Isolate Whey Protein Promotes Fluid Balance and Endurance Capacity Better Than Isolate Casein and Carbohydrate-Electrolyte Solution in a Warm, Humid Environment
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Preliminary Testing
2.3. Experimental Protocol
2.4. Laboratory Analysis
2.5. Statistical Analysis
3. Results
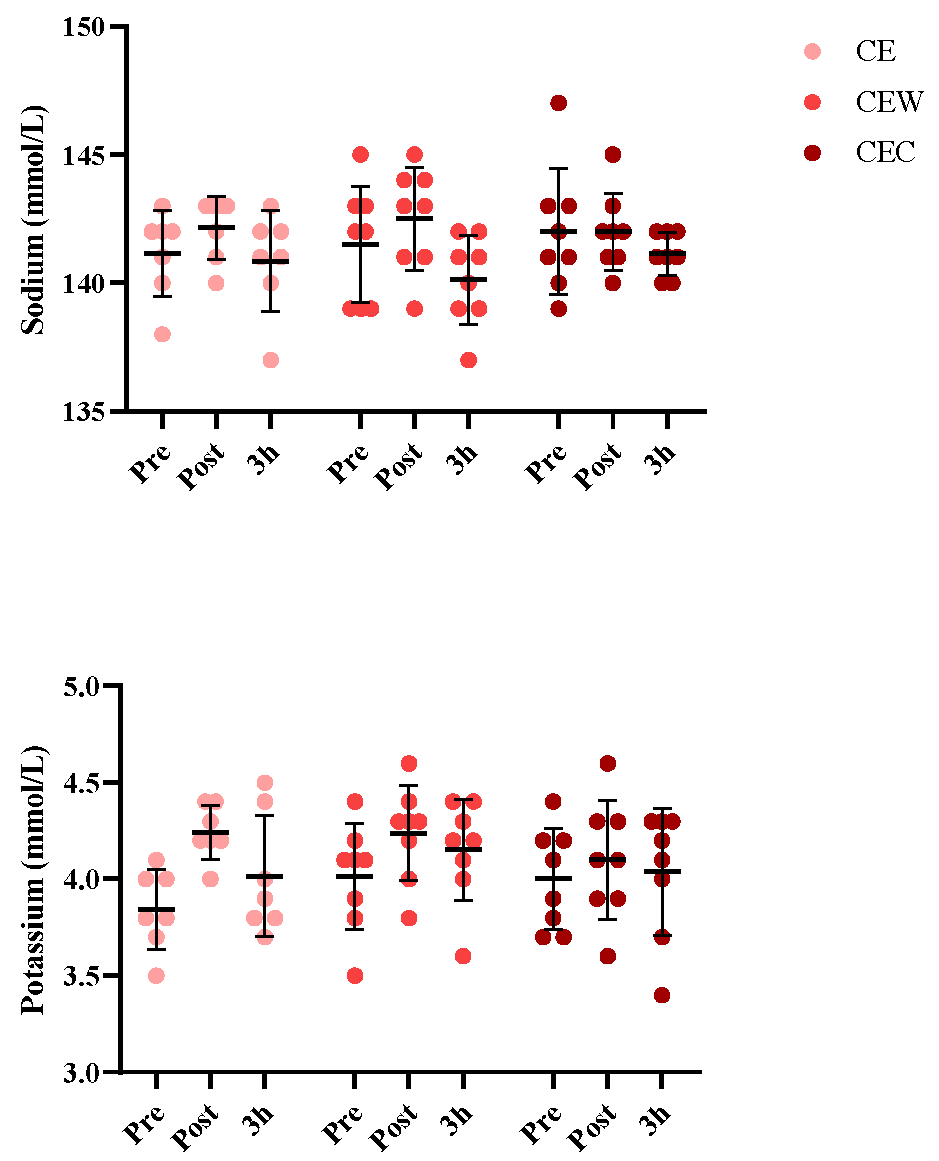
3.1. Electrolyte Balance
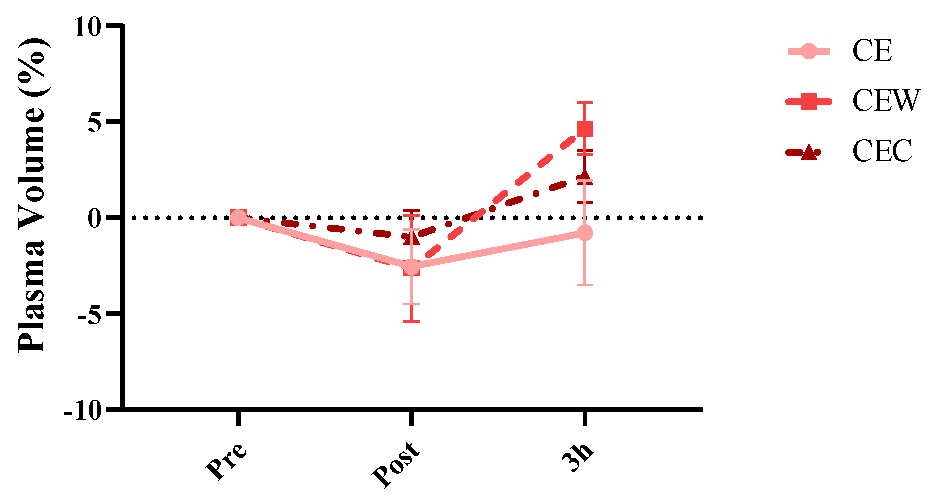
3.2. NFB and Fluid Retention
3.3. Subjective Feeling
3.4. Endurance Capacity Test
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marriott, B.M. Interaction of Water Bioavailability, Thermoregulation, and Exercise Performance, in Fluid Replacement and Heat Stress; National Academies Press: Cambridge, MA, USA, 1994. [Google Scholar]
- Tucker, M.A.; Six, A.; Moyen, N.E.; Satterfield, A.Z.; Ganio, M.S.; Caldwell, A.R.; Butts, C.L.; Robinson, F.B.; Reynebeau, H.C.; Kavouras, S.A.; et al. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 1992, 73, 1340–1350. [Google Scholar] [CrossRef]
- Convertino, V.A.; Armstrong, L.E.; Coyle, E.F.; Mack, G.W.; Sawka, M.N.; Senay, L.C.; Sherman, W.M. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sport. Exerc. 1996, 28, i–vii. [Google Scholar] [CrossRef]
- Shirreffs, S.M.; Maughan, R.J.; Tan, X.R.; Low, I.C.C.; Stephenson, M.C.; Kok, T.; Nolte, H.W.; Soong, T.W.; Lee, J.K.W.; Evans, G.H.; et al. Volume repletion after exercise-induced volume depletion in humans: Replacement of water and sodium losses. Am. J. Physiol. Physiol. 1998, 274, F868–F875. [Google Scholar] [CrossRef]
- Wong, S.H.; Williams, C. Influence of Different Amounts of Carbohydrate on Endurance Running Capacity Following Short Term Recovery. Int. J. Sports Med. 2000, 21, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Shirreffs, S.M.; Sawka, M.N. Fluid and electrolyte needs for training, competition, and recovery. J. Sports Sci. 2011, 29 (Suppl. S1), S39–S46. [Google Scholar] [CrossRef] [PubMed]
- Fan, P.W.; Burns, S.F.; Lee, J.K.W. Efficacy of Ingesting an Oral Rehydration Solution after Exercise on Fluid Balance and Endurance Performance. Nutrients 2020, 12, 3826. [Google Scholar] [CrossRef] [PubMed]
- Halder, S.; Daw, S. Importance of Sports Drinks as a Performance Prerequisites. Senhri J. Multidiscip. Stud. 2020, 5, 2582–6840. [Google Scholar] [CrossRef]
- James, L.J.; Shirreffs, S.M. Effect of Electrolyte Addition to Rehydration Drinks Consumed After Severe Fluid and Energy Restriction. J. Strength Cond. Res. 2015, 29, 521–527. [Google Scholar] [CrossRef]
- Merson, S.J.; Maughan, R.J.; Shirreffs, S.M. Rehydration with drinks differing in sodium concentration and recovery from moderate exercise-induced hypohydration in man. Eur. J. Appl. Physiol. 2008, 103, 585–594. [Google Scholar] [CrossRef]
- Shirreffs, S.M.; Armstrong, L.E.; Cheuvront, S.N. Fluid and electrolyte needs for preparation and recovery from training and competition. J. Sports Sci. 2004, 22, 57–63. [Google Scholar] [CrossRef]
- Tambalis, K.D. The effect of electrolytes and energy drinks consumption on athletic performance—A narrative review. Eur. J. Fitness, Nutr. Sport Med. Stud. 2022, 3. [Google Scholar] [CrossRef]
- Aimutis, W.R. Bioactive Properties of Milk Proteins with Particular Focus on Anticariogenesis. J. Nutr. 2004, 134, 989S–995S. [Google Scholar] [CrossRef] [PubMed]
- Shirreffs, S.M.; Watson, P.; Maughan, R.J. Milk as an effective post-exercise rehydration drink. Br. J. Nutr. 2007, 98, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Watson, P.; Love, T.D.; Maughan, R.J.; Shirreffs, S.M. A comparison of the effects of milk and a carbohydrate-electrolyte drink on the restoration of fluid balance and exercise capacity in a hot, humid environment. Eur. J. Appl. Physiol. 2008, 104, 633–642. [Google Scholar] [CrossRef]
- Seifert, J.; Harmon, J.; DeClercq, P. Protein added to a sports drink improves fluid retention. Int. J. Sport Nutr. Exerc. Metab. 2006, 16, 420–429. [Google Scholar] [CrossRef]
- James, L.J.; Evans, G.H.; Madin, J.; Scott, D.; Stepney, M.; Harris, R.; Stone, R.; Clayton, D.J. Effect of varying the concentrations of carbohydrate and milk protein in rehydration solutions ingested after exercise in the heat. Br. J. Nutr. 2013, 110, 1285–1291. [Google Scholar] [CrossRef]
- Li, L.; Wong, S.H.-S.; Sun, F.-H. Effects of protein addition to carbohydrate–electrolyte solutions on postexercise rehydration. J. Exerc. Sci. Fit. 2015, 13, 8–15. [Google Scholar] [CrossRef]
- Li, L.; Sun, F.-H.; Huang, W.Y.-J.; Wong, S.H.-S. Effects of whey protein in carbohydrate-electrolyte drinks on post-exercise rehydration. Eur. J. Sport Sci. 2018, 18, 685–694. [Google Scholar] [CrossRef]
- Hobson, R.; James, L. The addition of whey protein to a carbohydrate–electrolyte drink does not influence post-exercise rehydration. J. Sports Sci. 2015, 33, 77–84. [Google Scholar] [CrossRef]
- Miller, T.A. NSCA’s Guide to Tests and Assessments; Human Kinetics: Champaign, IL, USA, 2012. [Google Scholar]
- Jackson, A.S.; Pollock, M.L.; Gettman, L.R. Intertester Reliability of Selected Skinfold and Circumference Measurements and Percent Fat Estimates. Res. Quarterly. Am. Alliance Heal. Phys. Educ. Recreat. 1978, 49, 546–551. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sport. Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Lee, M.-H.; Gisnarian, C.J.; Shann, K.G. Improved Estimation of Total Blood Volume Can Provide a Reliable Prediction of Dilutional Hematocrit and Oxygen Delivery during Cardiopulmonary Bypass. J. Extra-Corpor. Technol. 2019, 51, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Judelson, D.A.; Maresh, C.M.; Anderson, J.M.; Armstrong, L.E.; Casa, D.J.; Kraemer, W.J.; Volek, J.S. Hydration and muscular performance: Does fluid balance affect strength, power and high-intensity endurance? Sport. Med. 2007, 37, 907–921. [Google Scholar] [CrossRef]
- Savoie, F.-A.; Kenefick, R.W.; Ely, B.R.; Cheuvront, S.N.; Goulet, E.D.B. Effect of Hypohydration on Muscle Endurance, Strength, Anaerobic Power and Capacity and Vertical Jumping Ability: A Meta-Analysis. Sports Med. 2015, 45, 1207–1227. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; Cheuvront, S.N.; Galloway, S.D.; Shirreffs, S.M. Fluid needs for training, competition, and recovery in track-and-field athletes. Int. J. Sport Nutr. Exerc. Metab. 2019, 29, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Ganio, M.S.; Armstrong, L.E.; Casa, D.J.; McDermott, B.P.; Lee, E.C.; Yamamoto, L.M.; Marzano, S.; Lopez, R.M.; Jimenez, L.; Le Bellego, L.; et al. Mild dehydration impairs cognitive performance and mood of men. Br. J. Nutr. 2011, 106, 1535–1543. [Google Scholar] [CrossRef]
- Shirreffs, S.M. Hydration in sport and exercise: Water, sports drinks and other drinks. Nutr. Bull. 2009, 34, 374–379. [Google Scholar] [CrossRef]
- Wong, S.H.-S.; Chen, Y. Effect of a carbohydrate-electrolyte beverage, lemon tea, or water on rehydration during short-term recovery from exercise. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 300–310. [Google Scholar] [CrossRef]
- James, L.J.; Gingell, R.; Evans, G.H. Whey protein addition to a carbohydrate-electrolyte rehydration solution ingested after exercise in the heat. J. Athl. Train. 2012, 47, 61–66. [Google Scholar] [CrossRef]
- Leser, S. Potential role for protein in assisting post-exercise rehydration. Nutr. Bull. 2011, 36, 224–234. [Google Scholar] [CrossRef]
- Tang, J.E.; Moore, D.R.; Kujbida, G.W.; Tarnopolsky, M.A.; Phillips, S.M. Ingestion of whey hydrolysate, casein, or soy protein isolate: Effects on mixed muscle protein synthesis at rest and following resistance exercise in young men. J. Appl. Physiol. 2009, 107, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Hall, W.L.; Millward, D.J.; Long, S.J.; Morgan, L.M. Casein and whey exert different effects on plasma amino acid profiles, gastrointestinal hormone secretion and appetite. Br. J. Nutr. 2003, 89, 239–248. [Google Scholar] [CrossRef]
- Wapnir, R.; Zdanowicz, M.M.; Teichberg, S.; Lifshitz, F. Oral hydration solutions in experimental osmotic diarrhea: Enhancement by alanine and other amino acids and oligopeptides. Am. J. Clin. Nutr. 1988, 48, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Lima, A.A.; Carvalho, G.; Figueiredo, A.A.; Gifoni, R.; Soares, A.M.; Silva, E.A.; Guerrant, R.L. Effects of an alanyl-glutamine—Based oral rehydration and nutrition therapy solution on electrolyte and water absorption in a rat model of secretory diarrhea induced by cholera toxin. Nutrition 2002, 18, 458–462. [Google Scholar] [CrossRef] [PubMed]
- James, L.J.; Clayton, D.; Evans, G.H. Effect of milk protein addition to a carbohydrate–electrolyte rehydration solution ingested after exercise in the heat. Br. J. Nutr. 2011, 105, 393–399. [Google Scholar] [CrossRef]
- Armstrong, L.E.; Pumerantz, A.C.; Fiala, K.A.; Roti, M.W.; Kavouras, S.A.; Casa, D.J.; Maresh, C.M. Human Hydration Indices: Acute and Longitudinal Reference Values. Int. J. Sport Nutr. Exerc. Metab. 2010, 20, 145–153. [Google Scholar] [CrossRef]
- Armanini, D.; Bordin, L.; Dona’, G.; Andrisani, A.; Ambrosini, G.; Sabbadin, C. Relationship between water and salt intake, osmolality, vasopressin, and aldosterone in the regulation of blood pressure. J. Clin. Hypertens. 2018, 20, 1455. [Google Scholar] [CrossRef]
- Evans, G.H.; Shirreffs, S.M.; Maughan, R.J. Postexercise rehydration in man: The effects of carbohydrate content and osmolality of drinks ingested ad libitum. Appl. Physiol. Nutr. Metab. 2009, 34, 785–793. [Google Scholar] [CrossRef]
- Osterberg, K.L.; Pallardy, S.E.; Johnson, R.J.; Horswill, C.A. Carbohydrate exerts a mild influence on fluid retention following exercise-induced dehydration. J. Appl. Physiol. 2010, 108, 245–250. [Google Scholar] [CrossRef]
- Schmedes, M.; Bendtsen, L.Q.; Gomes, S.; Liaset, B.; Holst, J.J.; Ritz, C.; Reitelseder, S.; Sjödin, A.; Astrup, A.; Young, J.F.; et al. The effect of casein, hydrolyzed casein, and whey proteins on urinary and postprandial plasma metabolites in overweight and moderately obese human subjects. J. Sci. Food Agric. 2018, 98, 5598–5605. [Google Scholar] [CrossRef]

| CE | CEW | CEC | |
|---|---|---|---|
| Carbohydrate (g) | 66 | 44 | 44 |
| Protein (g) | 0 | 22 | 22 |
| Sodium (mM) | 14 | 14 | 14 |
| Potassium (mM) | 3. 3 | 3. 3 | 3. 3 |
| Energy (kcal/L) | 264 | 264 | 264 |
| Variable | CE | CEW | CEC |
|---|---|---|---|
| Measure | |||
| Anthropometry | |||
| Age (y) | 24.3 ± 2.4 | 24.6 ± 2.1 | 24.2 ± 1.8 |
| Body mass (kg) | 75.2 ± 3.6 | 74.7 ± 4.1 | 76.5 ± 5.2 |
| Stature (cm) | 176.4 ± 6.8 | 177.1 ± 5.4 | 176.6 ± 7.3 |
| BMI (kg.m−2) | 24.2 ± 1.5 | 23.9 ± 1.3 | 24.3 ± 1.7 |
| VO2max (mL/kg/min) | 49.8 ± 4.1 | 48.5 ± 3.9 | 50.2 ± 4.4 |
| Biochemical markers | |||
| USG (g/mL) | 1.019 ± 0.002 | 1.018 ± 0.002 | 1.018 ± 0.002 |
| Glucose (mg/dl) | 91.33 ± 6.26 | 93.25 ± 7.41 | 91.68 ± 5.17 |
| Na (mmol/L) | 141 ± 1.67 | 141± 2.1 | 141 ± 1.49 |
| K (mmol/L) | 3.8 ± 0.2 | 4 ± 0.2 | 4 ± 0.1 |
| Hemoglobin (g/dL) | 14.47 ± 0.71 | 14.95 ± 0.62 | 14.96 ± 0.85 |
| Hematocrit (%) | 44.02 ± 1.93 | 43.72 ± 1.42 | 44.51 ± 1.14 |
| PV (ml) | 2883.42 ± 201.79 | 2800.25 ± 216.54 | 2852 ± 231.76 |
| Variable | Trial | Mean ± SD | ANOVA p-Value |
|---|---|---|---|
| Body mass loss (kg) | CE CEW CEC | 1.61 ± 0.17 1.62 ± 0.11 1.61 ± 0.12 | p = 0.997 |
| Dehydration time (min) | CE CEW CEC | 11.42 ± 2.17 12.75 ± 1.53 12.63 ± 1.27 | p = 0.418 |
| Volume of fluid consumed during the rehydration period (mL) | CE CEW CEC | 2235.71 ± 188.66 2287.5 ± 203.10 2303.75 ± 246.05 | p = 0.820 |
| Variable | Trial | Mean ± SD | ANOVA | Pairwise Comparison | ES (95% CI) |
|---|---|---|---|---|---|
| Physical Capacity | CE CEW CEC | 12.9 ± 1.01 11.4 ± 1.41 14.25 ± 1.58 | p = 0.002 | CE vs CEW: p = 0.142 CE vs CEC: p = 0.215 CEW vs CEC: p = 0.001 | 0.7 (−0.35, 3.35) 0.29 (−3.2, 0.50) −0.59 (−4.64, −1.05) |
| Pre | Post | |
|---|---|---|
| Mean Skin Temperature | ||
| CE | 37.7 ± 0.3 | 37.3 ± 0.5 |
| CEW | 37.2 ± 0.7 | 37.5 ± 0.6 |
| CEC | 37.5 ± 0.8 | 37.9 ± 0.8 |
| Heart Rate | ||
| CE | 75 ± 8 | 181 ± 6 |
| CEW | 76 ± 2 | 178 ± 4 |
| CEC | 78 ± 5 | 187 ± 4 |
| Ratings of Perceived Exertion | ||
| CE | - | 17 ± 2 |
| CEW | - | 16 ± 2 |
| CEC | - | 19 ± 2 |
| Thermal Stress (10 unbearable cold; 10 unbearable heat) | ||
| CE | 3 ± 1 | 7 ± 1 |
| CEW | 3 ± 1 | 7 ± 2 |
| CEC | 3 ± 1 | 9 ± 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gholizadeh, M.; Shakibaee, A.; Bagheri, R.; Camera, D.M.; Shirvani, H.; Dutheil, F. Isolate Whey Protein Promotes Fluid Balance and Endurance Capacity Better Than Isolate Casein and Carbohydrate-Electrolyte Solution in a Warm, Humid Environment. Nutrients 2023, 15, 4374. https://doi.org/10.3390/nu15204374
Gholizadeh M, Shakibaee A, Bagheri R, Camera DM, Shirvani H, Dutheil F. Isolate Whey Protein Promotes Fluid Balance and Endurance Capacity Better Than Isolate Casein and Carbohydrate-Electrolyte Solution in a Warm, Humid Environment. Nutrients. 2023; 15(20):4374. https://doi.org/10.3390/nu15204374
Chicago/Turabian StyleGholizadeh, Mahdi, Abolfazl Shakibaee, Reza Bagheri, Donny M. Camera, Hossein Shirvani, and Frederic Dutheil. 2023. "Isolate Whey Protein Promotes Fluid Balance and Endurance Capacity Better Than Isolate Casein and Carbohydrate-Electrolyte Solution in a Warm, Humid Environment" Nutrients 15, no. 20: 4374. https://doi.org/10.3390/nu15204374
APA StyleGholizadeh, M., Shakibaee, A., Bagheri, R., Camera, D. M., Shirvani, H., & Dutheil, F. (2023). Isolate Whey Protein Promotes Fluid Balance and Endurance Capacity Better Than Isolate Casein and Carbohydrate-Electrolyte Solution in a Warm, Humid Environment. Nutrients, 15(20), 4374. https://doi.org/10.3390/nu15204374






