17 → 0.49 ± 0.25; +32%, p = 0.001 ΔUnsaturated 0.03 ± 0.01 → 0.04 ± 0.03; +33%, p = 0.1 ΔSaturated 0.30 ± 0.15 → 0.39 ± 0.19; +30%, p < 0.001 Femoral mid-diaphysis: BMAT unchanged and decrease in unsaturated lipids ΔBMAT: 4.89 ± 2.96 → 3.92 ± 2.33; −20%, p = 0.09 ΔUnsaturated 0.43 ± 0.29 → 0.30 ± 0.24; −30%, p = 0.02 ΔSaturated 3.35 ± 1.95 → 2.93 ± 1.73; −13%, p = 0.3 Tibia distal (metaphysis): Decrease in BMAT and decrease in saturated lipids ΔBMAT: 11.39 ± 3.02 → 10.01 ± 2.00; −12%, p = 0.04 ΔUnsaturated 1.31 ± 0.62 → 1.45 ± 0.76; +11%, p = 0.39 ΔSaturated 8.82 ± 2.41 → 7.72 ± 1.65; −12%, p = 0.02 vBMD L1–L2: Decrease in vBMD 200 ± 39 mg/cm3 → 193 ± 38 mg/cm3; −3%, p = 0.04 |
| Huber et al. Radiology, 2023 [57] | n = 54 Age 18 ± 3 years, range 13–24 years Female: 41 T2D: unknown Postmenopausal: none | SG: n = 25 Control: n = 29 (dietary and exercise counselling) Preoperative and after 24 months | BMAT L1–L2 vBMD L1–L2 | Increase in BMAT 2 years after SG ΔBMAT: SG 0.38 ± 0.15 → 0.48 ± 0.19; +26% p = 0.001 Controls 0.46 ± 0.22 → 0.52 ± 0.25; +13% p = 0.11 p-value for 24 months change between groups: p = 0.40 Decrease in vBMD after SG ΔvBMD (trabecular) mg/cm3: SG 250 ± 28 → 232 ± 29; −7.2% p < 0.001 Controls 242 ± 34 → 241 ± 33; −0.4% p = 0.99 p-value for 24 months change between groups: p < 0.001 Inverse correlation between ΔBMAT and ΔvBMD (r = −0.41 p = 0.01). |
| Bredella, Bone, 2017 [58] | n = 21 Age 49 ± 9 years Female: 86% Postmenopausal: Unknown T2D: 38% | RYGB: n = 11 T2D: n = 2 (18%) SG: n = 10 T2D: n = 6 (60%) Preoperative and 1-year postoperative | BMAT: (1H MRS) L1–L2 (LS); femur (metaphysis and diaphysis) vBMD: QCT L3–L4, femoral neck and total hip | ΔBMAT (data estimated from graph): Increase in BMAT of the lumbar spine and femoral diaphysis after SG RYGB: Lumbar spine: −6%; ns Diaphysis: −2%; ns Metaphysis: +2%; ns SG: Lumbar spine +20%; p < 0.05 Diaphysis: +18%; p < 0.05 Metaphysis: −6%; ns vBMD: Decrease after both RYGB and SG Other: No difference between T2D+ and T2D− Excluding male subjects, did not change the results Positive correlation between ΔBMI/VAT and ΔBMAT |
| Ivaska et al. Bone, 2017 [59] | n = 18 (subpopulation) Age: unknown (whole group: 45 ± 9.5 years) Female: unknown (whole group: n = 42, 91%) T2D: n = 8 (38%) Postmenopausal: unknown | RYGB: n = 7 SG: n = 14 Preoperative and 6 months postoperative | BMAT: 1H MRS (vertebra) vBMD: QCT L1–L2, VAT | ΔBMAT: No difference in BMAT after RYGB or SG Total: median change −10.7%, p = 0.18 Negative correlation between BMAT and vBMD pre- and postoperative, in subjects T2D− (r = −0.74, p = 0.01 and r = −0.82, p = 0.007, respectively) No correlation between BMAT and vBMD in T2D+ Exact number of subjects with BMAT measurements remains unclear, data only in graph, no exact data on ΔBMAT in table or graph Unclear in which vertebral body BMAT was quantified |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tencerova, M.; Duque, G.; Beekman, K.M.; Corsi, A.; Geurts, J.; Bisschop, P.H.; Paccou, J. The Impact of Interventional Weight Loss on Bone Marrow Adipose Tissue in People Living with Obesity and Its Connection to Bone Metabolism. Nutrients 2023, 15, 4601. https://doi.org/10.3390/nu15214601
Tencerova M, Duque G, Beekman KM, Corsi A, Geurts J, Bisschop PH, Paccou J. The Impact of Interventional Weight Loss on Bone Marrow Adipose Tissue in People Living with Obesity and Its Connection to Bone Metabolism. Nutrients. 2023; 15(21):4601. https://doi.org/10.3390/nu15214601
Chicago/Turabian StyleTencerova, Michaela, Gustavo Duque, Kerensa M. Beekman, Alessandro Corsi, Jeroen Geurts, Peter H. Bisschop, and Julien Paccou. 2023. "The Impact of Interventional Weight Loss on Bone Marrow Adipose Tissue in People Living with Obesity and Its Connection to Bone Metabolism" Nutrients 15, no. 21: 4601. https://doi.org/10.3390/nu15214601
APA StyleTencerova, M., Duque, G., Beekman, K. M., Corsi, A., Geurts, J., Bisschop, P. H., & Paccou, J. (2023). The Impact of Interventional Weight Loss on Bone Marrow Adipose Tissue in People Living with Obesity and Its Connection to Bone Metabolism. Nutrients, 15(21), 4601. https://doi.org/10.3390/nu15214601







