Oral Hypofunction and Risk of Weight Change among Independent Older Adults
Abstract
1. Introduction
2. Materials and Methods
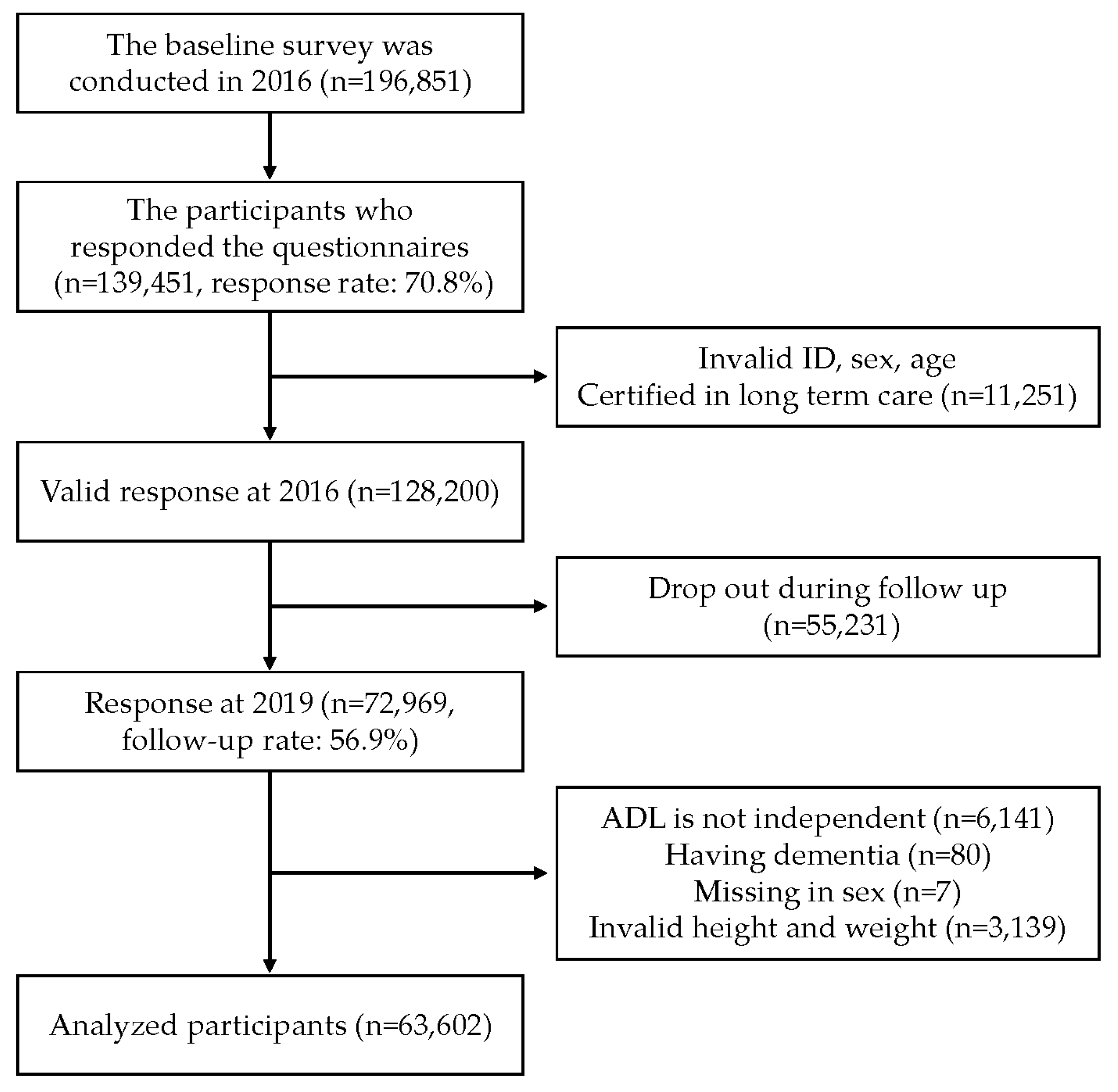
2.1. Study Design and Participants
2.2. Outcome Variables
2.3. Explanatory Variables
2.4. Covariates
2.5. Statistical Analysis
2.6. Ethical Issues
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leij-Halfwerk, S.; Verwijs, M.H.; van Houdt, S.; Borkent, J.W.; Guaitoli, P.R.; Pelgrim, T.; Heymans, M.W.; Power, L.; Visser, M.; Corish, C.A.; et al. Prevalence of Protein-Energy Malnutrition Risk in European Older Adults in Community, Residential and Hospital Settings, According to 22 Malnutrition Screening Tools Validated for Use in Adults ≥65 Years: A Systematic Review and Meta-Analysis. Maturitas 2019, 126, 80–89. [Google Scholar] [CrossRef]
- Gaddey, H.L.; Holder, K. Unintentional Weight Loss in Older Adults. Am. Fam. Physician 2014, 89, 718–722. [Google Scholar]
- Sulmont-Rossé, C.; Van Wymelbeke-Delannoy, V.; Maître, I. Prevalence of Undernutrition and Risk of Undernutrition in Overweight and Obese Older People. Front. Nutr. 2022, 9, 892675. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, T.A.; Paudel, S.; Gasevic, D.; Ryan, J.; Freak-Poli, R.; Owen, A.J. The Association of Weight Change and All-Cause Mortality in Older Adults: A Systematic Review and Meta-Analysis. Age Ageing 2021, 50, 697–704. [Google Scholar] [CrossRef]
- Liu, X.; Tou, N.X.; Gao, Q.; Gwee, X.; Wee, S.L.; Ng, T.P. Frailty and Risk of Cardiovascular Disease and Mortality. PLoS ONE 2022, 17, e0272527. [Google Scholar] [CrossRef] [PubMed]
- Biggs, M.L.; Mukamal, K.J.; Luchsinger, J.A.; Ix, J.H.; Carnethon, M.R.; Newman, A.B.; de Boer, I.H.; Strotmeyer, E.S.; Mozaffarian, D.; Siscovick, D.S. Association between Adiposity in Midlife and Older Age and Risk of Diabetes in Older Adults. JAMA 2010, 303, 2504–2512. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, H.; Sanmartin Berglund, J.; Renvert, S. Longitudinal Evaluation of Periodontitis and Tooth Loss among Older Adults. J. Clin. Periodontol. 2019, 46, 1041–1049. [Google Scholar] [CrossRef]
- Borg-Bartolo, R.; Roccuzzo, A.; Molinero-Mourelle, P.; Schimmel, M.; Gambetta-Tessini, K.; Chaurasia, A.; Koca-Ünsal, R.B.; Tennert, C.; Giacaman, R.; Campus, G. Global Prevalence of Edentulism and Dental Caries in Middle-Aged and Elderly Persons: A Systematic Review and Meta-Analysis. J. Dent. 2022, 127, 104335. [Google Scholar] [CrossRef]
- Kusama, T.; Nakazawa, N.; Kiuchi, S.; Kondo, K.; Osaka, K.; Aida, J. Dental Prosthetic Treatment Reduced the Risk of Weight Loss among Older Adults with Tooth Loss. J. Am. Geriatr. Soc. 2021, 69, 2498–2506. [Google Scholar] [CrossRef]
- Dibello, V.; Lobbezoo, F.; Sardone, R.; Lozupone, M.; Castellana, F.; Zupo, R.; Pilotto, A.; Daniele, A.; Solfrizzi, V.; Manfredini, D.; et al. The Relationship between Oral Health-Related Quality of Life and Body Mass Index in an Older Population from Southern Italy: The Salus in Apulia Study. J. Pers. Med. 2023, 13, 1300. [Google Scholar] [CrossRef]
- Son, K.Y.; Kwon, H.; Park, J.H.; Joh, H.-K.; Hwang, S.E.; Cho, S.H.; Han, K.; Cho, B.; Park, Y.-G. Association between Weight Change over a Period of 4 Years and Mortality in Korean Older Adults. Geriatr. Gerontol. Int. 2020, 20, 474–481. [Google Scholar] [CrossRef]
- Yazawa, A.; Inoue, Y.; Kondo, N.; Miyaguni, Y.; Ojima, T.; Kondo, K.; Kawachi, I. Accuracy of Self-Reported Weight, Height and Body Mass Index among Older People in Japan. Geriatr. Gerontol. Int. 2020, 20, 803–810. [Google Scholar] [CrossRef]
- Whitcomb, B.W.; Naimi, A.I. Things Don’t Always Go as Expected: The Example of Nondifferential Misclassification of Exposure-Bias and Error. Am. J. Epidemiol. 2020, 189, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Hirano, H.; Ohara, Y.; Nishimoto, M.; Iijima, K. Oral Frailty Index-8 in the Risk Assessment of New-Onset Oral Frailty and Functional Disability among Community-Dwelling Older Adults. Arch. Gerontol. Geriatr. 2021, 94, 104340. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Hirano, H. Decline in Oral Function and Its Management. Int. Dent. J. 2022, 72, S12–S20. [Google Scholar] [CrossRef] [PubMed]
- Kugimiya, Y.; Motokawa, K.; Yamamoto, K.; Hayakawa, M.; Mikami, Y.; Iwasaki, M.; Ohara, Y.; Shirobe, M.; Edahiro, A.; Watanabe, Y.; et al. Relationship between the rate of a decreased oral function and the nutrient intake in community-dwelling older persons: An examination using oral function-related items in a questionnaire for latter-stage elderly people. Nihon Ronen Igakkai Zasshi 2021, 58, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Ueno, M.; Shimazu, T.; Sawada, N.; Tsugane, S.; Kawaguchi, Y. Validity of Self-Reported Tooth Counts and Masticatory Status Study of a Japanese Adult Population. J. Oral. Rehabil. 2018, 45, 393–398. [Google Scholar] [CrossRef]
- Satake, S.; Senda, K.; Hong, Y.-J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for Assessing Frailty Status. Geriatr. Gerontol. Int. 2016, 16, 709–715. [Google Scholar] [CrossRef]
- Kiesswetter, E.; Hengeveld, L.M.; Keijser, B.J.; Volkert, D.; Visser, M. Oral Health Determinants of Incident Malnutrition in Community-Dwelling Older Adults. J. Dent. 2019, 85, 73–80. [Google Scholar] [CrossRef]
- Kusama, T.; Takeuchi, K.; Kiuchi, S.; Aida, J.; Kondo, K.; Osaka, K. Weight Loss Mediated the Relationship between Tooth Loss and Mortality Risk. J. Dent. Res. 2023, 102, 45–52. [Google Scholar] [CrossRef]
- Naimi, A.I.; Whitcomb, B.W. Estimating Risk Ratios and Risk Differences Using Regression. Am. J. Epidemiol. 2020, 189, 508–510. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, T.R.; Lee, K.J.; Ryan, P.; Salter, A.B. Multiple Imputation for Handling Missing Outcome Data When Estimating the Relative Risk. BMC Med. Res. Methodol. 2017, 17, 134. [Google Scholar] [CrossRef] [PubMed]
- Royston, P.; White, I.R. Multiple Imputation by Chained Equations (MICE): Implementation in Stata. J. Stat. Softw. 2011, 45, 1–20. [Google Scholar] [CrossRef]
- Onder, G.; Liperoti, R.; Soldato, M.; Cipriani, M.C.; Bernabei, R.; Landi, F. Chewing Problems and Mortality in Older Adults in Home Care: Results from the Aged in Home Care Study. J. Am. Geriatr. Soc. 2007, 55, 1961–1966. [Google Scholar] [CrossRef]
- Hussein, S.; Kantawalla, R.F.; Dickie, S.; Suarez-Durall, P.; Enciso, R.; Mulligan, R. Association of Oral Health and Mini Nutritional Assessment in Older Adults: A Systematic Review with Meta-Analyses. J. Prosthodont. Res. 2022, 66, 208–220. [Google Scholar] [CrossRef] [PubMed]
- Gellacic, A.S.; Teixeira, D.S.C.; Antunes, J.L.F.; Narvai, P.C.; Lebrão, M.L.; Frazão, P. Factors Associated with Deterioration of Self-Rated Chewing Ability among Adults Aged 60 Years and Older over a 6-Year Period. Geriatr. Gerontol. Int. 2016, 16, 46–54. [Google Scholar] [CrossRef]
- Kusama, T.; Takeuchi, K.; Kiuchi, S.; Aida, J.; Hikichi, H.; Sasaki, S.; Kondo, K.; Osaka, K. Dental Prosthesis Use Is Associated with Higher Protein Intake among Older Adults with Tooth Loss. J. Oral. Rehabil. 2023, 50, 1229–1238. [Google Scholar] [CrossRef]
- Gray-Donald, K.; St-Arnaud-McKenzie, D.; Gaudreau, P.; Morais, J.A.; Shatenstein, B.; Payette, H. Protein Intake Protects against Weight Loss in Healthy Community-Dwelling Older Adults. J. Nutr. 2014, 144, 321–326. [Google Scholar] [CrossRef][Green Version]
- Kang, J.; Smith, S.; Pavitt, S.; Wu, J. Association between Central Obesity and Tooth Loss in the Non-Obese People: Results from the Continuous National Health and Nutrition Examination Survey (NHANES) 1999-2012. J. Clin. Periodontol. 2019, 46, 430–437. [Google Scholar] [CrossRef]
- Iwasaki, T.; Fukuda, H.; Kitamura, M.; Kawashita, Y.; Hayashida, H.; Furugen, R.; Koyama, Z.; Ando, Y.; Saito, T. Association between Number of Pairs of Opposing Posterior Teeth, Metabolic Syndrome, and Obesity. Odontology 2019, 107, 111–117. [Google Scholar] [CrossRef]
- Östberg, A.-L.; Bengtsson, C.; Lissner, L.; Hakeberg, M. Oral Health and Obesity Indicators. BMC Oral. Health 2012, 12, 50. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, G.H.; Dominguez, B.L.; Schork, M.A.; Loesche, W.J. Functional Units, Chewing, Swallowing, and Food Avoidance among the Elderly. J. Prosthet. Dent. 1997, 77, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Van der Bilt, A. Assessment of Mastication with Implications for Oral Rehabilitation: A Review. J. Oral. Rehabil. 2011, 38, 754–780. [Google Scholar] [CrossRef] [PubMed]
- Tada, A.; Miura, H. Association of Mastication and Factors Affecting Masticatory Function with Obesity in Adults: A Systematic Review. BMC Oral. Health 2018, 18, 76. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, N.; Kikutani, T.; Tamura, F.; Groher, M.; Kuboki, T. Videoendoscopic Assessment of Swallowing Function to Predict the Future Incidence of Pneumonia of the Elderly. J. Oral. Rehabil. 2012, 39, 429–437. [Google Scholar] [CrossRef]
- Hanson, L.C.; Ersek, M.; Lin, F.C.; Carey, T.S. Outcomes of Feeding Problems in Advanced Dementia in a Nursing Home Population. J. Am. Geriatr. Soc. 2013, 61, 1692–1697. [Google Scholar] [CrossRef]
- Takehara, S.; Hirani, V.; Wright, F.A.C.; Naganathan, V.; Blyth, F.M.; Le Couteur, D.G.; Waite, L.M.; Seibel, M.J.; Handelsman, D.J.; Cumming, R.G. Appetite, Oral Health and Weight Loss in Community-Dwelling Older Men: An Observational Study from the Concord Health and Ageing in Men Project (CHAMP). BMC Geriatr. 2021, 21, 255. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, K.; Aida, J.; Ito, K.; Furuta, M.; Yamashita, Y.; Osaka, K. Nutritional Status and Dysphagia Risk among Community-Dwelling Frail Older Adults. J. Nutr. Health Aging 2014, 18, 352–357. [Google Scholar] [CrossRef]
- Okabe, Y.; Furuta, M.; Akifusa, S.; Takeuchi, K.; Adachi, M.; Kinoshita, T.; Kikutani, T.; Nakamura, S.; Yamashita, Y. Swallowing Function and Nutritional Status in Japanese Elderly People Receiving Home-Care Services: A 1-Year Longitudinal Study. J. Nutr. Health Aging 2016, 20, 697–704. [Google Scholar] [CrossRef]
- Iwasaki, M.; Motokawa, K.; Watanabe, Y.; Shirobe, M.; Ohara, Y.; Edahiro, A.; Kawai, H.; Fujiwara, Y.; Kim, H.; Ihara, K.; et al. Oral Hypofunction and Malnutrition among Community-Dwelling Older Adults: Evidence from the Otassha Study. Gerodontology 2022, 39, 17–25. [Google Scholar] [CrossRef]
- Wu, S.-J.; Shieh, S.-H.; Lai, Y.-J.; Shih, Y.-T.; Hwu, Y.-J. Effects of an Eating Ability Promotion Program for Community-Dwelling Older Adults. J. Am. Med. Dir. Assoc. 2020, 21, 1336–1340.e1. [Google Scholar] [CrossRef] [PubMed]
- Cassolato, S.F.; Turnbull, R.S. Xerostomia: Clinical Aspects and Treatment. Gerodontology 2003, 20, 64–77. [Google Scholar] [CrossRef] [PubMed]
- Bots-VantSpijker, P.C.; Bruers, J.J.M.; Bots, C.P.; Vanobbergen, J.N.O.; De Visschere, L.M.J.; de Baat, C.; Schols, J.M.G.A. Opinions of Dentists on the Barriers in Providing Oral Health Care to Community-Dwelling Frail Older People: A Questionnaire Survey. Gerodontology 2016, 33, 268–274. [Google Scholar] [CrossRef]
- Da Mata, C.; Allen, P.F. Providing Oral Healthcare to Older Patients-Do We Have What It Takes? Int. J. Environ. Res. Public Health 2023, 20, 6234. [Google Scholar] [CrossRef]
- Nakazawa, N.; Kusama, T.; Cooray, U.; Yamamoto, T.; Kiuchi, S.; Abbas, H.; Yamamoto, T.; Kondo, K.; Osaka, K.; Aida, J. Large Contribution of Oral Status for Death Among Modifiable Risk Factors in Older Adults: The Japan Gerontological Evaluation Study (JAGES) Prospective Cohort Study. J. Gerontol. A Biol. Sci. Med. Sci. 2023, 78, 167–173. [Google Scholar] [CrossRef] [PubMed]
| All Participants | Weight Change during Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|
| >5% Loss | ≤5% Change | >5% Gain | ||||||
| n | % | n | % | n | % | n | % | |
| Total | 63,602 | 100.0 | 9676 | 15.2 | 47,331 | 74.4 | 6595 | 10.4 |
| Number of remaining teeth | ||||||||
| ≥20 teeth | 38,210 | 100.0 | 5203 | 13.6 | 29,254 | 76.6 | 3753 | 9.8 |
| 10–19 teeth | 12,954 | 100.0 | 2173 | 16.8 | 9390 | 72.5 | 1390 | 10.7 |
| 0–9 teeth | 12,438 | 100.0 | 2299 | 18.5 | 8687 | 69.8 | 1452 | 11.7 |
| Chewing difficulty | ||||||||
| No | 48,421 | 100.0 | 7021 | 14.5 | 36,534 | 75.5 | 4866 | 10.0 |
| Yes | 15,181 | 100.0 | 2655 | 17.5 | 10,797 | 71.1 | 1729 | 11.4 |
| Swallowing problems | ||||||||
| No | 52,882 | 100.0 | 7958 | 15.0 | 39,464 | 74.7 | 5460 | 10.3 |
| Yes | 10,720 | 100.0 | 1718 | 16.0 | 7867 | 73.4 | 1135 | 10.6 |
| Xerostomia | ||||||||
| No | 51,742 | 100.0 | 7627 | 14.7 | 38,862 | 75.1 | 5252 | 10.2 |
| Yes | 11,860 | 100.0 | 2049 | 17.3 | 8469 | 71.4 | 1343 | 11.3 |
| Sex | ||||||||
| Men | 30,427 | 100.0 | 4615 | 15.1 | 22,813 | 75.0 | 2999 | 9.9 |
| Women | 33,175 | 100.0 | 5061 | 15.3 | 24,518 | 73.9 | 3596 | 10.8 |
| Age | ||||||||
| 65–69 | 21,426 | 100.0 | 2698 | 12.6 | 16,341 | 76.3 | 2387 | 11.1 |
| 70–74 | 19,138 | 100.0 | 2635 | 13.8 | 14,510 | 75.8 | 1993 | 10.4 |
| 75–79 | 14,424 | 100.0 | 2363 | 16.4 | 10,642 | 73.8 | 1419 | 9.8 |
| 80–84 | 6604 | 100.0 | 1431 | 21.7 | 4579 | 69.3 | 594 | 9.0 |
| 85– | 2010 | 100.0 | 549 | 27.3 | 1259 | 62.6 | 202 | 10.1 |
| Smoking status | ||||||||
| Never | 6395 | 100.0 | 1092 | 17.1 | 4443 | 69.5 | 860 | 13.5 |
| Past | 19,189 | 100.0 | 2884 | 15.0 | 14,440 | 75.3 | 1865 | 9.7 |
| Current | 38,018 | 100.0 | 5701 | 15.0 | 28,448 | 74.8 | 3869 | 10.2 |
| Alcohol consumption | ||||||||
| Never | 26,815 | 100.0 | 3754 | 14.0 | 20,446 | 76.2 | 2615 | 9.8 |
| Past | 6002 | 100.0 | 1020 | 17.0 | 4247 | 70.8 | 734 | 12.2 |
| Current | 30,785 | 100.0 | 4901 | 16.0 | 22,638 | 73.5 | 3246 | 10.5 |
| Comorbidities | ||||||||
| Hypertension | 27,418 | 100.0 | 4456 | 16.2 | 20,197 | 73.7 | 2765 | 10.1 |
| Diabetes | 7792 | 100.0 | 1566 | 20.1 | 5543 | 71.1 | 683 | 8.8 |
| Cancer | 2324 | 100.0 | 382 | 16.4 | 1638 | 70.5 | 304 | 13.1 |
| Stroke | 1404 | 100.0 | 238 | 16.9 | 997 | 71.1 | 169 | 12.0 |
| Marital status | ||||||||
| Without a spouse | 15,050 | 100.0 | 2422 | 16.1 | 10,910 | 72.5 | 1718 | 11.4 |
| With a spouse | 48,552 | 100.0 | 7254 | 14.9 | 36,421 | 75.0 | 4877 | 10.1 |
| Education (year) | ||||||||
| ≤9 | 16,610 | 100.0 | 2885 | 17.4 | 11,864 | 71.4 | 1861 | 11.2 |
| 10–12 | 27,982 | 100.0 | 4111 | 14.7 | 20,957 | 74.9 | 2914 | 10.4 |
| ≥13 | 19,010 | 100.0 | 2680 | 14.1 | 14,510 | 76.3 | 1820 | 9.6 |
| Equivalent income (million JPY) | ||||||||
| <2.00 | 28,872 | 100.0 | 4714 | 16.3 | 21,011 | 72.8 | 3146 | 10.9 |
| 2.00–4.00 | 27,036 | 100.0 | 3895 | 14.4 | 20,435 | 75.6 | 2706 | 10.0 |
| >4.00 | 7694 | 100.0 | 1067 | 13.9 | 5884 | 76.5 | 743 | 9.6 |
| Denture use | ||||||||
| No | 23,793 | 100.0 | 3347 | 14.1 | 18,032 | 75.8 | 2414 | 10.1 |
| Yes | 39,809 | 100.0 | 6329 | 15.9 | 29,299 | 73.6 | 4181 | 10.5 |
| Walking time (min/day) | ||||||||
| <30 | 14,677 | 100.0 | 2638 | 18.0 | 10,390 | 70.8 | 1649 | 11.2 |
| 30–59 | 23,958 | 100.0 | 3636 | 15.2 | 17,989 | 75.1 | 2333 | 9.7 |
| ≥60 | 24,967 | 100.0 | 3402 | 13.6 | 18,952 | 75.9 | 2613 | 10.5 |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Body mass index | 22.8 | (3.0) | 23.5 | (3.3) | 22.8 | (2.9) | 22.0 | (3.0) |
| >5% Weight Loss | >5% Weight Gain | |||
|---|---|---|---|---|
| (vs. ≤5% Weight Change) | (vs. ≤5% Weight Change) | |||
| (n = 57,007) | (n = 53,926) | |||
| Crude model RR (95% CI) | Adjusted model RR (95% CI) a | Crude model RR (95% CI) | Adjusted model RR (95% CI) a | |
| Oral health status | ||||
| Number of remaining teeth | ||||
| ≥20 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| 10–19 | 1.25 (1.19–1.30) *** | 1.16 (1.10–1.21) *** | 1.13 (1.07–1.20) *** | 1.13 (1.06–1.20) *** |
| 0–9 | 1.39 (1.33–1.45) *** | 1.17 (1.11–1.23) *** | 1.26 (1.19–1.33) *** | 1.23 (1.14–1.31) *** |
| Chewing difficulty | ||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Yes | 1.22 (1.18–1.27) *** | 1.12 (1.07–1.16) *** | 1.17 (1.12–1.24) *** | 1.09 (1.04–1.15) ** |
| Swallowing problems | ||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Yes | 1.07 (1.02–1.12) ** | 1.01 (0.97–1.06) | 1.04 (0.98–1.10) | 1.01 (0.95–1.08) |
| Xerostomia | ||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Yes | 1.19 (1.14–1.24) *** | 1.11 (1.06–1.16) *** | 1.15 (1.09–1.22) *** | 1.09 (1.03–1.15) ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shiota, C.; Kusama, T.; Takeuchi, K.; Kiuchi, S.; Osaka, K. Oral Hypofunction and Risk of Weight Change among Independent Older Adults. Nutrients 2023, 15, 4370. https://doi.org/10.3390/nu15204370
Shiota C, Kusama T, Takeuchi K, Kiuchi S, Osaka K. Oral Hypofunction and Risk of Weight Change among Independent Older Adults. Nutrients. 2023; 15(20):4370. https://doi.org/10.3390/nu15204370
Chicago/Turabian StyleShiota, Chihiro, Taro Kusama, Kenji Takeuchi, Sakura Kiuchi, and Ken Osaka. 2023. "Oral Hypofunction and Risk of Weight Change among Independent Older Adults" Nutrients 15, no. 20: 4370. https://doi.org/10.3390/nu15204370
APA StyleShiota, C., Kusama, T., Takeuchi, K., Kiuchi, S., & Osaka, K. (2023). Oral Hypofunction and Risk of Weight Change among Independent Older Adults. Nutrients, 15(20), 4370. https://doi.org/10.3390/nu15204370






